Antatomy Lec 9: Ch 8
1/36
Earn XP
Description and Tags
Spinal Cord and Nerve Roots
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
37 Terms
Segments of the spinal cord
Cervical (C1 - C8)
Thoracic (T1 - T12)
Lumbar (L1 - L5)
Sacral (S1 - S5)
Coccygeal (C01)
Where does the spinal chord end
Cornus medullaris at L1 or L2
Below that are nerve roots with no spinal cord, forming cauda equina
Tapers into filum terminale = thin strand of connective tissue running in the center of the cauda equina.
Cervical Enlargement
(C5 - T1) gives rise to roots for arms
Lumbosacral Enlargement
(L1 - S3) give rise to nerve roots for the legs
exiting nerve roots
Short distance from the spinal cord, before leaving the spinal canal, the sensory and motor nerve roots fuse to form a single mixed spinal nerve for each segment.
vertebral body
a sturdy cylindrical section of the bone located anteriorly
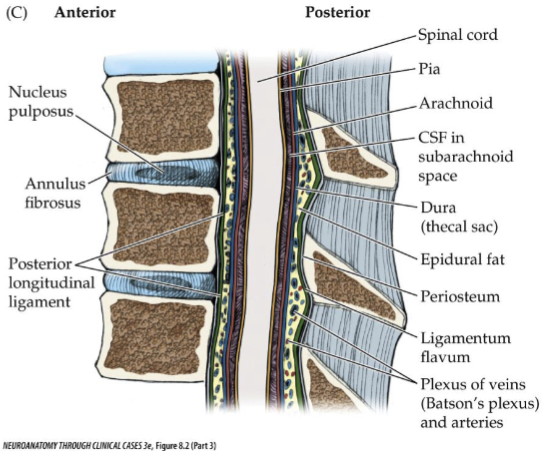
intervertebral discs
connective tissue that separates vertebral bodies from each other
consisting of:
Central nucleus pulposus surrounded by
A capsule called annulus fibrosus
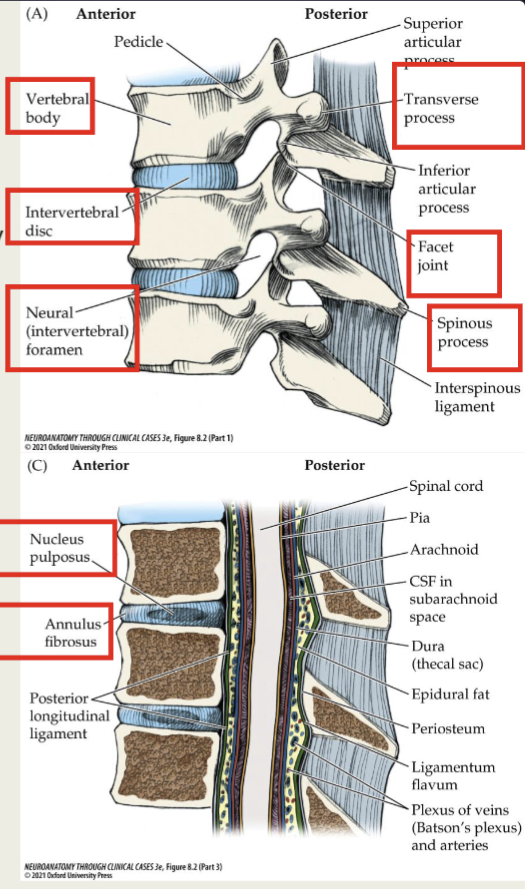
posterior arch of bone around the neural elements
– Pedicles
– Transverse processes
– Laminae
– Spinous processes
– Superior Articular Processes
– Inferior Articular Processes
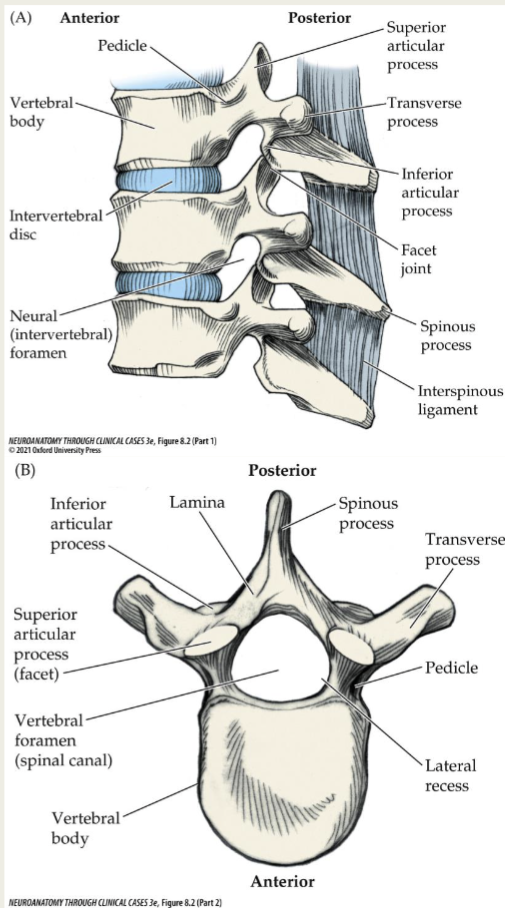
Spinal Cord runs through…surrounded by
the spinal canal (vertebral foramen)
– Pia
– Arachnoid
– Dura mater
– Epidural fat
– Periosteum
– Batson’s plexus – valveless meshwork of epidural veins
– Ligamentum flavum
Nerve Roots Exit via
he neural (intervertebral) formina
Disc herniations are most common at
cervical and lumbosacral levels
For both cervical and lumbosacral disc herniations, the nerve root involved usually corresponds to the lower of the adjacent two vertebrae
C5 - C6 disc herniation produces
C6 radiculopathy
L5 - S1 disc herniation produces
S1 radiculopathy
Thoracic, lumbar, and sacral nerve rooms exit…
below the correspondingly numbered vertebral bone
Unlike cervical roots, lumbar and sacral nerve roots must travel downward several levels before they exit the spinal canal.
Cervical roots exit
above the correspondingly numbered vertebral bones (except C8 = between C7 and T1)
– Fairly horizonal course as they emerge from the dural or thecal sac
– Cervical discs are constrained by the posterior longitudinal ligament
Far lateral disc herniation
– Will reach the nerve root exiting at that level
– Resulting in an impingement of the next higher nerve root
Example:
– Far lateral L4 - L5 disc herniation can cause an L4radiculopathy
– Central disc herniation at the level of the cauda equina can impinge on nerve roots lower than the level of herniation
Dermatome
sensory region of skin innervated by a nerve root
– Useful for clinically isolating lesions
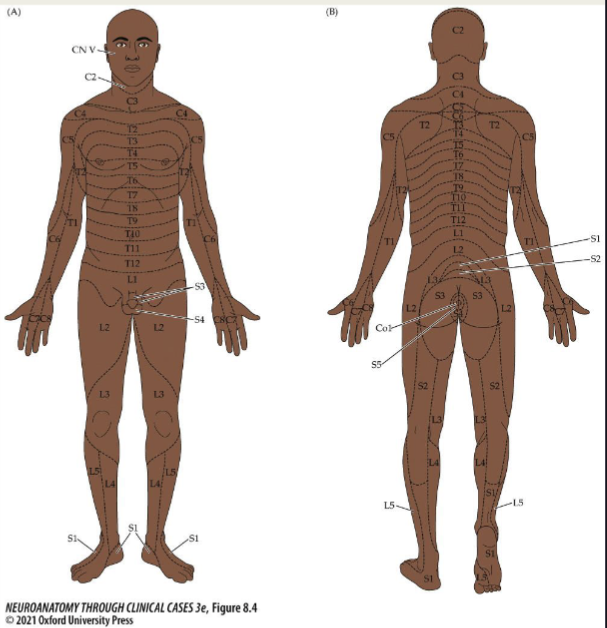
major dermatome locations cervical and thoracic
■ Sensation of the face is provided by the trigeminal nerve
■ Remainder of head is supplied by C2
■ Nipples are level of T4
■ Umbilicus is at T10
■ C5 through T1 represented on mainly upper extremities
■ C5 Shoulder
■ C6 Lateral arm and first two digits
■ C7 Middle digit
■ C8 fourth and fifth digits
major dermatome locations lumbar and sacral
■ L4 = extends over anteromedial shin
■ L5 = Extends down the anterolateral shin and dorsum of the foot to the big toe
■ S1 = small toe, lateral foot, sole and calf
■ S2, S3, and S4 innervate the perineal area in a saddle - like distribution
Myotome
muscles innervated by a single nerve root
Neuropathy
general term meaning nerve disorder
– Site of pathology can be in the axons, myelin, or both.
– Effect large - diameter, small - diameter fibers or both
– Reversible or permanent
– Focal (mononeuropathy), multifocal (mononeuropathy multiplex) or generalized (polyneuropathy).
– Neuropathy affecting the spinal nerve roots is called radiculopathy
Common neuropathies
Diabetes
Mechanical Causes
Infectious disorders
Toxins
Malnutrition
Immune disorders
Hereditary Neuropathies
Diabetes
– Compromise of microvascular blood supply
– Oxidative stress, autoimmunity, neurotrophic and biochemical disturbances
– Most common – distal symmetrical polyneuropathy– glove and stocking sensory loss.
– Acute diabetic mononeuropathy – can affect any cranial or spinal nerve (most common in CN III and the femoral and sciatic nerves)
Mechanical Causes
– Extrinsic compression, traction, laceration, or entrapment by intrinsic structures such as bone or connective tissue.
Neurapraxia
mild mechanical disruption of nerve and temporary impairment of nerve conduction
Wallerian degeneration
degeneration of axons and myelin distal to the site of injury
Complex Regional Pain Syndrome
occasional long - term complications include incomplete or aberrant reinnervation
■ Type 1 = reflex sympathetic dystrophy – more common and follows an injury without specific nerve damage
■ Type 2 = causalgia – follows damage to a specific nerve
Both have intense local burning pain accompanied by edema, sweating, and changes in skin blood supply
Infectious disorders
Lyme disease, HIV, CMV, varicella - zoster virus or hepatitis B
Immune disorders: Guillain-Barre syndrome
Caused by immune - mediated demyelination of peripheral nerves
Variant forms affect axons or nodes of Ranvie
Onset 1 - 2 weeks following a viral illness (Campylobacter, HIV, or other infections)
Presentation – ascending progressive weakness, areflexia, and tingling paresthesia of the hands and feet, with motor involvement more severe than sensory.
Diagnosis = clinical presentation, CSF with elevated protein, EMG that detects demyelination
Treatment = plasmapheresis or intravenous immunoglobulin therapy
Myasthenia gravis
– Immune - mediated disorder in which there are circulating antibodies against the postsynaptic nicotinic acetylcholine receptors at the neuromuscular junction of skeletal muscles
– Can be accompanied by other autoimmune phenomena such as hypothyroidism, lupus, rheumatoid arthritis, and vitiligo
Myasthenia gravis: clinical features, diagnosis and treatment
Clinical features include: generalized symmetrical weakness, especially of proximal limb muscles, neck muscle, the diaphragm, and eyes muscles
– Weakness becomes more severe with repeated us of a muscle
– Diagnosis: based on clinical feature and several diagnostic tests (ice pack test, repetitive nerve stimulation, measurement of antibodies, single - fiber EMG, and chest CT or MRI
– Treatment : Immune therapy
Myopathies
“muscle disorders”
Produce weakness that is more severe proximally than distally
Myosotis
immune - mediated inflammatory myopathy
– Sporadic inclusion body myositis
– Dermatomyositis
– Polymyositis
– Necrotizing myopathy
– Duchenne muscular dystrophy = most common form of muscular dystrophy
Radiculopathy
Sensory or motor dysfunction caused by pathology of the nerve root.
Burning, tingling pain that radiates down a limb in the dermatome of the affected root
Chronic radiculopathy can result in atrophy and fasciculations
Common cause if disc herniation
– Nucleus pulposus extrudes through a tear in the annulus fibrosus
Radiculopathy location likelihood
■ Lumbosacral 2 - 3X more common than cervical
■ Thoracic spine is less mobile = unlikely herniation
Common Causes of Radiculopathy
■ Disc herniation
■ Osteophytes
Bony growths
■ Spinal stenosis
Narrowing of the spinal canal
■ Trauma
■ Diabetes
■ Epidural abscess
■ Epidural metastases
■ Meningeal carcinomatosis
■ Nerve sheath tumors (schwannomas and neurofibromas)
■ Guillain – Barré syndrome
■ Herpes zoster (shingles)
■ Lyme disease
■ Cytomegalovirus
■ Idiopathic neuritis
Cauda equina syndrome
■ Impaired fxn of multiple nerve roots below L1 or L2
■ Sensory loss in a S2 to S5 distribution
Saddle anesthesia
Other symptoms include: urinary retention, constipation, decreased recal tone, fecal incontinence, ED