Regional anatomy 10 -- the thorax 3
1/50
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
51 Terms
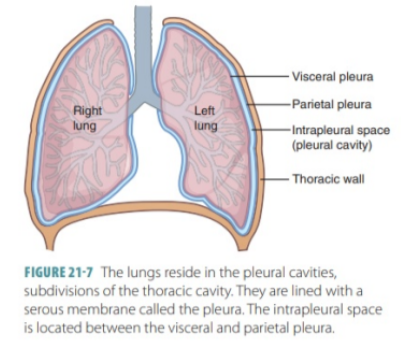
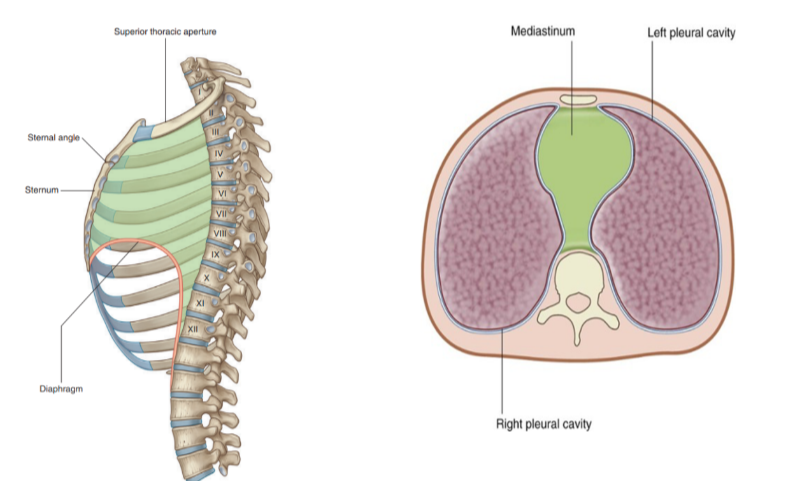
Pleural cavities
In the thorax we have 2 pleural cavities — each on either side of the mediastinum surrounding the lungs—
Superiorly — extend above rib I into the root of the neck
Inferiorly → Extend to a level just above the costal margin.
The medial wall of each pleural cavity is the mediastinum.
Each cavity is lined by a single layer of flat cells — the mesothelium — and an associated supporting connective tissue
Both layers form the actual “pleura”
Divided into 2 sections based on location —
Parietal pleura —
Outer section, associated with walls of the cavity
Visceral pleura —
Inner surface — adheres to and covers lungs
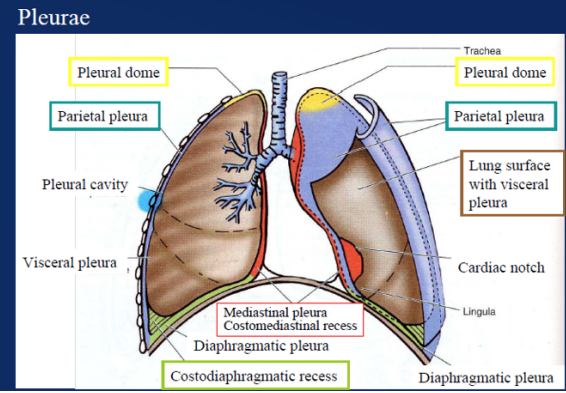
Pleural division based on location image
Parietal pleura —
Outer section, associated with walls of the cavity
Visceral pleura —
Inner surface — adheres to and covers lungs
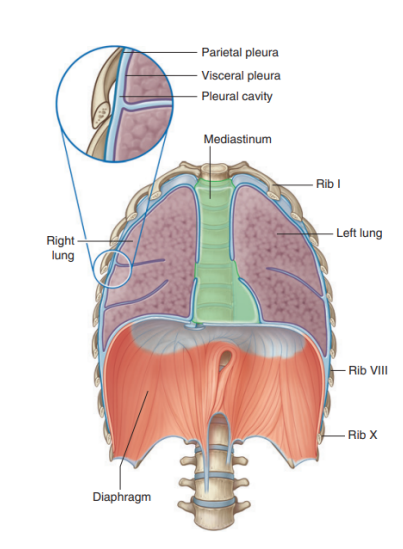
Specificities about the parietal pleura
Pleura related to the ribs and intercostal spaces — called costal part
Pleura covering the diaphragm — diaphragmatic part
Pleura covering the mediastinum — mediastinal part
Pleura lining the cervical extension of the pleural cavity — cervical pleura
(dome of pleura or pleural cupola)
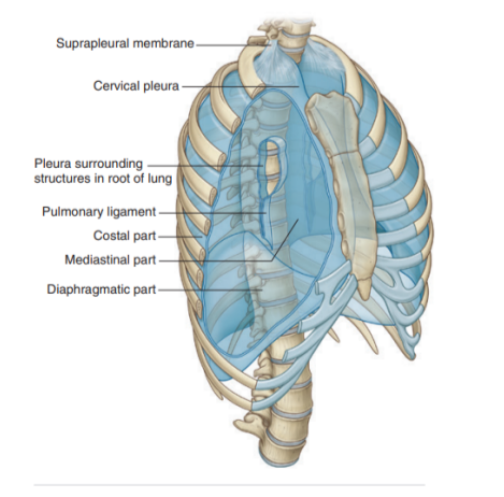
Suprapleural membrane
Covers superior surface of cervical pleural cavity
The connective tissue membrane is laterally attached to the medial margin of the first rib & behind to the transverse process of vertebra CVII
Receives fibers from the scalene muscles — functions to keep the membrane under tension
Supra pleural muscles provide apical support for the pleural cavity in the root of the neck
Lines of pleural reflection
Lines of pleural reflection —
Outline where parietal pleura abruptly change direction
As it passes from one wall of the pleural cavity to another
Superiorly —
Pleural cavity can project above the first costal cartilage but not above the neck of rib I
Due to inferior slope of rib I to its articulation with the manubrium
Anteriorly —
Pleural cavities approach each other posteriorly to the upper part of the sternum
Parietal pleura (posterior to lower sternum) doesn’t come to midline on the left the same way it does on the right
Due to presence of the middle mediastinum and its structures causing a bulging to the left
Inferiorly —
Costal pleura reflects onto the diaphragm above the costal margin
Also some vertical lines indicating extension of pleural cavity
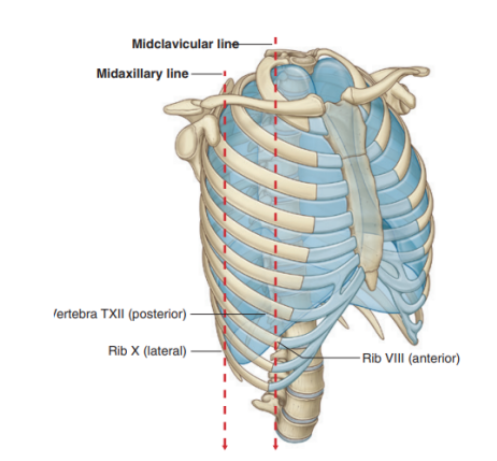
Vertical lines indicating extension of the pleural cavity
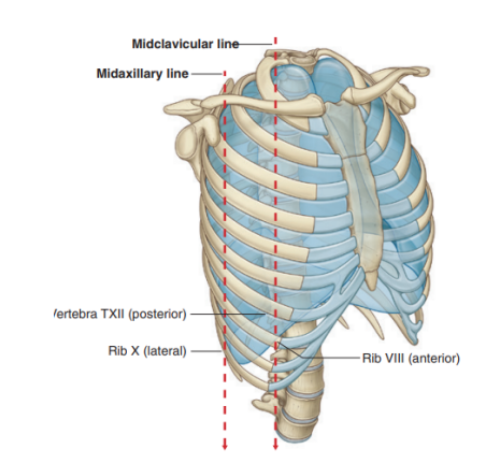
Midclavicular line —
Pleural cavity extends inferiorly from the clavicles to approximately rib VIII
Midaxillary line —
Extends to rib X
Inferior margin of the parietal pleura takes an oblique path laterally from the level of rib VII in the midclavicular line to rib X in the midaxillary line and the T12 vertebra at the vertebral columns
Visceral pleura —
In continuity with the parietal pleura at the hilum of each lung — where structures enter & leave the organ
Firmly attached to the lung surface, including both opposed surfaces of the fissures dividing the lungs into lobes
Although innervated by visceral afferent nerves that accompany bronchial vessels, pain is generally not elicited from this tissue
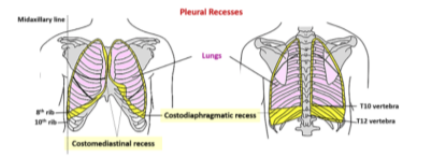
Pleural recesses
Two types of recesses —
The costodiaphragmatic recess
Also called costophrenic angles
Larger, located between the costal & diaphragmatic pleura of right & left pleural cavities
Occur at the costal reflection where the costal pleura becomes continuous with the diaphgramatic pleura
Deepest after broad expiration & shallowest after forced inspiration
The costomedisrinal recess
Smaller, anteriorly at the sternal reflection where the costal pleura is in contact with the mediastinal pleura
Larger on the left side due to cardiac notch of the left lung
Clinical drop — pleural effusion
Occurs when excess fluid accumulates within the pleural space
As the fluid accumulates within the pleural space the underlying lung is compromised and may collapse as the volume of fluid increases
The fluid will usually be aspirated to determine the cause, which could be —
Infections, malignancy, cardiac failure, hepatic disease, pulmonary embolism
A large pleural effusion needs to be drained to allow the collapsed part of the lung to reexpand and improve breathing
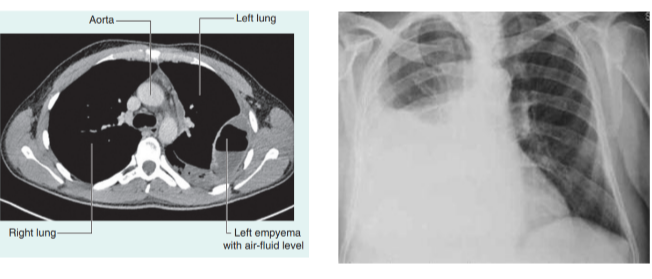
Clinical drop — pneumothroax
Presence of air in the pleural cavity
Increased air pressure could cause lung collapse
Could be due to —
Penetrating thoracic wound
Spontaneous rupture of pulmonary bulla (spontaneous pneumothorax)
Fractured rib
Anesthetist’s needle puncturing pleura during stellate ganglion block
Making a loin incision to expose kidney
To perform adrenalctomy or to drain a subphrenic abscess
Tension pneumothorax — condition where the ruptured tissues of thoracic wall form a valve permitting air to enter the pleural cavity upon inspiration but not allowing air to escape during expiration, thus increasing the pressure inside & pushing mediastinal structures to the opposite side
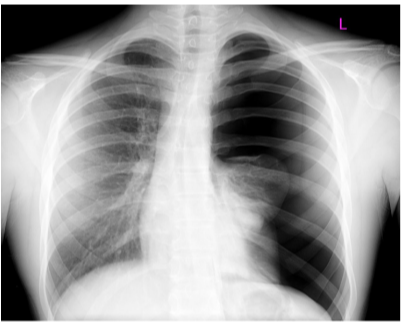
Lungs — general
Lie on either side of the mediastinum and surrounded by the pleural cavities
Air enters them via the main bronchi
Pulmonary arteries deliver deoxygenated blood to the lungs from the right ventricle, while oxygenated blood returns to the left atrium via the pulmonary veins
(contrary to “normal” functioning of veins & arteries).
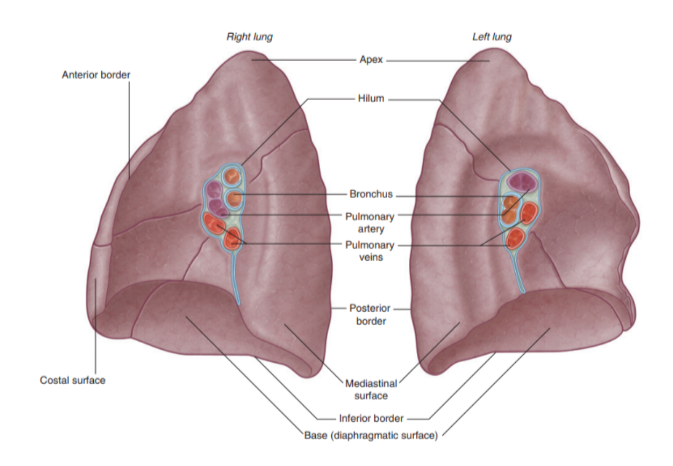
Landmarks recognizable in the lung
The base —
Situated on the diaphragm
The apex —
Projects above rib 1 & into root of neck
Costal surface —
Adjacent to ribs + Intercostal spaces
Mediastinal surface —
Lies against mediastinum anteriorly & vertebral column posteriorly — this surface contains the hilum
3 borders —
Inferior border —
Sharp, separates the base from the costal surface
Anterior border —
Sharp, separates costal surface from medial surface
Posterior border —
Smooth & rounded, separates costal surface from medial surface
We can also recognize certain indentations corresponding to surrounding structures
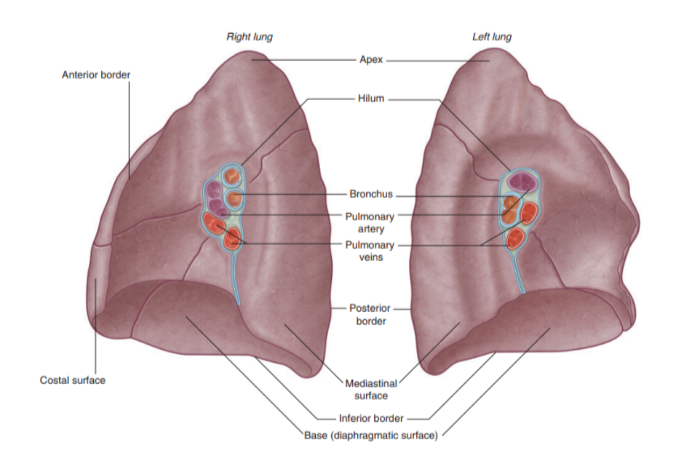
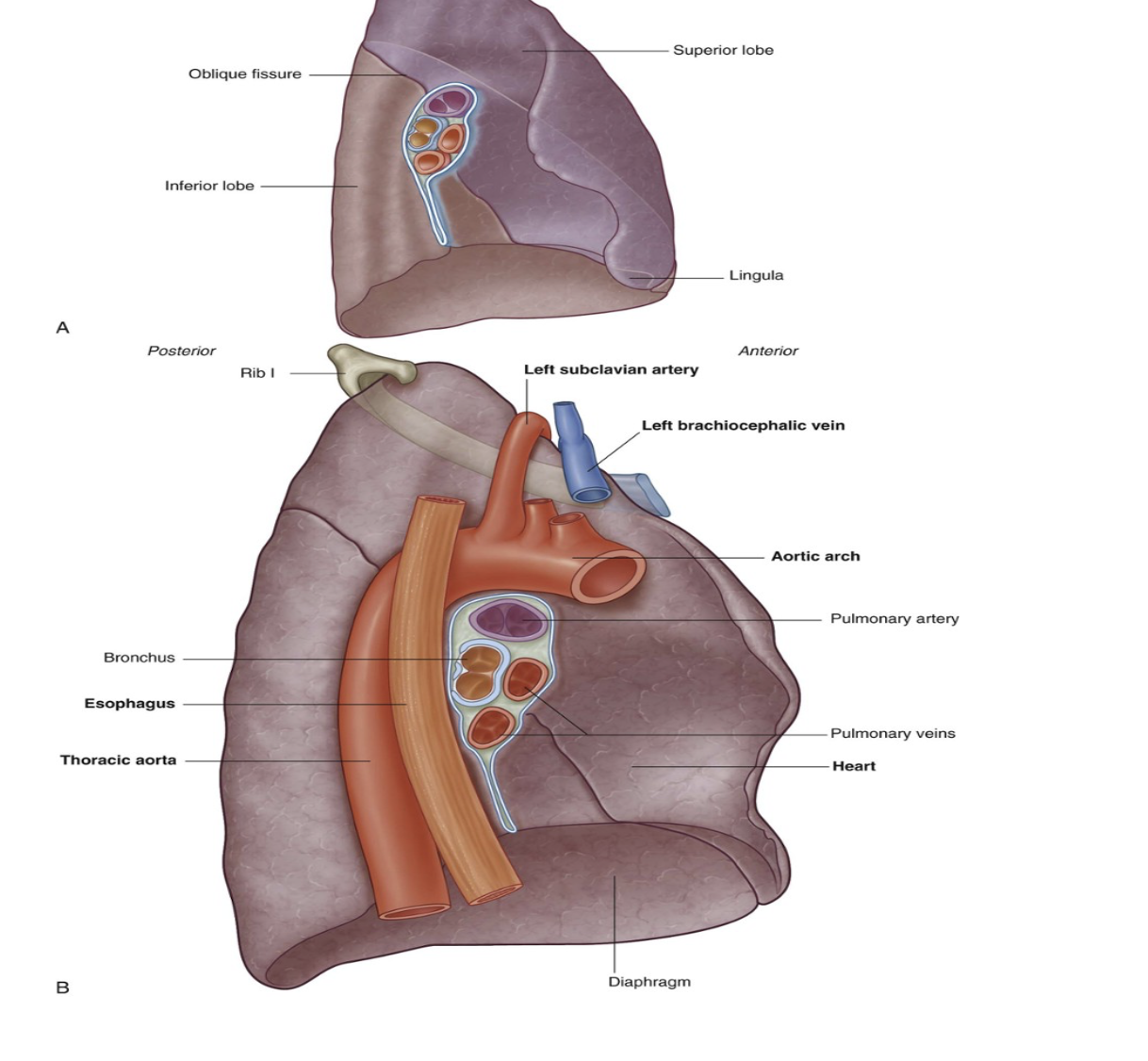
Root + hilum
The root —
A short tubular collection of structures attaching each lung to structures in the mediastinum
Covered in a sleeve of mediastinal pleura reflecting onto the lung surface as visceral pleura
Originates the pulmonary ligament — thin blade-like pleural fold projecting from the root towards the mediastinum, functioning to stabilize the position of the inferior lobe
The hilum —
The region outlined by this pleural reflection on the medial lung surface — where structures enter & leave
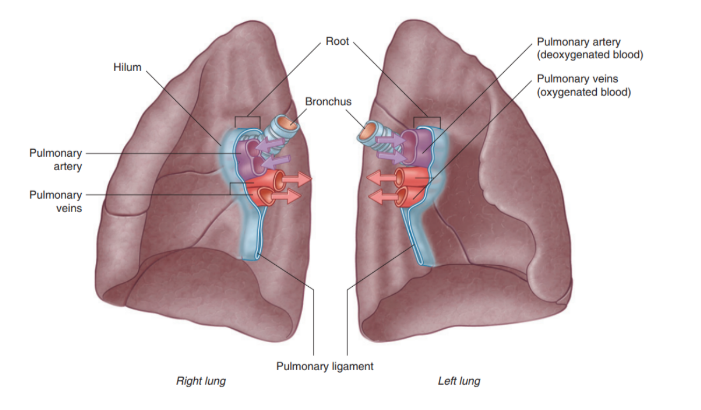
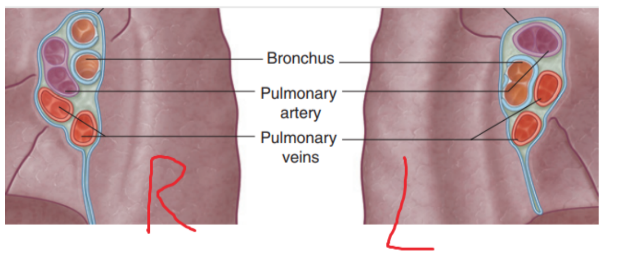
Structures we can find in each root & hilum —
Pulmonary artery
2 Pulmonary veins
Main bronchus
Bronchial vessels
Nerves
Lymphatics
The pulmonary artery is in most cases found at most superior portion of the hilum, while the pulmonary veins are inferior & the bronchi are posterior
On the side side however, the lobar bronchus to the superior lobe branches from the main bronchus in the root, unlike on the left where it branches in the lung itself superiorly to the pulmonary artery
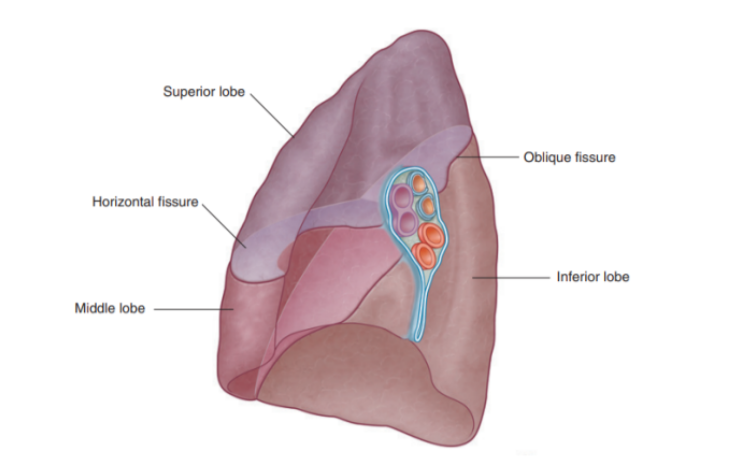
Fisssures of right lung
Has 2 fissures (formed by invaginations of the visceral pleura) —
Oblique fissure
Separates inferior lobe from superior & middle lobe
Horizontal fissure —
Separates superior lobe from middle lobe
Can be easily landmarked and correspond to specific ribs — important as they delimit zones of ascolatation
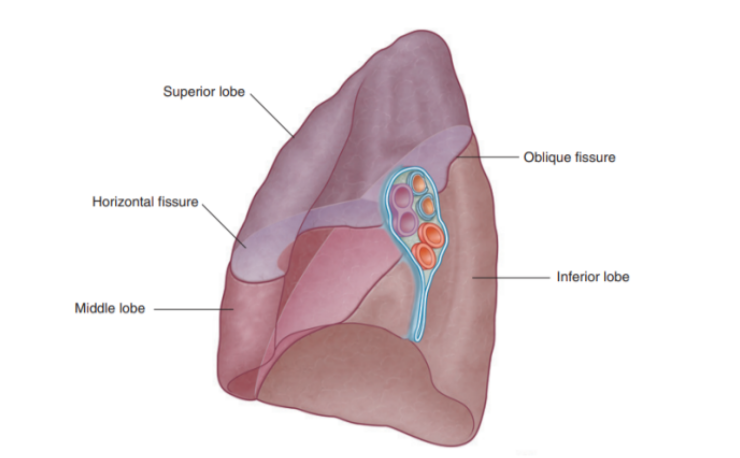
Lobes of right lung
Has 3 lobes — superior, middle, and inferior
Lobal attachment to surrounding mediastinal structures —
Superior lobe — in contact with the upper part of the anterolateral wall and the apex of this lobe projects into the root of the neck
Surface of the middle lobe — adjacent to lower anterior & lateral wall
Costal surface of inferior lobe — in contact with the posterior & inferior walls
Important structures in the mediastinum & root of neck that are adjacent to medial surface of right lung
Heart
Inferior & Superior vena cava
Azygos vein
Esophagus
Note about subclavian vessels & right lung
The right subclavian artery & vein arch over & are related to the superior lobe of the right lung as they pass. over the dome of the cervical pleura & into the axilla
Left lung lobes & fissure
2 — superior & inferior, with fissure separating them
Superior lobe —
In contact with upper part of anterolateral wall & apex of this lobe projects into the root of the neck contact
Costal surface of inferior lobe — in contact with posterior & inferior walls
Oblique fissure —
Separates superior & inferior lobe — slightly more oblique than that on right lung
Left lung is slightly smaller than right lung due to heart on left side (thus left lung has corresponding cardiac notch & additionally the associated lingula of the left lung which projects over the heart bulge
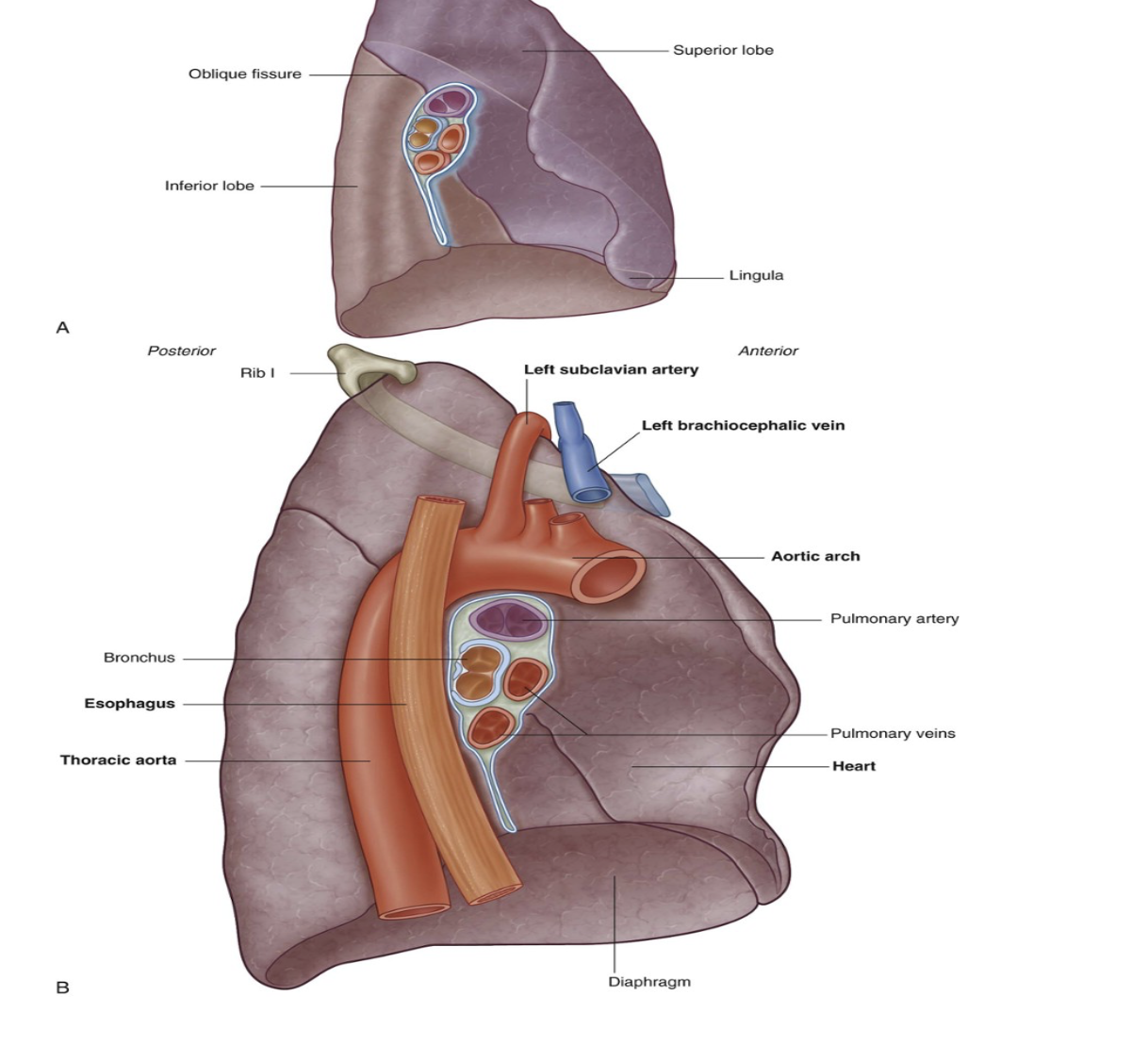
Important structures in the mediastinum & root of neck that are adjacent to medial surface of left lung
Heart
Aortic arch,
Thoracic aorta
Esophagus
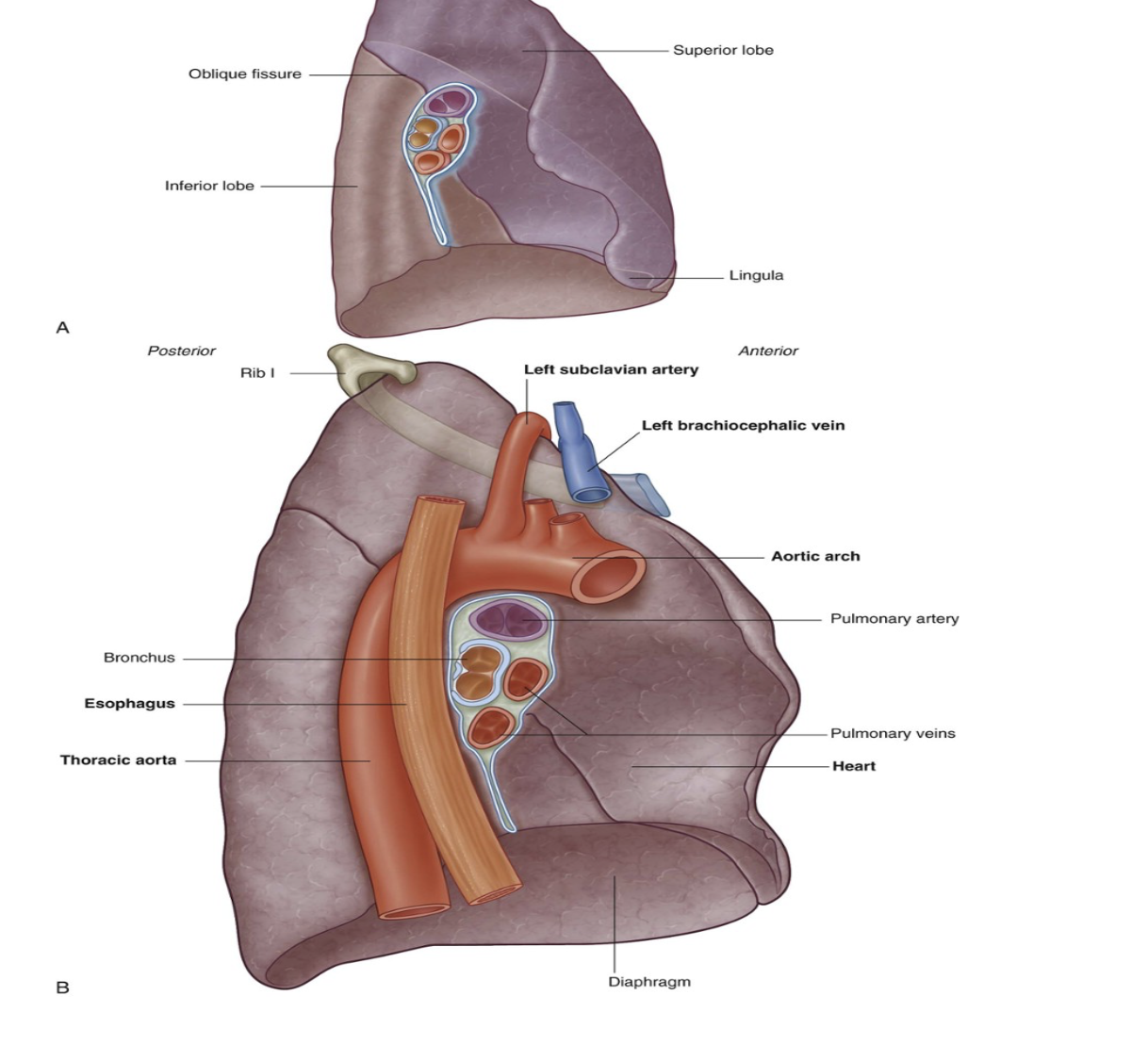
Note about subclavian vessels & left lung
The left subclavian artery and vein arch over and are related to the superior lobe of the left lung as they pass over the dome of the cervical pleura and into the axilla
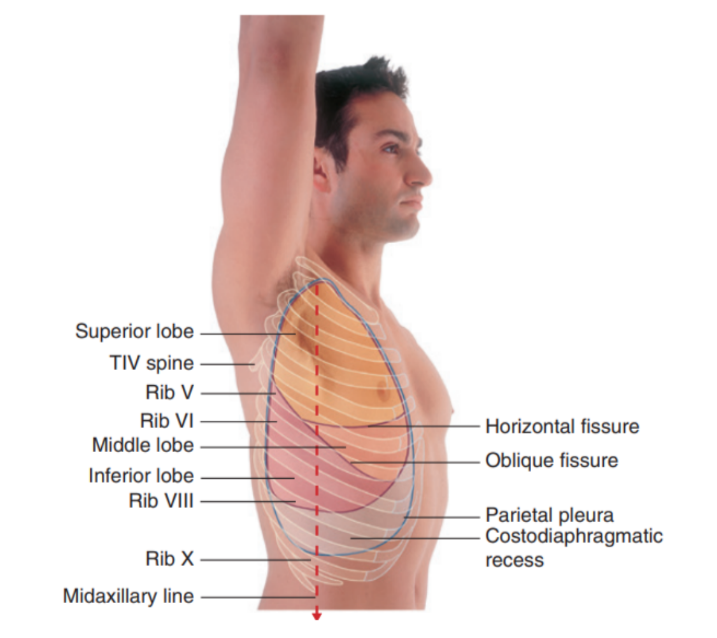
Surface anatomy relating to the fissures and lobes
Palpable surface landmarks —
Can be used to visualize the normal outlines of the pleural cavities & lungs & to determine the positions of the pulmonary lobes & fissures —ex.
Superiorly, we can see the parietal pleura projects above the first costal cartilage & anteriorly approaches the midline posterior to the sternum (uppermost section). Left parietal pleura doesn’t come close to the midline as much as the right lobe due to the heart bulging on the left side
Inferiorly, the pleura reflects on the diaphragm, above the costal margin & courses around the thoracic wall following an VIII, X, XII contour
(Ie. rib VIII in the midclavicular line, rib X in the midaxillary line, and vertebra TXII posteriorly)
Lungs don’t completely fill areas surrounded by pleural cavities — particularly anteriorly & inferiorly —
Costomediastinal recesses —
Occur anteriorly, particularly on the left side in relationship to the heart bulge
Costodiaphragmatic recesses —
Occur inferiorly between the lower lung margin & the lower margin of the pleural cavity
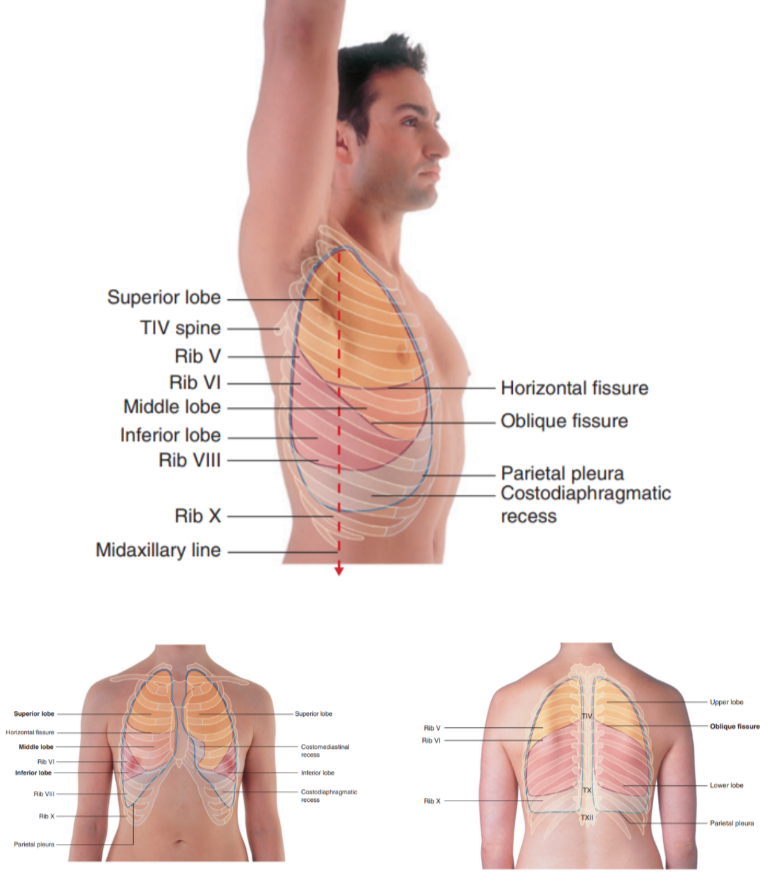
Margins of lungs related to ribs
Inferior lung margin —
Found at bottom of the thoracic wall, following a VI, VIII, X contour (ie. rib VI in the midclavicular line, rib VIII in the midaxillary line, and vertebra TX posteriorly)
Oblique fissure position —
Located in the midline, near the spine of vertebrae TIV, moves laterally downwards crossing fourth and fifth intercotal spaces and reaches VI laterally
Horizontal fissure(right side) —
Follows the contour of rib IV and its costal cartilage
Oblique fissures on both sides follow the contour of rib VI and its costal cartilage
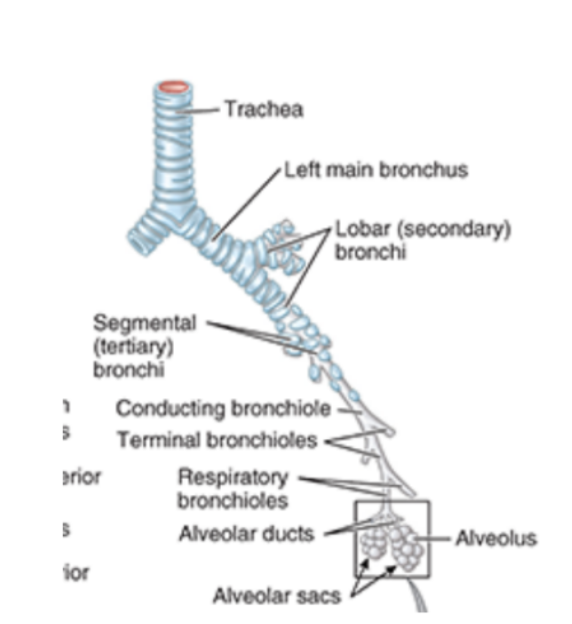
Bronchial tree —
Begins at level of larynx
Airway walls are supported by C-shaped rings of hyaline cartilage — trachea — flexible tube extending from vertebral level CVI in lower neck to vertebral level TIV/V in the mediastinum —
Here bifurcates into right & left main bronchus — can see the carina
In the lungs, the bronchi branch in a constant fashion to form branches of tracheobronchial tree
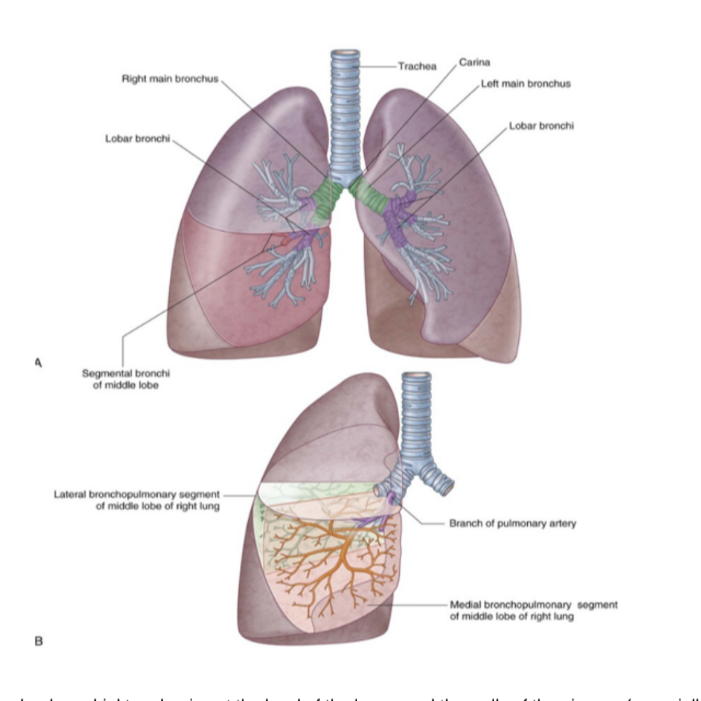
Branches of tracheobronchial tree
Each main bronchi divides into secondary bronchi
Each supplying a specific lobe of lung & dividing into several segmental bronchi to supply the segments
In each bronchopulmonary segment, the segmental bronchi give rise to multiple divisions — ultimately to bronchioles — which further subdivide & supply the respiratory surfaces
Bronchi walls are held open by discontinuous elongated plates of cartilage — not present in bronchioles
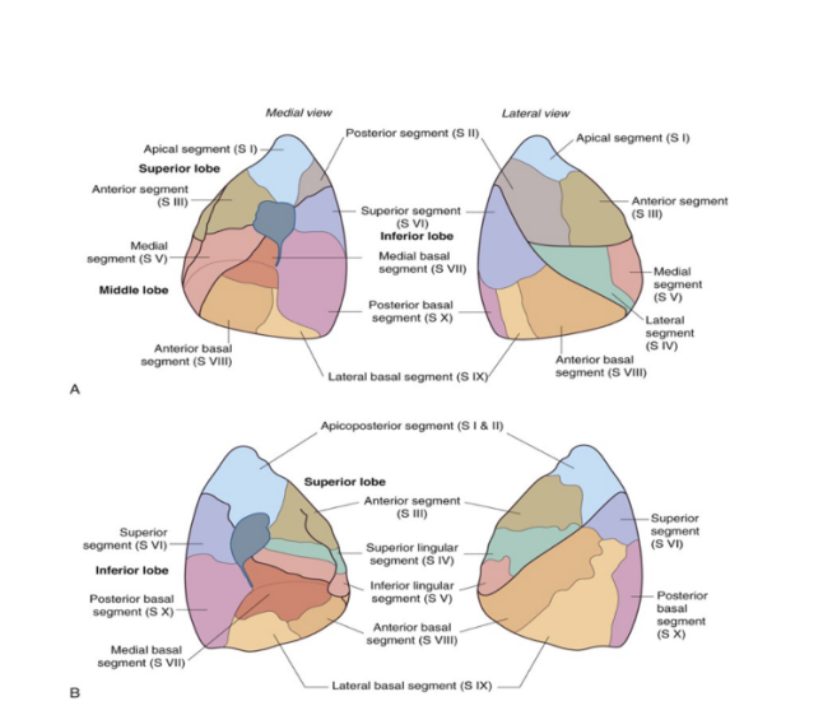
Lung/bronchopulmonary segments
Pyramidally shaped & are the largest subdivisions of a lobe with several important properties —
Apices face the lung root with their bases facing the pleural surface
Separated from adjacent segments by connective tissue septa
Supplied independently by a segmental bronchus & a tertiary branch of the pulmonary artery
Named according to segmental bronchi supplying them
Drained by intersegmental parts of the pulmonary veins lying in connective tissue between & drain adjacent segments
Can usually find 18-20 segments —
10 in right lung, 8-10 in left — dependent on combining of segments
Surgically resectable
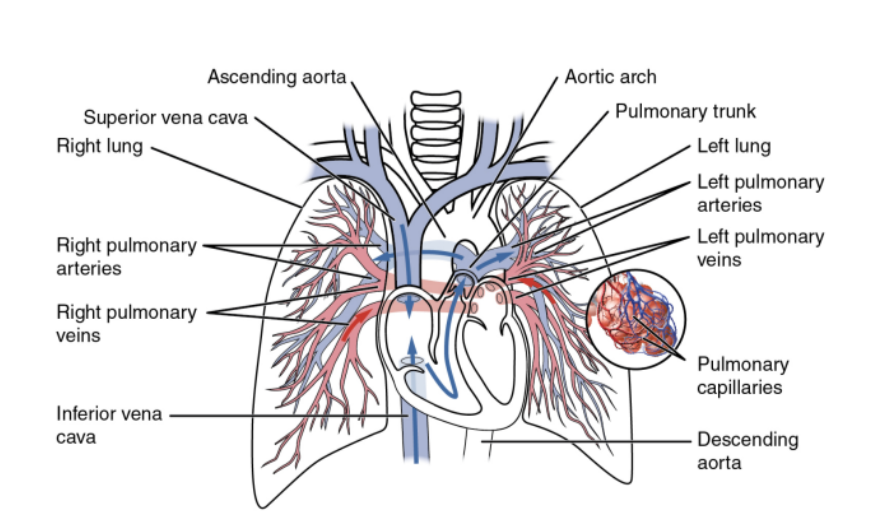
Overall vasculature of the lungs image
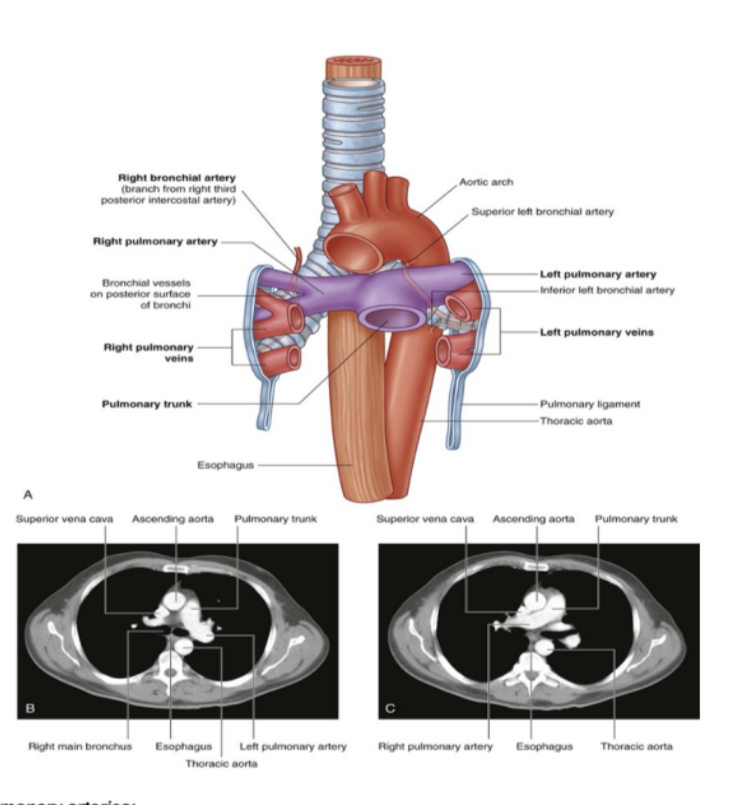
Pulmonary arteries (overall)
1 right, 1 left, originate from the pulmonary trunk & carry deoxygenated blood to the lungs from the right ventricle of the heart
Bifurcation of pulmonary trunk occurs to left of midline just inferior to vertebral level TIV/V, and anteroinferiorly to the left of the bifurcation of the trachea
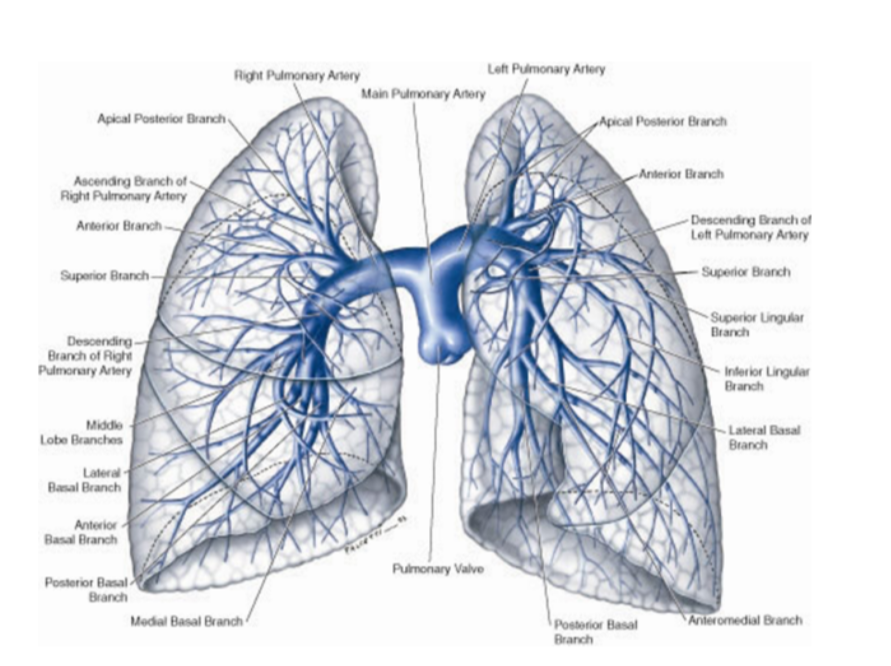
Right vs left pulmonary arteries
Right pulmonary artery —
Slightly longer than left
Crosses horizontally at the mediastinum passes anteriorly & inferiorly to the bifurcation of the trachea, & anteriorly to the right main bronchus — also posteriorly to the ascending aorta, superior vena cava, and upper right pulmonary vein
Enters into root of lung giving off a large branch to the superior lobe of the lung
Main branch continues through hilum to give off a second recurrent branch to superior lobe before dividing to supply both the midline & inferior lobes
Left pulmonary artery —
Shorter than the right, anterior to the descending aorta & posterior to the superior pulmonary vein
Pulmonary veins —
On both sides — superior & inferior pulmonary vein
Carry oxygenated blood from lungs back to heart
Begin at hilum, pass through root of lung, & immediately drain into left atrium
Pulmonary circulation —
The movement of blood from the heart to the lungs for oxygenation, then back to the heart again — steps —
Blood enters the right atrium of the heart through the superior & inferior vena cavae
The right atrium contracts, thus pushing the blood through the tricuspid valve into the right ventricle
The right ventricle contracts, pushing the blood through the pulmonary valve & into the pulmonary artery
The pulmonary artery carries the deoxygenated blood to the lungs
Where it picks up O2 & releases CO2 via gas exchange
The oxygenated blood then travels back to the heart through the pulmonary veins to enter the left atrium
The left atrium contracts, pushing blood through the mitral valve & into the left ventricle
Left ventricle contracts, pushing oxygenated blood through aortic valve & into aorta
Aorta distributed oxygenated blood to remainder of body, delivering O2 & nutrients to the organs & tissues
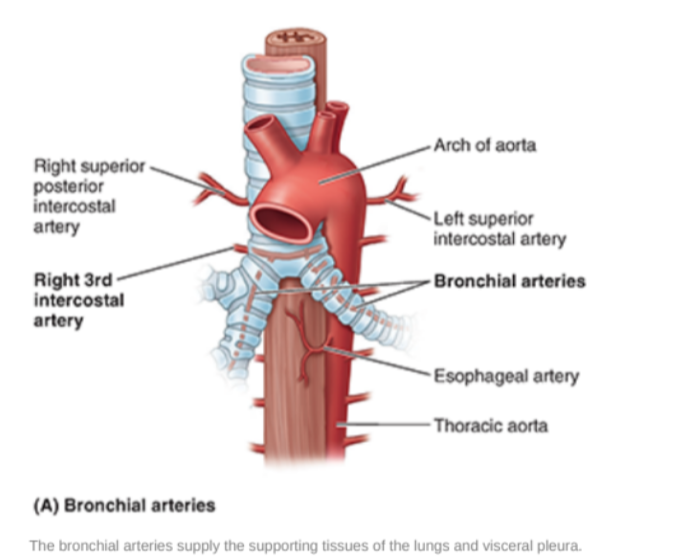
Bronchial arteries
Along. with the veins form part of the nutritive system of vasculature of the lungs
Interconnect within the lung with branches of the pulmonary arteries & veins
Originate from the thoracic aorta or one of its branches —
A singular right bronchial artery normally arises from the third posterior intercostal artery
Occasionally originates from upper left bronchial artery
2 left bronchial arteries directly arise from the anterior surface of the thoracic aorta —
Superior left bronchial artery arises — vertebral level TV
Inferior left bronchial artery arises inferior to left bronchus
They run on the posterior surfaces of the bronchi & ramify in the lungs to supply pulmonary tissues
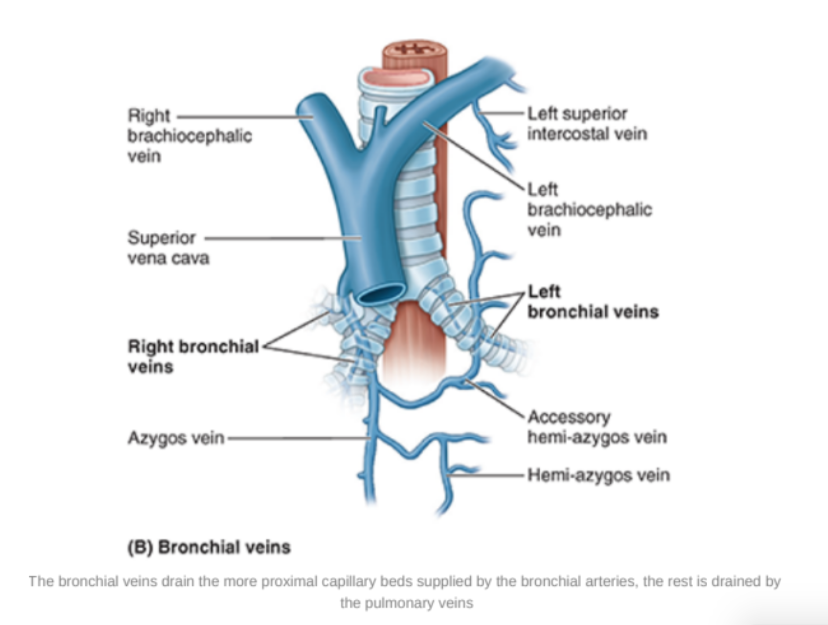
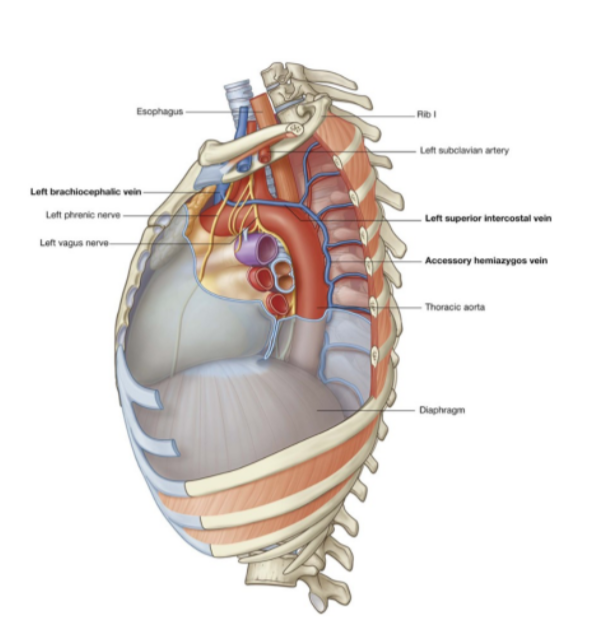
Bronchial veins —
Right bronchial vein drains into the azygos vein
Left bronchial vein drains into the accessory hemi-azygos or left superior intercostal vein
Bronchial veins also receive some blood from esophageal veins
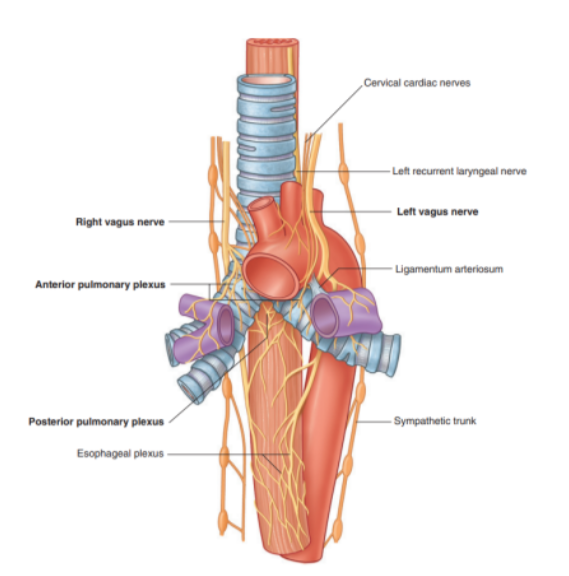
Innervation of the lungs
Nerves of lungs & visceral pleura are derived from the pulmonary plexuses anterior & (mainly) posterior to the roots of the lungs
These nerve networks contain parasympathetic, sympathetic, & visceral afferent fibers
These interconnected plexuses lie anteriorly & posteriorly to the tracheal bifurcation & main bronchi
The anterior plexus is much smaller than the posterior plexus
Branches of these plexuses, which ultimately originate from the sympathetic & vagus trunks, are distributed along branches of the airway & vessels
posterior from vagus, anterior from
The visceral efferents from the vagus system allow the constriction of the bronchiole, those from the sympathetic system dilate the bronchioles
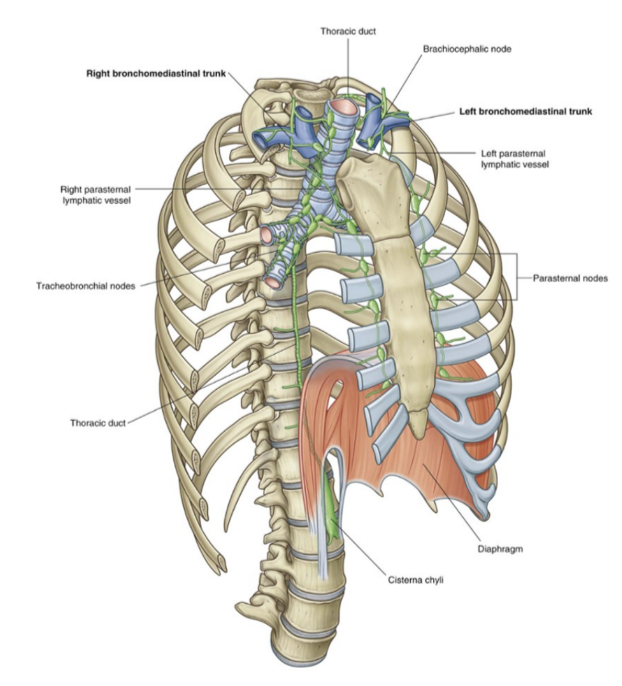
Lymphatic drainage
Venous lymphatics found in the lungs (superficial, subpleural, and deep) all drain into tracheobronchial nodes which are located around the roots of the lobar & main bronchi as well as the trachea (on the sides)
These lymph nodes extend from within the lung, through the hilum & root, and into the posterior mediastinum
Efferent vessels from these nodes — pass superiorly along trachea to unite with similar vessels originating from parasternal & brachiocephalic nodes
These ndes are found anteirorly to the veins of the same name in the superior mediastinum
This coming together of vessels causes formation of right & left bronchomedastinal trunks —
Directly drain into deep veins of the neck or into the right lymphatic trunk (or thoracic duct)
Mesiastinum
The central portion of the thoracic cavity that separates the pleural cavities
Extends from the sternum to the bodies o the vertebrae, and from the superior thoracic aperture to the diaphragm
Contains many structures — such as
Thymus, pericardial sac (& thus heart), trachea, and many major arteries & veins —
Also serves as a place of passage for many different structures
Subdivisions of the mediastinum
Divided into 2 smaller sections at the transverse plane, extending from the sternal angle to the intervertebral disc betwen TIV & TV
Splits into —
Superior mediastinum
Inferior mediastinum
Further partitioned into the anterior, middle, and posterior mediastinum by the pericardial sac
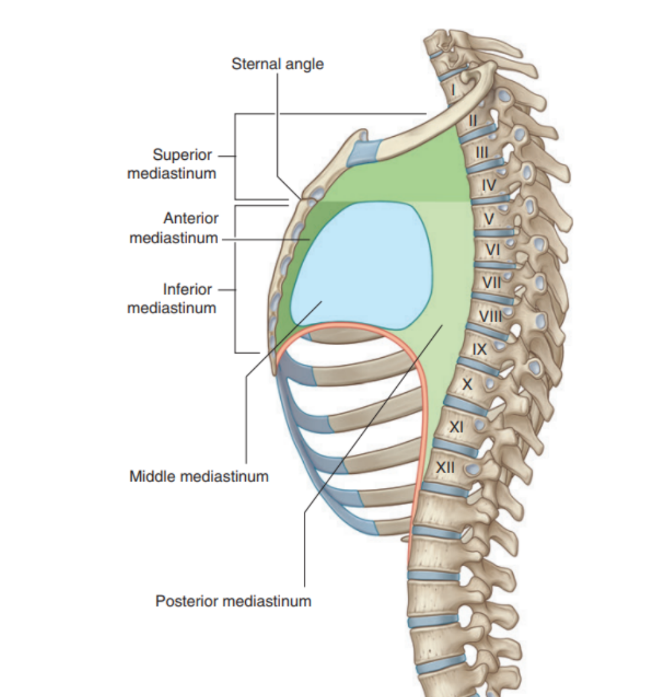
Superior mediastinum
Extends inferiorly from the superior thoracic aperture to the horizontal plane including sternal angle anteriorly & passes approximately through the IV disk of T$ & T% vertebrae posteriorly — often referred to as the transverse thoracic plane
Found posterior to the manubrium of the sternum & anterior to the bodies of the first 4 thoracic vertebraes
In continuation with the neck above & inferior mediastinum below
Major recognizable structures —
Thymus
Right & left brachiocephalic veins
Left superior intercostal vein
Superior vena cava
Arch of the aorta with its three large branches
Trachea
Esophagus
Phrenic nerves
Vagus nerves
Left recurrent laryngeal branch of the left vagus nerve
Thoracic duc
Other small nerves, blood vessels, and lymphatics
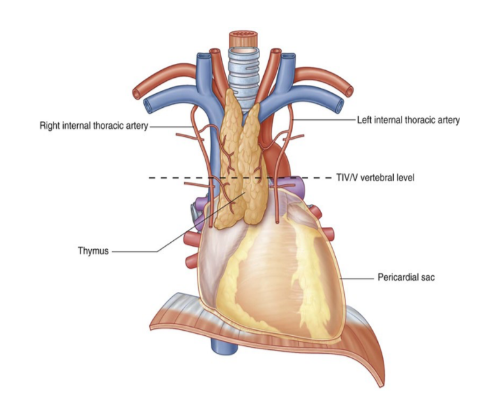
Thymus —
Most anterior component of the superior mediastinum, posterior to the manubrium
Bilobed asymmetrical organ
Upper extent of the thymus can reach into the neck as high as the thyroid gland, lower portion typically extends into anterior mediastinum over the pericardial sac
Begins to atrophy post-puberty
Arteries to the thymus —
Consist of small branches originating from the internal thoracic arteries
Venous drainage —
Usually into the left brachiocephalic vein & possibly into the internal thoracic veins
Right & left brachiocephalic veins
Located immediately posterior to the thymus
They form on each side at the junction between the internal jugular & subclavian veins
Left brachiocephalic vein crosses the midline & joins with the right brachiocephalic vein to form the superior vena cava
Right brachiocephalic vein begins posterior to the medial end of the right clavicle & vertically passes down
The left brachiocephalic vein begins posterior to the medial end of the left clavicle
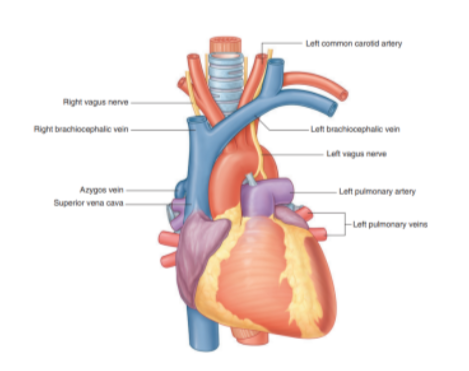
Left superior intercostal vein
Receives the second, third, & sometimes 4th posterior intercostal veins, usually the left bronchial veins, & sometimes the left pericardiacophrenic vein
Passes over the left side of the aortic arch, lateral to the left vagus nerve & medial to the left phrenic nerve, before entering the left brachiocephalic vein
Inferiorly may connect with the accessory hemiazygos vein (superior hemiazygos vein)
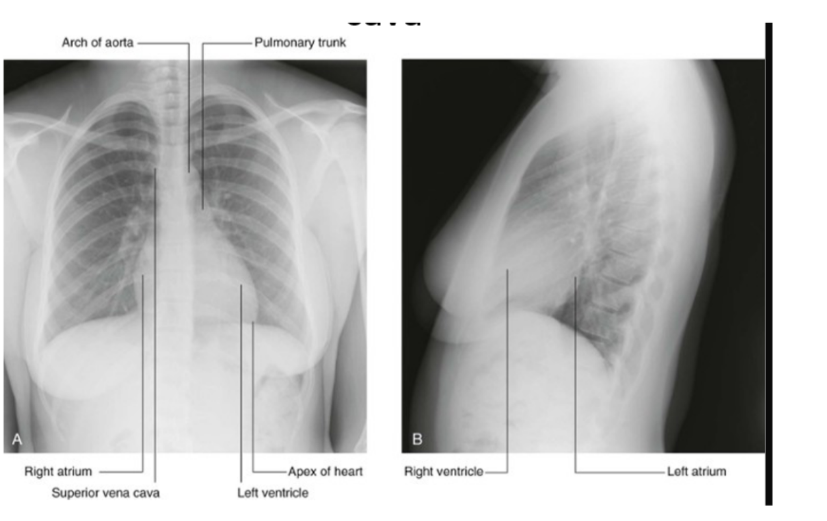
Superior vena cava
Begins posterior to the lower edge of the right first costal cartilage, where the right & left brachiocephalic veins join
Terminates at the lower edge of the right third costal cartilage, where it joins the right atrium
The lower half of it is within the pericardial sac (& thus in the middle mediastinum)
Superior vena cava receives the azygos vein immediately before entering the pericardial sac & may also receive pericardial & mediastinal veins
Can be easily visualized forming part of the right superolateral border of the mediastinum on a chest radiograph
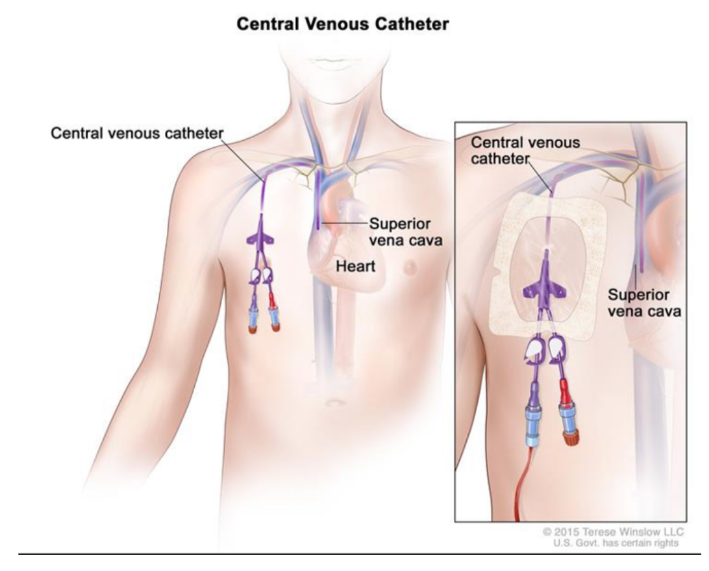
Clinical drop — venous access for lines/venous catheter
Large systematic veins are used to establish central venous access for administering large amounts of fluid, drugs, and blood
Most of these lines (small-bore tubes) are introduced through venous puncture into the axillary, subclavian, or internal jugular veins
The lines are then passed through the main veins of the superior mediastinum, with the tips of the lines usually residing in the distal portion of the superior vena cava or in the right atrium
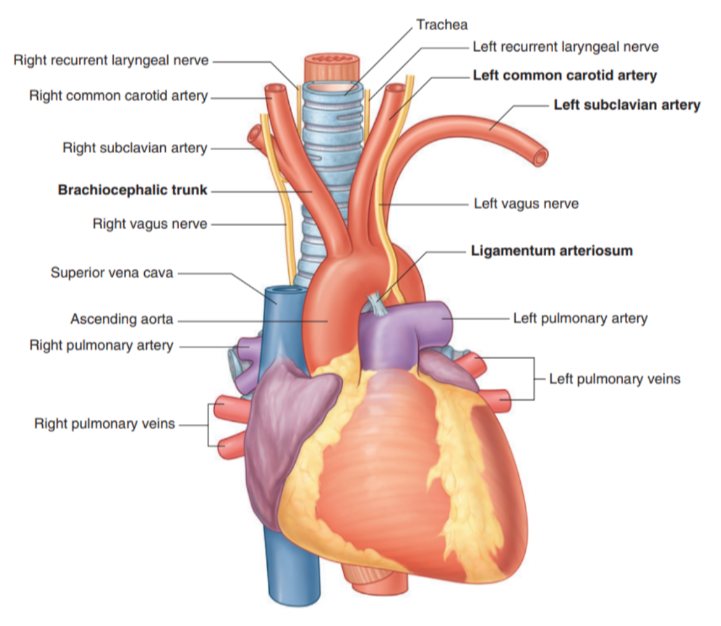
Arch of aorta
The thoracic portion of the aorta can be divided into the ascending aorta, arch of the aorta, & thoracic (descending) aorta —
Only the arch of the aorta is in the superior mediastinum
The arch extends as high as the midlevel of the sternal manubrium & is initially anterior, but later moves laterally to the trachea
From the arch we have 3 branches, each of which is crossed by the left brachiocephalic vein —
Brachiocephalic trunk
Left common carotid artery
Left subclavian artery
In this region we can also recognize the ligamentum arteriosus which is formed from the embryological structure known as the ductus arteriosus.
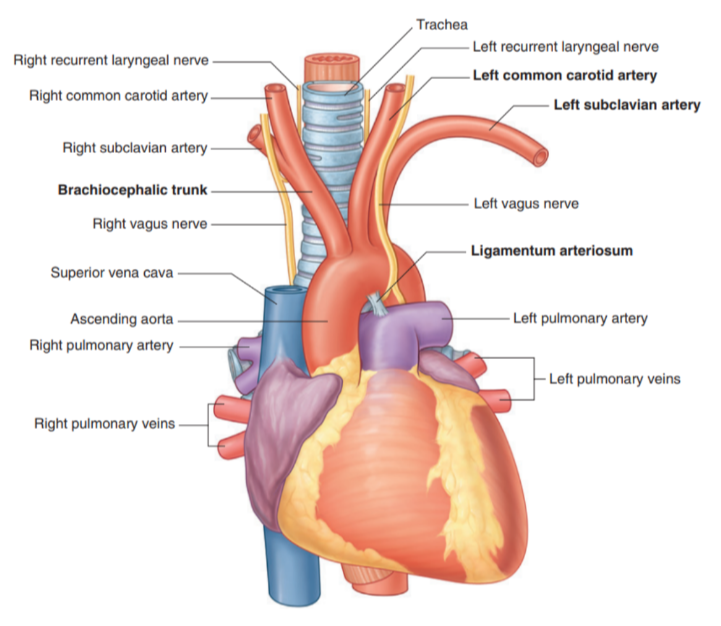
Branches of arch of aorta
Brachiocephalic trunk —
Largest of the three branches
Originates from behind the manubrium — slightly more anterior than the other branches
At the upper edge of the right sternoclavicular joint divides into —
Right common carotid — supplies right side of head
Right subclavian artery — supplies right upper limb
In some cases may have another branch for the supply of the thymus
Thyroid Ima Artery
Left common carotid artery:
Arises from the arch immediately to the left and slightly posterior to the brachiocephalic trunk
Ascends through the superior mediastinum along the left side of the trachea
Supplies the left side of the head and neck.
Left subclavian artery:
Arises from the arch of the aorta immediately to the left of, and slightly posterior to the left common carotid artery
Ascends through the superior mediastinum along the left side of the trachea
The major blood supply to the left upper limb.
Branches of the thoracic aorta table

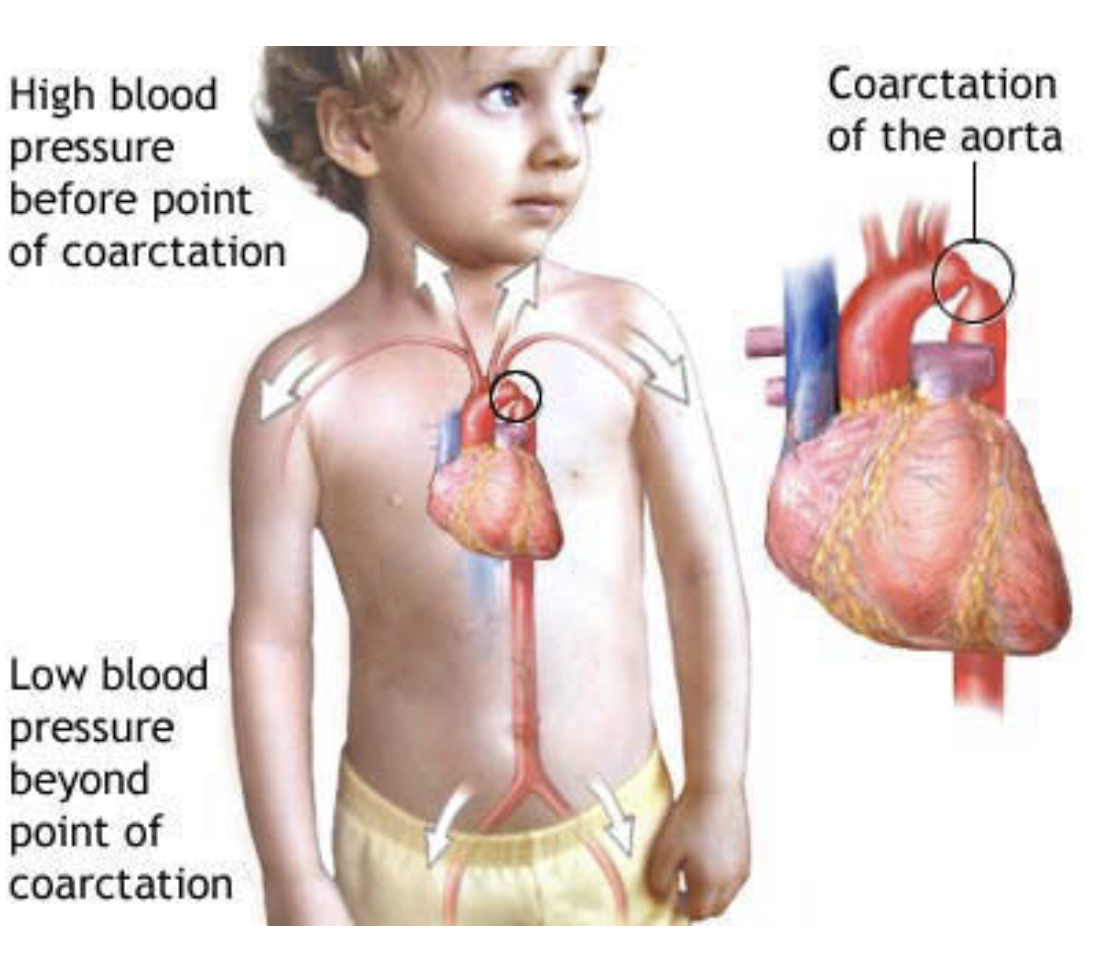
Clinical drop — coarctation of the aorta
A congenital abnormality where the aortic lumen is constricted just distal to the origin of the left subclavian artery
At this point the aorta becomes significantly narrowed & the blood supply to the abdomen & lower limbs is diminished
Collateral vessels may develop around the chest wall & abdomen to supply the lower body
These intercostal veins which form a bypass to supply the descending thoracic aorta may lead to erosions of the inferior margins of the ribs — can be observed in radiographs as inferior rib notching
This coarctation also affects the heart, which has to pump the blood at a higher pressure to maintain peripheral perfusion — may produce cardiac failure
Trachea & esophagus
Trachea —
Midline structure palpable in the jugular notch as it enters the superior mediastinum
Divides into right & left main bronchi just inferior to the transverse plane between sternal angle & vertebral level TIV/V — also where the esophagus continues into the posterior mediastinum
Esophagus —
Posterior to the trachea & immediately anterior to the vertebral column
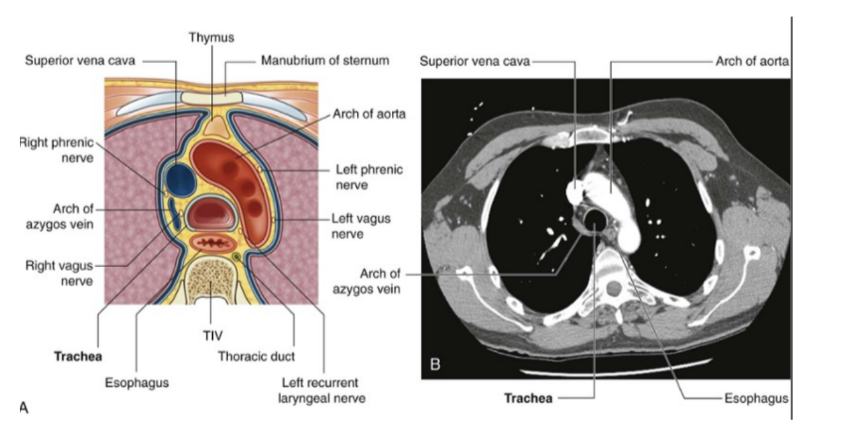
Nerves of the superior mediastinum
At the level of the superior mediastinum we mainly have the vagus & diaphragmatic/phrenic nerve —
Right & left vagus nerves of superior mediastinum
Right vagus nerve —
Enters superior mediastinum between right brachiocephalic vein & brachiocephalic trunk
Then goes down along trachea & passes posterior to roof of right lung then near esophagus to arrive at diaphragm
Left vagus nerve —
Enters mediastinum between left brachiocephalic vein & left common carotid artery
Passes posteriorly to the root of the left lung
At the level in which it crosses to the lateral side of the arch of the aorta there is the origin of the laryngeal nerve
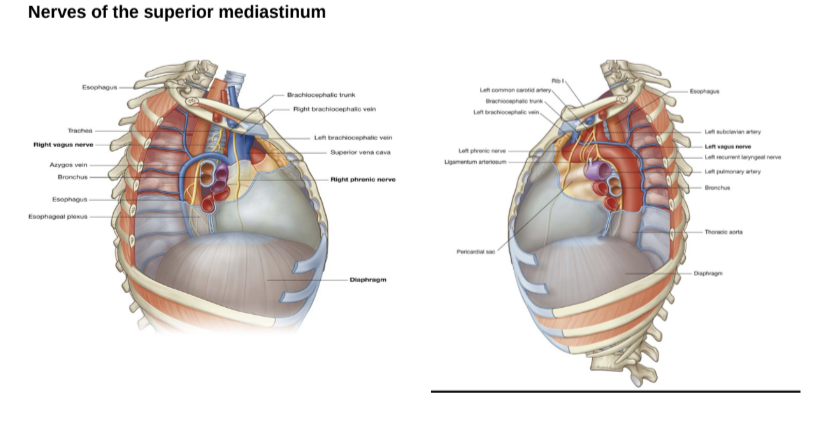
Phrenic nerve? left recurrent laryngeal nerve? slides & sbobina saying different things