PA exam #2
1/97
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
98 Terms
Anterior Thoracic Cage
Suprasternal notch, Sternum, manubriosternal angle (angle of louis), costal angle
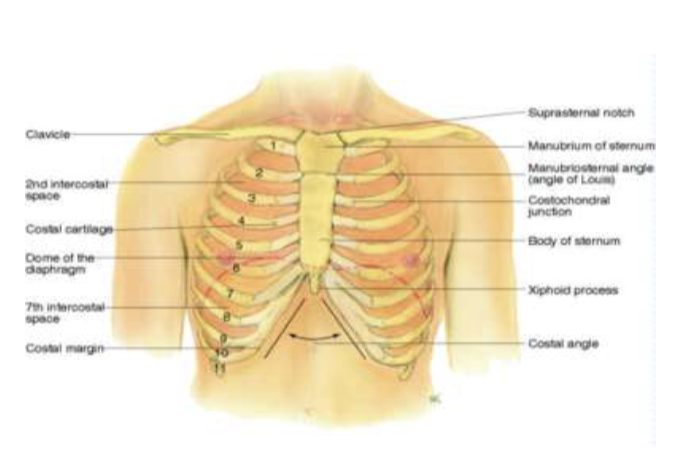
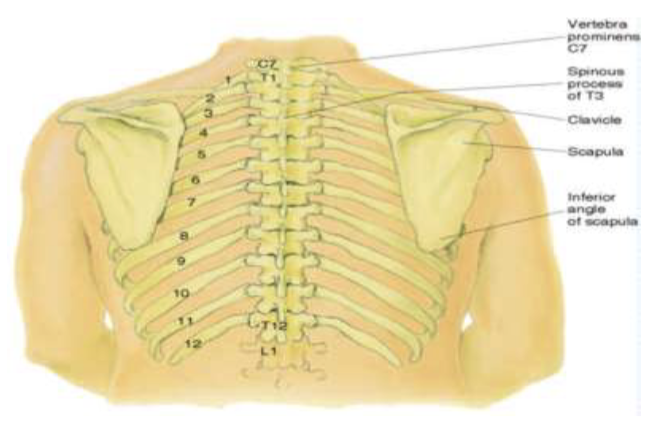
Posterior Thoracic Cage
Vertebra Prominens (C7), Spinous Processes, Inferior border of the scapula (7th or 8th rib), 12th rib (palpate midway between spine and side to find the location free tip_
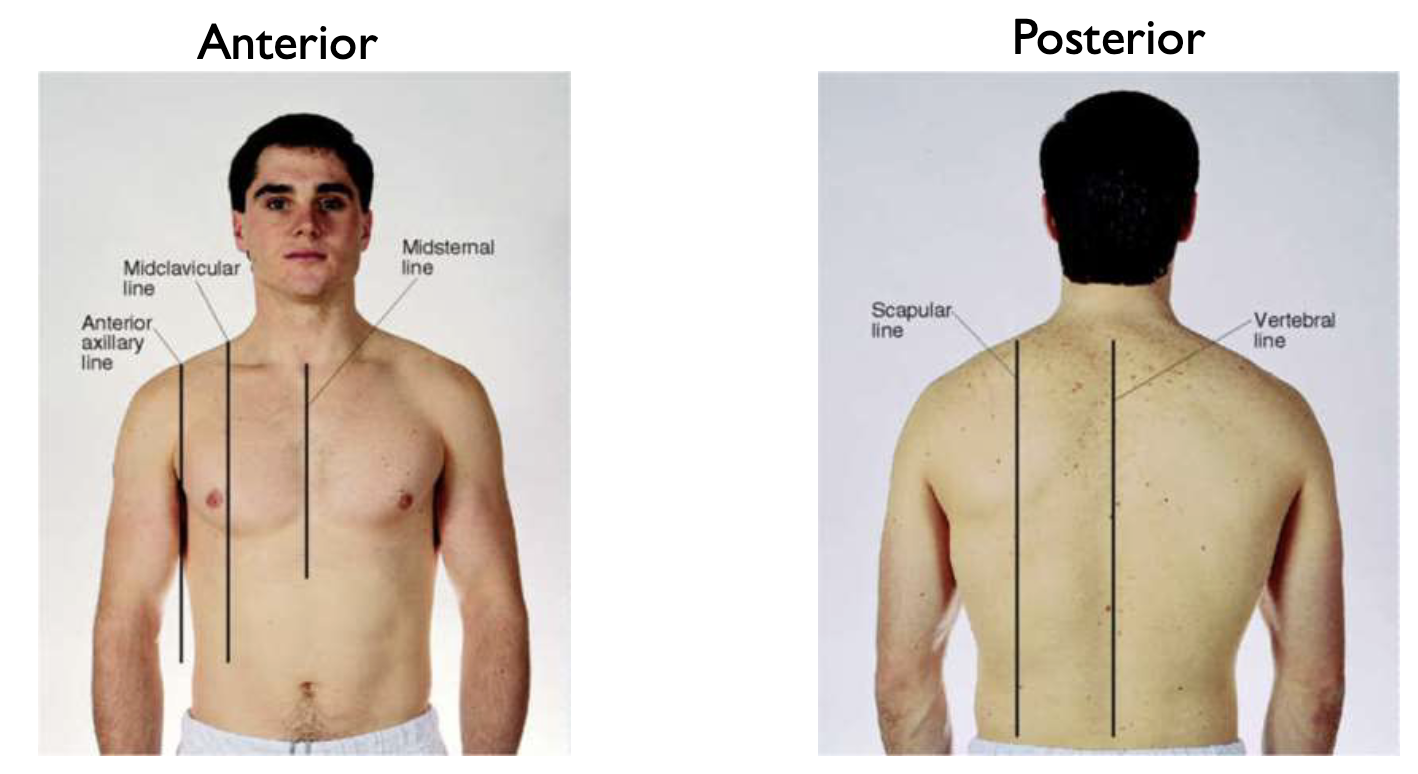
Reference Lines (anterior + posterior)
Anterior Axillary Line, Midclavicular line, midsternal line, scapular line, vertebral line
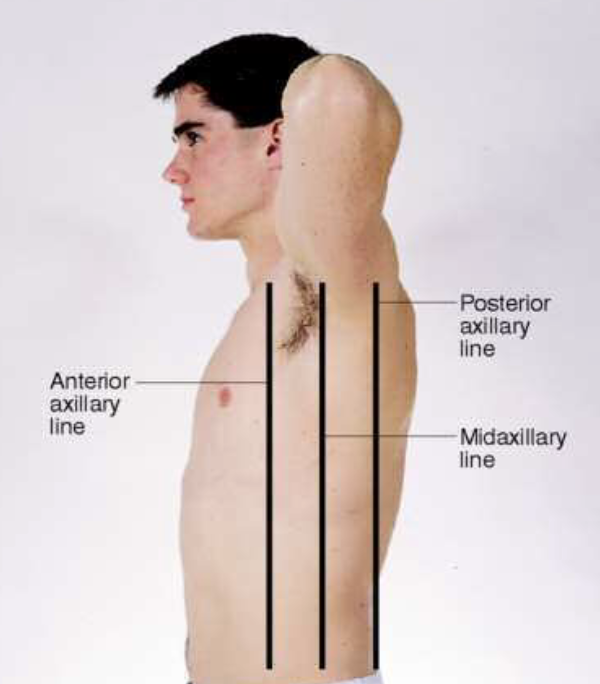
Lateral Reference Lines
anterior axillary, posterior axillary, midaxillary lines
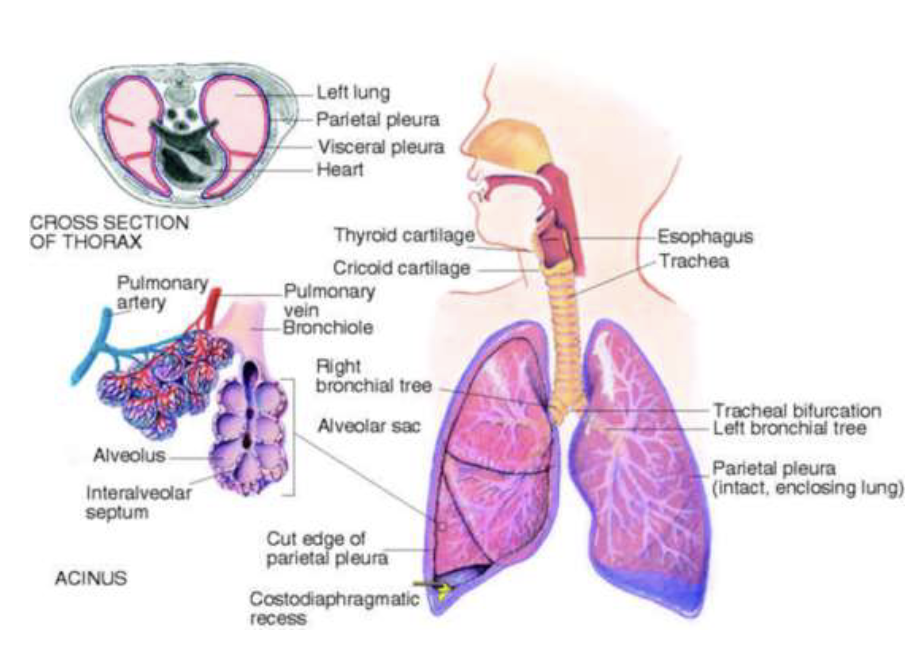
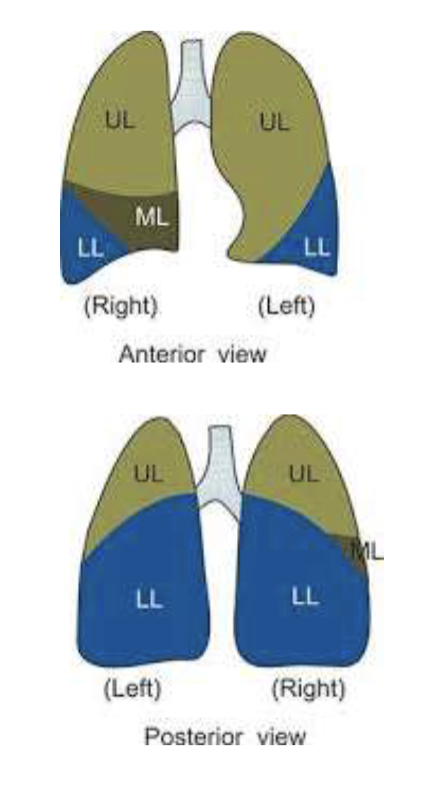
Structure of Lungs
Pleurae (visceral, parietal), Costodiaphragmatic recess, trachea, bronchial tree
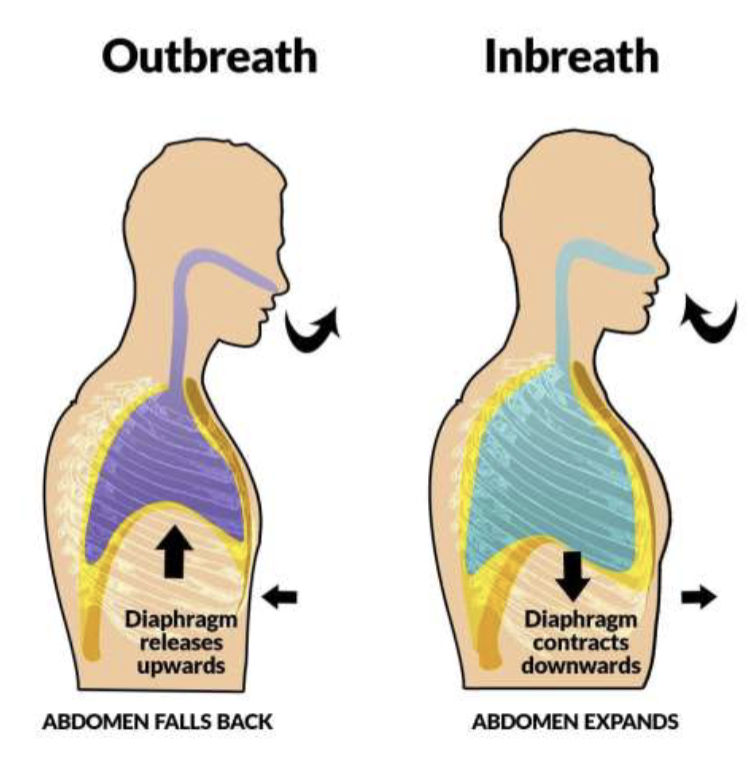
Mechanics of Ventilation
supply O2 to body for energy production, remove CO2 as a waste product, maintain acid-base balances of arterial blood, maintain heart exchange
Thoracic Past Medical History (PMH)
ask patient about…
existing respiratory diagnosis
allergies
lung injury
history of intubation
smoking
respiratory exposure
previous thoracic surgeries
lung disease/cancer in family
Thoracic Review of Systems (ROS)
Frequent respiratory infections, cough, sputum production (hemoptysis = blood-streaked sputum), dyspnea (SOB), dyspnea on exertion, wheezing, orthopnea, chest pain with breathing
Trauma Informed Care
realizing the widespread impacts of trauma, recognizing signs and symptoms of trauma, responding by fully integrating knowledge about trauma into policies, procedures and practices, seeking to actively resist re-traumatization
Thoracic Physical Exam Overview
Inspection
Respiratory excursion
Palpate for tactile fremitus
Percuss for symmetry
Diaphragmatic excursion
Auscultate posterior chest
Repeat inspection, palpation, percussion and auscultation on anterior chest
Thoracic: Inspection
observe for signs of respiratory distress
note skin abnormalities/color
note shape and configuration of chest wall
listen for any audible sounds of breathing (wheezing, stridor, whistling)
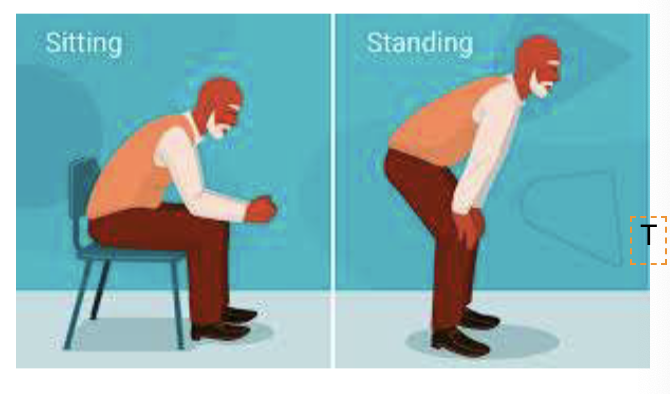
Tripod Positioning
It's commonly adopted by individuals experiencing shortness of breath or respiratory distress, as it can help improve breathing
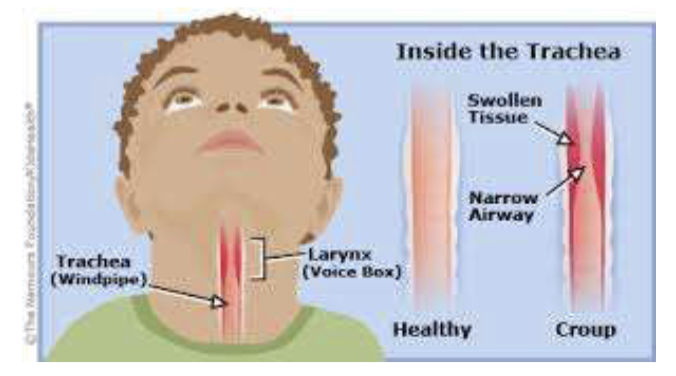
Stridor
Abnormal Finding! Medical emergency!
audible harsh, high pitched, crowing sounds associated with airway obstruction in or near the larynx
can be heard on inspiration and/or expiration
May hear with or without a stethoscope
Medical emergency
Ex: croup, epiglottitis, foreign body aspiration, airway edema from anaphylaxis
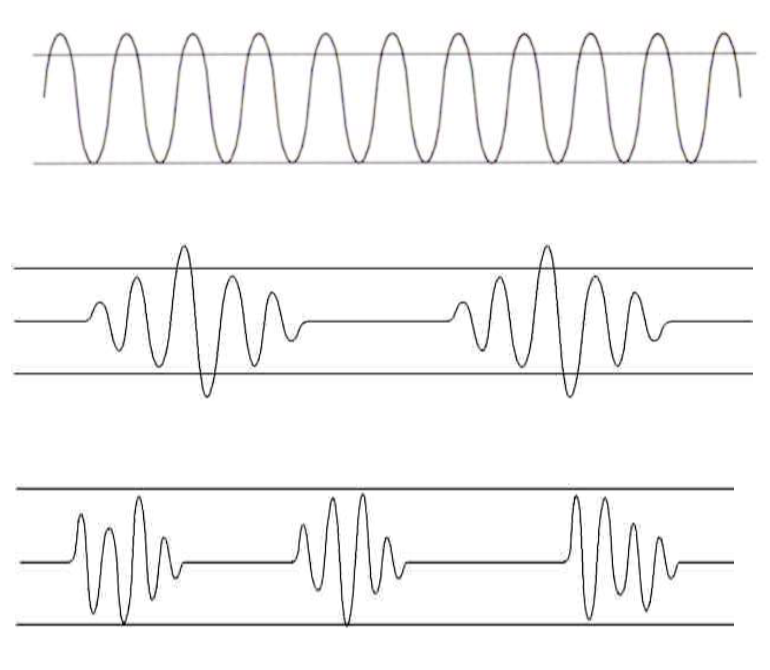
Respiration Patterns
Normal Breathing,
Sigh,
Tachypnea (shallow breathing >20/min),
Bradypnea (<12/min, with or without a change in tidal volume),
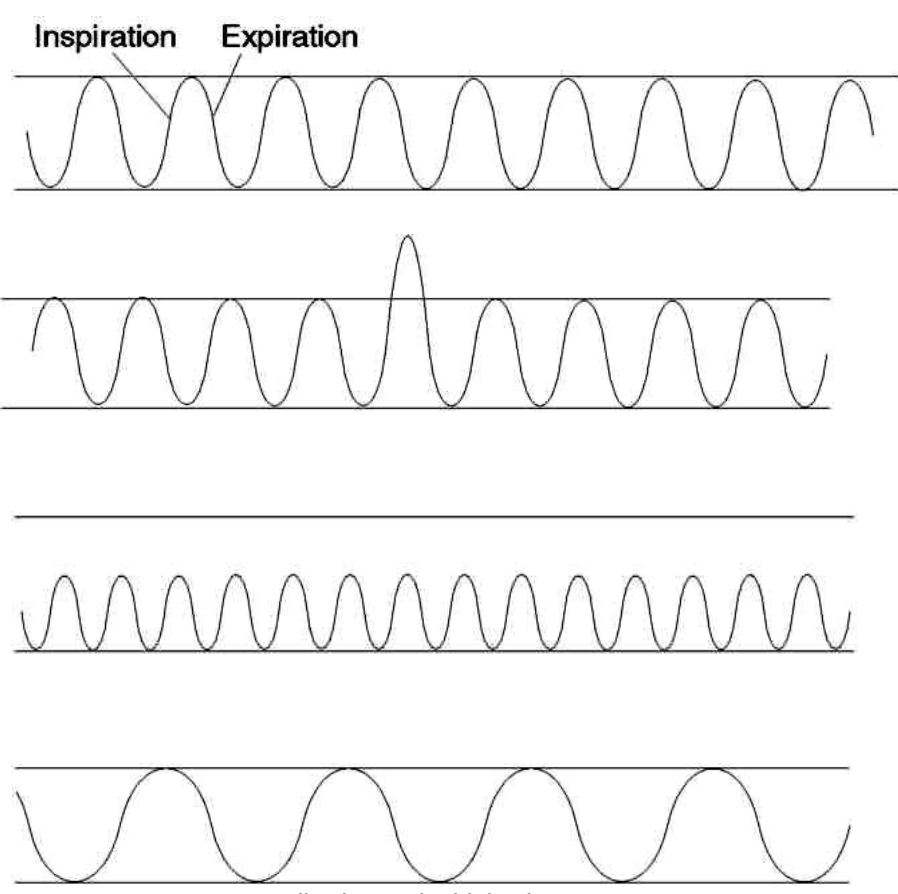
Respiration Patterns Contd.
Hyperventilation (more than standard tidal volume ex: Kyssmaul breathing)
Cheyne-Stokes (death and dying breathing pattern with periods of apnea (no breathing) and then kicks in with increased tidal volume and then decreases)
Ataxic Breathing - Biot’s (brain dead)
Paradoxical Breathing (brain injury, diaphragm moves in opposite direction than it should during inspiration and expiration causing the lung to deflate during inspiration)
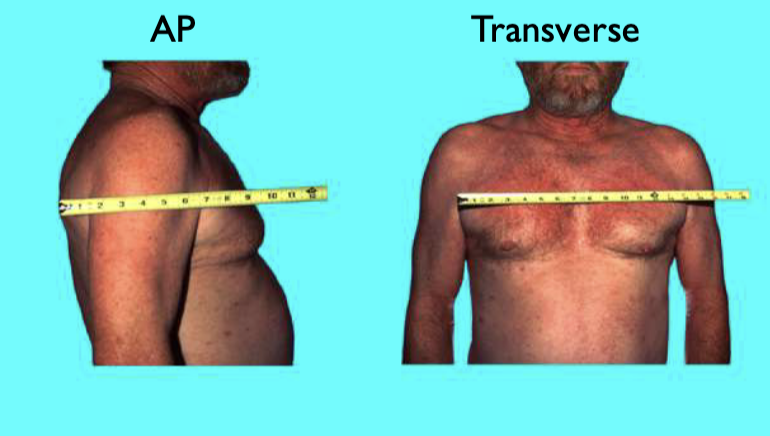
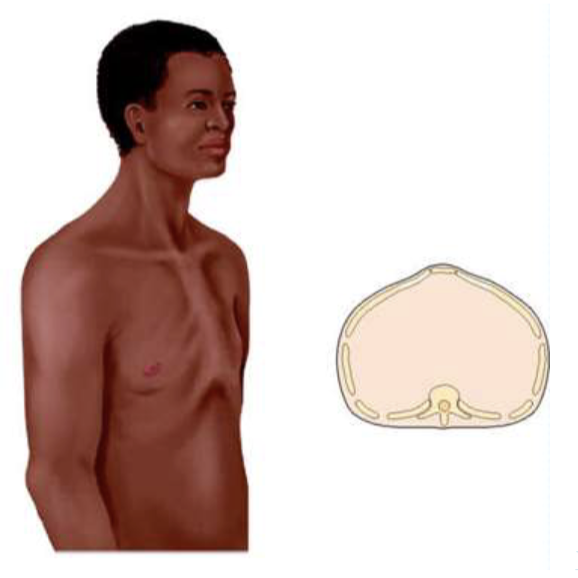
Thoracic Inspection:
AP: Transverse Ratio
normal anteroposterior:transverse ration = 1:2
Costal angle should be around 90 degrees
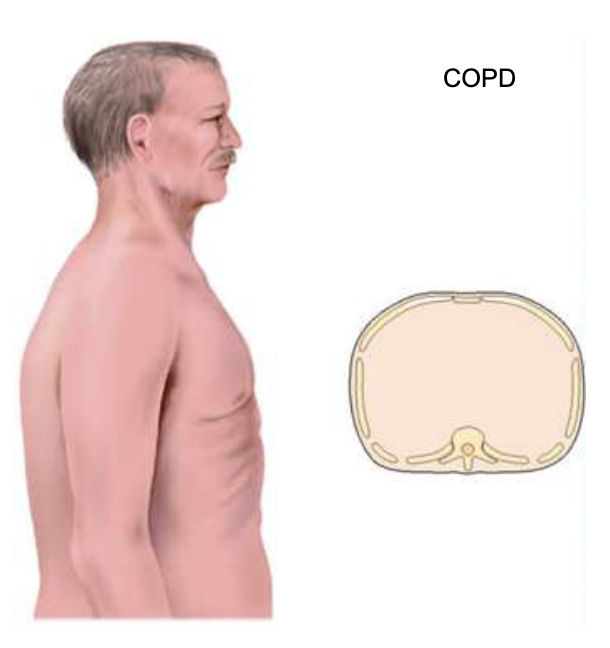
Abnormal Configurations of the Thorax
Barrel Chested (COPD), Pectus excavatum, Pectus Carinatum, Kyphoscoliosis, Kyphosis,
Barrel Chested
abnormal, COPD
Pectus Excavatum
abnormal, more dangerous because the sternum is tucked in and there’s pressure on the underlying organs

Pectus Carinatum
abnormal
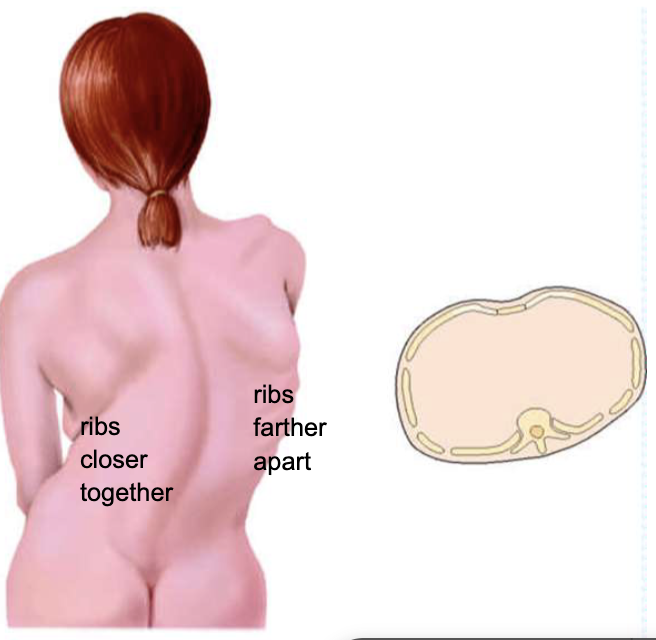
Kyphoscoliosis
abnormal, ribs closer together on one side and ribs rather apart on other
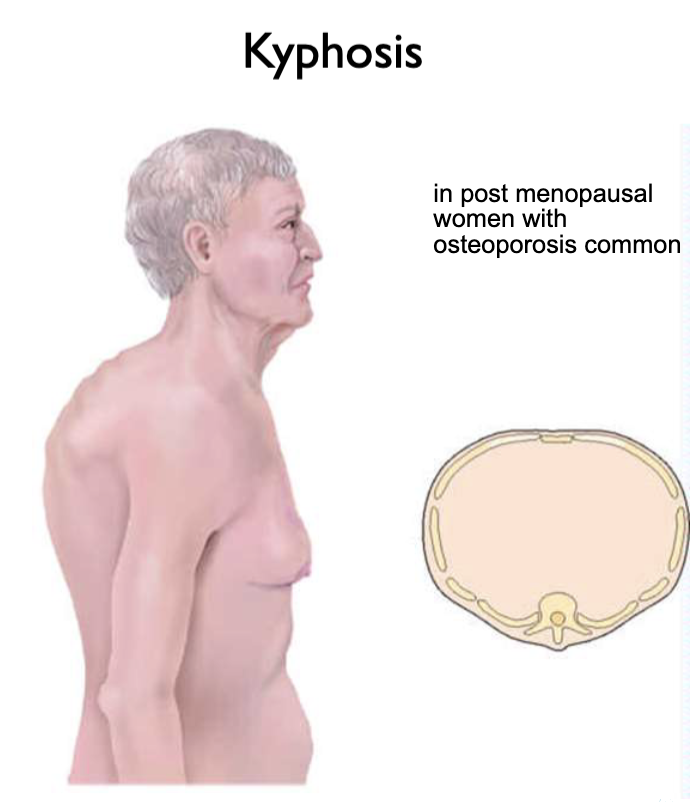
Kyphosis
abnormal, common in post-menopausal women with osteoporosis
Infant Thorax
Developmental Considerations! Barrel Chest in infant is normal!
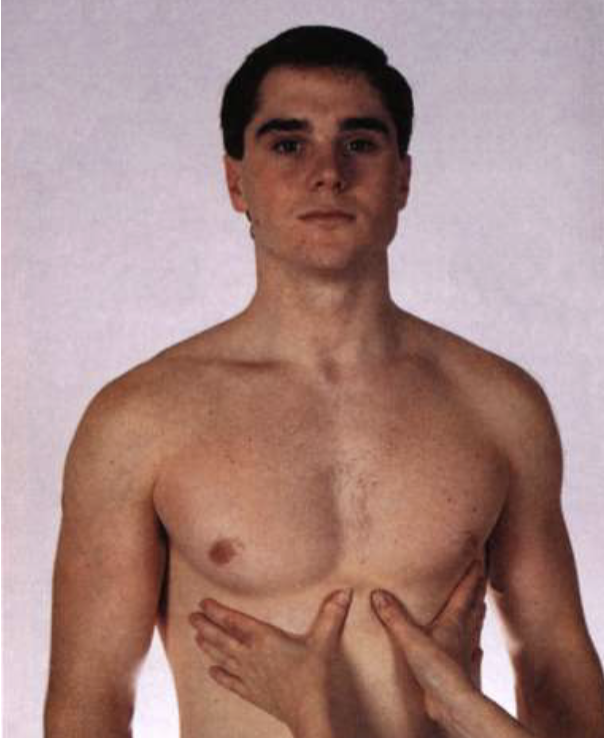
Palpate for symmetric Chest Expansion
Place both hands on posterior chest with thumbs at T9 or T10
Pinch up a small fold of skin
Ask person to take a deep breath
Thumbs should move apart symmetrically
HOT TIP: T7 is in line with the inferior tip of scapula
Normal finding: symmetrical expansion of the chest

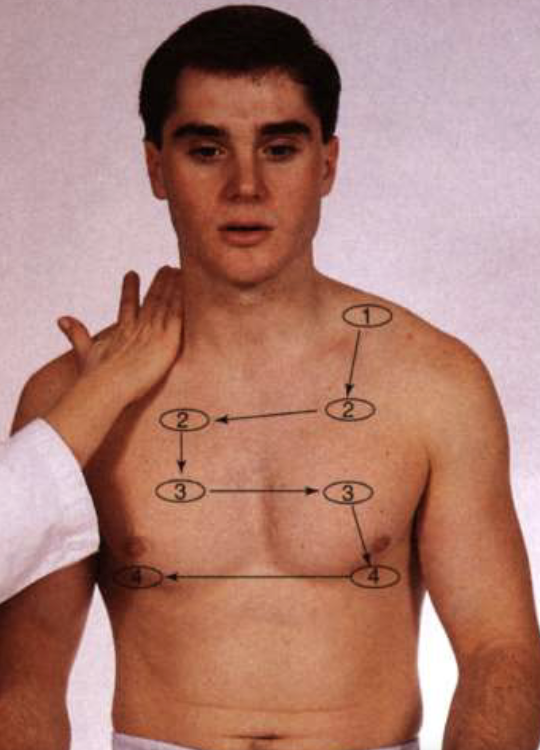
Palpate for tactile fremitus
Use palmar base of fingers or ulnar edge, touch chest while patient says “ninety-nine”
Start over apices and palpate from side to side to make a comparison
Normal finding: symmetrical vibrations
HOT TIP: the vibrations of sounds are conducted BETTER through a DENSE OR SOLID structure than a porous one so anything that increases density of lung will increase fremitus
Hear it louder over tumor
Air = porous

Thoracic: Percussion - Good Technique
ask the patient to cross their arms to spread the back
hyperextend your middle finger and press distal interphalangeal joint firmly in the intercostal space
Ideally no other finger will touch the chest wall (will dampen sound)
Use tip of your opposite middle finger to strike the distal joint with firm and quick strokes
Use the lightest pressure that produces a clear note and increase striking power if needed for a thicker chest wall
Start at the apices and move from side to side for comparison as you move downward to about T10
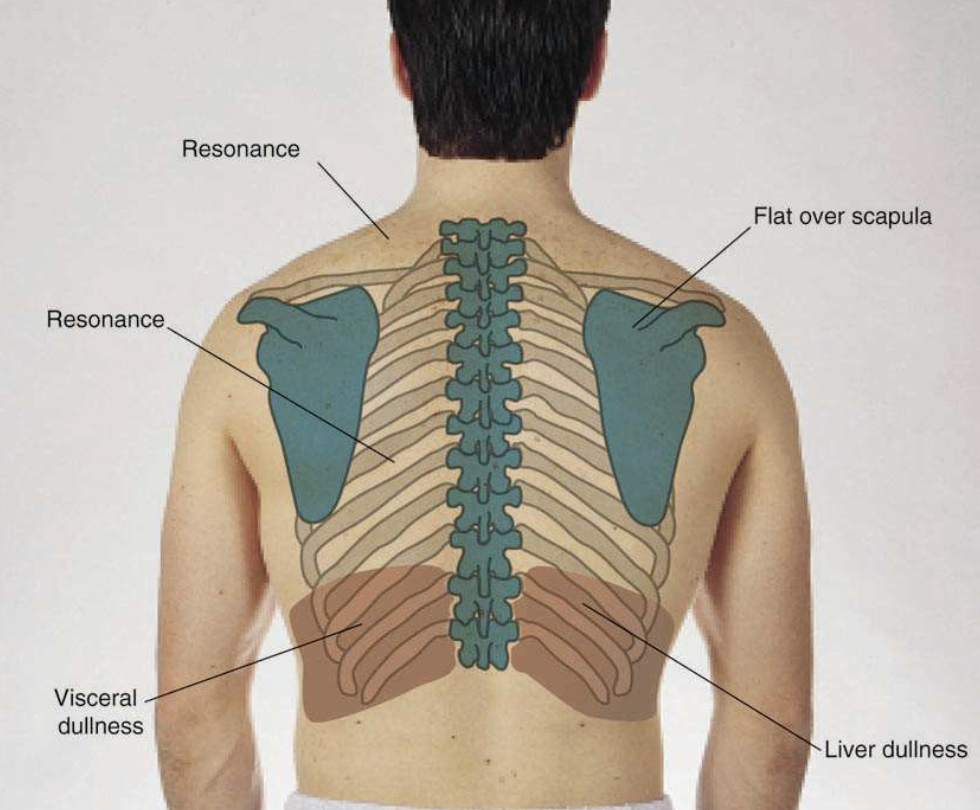
Percussion of the posterior Chest
percussion helps to establish whether the underlying tissues are air-filled, fluid-filled, or consolidated
Consolidation: when the air that usually fills the small airways in your lungs is replaced with pus, blood, water or a solid)

General Principles for Percussion Notes
Percussion produces sound that reflects the density of the underlying structure
Structures with more internal air (lungs) produce a louder, deeper and longer percussion notes because the sound can vibrate more freely
A denser, more solid structure (liver) gives a softer highter, shorter percussion not because the internal fluid/dense tissue restricts sounds from vibrating as freely
The depth of percussion has limits: vibrations produced from percussion only reaches a depth of about 5cms
Percussion Notes
Flat
Dull
Tympany
Resonance
Hyperesonance
Flat
more dense/solid tissue
Very soft, high pitched, short duration
Heard over very dense tissue (bone or muscle)
Dull
More dense/solid tissue
soft, muffled, moderate to high pitched, short duration
normal finding over dense fluid filled tissue such as the liver
If heard over the lung field, may indicate lobar pneumonia
Tympany
loud, drum like, high pitched or musical sounds, moderately long duration
Normal heard over enclosed air/fluid filled cavities (ex: stomach, bowel, bladder)
If heard in lung may be large pneumothorax
Resonance
Less dense/more air tissue
Moderate to loud, low pitched (clear hollow), moderate duration
Normally heard over air filled tissues (healthy lung tissue)
Hyperresonance
less dense/more air tissue
loud booming, very low pitched, long duration,
hyperinflated lungs as with COPD (overfilled balloon)
Expected Percussion Notes on Posterior Chest
Diaphragmatic Excursion
Diaphragmatic Excursing is the descent of the diaphragm with respirations
percuss for diaphragmatic excursion
assess degree of symmetry for diaphragm movement with respiration
Normal excursion = 3-5.5cms and symmetrical bilaterally
HOT TIP: you aren’t percussing the actual diaphragm, but rather the boundary between the resonant lung tissue and the duller structures below
Absent decent of the diaphragm can indicate pleural effusion or atelectasis of lower lobe on the affected side
Auscultate Posterior Lung Fields
Listen in a similar pattern as percussion for side to side comparison while the patient takes deep breaths
Use the DIAPHRAGM and hold firmly against bare skin
Listen in each location for one full respiration starting at the apices (C7) to the bases (T10), as well as laterally from axilla down to 8th/9th rib
Healthy lungs will be clear to auscultation (CTA)
Normal Breath Sounds by Location
Bronchial (tracheal) = loud, course, blowing sound, normal over trachea, length of inspiration heard < or = expiration
Bronchovesicular = medium pitched, moderately loud, normal over mainstem bronchi, length of inspiration heard = expiration
NOT normal to hear bronchovesicular in the peripheral lung field
Vesicular = soft/low pitched breezy sound, normal over peripheral lung fields, length of inspiration is heard > expiration
General Principles of Breath Sound Volume
Normal, air-filled lungs are insulators of sound coming from within (voice/breath sounds)
Vocal sounds from within the lung travel more easily through liquid (or densities) compared to air, therefore breath sounds are louder over areas of consolidation in the lung.
Breath sounds are quieter than normal over areas where fluid or air has accumulated within the pleural space because there is a physical barrier preventing the sound from making it to your stethoscope.
When there is an airway blockage (food, mucous plug, etc), you will note diminished or absent breath sounds in areas distal to that blockage due to the prevention of air flow to those airways.
Adventitious Breath Sounds
Abnormal!
Fine Crackles (like hair twisting)
crackling or popping, commonly heard on late inspiration
caused by air colliding with secretions or small airways popping open
Course Crackles (like velcro)
harsh, moist popping/bubbling sounds heard on early inspiration
caused by air bubbles moving through secretions in the large bronchi
Adventitious Breath Sounds Contd.
Abnormal!
Wheezes
Sonorous (Ronchi)
low pitched snoring sounds most heard on expiration
Single note like musical snoring or moaning
Caused by blockages in the main airways by secretions, foreign body or a mass (ex: bronchitis)
Sibilant
squeaky sound heard during inspiration and expiration
caused by narrowed/blocked airways as with asthma attack
Pleural Friction Rub
Grating sound heard during inspiration and expiration
Occurs when the pleura become inflamed and rub together
Ex: Pleurisy, pneumonia, pulmonary embolism lung cancer
Transmitted Voice Sounds
Only do test if there’s abnormal bronchovesicular or bronchial breath sounds
Assess the transmitted voice sounds using on of these techniques (indicative of underlying consolidation if present)
Bronchophony
Egophony
Whispered Pectoriloquy
Bronchophony
listen while the patient ways “99”
NORMALLY sounds are muffled/indistinct
IF BRONCHOPHONY IS PRESENT, sounds will be louder/clear, indicating abnormality like pneumonia
Egophony
Listen while the patient says “EE”
NORMALLY will hear a muffled long E sound
IF EGOPHONY IS PRESENT, the E will sound like an A and may indicate pneumonia
Whispered Pectoriloquy
Listen while patient whispers “99”
NORMALLY faint/absent sound
IF WHISPERED PECTORILOQUY, louder clear whispered “99”
Inspection: Anterior Chest Wall
shape and configuration of chest wall (not deformities or asymmetry)
accessory muscles (not any retractions)
Palpate for Symmetric Anterior Chest Expansion
Palpate for Tactile Fremitus
may use ball of palm or the ulnar surface of the hand
If breasts are present, gently displace the tissue to assess beneath as necessary
Normal finding: equal bilaterally
Percuss the anterior Chest
Auscultate Anterior Chest
RML is auscultated best on the anterior chest
Summary of Healthy Lung Exam Findings
Trachea = midline
Tactile Fremitus = normal/symmetrical
Percussion = resonant
Breath Sounds = vesicular except over large bronchi or trachea
Adventitious Sounds = none
Tracheobronchial tree and alveoli are clear, pleurae are thin and close together, mobility of chest wall is unimpaired
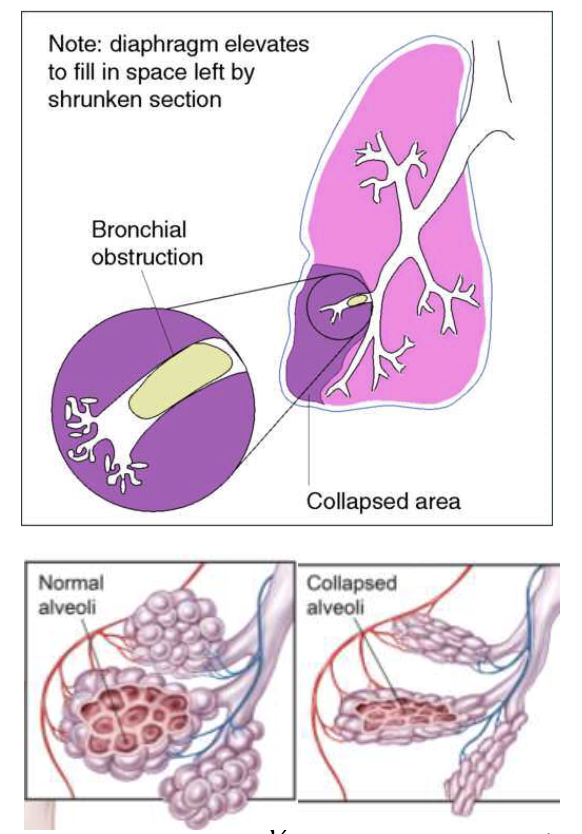
Atelectasis
Partial Lobar Obstruction, Abnormal! Collapse of the alveoli due to mucous plug, foreign body or due to surrounding pressure
trachea = may be shifted towards involved side in SEVERE situations
tactile fremitus = decreased to absent over the affected area
percussion = dull over collapsed airless area only
breath sounds = decreased or absent over collapsed airless airleas
adventitious sounds = may have wheezes (rhonchi) and crackles depending on severity
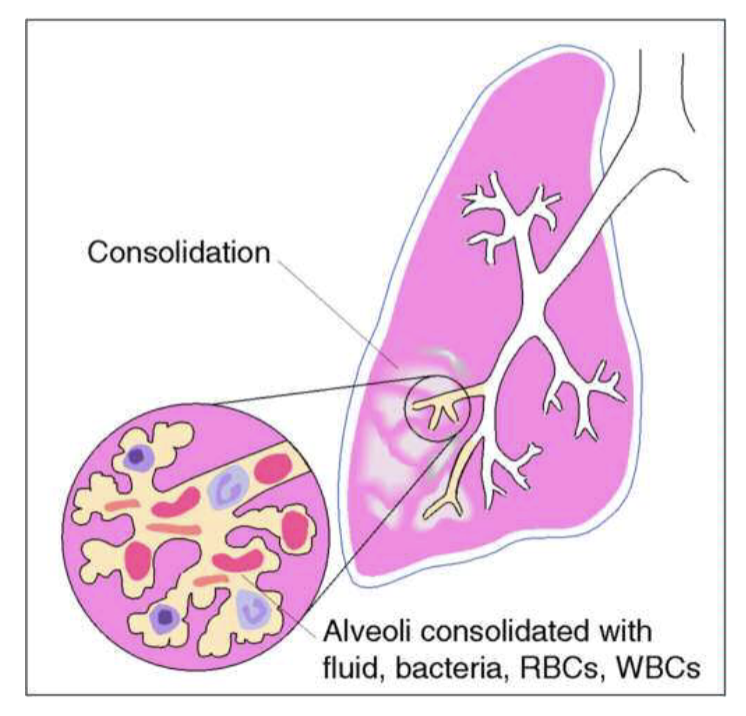
Consolidation
Lobar Pneumonia, Abnormal! Infection causing the alveoli to fill with fluid, bacteria, blood and pus
Trachea = midline
Tactile Fremitus = increased over involved are with bronchophony
Percussion = dull over involved are
Breath Sounds = bronchial over involved area (should be vesicular)
Adventitious sounds = crackles over involved area
may be accompanied by fever
Pneumonia
fluid in alveoli and inflamed bronchiole
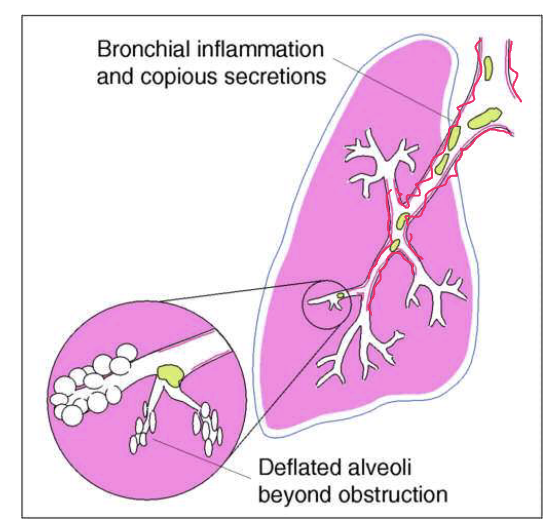
Bronchitis
inflammation of the bronchi (usually chronically), causing mucous build up
trachea = midline
tactile fremitus = normal
percussion = resonant
breath sounds = vesicular except perhaps over large bronchi or trachea
Adventitious sounds = non OR course crackles and/or sonorous wheezes (rhonchi)
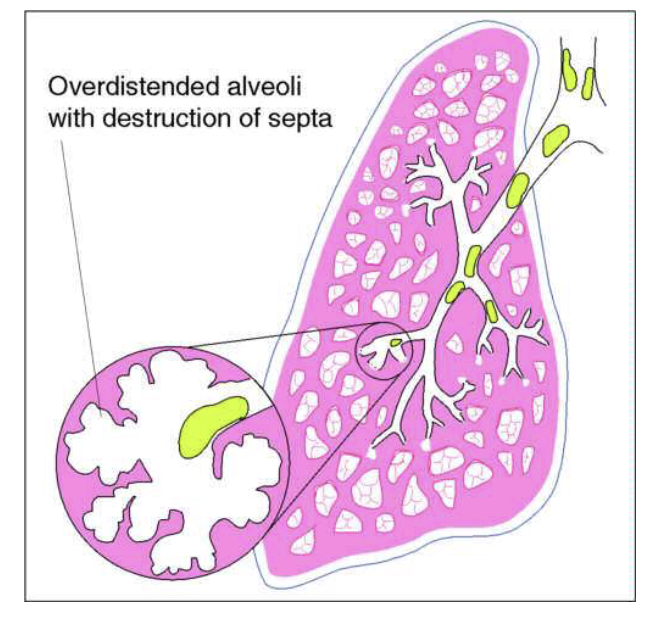
Emphysema
slowly progressive disorder (often due to smoking) in which the distal air spaces enlarge, and lungs become hyperinflated; often also develops chronic bronchitis
trachea = midline
tactile fremitus = decreased
percussion = hyper-resonant
breath sounds = decreased to absent
adventitious sounds = none or scattered coarse crackles and/or sonorous wheezes (rhonchi) associated with chronic bronchitis
Over time will develop barrel chest, severe DOE, and decreased diaphragmatic excursion
COPD
exhalation is the problem, still left over air that’s trapped, so over time it increases!
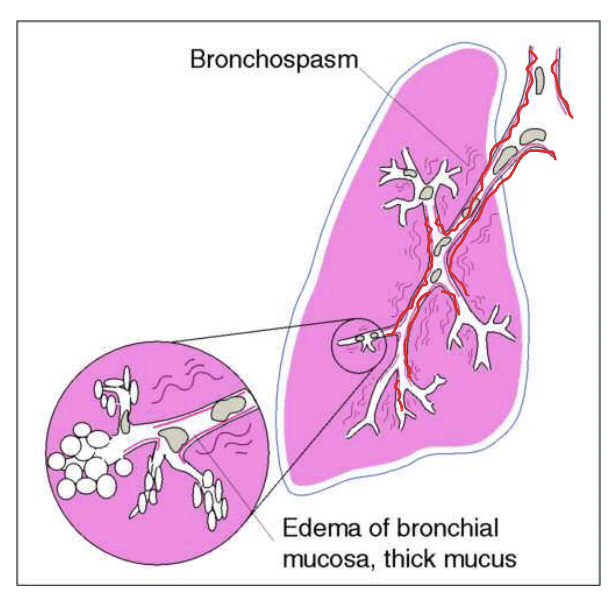
Asthma
widespread, usually intermittent and reversible narrowing of the tracheobronchial tree (bronchospasm and underlying inflammation), diminishing airflow
trachea = midline
tactile fremitus = decreased during attacks
percussion = resonant to hyper-resonant during attacks
breath sounds = often obscuring by wheezes during/surrounding attacks
adventitious sounds = wheezes during attacks
Pleural Effusion
fluid accumulation in the pleural space, separating air-filled lung from the chest wall, blocking the transmission of sound
trachea = shifted toward unaffected side with severe, large effusions only
tactile fremitus = decreased to absent over affected area
percussion = dull over fluid/affected area
breath sounds = decreased to absent over affected area
adventitious sounds = usually none, however friction rub possible over affected area
can be result of “third spacing”, pneumonia, cancer, etc
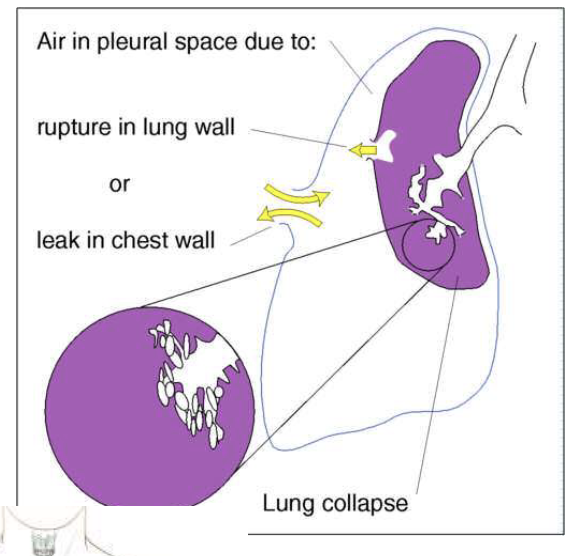
Pneumothorax
air leak into the pleural space, usually unilaterally, causing the lung to recoil from the chest wall. Pocket of air in the pleural space blocks the transmission of sound via stethoscope
trachea = shifted away from the involved side if excessive (tension pneumothorax)
tactile fremitus = decreased to absent over affected area
percussion = hyper-resonant over affected area
breath sounds = decreased to absent over affected area
adventitious sounds = none
usually accompanied by SOB/DOE and low O2 saturation
air leak into that airspace
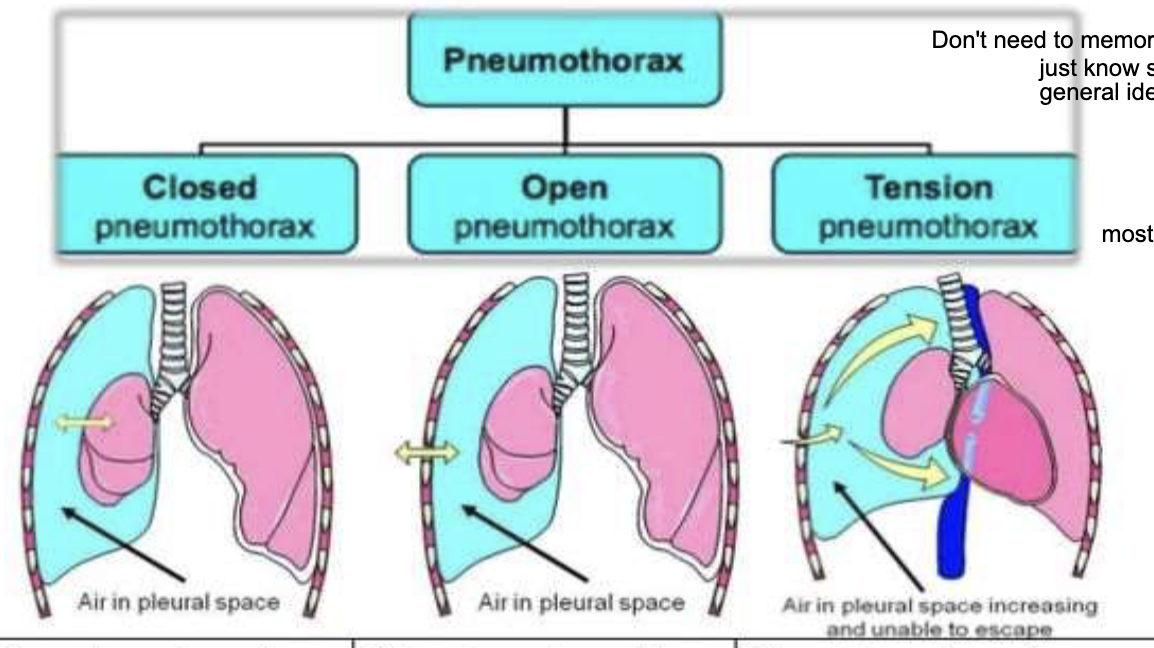
Types of pneumothorax
closed pneumothorax = least severity, pleural cavity pressure is < the atmospheric pressure
ex: collapsed lung, scuba diving, blunt trauma, smoking/inhaled drugs, various lung diseases
open pneumothorax = middle severity, pleural cavity pressure is equal to atmospheric pressure
traumatic pneumo, blunt or penetrating injury, invasive medical procedures
tension pneumothorax = most severity, pleural cavity pressure is > the atmospheric pressure
trauma causing one way valve
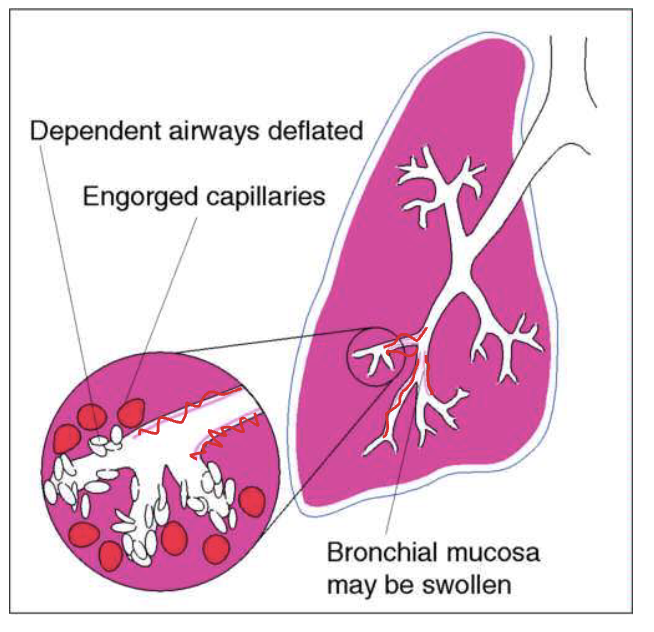
Pulmonary Edema (Congestive Heart Failure)
increased pressure in pulmonary vasculature due to fluid overload, causing congestion and interstitial edema around the alveoli and fluid may push into alveoli. Bronchial mucosa may also be edematous
trachea = midline
tactile fremitus = normal to decreased
percussion = resonant
breath sounds = vesicular
adventitious sounds = crackles in the dependent portions of lungs, possibly wheezes - fluid alveolar sacks with water
may be accompanies by JVD, lower extremity edema, hepatomegaly, DOE
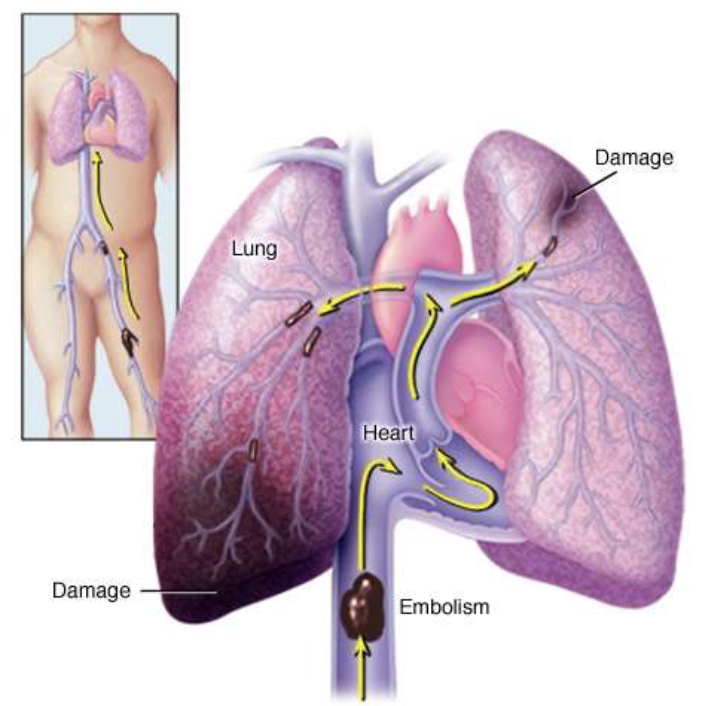
Pulmonary Embolism
blockage in the arteries bringing blood to the lung tissue (usually a clot), which leads to lung tissue damage
trachea = midline
tactile fremitus = normal
percussion = resonant
breath sounds = vesicular
adventitous sounds = usually none
may be accompanied by SOE/DOE, tachycardia, pain with inspiration, cardiac arrest
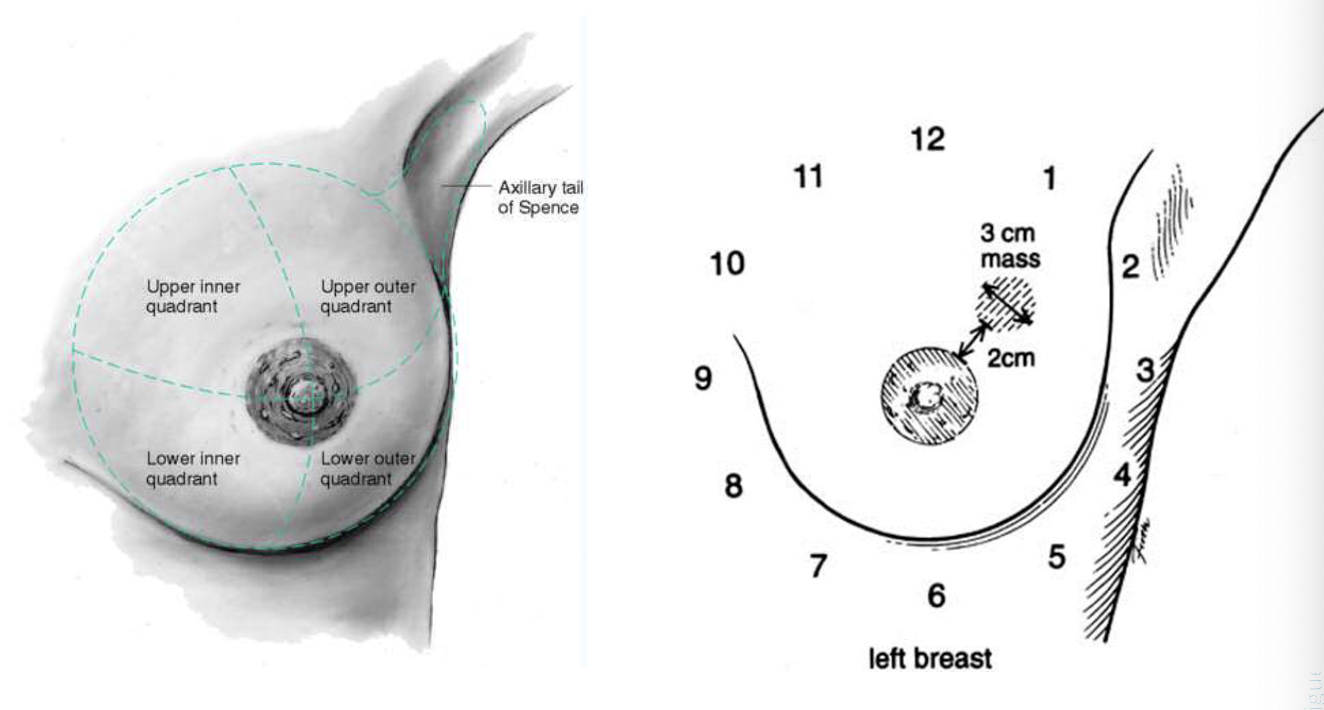
External anatomy of assigned female at birth (AFAB) Mammary Gland
The AFAB mammary tissue lies between 2nd and 6th ribs, between the sternal edge to mid axillary line.
The nipple is just below center
The superior lateral corner called Tail of Spence projects up and into axilla.
Developed mammary tissue is composed of
glandular tissue which is located into 15-20 lobes surrounding the nipple
fibrous bands of tissue including suspensory ligaments (Cooper’s), which support the glandular tissue
fat or adipose tissue throughout and predominates the mammary tissue
Clinical Points of References for breasts
Clock and Quadrants
upper inner quadrant
upper outer quadrant
lower inner quadrant
lower outer quadrant
axillary tail of Spence
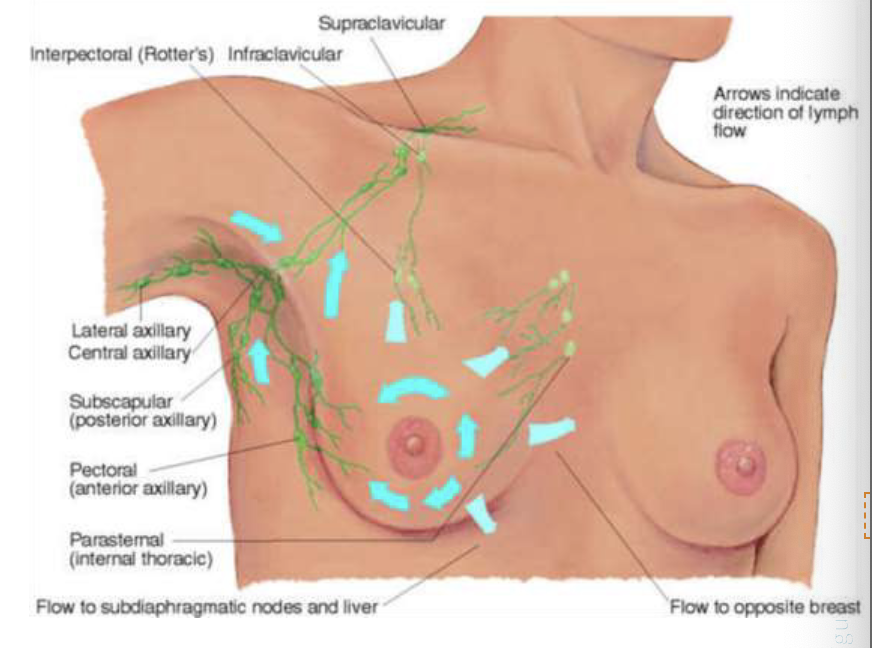
Lymphatics of breast
Axillary nodes
central axillary nodes
pectoral nodes
subscapular nodes
lateral axillary nodes
Drainage patterns
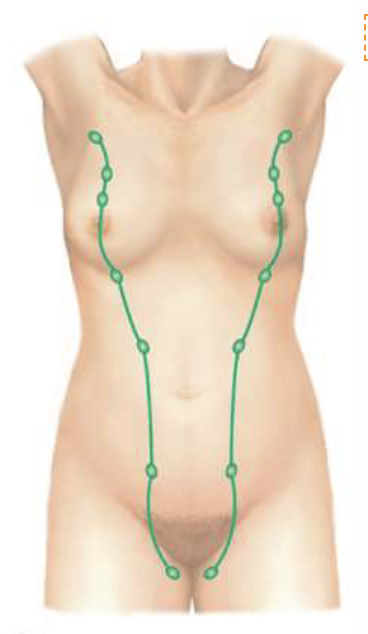
Supernumerary Breast or Nipple
extra nipples
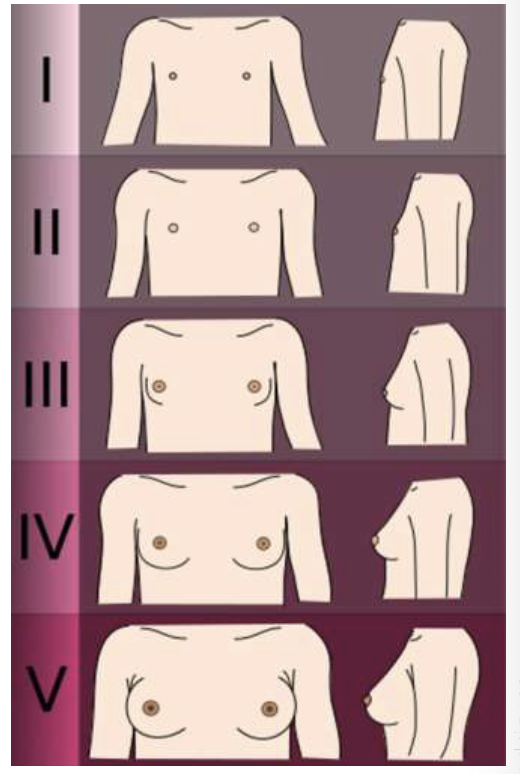
Tanner Stages
Stage 1: pre adolescent - elevation of nipple only
Stage 2: breast bud stage - elevation of breast and nipple as a small mound; enlargement of areolar diameter
Stage 3: further enlargement of elevation of breast and areola
Stage 4: projection of areola and nipple to form a secondary mound above the level of breast/chest
Stage 5: mature stage, projection of nipple only. Areola has receded to general contour of the breast/chest
AMAB Mammary Tissue
Rudimentary structure consisting of a thing disk of undeveloped tissue underlying the nipple
Areola is well developed, although the nipple is relatively very small
During adolescence, it is common for the breast tissue to temporarily enlarge, producing gynecomastia - usually unilateral and temporal
Gynecomastia (abnormally enlarged AMAB mammary tissue) may appear with aging due to testosterone deficiency
Most breast cancers in AMAB patient appear under the nipple
Breast PMH
personal history of breast disease/cancer
surgeries
family history of breast cancer
self-care behaviors
Breast ROS
pain
lump
nipple discharge
skin changes/rash
swelling
trauma
nippel inversion
Preparation for breast exam
position
draping (gown should be open in front, drape the side not being examined)
Small pillow
Ruler marked in centimeters or caliber
Inspect
Note size and symmetry (mild baseline asymmetry can be normal)
Note contour (masses, dimpling, flattening)
Note skin color, thickening, edema, venous pattern
Visible blue vascular pattern over bilateral breasts is normal finding during pregnancy. Unilateral, pronounced vasculature (esp in the absence of pregnancy) is abnormal
Inspect: Retraction Maneuvers
tissue should move symmetrically and hang freely without pulling, dimpling or retractions
patient bends down
Edema (Peu d’orange)
abnormal
can be a sign of inflammatory breast cancer
radiation can cause this as well, ask history
Retractions/Dimpling
abnormal
dimpling
retractions
these are both breast cancers and tumors

Inspection of Nipple
Note size, shape, direction in which they point (inversion present)
ask if inversion has always been like that
Note rashes, flaking, fissures or ulcerations
Note any obvious spontaneous discharge (is it clear, milky, purulent, blood)
if it’s unilateral and bloody, that’s a concern
bilateral clear or milky discharge can be normal
Possible Nipple Findings
Nipple retraction (can be normal OR abnormal)
Paget’s Disease (abnormal)
covered in eczema/scales

Inspect and Palpate Axillae
Note rash or skin changes signifying infection
Lift pts arm and support it yourself (use left hand to palpate right axilla)
Reach high into axilla and palpate in 4 directions
down mid axillary line, anterior axillary line, posterior axillary line, along inner aspect of upper arm
Note any palpable lymph nodes
tenderness?
ALWAYS investigate palpable lymph nodes!
Palpate Breasts
Best position is when tissue is flattened
A thorough exam should take 3 min/side
Use fingertips with light, medium and deep pressure
Bimanual palpation is helpful with large pendulous breast tissue
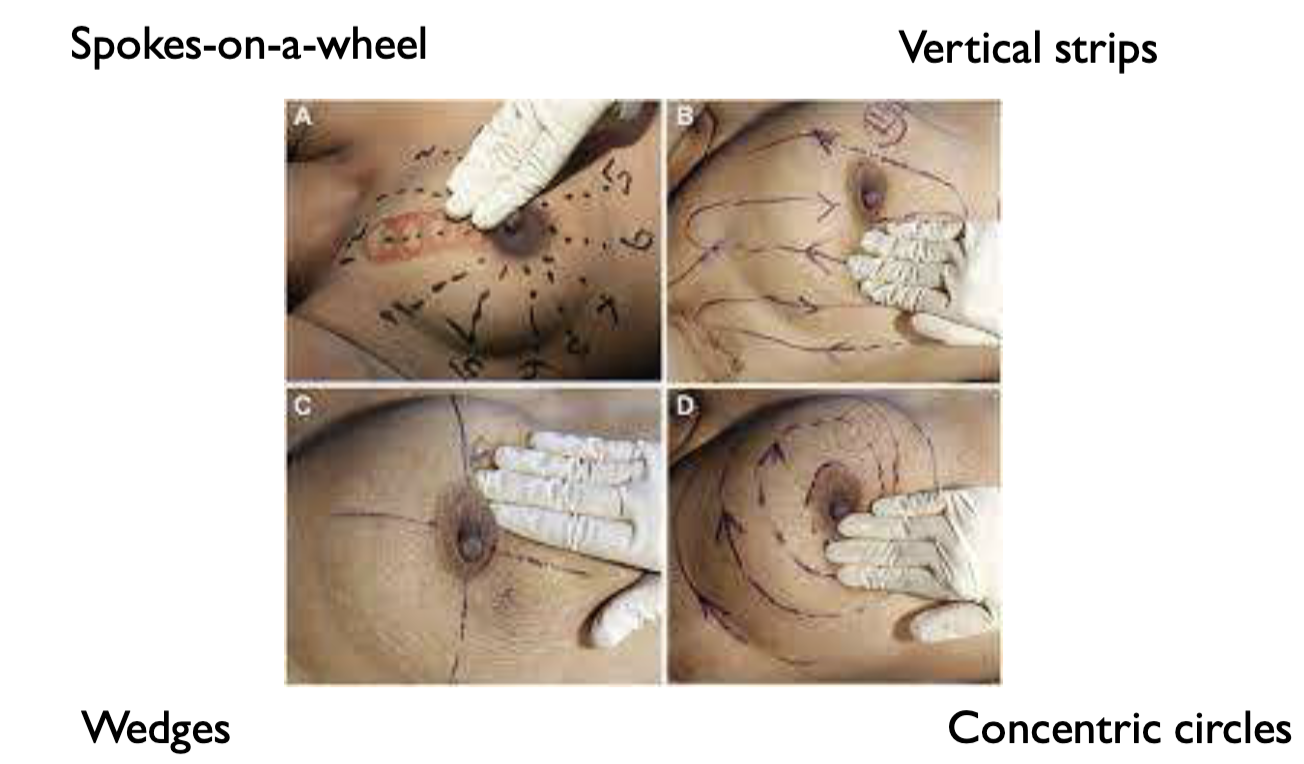
Pattern of Breast Palpation
Spokes on a wheel
Vertical strips
Wedges
Concentric circles
Breast Bimanual Palpation
specially helpful with large pendulous mammary tissue
also helpful to further characterize a lump if not felt well in the supine position

If any lumps are present, note:
Location - clock or quadrants (more specific the better)
Size - width x length x depth
Shape - oval, round, lobulated
Consistency - soft, firm, hard
Mobility - movable, fixed
Distinctness - solitary or multiple
Nipple - displaced or retraction
Overlying skin - erythema, dimpling, retraction
Tenderness
Lymphadenopathy
Palpate Nipple
if discharge is present, note color, quantity, and consistency
keep hands flat and down and inward
Discuss Breast/Chest Self Awareness
Recommendation of:
national comprehensive cancer network (NCCN)
Understand/Learn what your “normal” is so abnormalities can be detected
Changes to look for
a lump
nipple discharge other than milk, especially a bloody discharge
swelling
a range in size or shape
skin irritation, such as redness, thickening or dimpling of the skin
swollen lymph nodes in the armpit
nipple problems, such as pain or redness
Assessment of assigned male at birth (AMAB) mammary tissue
DO NOT OMIT (everyone gets a chest exam)
Inspect the chest wall noting skin surface and any lumps or swelling
Palpate the nipple - should feel even with no nodules
Typically has a flat disk of undeveloped tissue beneath the nipple
Gynecomastia = feels like a smooth firm/rubbery, movable disk beneath the nipple (unintentional swelling of the breast tissue)
occurs normally during puberty and may be unilateral or bilateral
can also occur in the aging population due to drops in testosterone
Most cancers will appear beneath or immediately around the nipple in biological males
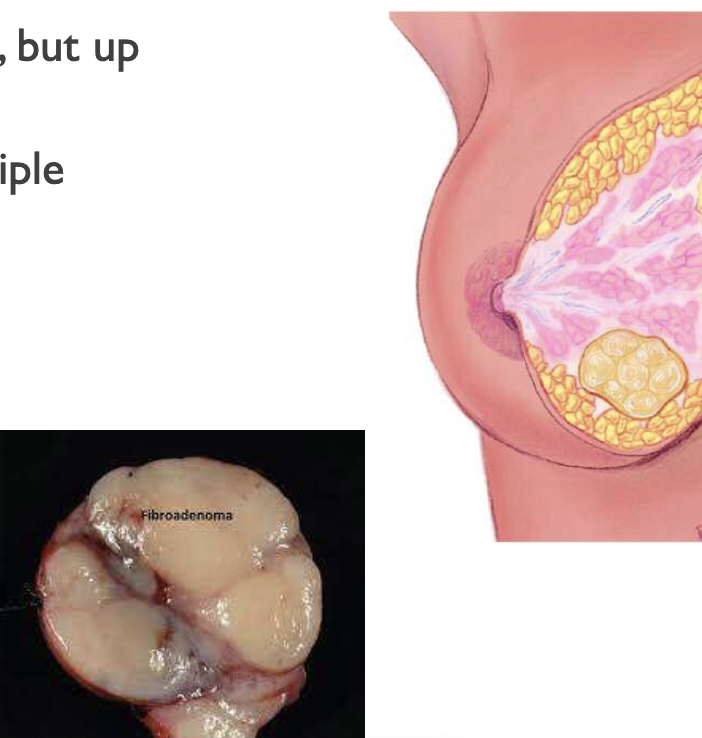
Fibroadenomas
benign finding
most commonly aged 15-25, but up to age 55
usually single, may be multiple
round, disclike, or lobular
may be soft, usually firm
well delineated
very mobile
usually nontender (some patients say it’s tender)
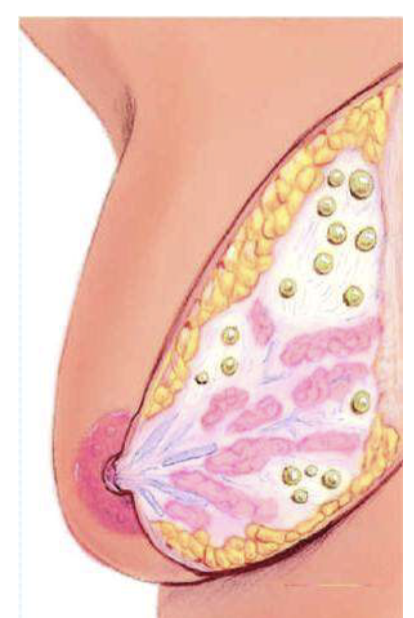
Fibrocystic Breast Disease
most common benign finding
thickening of generalized tissue with cyst formation (may be intermittent)
Age 30-50, regress after menopause except with estrogen therapy
Most common benign breast condition
Cysts are round, well delineated, soft to firm, and elastic feeling/bouncy
Cysts are mobile and often tender
On exam, overall nodular/dense feel
very painful before period
Mammary Carcinoma
AFAB:
most common over 50, however can be diagnosed at a very young age
most common area is upper outer quadrant
AMAB:
most common >60 years old
Most often found beneath or just around the nipple
Both:
usually single, although may coexist with other nodules
irregular or stellate
firm or hard
not clearly delineated form surrounding tissues
may be fixed to skin or underlying tissues
usually nontender
may have associative lymphadenopathy
if no lymph nodes involved then it’s not metastatic
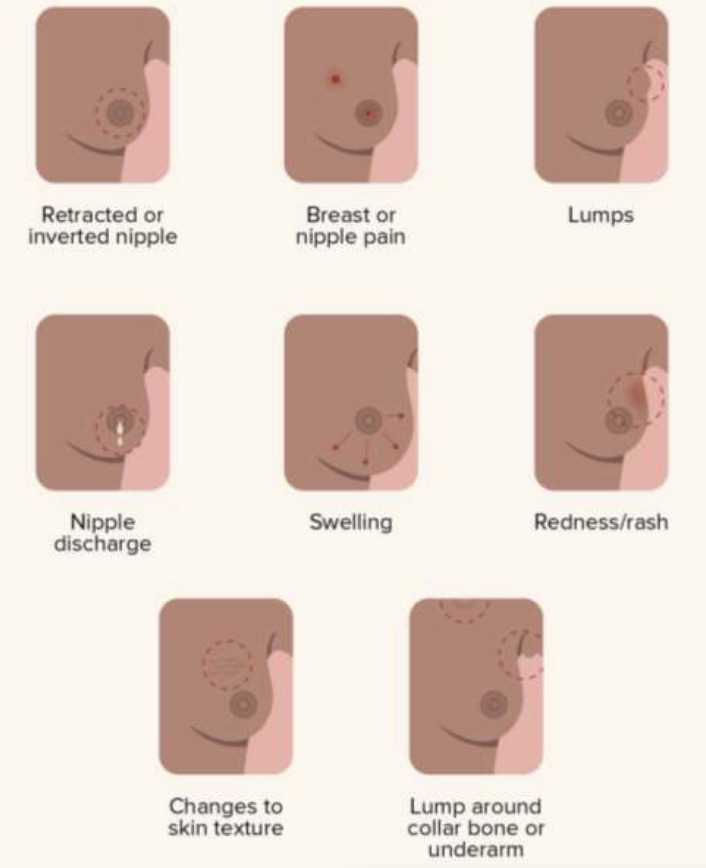
Possible signs of breast cancer
retracted or inverted nipple
breast or nipple pain
lumps
nipple discharge
swelling
redness/rash
charges to skin texture
lump around collar bone or underarm
AFAB cancer risk factors
Non modifiable risk factors:
Cisgender female > 50
Personal history of breast cancer
Mutation of BRCA I and BRCA 2 (among others)
First-degree relative with breast cancer
Previous breast/chest irradiation
Menarche < 12; menopause > 50
Modifiable risk factors:
Nulliparity or first child after 30
Use of combined HRT (esp in post menopausal setting)
Alcohol intake of 2+ drinks daily (but really any amount)
Physical inactivity
Post menopausal obesity
Never breast/chest feeding
AMAB cancer risk factors
age > 60
Family History of breast cancer
BRCA I or 2 mutation
Exposure to estrogen
hormone therapy for prostate cancer
gender affirming hormone therapy including estrogen/progesterone
Klinefelter’s syndrome
liver disease
obesity
disease/surgery of testicles
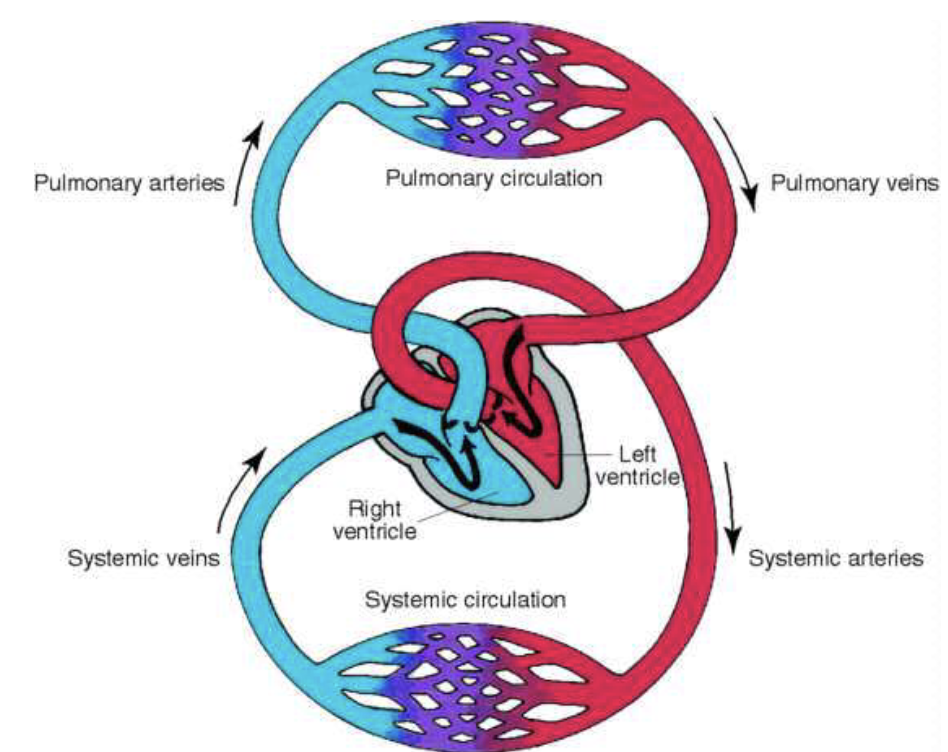
Pulmonary/Systemic Circulation
Internal Position/Surface Landmarks
precordium
mediastinum
2nd to 5th intercostal
Base vs apex
Apical impulse/PMI
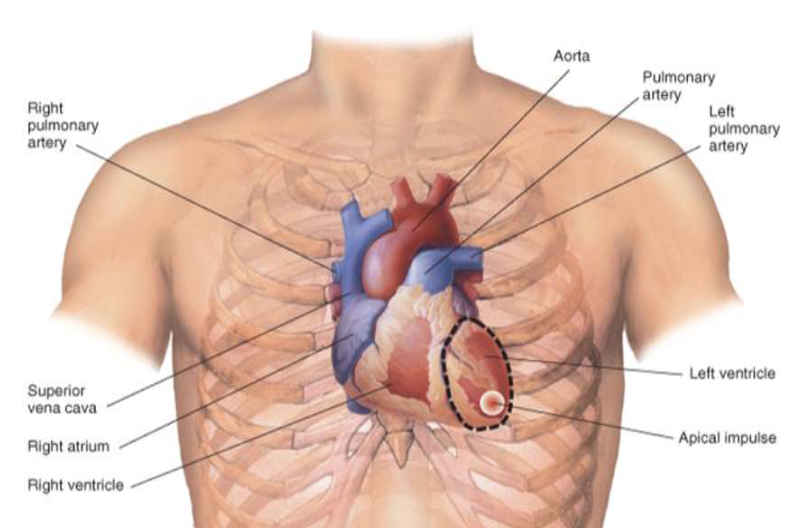
Great Vessels of the Heart

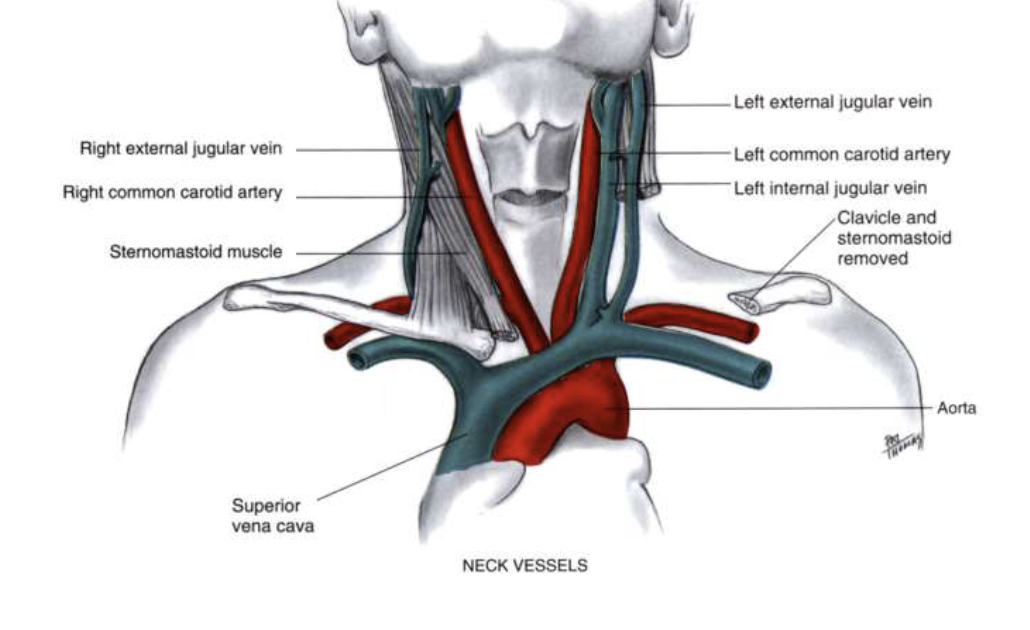
Neck Vessels
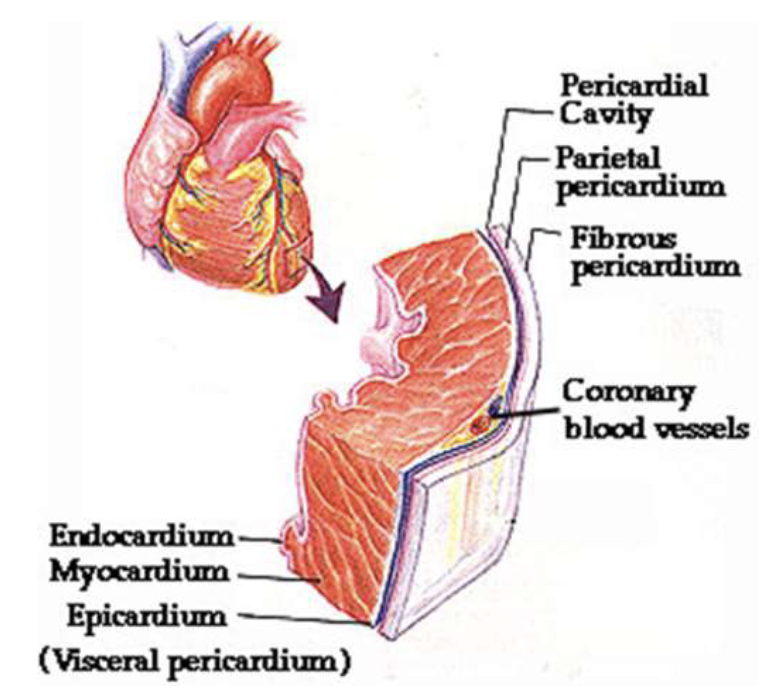
Layers of the heart
Internal Anatomy of Heart
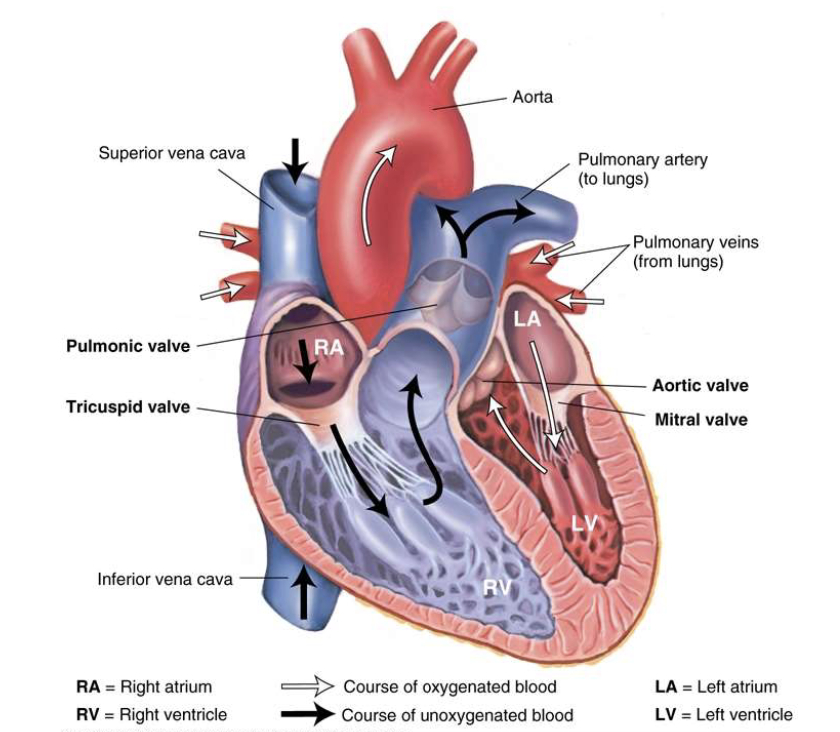
Heart as a pump
systole: SI - closing of AV valves - the ventricles contract
the right ventricle pumps blood into the pulmonary arteries (pulmonic valve is open)
the left ventricle pumps blood into the aorta (aortic valve is open)
diastole: S2 - closing of semilunar valves - the ventricles
blood flows from the right atrium → right ventricle (tricuspid valve is open)
blood flows from the left atrium → left ventricle (mitral valve is open)