lecture 2,3,4 - mucosal microbiomes and oral diseases
1/31
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
32 Terms
what are koch’s postulates
organism must be present in all cases of disease and absent in healthy
organism must be isolated from disease cases producing pure cultures
organism must cause disease in healthy individual when introduced
organism re-isolated from experimental host must be identical to original host
why are koch’s postulates not true for all?
pathobionts = opportunistic microorganisms/ non-infectious agent that can become pathogenic/virulent in the immunocompromised such as candida fungus = thrush
not know media to grow organism in so not always see, metagenomic sequencing find unexpected organisms
pathobionts disease in immunocompromised but not in healthy
not apply to polymicrobial conditions
why are Koch’s postulates not true for H. pylori causing peptic ulcer disease?
Pylori not present in non-steroidal anti-inflammatory ulcers (peptic ulcers) so doesn’t cause all peptic ulcers
Took culture of pylori, drank it and took H2 antagonists to stop acid production so not a normal healthy individual as normally produce acid as wanted to give pylori a chance to get established so research not conducted properly as koch's postulates not fulfilled
role of the mouth
Digestion
Intake of food
Mechanical breakdown – chewing (Hard tissues e.g. teeth)
Moistens and lubricates - saliva
Start of digestive process – salivary enzymes
Formation of bolus – mechanical processes - help swallow food
Respiration
Inlet to upper respiratory tract (mouth breathing)
Speech
Manipulation of sounds (air) - communication
what is the oral mucosa lined by?
stratified squamous epithelia (lining mucosa) - soft areas of mouth
what do the sites of the mouth involved in chewing (masticatory epithelia) have?
layer of keratin
on areas of tongue and top of teeth
what is the role of the gums?
gingiva (gums) overlies mandible and maxilla and helps support the teeth
what is the gingival crevice/ sulcus?
lined with non-keratinized epithelium (crevicular epithelium) that thins towards the base where it meets with the tooth
what happens at the base of the gingival sulcus?
epithelium transitions to an incompletely differentiated epithelium (junctional epithelium)
what is junctional epithelium?
highly permeable allowing constant passage of fluid (gingival crevicular fluid) and cells
what is a microbiome?
Ecological community of commensal, symbiotic and pathogenic microorganisms within a body space or other environment-
Lederberg & McCray 2001
how are microbiomes analysed?
DNA sequencing - bioinformatics
targeted microbiome analysis: sequence 16S rRNA gene for bacteria to identify what is present and its abundance
shot-gun metagenomics: sequencing all the DNA in a sample and using bioinformatics to predict the source/ function of the DNA sequences - what is present, abundance and what its role is
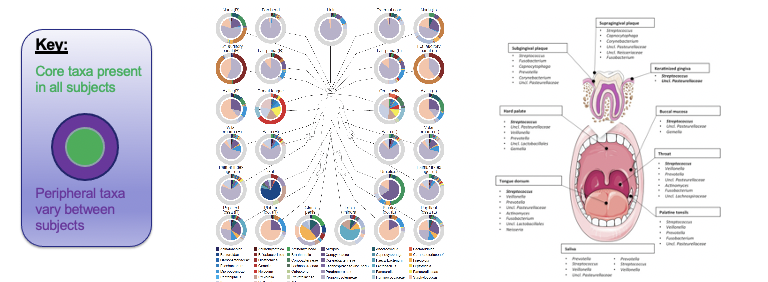
microbiome biogeography
what is dysbiosis?
Abnormality or imbalance of the microbial flora of the intestinal tract or other part of the body, especially when considered as a causative or contributory factor in disease
change in microbiota from healthy to disease state
Dysbiosis typically features one or more of what non-mutually exclusive characteristics:
bloom of pathobionts
loss of commensals
loss of diversity
what are pathobionts?
commensals that have the potential to cause pathology
typically present at low abundance but proliferate when changes in the environment occur (opportunistic pathogens)
why does dysbiosis result in a loss of commensals?
their restoration has the potential to reverse dysbiosis
what are commensals?
normal residing members of the microbiota
why does dysbiosis result in a reduction in diversity?
Diversity is associated with metabolic health
low bacterial diversity is associated with a number of diseases
what are oral diseases associated with dysbiosis?
Periodontal (gum) disease
Dental Caries (tooth decay) - disease of hard tissues
Oral cancer - disease of soft tissues
Peri-implantitis
Mucosal diseases
Leukoplakia
Lichen Planus
what defines a healthy oral microbiome? why not sure?
Large differences in healthy individuals
Genetic
Environmental
Lifestyle
Differences in study parameters
Experimental design
Bioinformatics analysis approaches
Lack of large scale studies
30 million people genome sequences v 10,000 publicly available microbiome data sets
The oral cavity has a distinct biogeography (i.e. the microbiome varies from site to site)
The expanded human oral microbiome database (eHOMD)
what is periodontal disease?
destructive inflammatory disease driven by dysbiosis of the oral microbiota
what is the non-specific plaque hypothesis?
what is the specific plaque/ microbial shift hypothesis?
what is the ecological plaque hypothesis?
what is the keystone pathogen hypothesis?
what is the Polymicrobial synergy and dysbiosis (PSD) model of periodontal disease?
Periodontitis is initiated by a synergistic and dysbiotic microbiota, within which different members, or specific gene combinations thereof, fulfil distinct roles that converge to shape and stabilize a disease-provoking microbiota
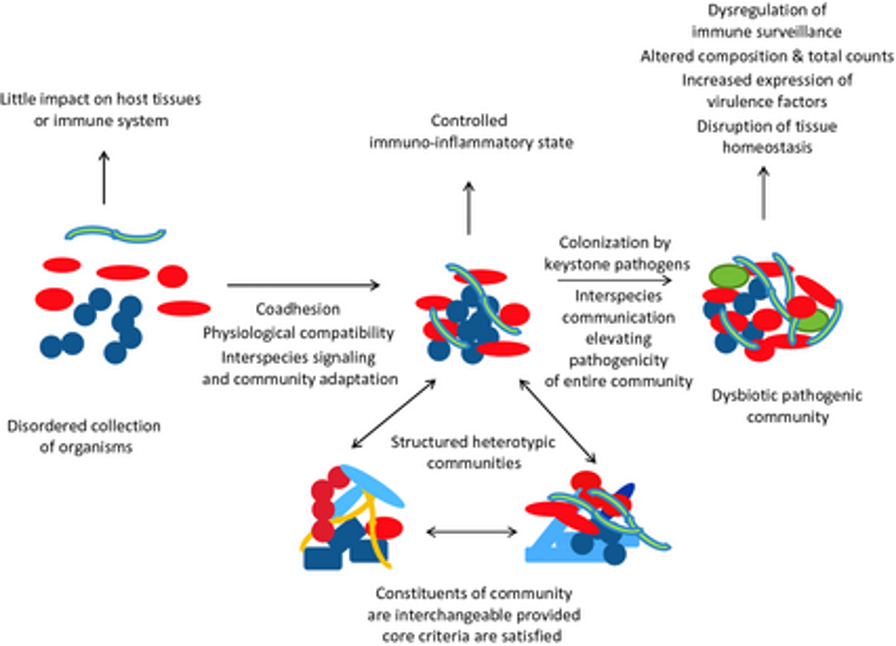
how does dysbiosis drive periodontal disease?
Immune response - not on or off, physiological levels of inflammation
what is osteoclastogenesis?
what is osteoblastogenesis?
what are dental caries?