Diseases of the Orbit
1/11
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
12 Terms
Orbital fracture
commonly from blunt trauma
Onset: 21-30yrs old
males > females
Orbital floor fractures make up 48% of all orbital fractures (near infraorbital canal) - energy displaces inferior from impact of greater sized object
Medial wall fractures make up 25.2% of all orbital fractures
Orbital Floor Fracture
Orbital floor fractures make up 48% of all orbital fractures (near infraorbital canal) - energy displaces inferior from impact of greater sized object
Symptoms: pain with eye movements, diplopia
Presentation:
Lid ecchymosis (bruising) and edema
Subcutaneous emphysema/crepitus: crackling sensation on palpation due to air in the subcutaneous tissue
Infraorbital nerve anesthesia: will involve the lower lid, cheek, side of the nose, upper lid, upper teeth and gum
Limited extraocular muscle motility: inferior rectus and inferior oblique will be involved
Can be the result of a hemorrhage or edema
Can be due to entrapment
Can be due to entrapment
Bone step off: present when the orbital rim is involved; A portion of the rim near the fracture will appear lower
Enophthalmos: posterior displacement of the globe (if severe)
proptosis
Other ocular findings: traumatic iritis, corneal abrasion, hyphema, increased intraocular pressure, lens subluxation or dislocation, retinal pathology
Work up: CT scan
Treatment
Nasal decongestants: individuals are advised to avoid blowing their nose for 14 days post injury
Systemic antibiotics
Systemic corticosteroids for severe edema
Surgical repair: done 2 weeks after initial trauma

Orbital Floor fracture Treatment
Nasal decongestants: individuals are advised to avoid blowing their nose for 14 days post injury
Systemic antibiotics
Systemic corticosteroids for severe edema
Surgical repair: done 2 weeks after initial trauma
Medial wall fractures
Medial wall fractures make up 25.2% of all orbital fractures
Typically associated with orbital floor fractures
Presentation:
Periorbital ecchymosis
Subcutaneous emphysema
Medial rectus entrapment will result in limited adduction and abduction
Cerebral spinal fluid rhinorrhea
Work up: CT scan
Treatment:
Nasal decongestants-individuals are advised to avoid blowing their nose for 14 days post injury
Systemic antibiotics
Systemic corticosteroids for severe edema
Surgical repair: done 2 weeks after initial trauma

Medial wall fracture Treatment
Nasal decongestants-individuals are advised to avoid blowing their nose for 14 days post injury
Systemic antibiotics
Systemic corticosteroids for severe edema
Surgical repair: done 2 weeks after initial trauma
Intraorbital foreign bodies
foreign body that occurs within the orbit but outside the globe
Occur after high velocity injury
BB gun pellet is the most common type of metallic intraorbital foreign body
Onset: younger individuals
males > females
Symptoms:
Decreased vision
Diplopia, pain
Presentation (depends on foreign body):
Orbital mass
Proptosis
Proptosis
Restricted extraocular muscle motility
Work up: determine if the globe is open or closed
MRI or CT scan
MRI is contraindicated with metallic foreign bodies
Treatment
Tentanus prophylaxis
Oral antibiotic (Consider anti-fungal medication if foreign body is organic)
Observation for small inert foreign bodies that are deeply embedded
Surgery (if large, inflamed, other ocular problems, composition that the body reacts to)
Intraorbital foreign body Treatment
Tentanus prophylaxis
Oral antibiotic (Consider anti-fungal medication if foreign body is organic)
Observation for small inert foreign bodies that are deeply embedded
Surgery (if large, inflamed, other ocular problems, composition that the body reacts to)
Intraocular foreign body
foreign body within the globe
Cause: typically caused by metal on metal tasks
Onset: 21-40 years old
males > females
Symptoms: dependent on the type of foreign body
Decrease vision, foreign body sensation, hyperemia, tearing, flashes or floaters
Presentation:
Scleral entry: conjunctival injection, chemosis, hemorrhage or laceration
Might lead to a deep anterior chamber d/t loss of aqueous from posterior chamber
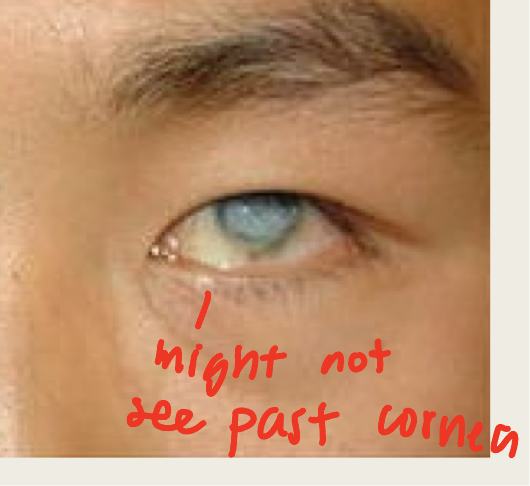
Corneal entry: corneal edema surrounding entry site or a positive Seidel sign
If the wound is self sealing a negative Seidel sign may be seen
Iris entry: iris transillumination and heterochromia may be seen
A peaked pupil may be present: the peak will point to the entry site
EOM restriction
Anterior chamber: focal area of corneal edema will be over the foreign body
Lens: focal lens opacities
Retina: most of the intraocular foreign bodies rest on the retina
Have worst prognosis
Complications:
Endophthalmitis, vitreous hemorrhage, retinal detachment, corneal scar, cataract, glaucoma and sympathetic ophthalmitis
Siderosis bulbi: caused by a retained intraocular foreign body that contains iron
Will occur as early as 18 days post traumatic event
Presentation: iris heterochromia, pupillary mydriasis, cataract formation, glaucoma & retinal pigmentation changes
Chalcosis: caused by retained intraocular foreign body that contains copper
must contain 85% copper
Presentation: chronic endophthalmitis, sunflower cataract, blue-green deposits on Descemet membrane, copper particles in the anterior chamber and reversible retinal toxicity
Work up: CT scan or MRI
Treatment:
Ideally foreign bodies are removed within 24 hours
Small inert foreign bodies may not be removed and observed
Systemic antibiotics (oral or intravenous-dependent on the foreign body)
Surgical removal
Intraocular foreign body Treatment
Ideally foreign bodies are removed within 24 hours
Small inert foreign bodies may not be removed and observed
Systemic antibiotics (oral or intravenous-dependent on the foreign body)
Surgical removal
Phthisis Bulbi
shrinkage and disorganization of the eye; functional loss of eye
Cause by: trauma, surgery, infection, inflammation, malignancy, retinal detachment or vascular lesion
Presentation: eye will have a square shape
Cornea will be thick and opaque, white
Sclera will be thickened
Iris neovascularization
Bad cataract
Retinal detachment
Treatment:
Cosmetic rehabilitation = fit w/ prosthetic shell
Pain management (meds depend on cause)
Dimensions of the Orbit
35mm high
45mm wide
40-45mm deep
Orbital myositis
Inflammation of 1+ of extraocular muscles
Idiopathic condition
Onset: third decade
Affects females more than males
Symptoms:
Orbital pain (can be moderate to severe) with eye movement
diplopia
Presentation: can be acute or chronic in nature
lid edema & ptosis
proptosis
chemosis
injection over the affected muscle
Restricted motility
With chronic cases, fibrosis and permanent restrictive myopathy can be seen
Work up: MRI or CT scan which will show enlargement of the extraocular muscles
Treatment: oral NSAIDs in mild cases with oral steroids for moderate to severe cases