Solute and Water Handling Part 1
1/58
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
59 Terms
The kidneys help to maintain the body’s extracellular fluid (ECF) volume by regulating the amount of ___ in the urine
Na+q
what is the most important contributor to the osmolality of the ECF?
Na+ (where Na+ goes, water follows)
t/f: The normal daily urinary excretion of Na+ equals the total Na+ filtered by the kidneys
false. The normal daily urinary excretion of Na+ is only a small fraction of the total Na+ filtered by the kidneys
The kidneys reabsorb % of the filtered Na+ by the time the tubule fluid reaches the renal pelvis
∼99.6
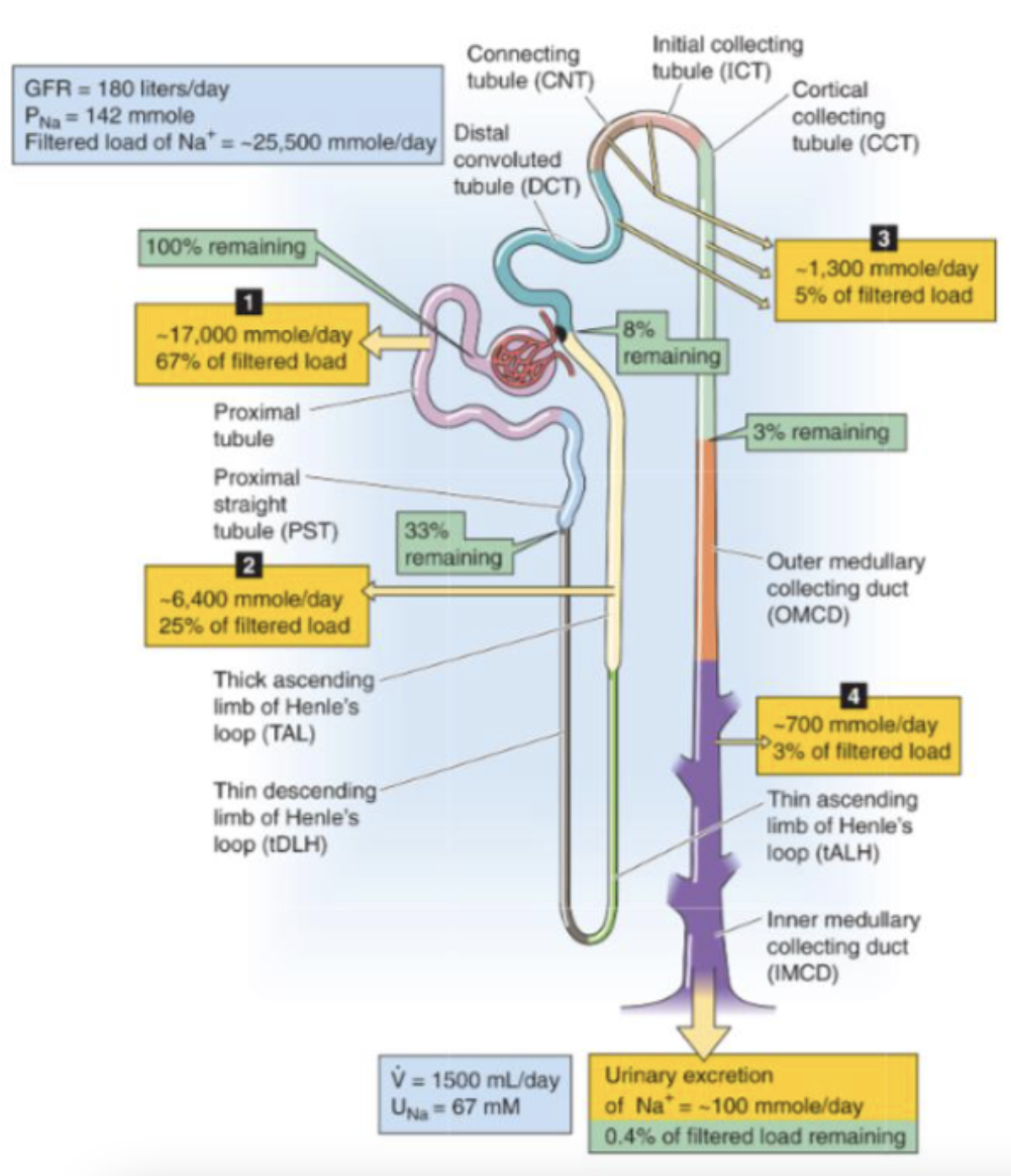
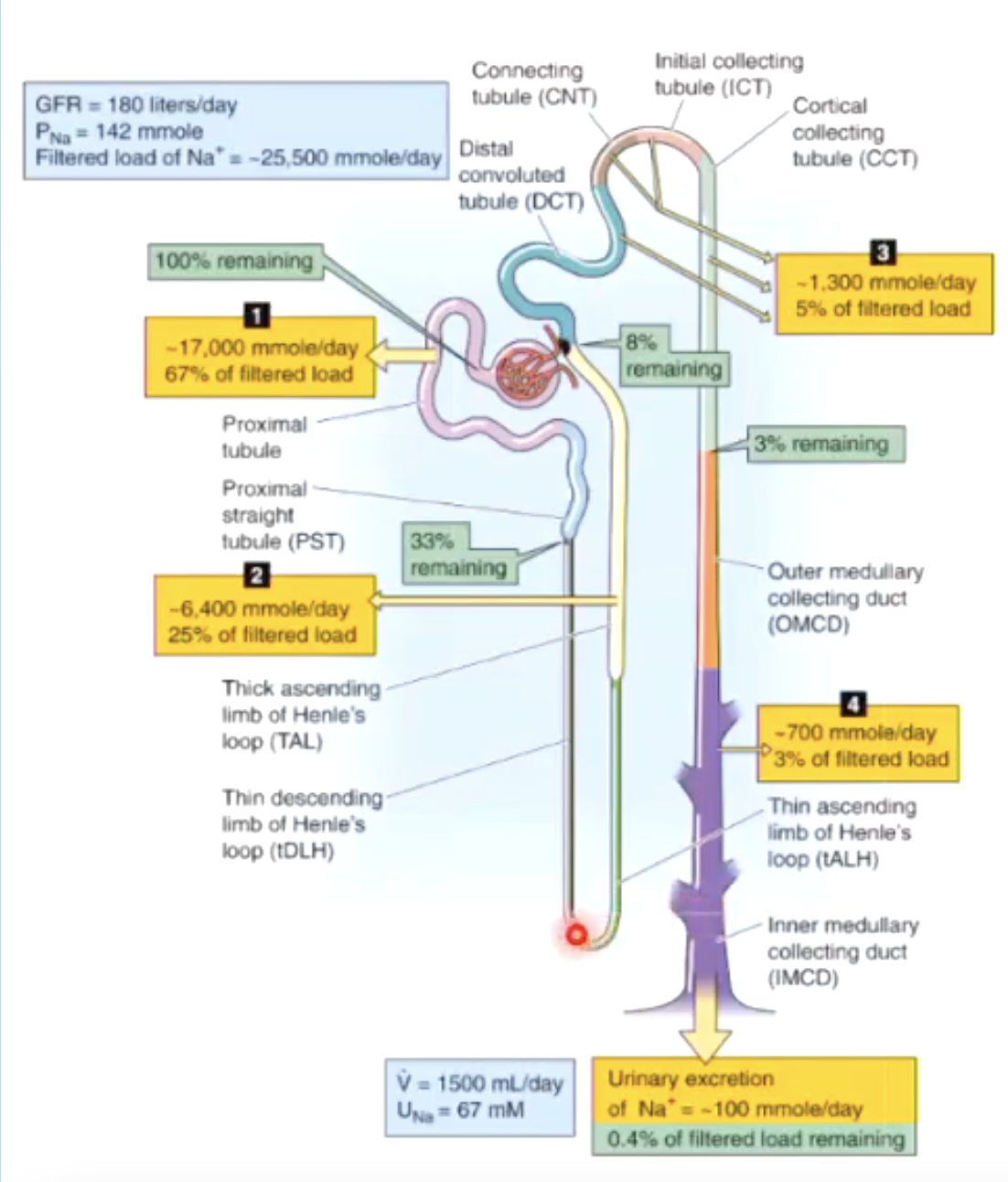
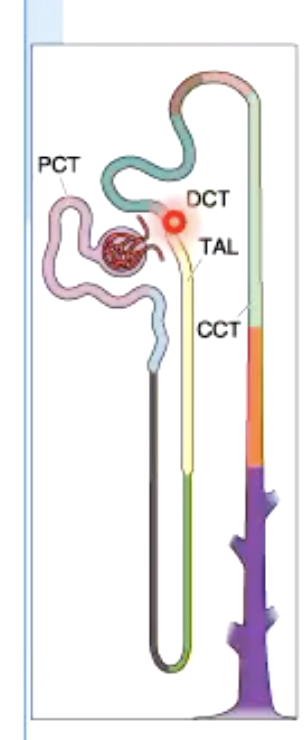
which portion reabsorbs the largest fraction of filtered Na+ (67%)?
proximal tubule
which portion reabsorbs the 25% of filtered Na+?
loop of Henle
The segments between the distal convoluted tubule and the cortical collecting tubule reabsorb % of the filtered Na+ load
~5%
The medullary collecting duct reabsorbs % of the filtered Na+ load
~3%
list the portions of renal system that reabsorb the most Na+ in order of most to least
proximal tubule (67%)
loop of Henle (25%)
segments between the distal convoluted tubule and the cortical collecting tubule (5%)
medullary collecting duct (3%
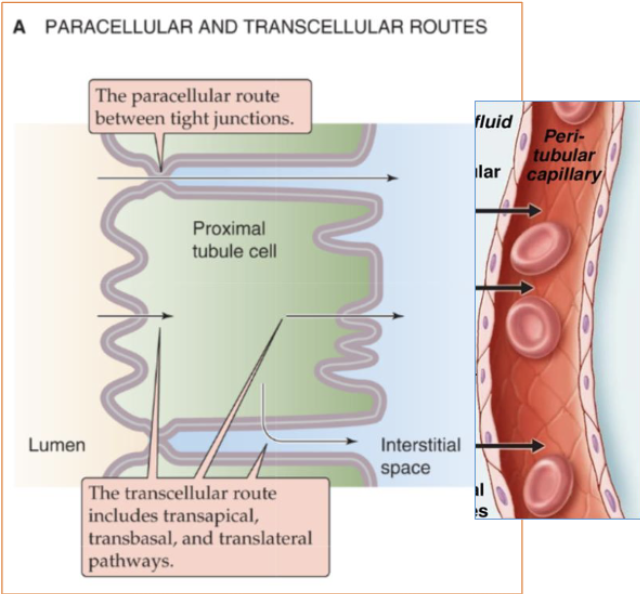
The tubule can reabsorb Na+ and Cl- via two pathways:
transcellular pathway
paracellular pathway
describe the transcellular pathway
Na+ and Cl- cross the apical and basolateral membranes before entering the blood
transport depends on electrochemical gradients, ion channels, and transporters
describe the paracellular pathway
Na+ and Cl- move by an extracellular route, through the tight junctions between cells
most diuretics target which portion of the renal system? why?
target starting at thick ascending limb of Henle’s loop (TAL) and after because the portion before that (proximal tubule) reabsorbs too significant of a fraction of Na+ (67%). meds that target proximal tubule will mess up too much.
t/f: proximal tubule is permeable to water
why is this important?
true
by the time you are reabsorbing sodium, you can absorb water at the same rate
in the first half of the proximal tubule, Na+ is reabsorbed with what solutes?
HCO3- (primarily)
other solutes (glucose, amino acids, Pi, lactate, etc.)
in the second half of the proximal tubule, Na+ is reabsorbed with what solutes?
Cl- (mainly)
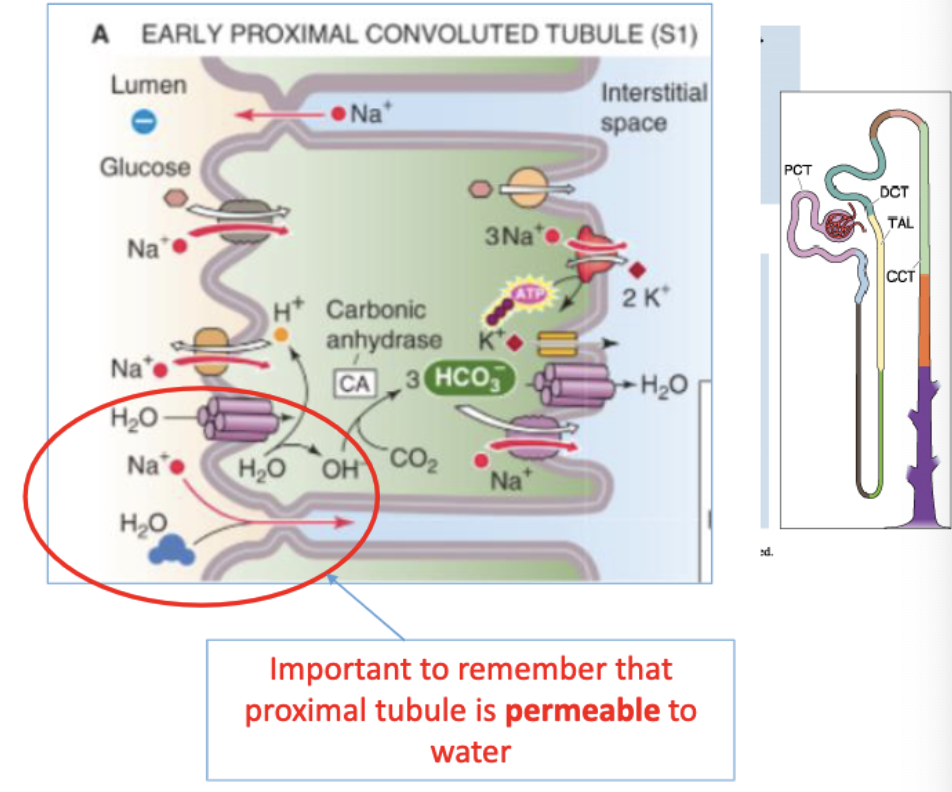
how does reabsorption occur in the proximal tubule?
(first half)
Na+ reabsorbed with HCO3- (and other solutes)
cotransporters in apical membrane couples downhill uptake of Na+ to uphill uptake of solutes (glucose, amino acids, phosphate, sulfate, lactate, carboxylic acids)
(second half)
Na+ reabsorbed with Cl-
Na+ entry also coupled to extrusion of H+ through Na-H exchanged
what is the renal disease that is either hereditary or acquired, results from an impaired ability of the proximal tubule to reabsorb HCO3−, Pi, amino acids, glucose, and low-molecular-weight proteins?
Fanconi syndrome
Fanconi syndrome is caused by the impaired ability of the proximal tubule to do what? what does this lead to?
inability to reabsorb HCO3-, Pi, amino acids, glucose, LMW proteins
Because other downstream nephron segments cannot reabsorb these solutes and protein, Fanconi syndrome results in increased urinary excretion of HCO3−, amino acids, glucose, Pi, and low MW proteins
what is an osmotic diuretic that is filtered into the tubular space where it increases tubular fluid osmolality?
Mannitol
what is mannitol? what does it do?
an osmotic diuretic that is filtered into the tubular space where it increases tubular fluid osmolality
results in impaired reabsorption of fluid → increased excretion of water
Bicarbonate is primarily reabsorbed in the
proximal tubule.
Metabolic acidosis can happen due to …?
urinary loss of bicarbonate CA inhibitors generally given for reasons other than diuresis.
because ocular fluid and CSF production is dependent on carbonic anhydrase (CA), inhibitors can be used to treat _______.
glaucoma
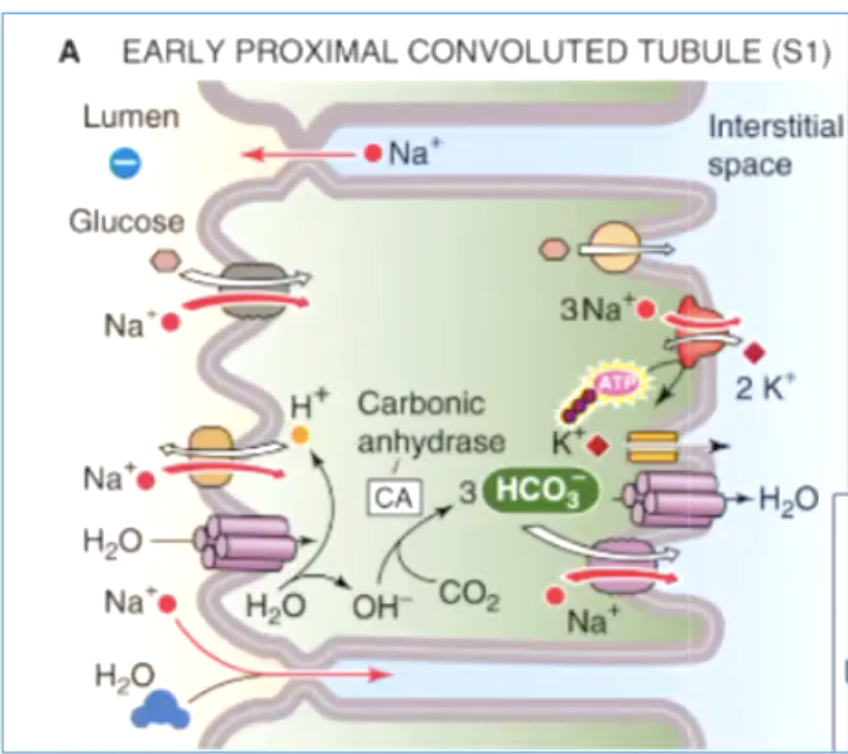
how is bicarbonate reabsorbed in the proximal tubule?
H+ ion secreted into lumen where it combines with filtered bicarbonate to form H2CO3
carbonic anhydrase (CA) enzyme converts H2CO3 → CO2 + H2O
CO2 diffuses into proximal tubule where it combines with H2O to form H2CO3 → H+ + HCO3-
HCO3- exits proximal tubule on blood side while H+ secreted back into tubule lumen
what are the 2 major mechanisms for taking up Na+ across the apical membrane in the thick ascending limb (TAL)?
Na/K/Cl cotransporter (NKCC2)
NHE3
how does the Na/K/Cl cotransporter tke up Na+ across the apical membrane?
couples the inward movement of ions driven by the downhill concentration gradients of Na+ and Cl−
what medications inhibit Na/K/Cl cotransporter?
loop diuretics (eg. furosemide and bumetanide)
the thick ascending limb (TAL) is called the…?
diluting segment
is TAL permeable or impermeable to water?
impermeable
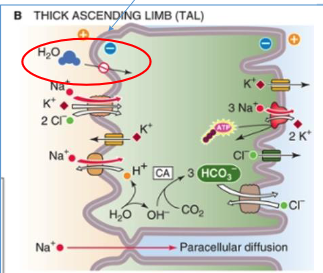
the most diluted urine is found where?
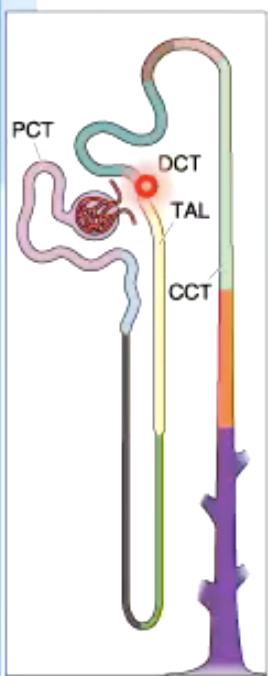
at the end of TAL/beginning of DCT
the most concentrated urine is found wher?
at the tip of the thin descending loop of Henle
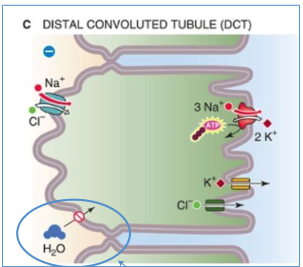
how is Na+ reabsorbed in the distal convoluted tubule (DCT)?
Na/Cl cotransporter (different from the Na/K/Cl channel by being independent of K+)
what medications inhibit Na/Cl cortransport?
thiazide diuretics (e.g., hydrochlorothiazide)
is DCT permeable or impermeable to water?
impermeable
Na+ reabsorption in the cortical collecting tubules (CCT) is mediated by?
the principal cell
in the cortical collecting tubules (CCT), Na+ crosses the apical membrane of the principal cell through…?
epithelial na+ channels
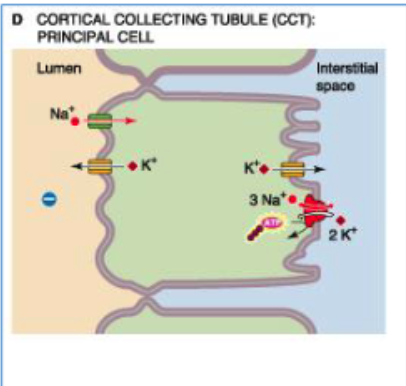
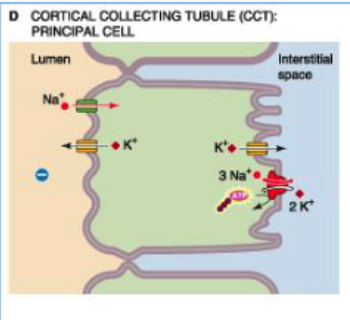
changing levels of what hormone may modulate the # of ENaCs (epithelial Na channels) that are open in the apical membrane of cortical collecting tubules?
aldosterone or AVP
what drugs block ENaCs (epithelial Na channels)?
diuretic drug amiloride (mild diuretic because Na+ reabsorption along collecting duct is modest)
Which of the following tubulary part of the nephron consumes the highest amount of ATP ?
A. Proximal tubule
B. Thin descending loop of Henle
C. Thick ascending loop of Henle
D. Distal convoluted tubule
E. Cortical collecting ducts
A. Proximal tubule
deals w highest amount of absorption (first step involves moleucles moving down concentration gradient but second part requires a lot of ATP to move those molecules toward the peritubular capillaries)
The kidney’s high O2 consumption reflects a high level of
active Na+ transport
Despite their low weight (<0.5% of body weight), the kidneys are responsible for % of total O2 consumption
7-10%
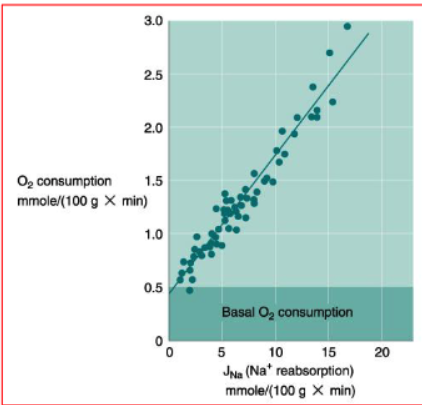
what does this graph tell us about Na+ reabsorption/transport and renal oxygen consumption?
All Na+ transport ultimately depends on the activity of ATP-driven Na-K pump and, therefore, on the generation of ATP by oxidative metabolism
renal O2 consumption is large and parallels Na+ reabsorption
An experiment is designed to determine how much of the plasma Na+ concentration is filtered into the tubule and subsequently reabsorbed. Isolated pump-perfused rodent kidney preparations are constructed. Plasma Na+ is 140 mEq/L and the filtered load is found to be 18 mEq/min. The predicted Na+ remaining in the tubule at the end of the descending limb of loop of Henle is which of the following?
A. 1 mEq/min
B. 2 mEq/min
C. 6 mEq/min
D. 12 mEq/min
E. 17 mEq/min
C. 6 mEq/min
18×0.67=12
18-12=6 mEq/min remaining
*end of descending limb of loop of Henle is the same as end of proximal tubule
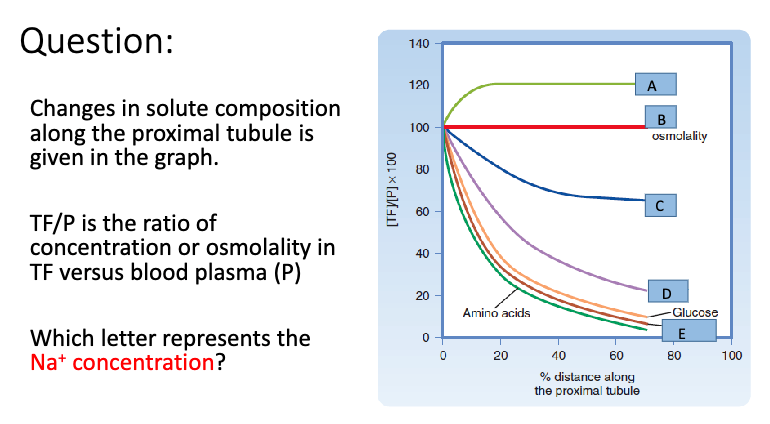
B
osmolality stays the same because although 67% of Na+ is being reabsorbed in the proximal tubule, an equal amount of water is also being moved which mean concentration of Na+ does not change. AMOUNT of Na+ would be decreasing (option D) but the concentration stays the same
in the proximal tubule, water mostly moves through _____ water channels on the apical and basolateral membranes
AQP1 (aquaporin)
t/f:water reabsorption at the proximal tubule is an active process.
false
Na+ can move from lumen to blood >>> the movement of water is not active, but passively follows the reabsorption of Na+
the water permeability of the proximal-tubule epithelium to water is very high
what are some examples of osmotic diuresis?
infusion of sucrose and mannitol
untreated diabetes mellitus
Normally, luminal [Na+] does not change along the proximal tubule. The only exception is ?
osmotic diuresis
what is osmotic diuresis?
poorly permeable substances are present in the plasma and, therefore, in the glomerular filtrate
what happens to luminal [Na+] in the proximal tubule when a pt has untreated diabetes mellitus?
blood glucose level may become too high for the capacity of renal tubules to reabsorb the highly elevated glucose load.
Glucose then acts as a poorly reabsorbed substance and as an osmotic diuretic
The TAL and all downstream segments have relatively low/high water permeability in the absence of AVP
low
The combination of NaCl reabsorption and low water permeability allows the TAL and all downstream segments to generate …?
a low luminal [Na+] and osmolality with respect to the surrounding interstitial fluid
what are the 3 major mechanisms through which the body regulates Na+ excretion?
glomerulotubular (GT) balance
increase reabsorption
Renin-angiotensin aldosterone
Arginine vasopressin increase Na+ reabsorption
Sympathetic Division of the ANS
decrease reabsorption
Atrial natriuretic peptide
Prostaglandin
Bradykinin
Dopamine
Bartter syndrome is a set of autosomal recessive genetic diseases characterized by ?
hypokalemia, metabolic alkalosis, and hyperaldosteronism
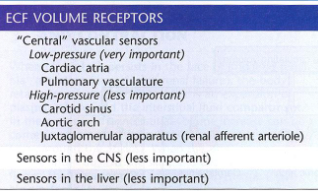
what ECF volume receptors are responsible for activating the regulation of Na+ excretion through the 3 major mechanisms? (glomerulotubular balance, renin/angio/arg/SNS, hormones)
what transporter is inactivated in Bartter syndrome?
Na+/K+/Cl− symporter
why does hypokalemia/decrease in ECFV occur in Bartter syndrome?
Inactivating mutations in gene coding for Na+/K+/Cl− symporter decrease NaCl reabsorption and K+ reabsorption by TAL
fall in ECFV stimulates aldosterone secretion → NaCl reabsorption and H+ secretion by distal tubule/collecting duct