PSYC 132: Chapter 13
1/20
Earn XP
Description and Tags
Affective Disorders
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
21 Terms
Affective disorders
Mental disorders characterized by dramatic changes or extremes of mood
Hormones affect thresholds for when a stimulus elicits a particular behavior or mood
Depression
Symptoms of depression can include:
Sadness
Feelings of worthlessness
Fatigue
Guilt
Indecisiveness
Disturbances in sleep and food intake
Absence of pleasure
Suicidal thoughts
Classification
Depression for more than 2 weeks diagnosed as
Major depressive disorder
Less severe symptoms that at least 2 years is
Dysthymia
Hormones and Depression
Thyroid hormones
Depression is correlated with low thyroid hormones
In some cases, it helps to administer thyroid-releasing hormone (TRH) → thyroid-stimulating hormone (TSH) → hormone production by the thyroid gland
Age is associated with declining thyroid function in many people
Extent that depression is caused by decreasing thyroid function with aging is unclear
Growth hormone and Prolactin
Correlation studies linking GH and prolactin are contradictory
Cortisol
Negative feedback system of the HPA axis appears to be impaired in some depressed individuals
Excessive cortisol found in about 50% of depressed individuals
Not seem to be related to stress because cortisol highest 3-4 hrs after sleep onset, when stress should be the lowest
Cushing syndrome → adrenal glands that produce excessive cortisol → depression is often a symptom
Addison disease → adrenal glands that produce insufficient cortisol → depression is often a symptom
Nonhuman animal studies are limited help as mood must be inferred
Estrogens
Deficits in estrogens linked with depression
However, there are many negative side effects associated with estrogen therapy
Sex differences in mood disorders begin at puberty; women are approximately twice as likely to develop a mood disorders
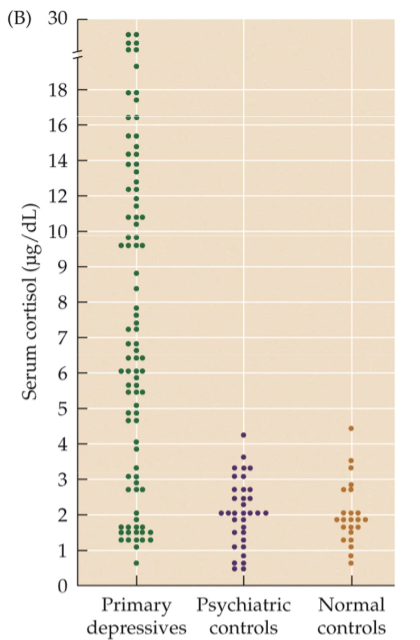
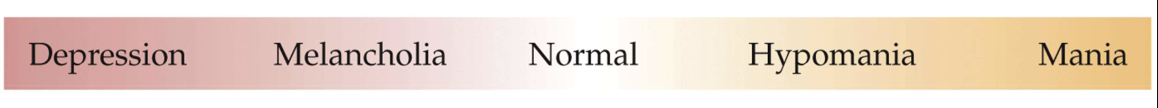
Fig. 13.2: HPA axis and depression
Blood cortisol concentrations are often higher in depressed than in nondepressed individuals
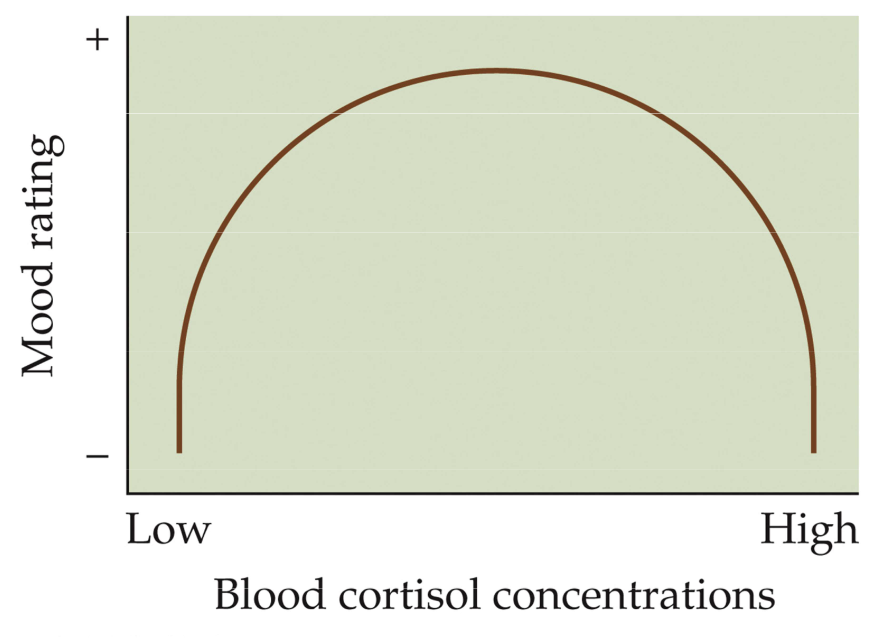
Fig. 13.4: Cortisol and mood
Optimal mood ratings correspond with moderate blood cortisol concentrations
Fig. 13.6: Estradiol withdrawal precipitation of depressive symptoms
When estradiol is withdrawn from women with a history of past depression, depression ensued
Postpartum depression (PPD)
Outcome of typical hormone changes associated with childbirth
Confusion about its definition and if it’s a unique disorder
Past PPD is the best predictor of future PPD
More likely among women bringing an unwanted pregnancy to term
Men are nearly as likely as women (68% : 82%) to have PPD symptoms within 2 months of childbirth
Perimenstrual Syndrome
(‘peri’ → ‘around the time’) A constellation of symptoms that recurs on a cyclical basis and is associated with menstruation
Symptoms:
Anxiety
Depression
Moodiness
Fatigue
Associated with the normal changes in steroid hormone levels during menstruation cycle
Most mood changes occur during late luteal phase when progesterone is peaking and estrogen is decreasing
No consistent differences in progesterone or estrogen have been found between women who do and do not report PMS
No endocrine or other biological disorder has been consistently related to PMS
PMS may be a consequence of modern civilization — of chronic cyclic hormonal functions
A typical women with have nearly 300 cycles by her mid thirties, with another 100-150 before menopause
Cognitive features
Some women report positive mood changes and improved cognitive performance
5-15% of women report elevated energy levels and well-being
Some report increase in sexual interest
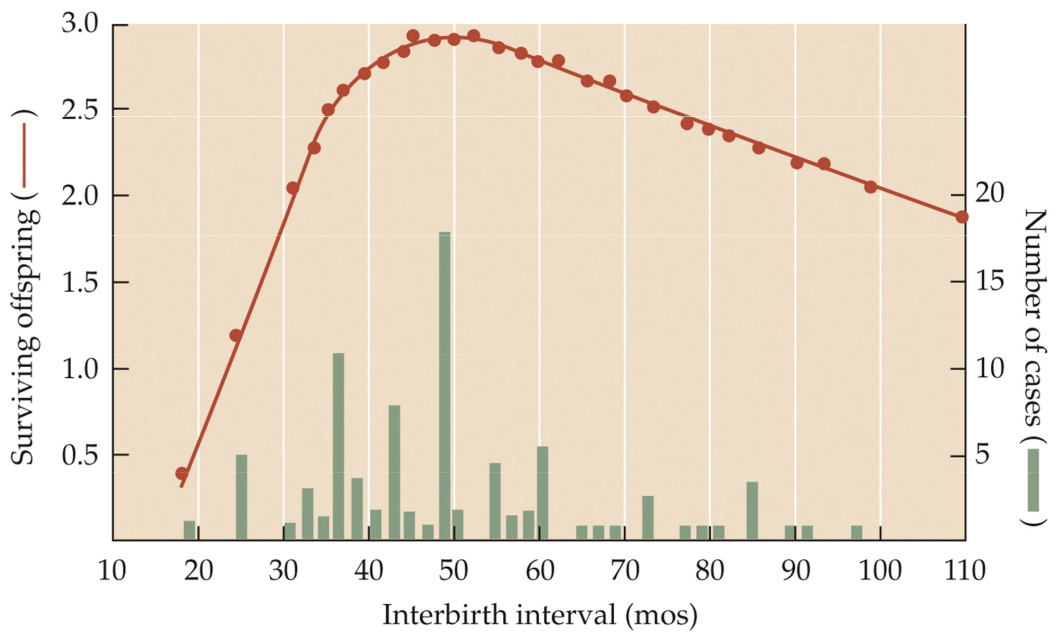
Fig. 13.8: Optimal human interbirth interval
The optimal birth spacing is about 50 months
Seasonal Affective Disorder (SAD) AKA winter depression
Seasonal changes in behavior in many human and nonhuman animals
Three features atypical of depression
Hyperphagia (abnormally high hunger)
Carbohydrate cravings
Hypersomnia (excessive sleepiness)
Prevalence is 1%-10% with higher rates at higher latitudes
More common in women than men (3.5 to 1)
Melatonin
Concentrations are higher during the night than during the day in both nocturnal and diurnal animals
Converted from serotonin in the pineal gland
Bright lights have been used to alleviate SAD presumably by resetting biological clocks by affecting timing of melatonin release
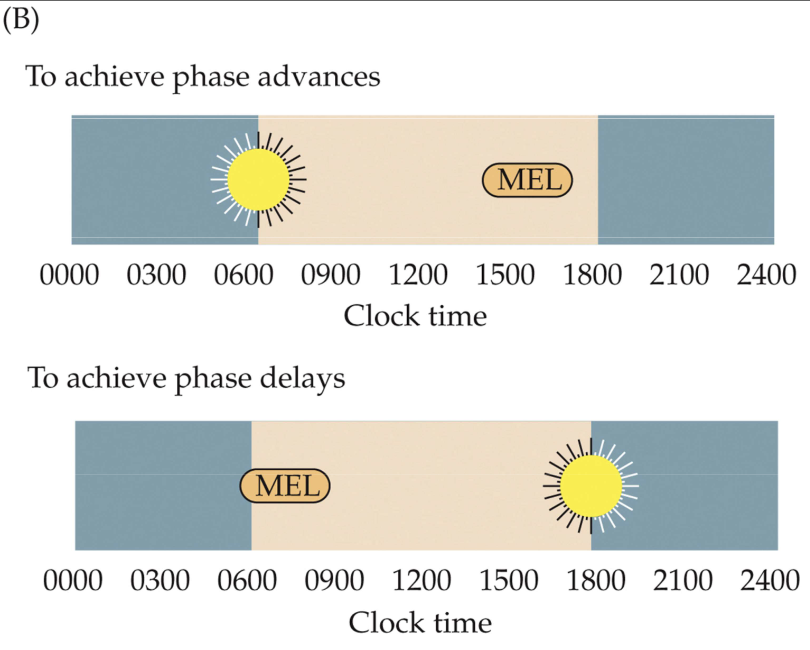
Fig. 13.14: Phase responses to melatonin
Phase advance
Light exposure scheduled in the morning and melatonin given in the afternoon
Phase delay
Light exposure scheduled in the evening and melatonin given in the morning
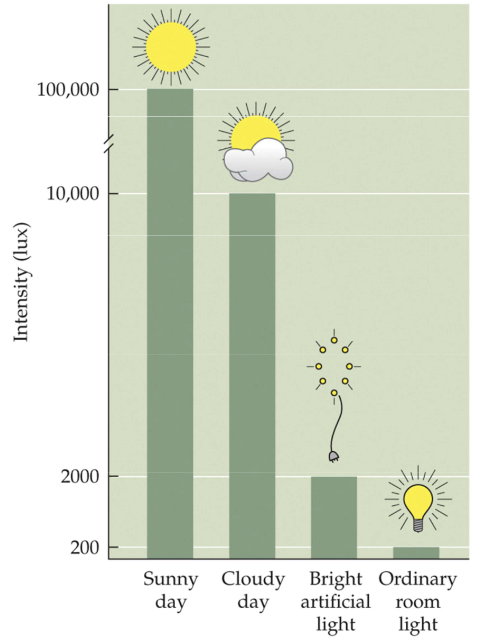
Fig. 13.15 Outdoor light is far brighter than artificial light
Artificial light is often around 200-500 lux
Below what is necessary to have a physiological effect on rhythms and mood
Sunlight may be 100,000 lux in intensity
Even on cloudy days → 10,000 lux
At least 1500 lux is necessary for the inhibition of human melatonin secretion
Complete blindness
About half of the 200,000 completely blind people in the US are free-running
24.2-24.9 hr periods
Often experience insomnia during the night and somnolence (drowsiness) during the day
Androgens and Affective Disorders
More than a quarter high school seniors are currently estimated to using anabolic steroids
Research on rodents has demonstrated that androgens have rewarding properties
e.g. Syrian hamsters prefer an aqueous solution with testosterone over plain water
Gynecomastia (breast enlargement in males)
Peripheral conversion of androgens to estrogens
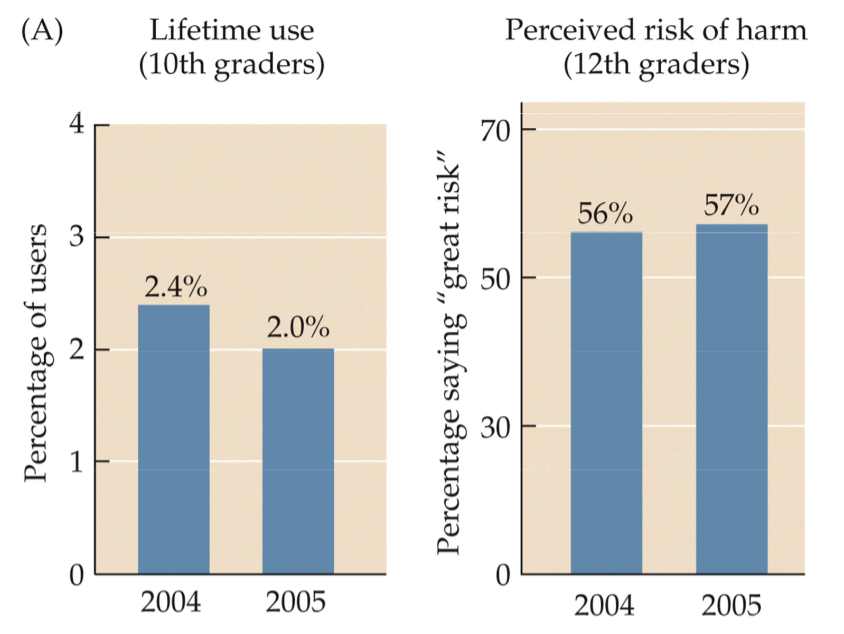
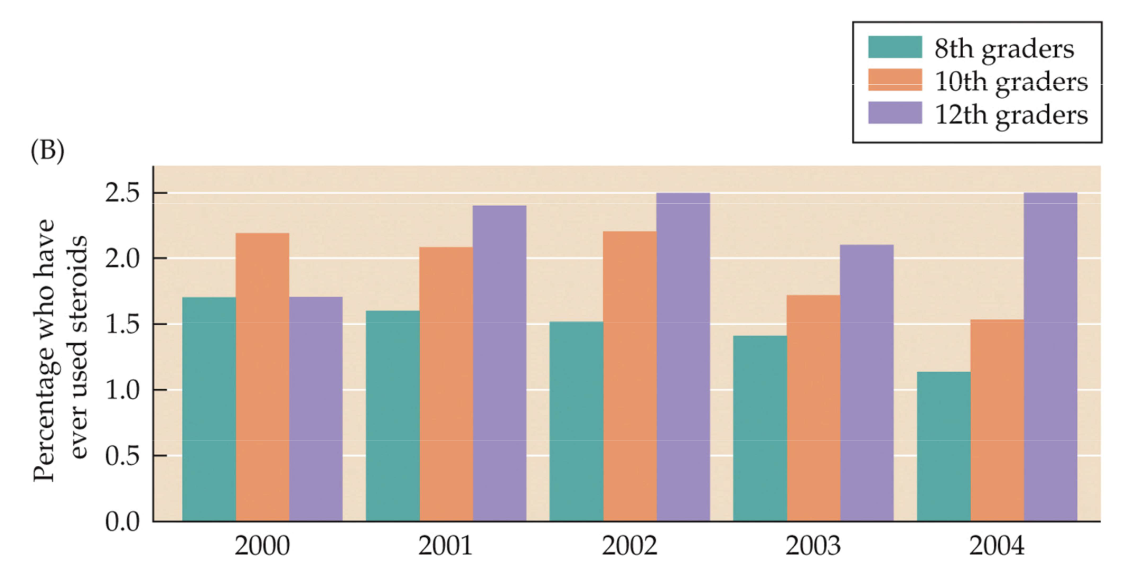
Fig. 13.17: Lifetime use of anabolic steroids
Decreased among 10th graders in 2005
Perceived risk of harm among HS seniors has increased
Contrasts with previous years that showed increased usage (see image)
Steroid use
Adverse effects
Immune dysfunction
Liver dysfunction
Kidney dysfunction
Cardiovascular dysfunction
Endocrine dysfunction
Depression has been observed in those who stop steroid use
Acute myocardial infarction (heart attack) and suicide are the most common causes of premature death among steroid abusers
Anorexia Nervosa
Serious, potentially life-threatening. Characterized by self-starvation and excessive weight loss
Bulimia Nervosa
Serious, potentially life-threatening. Characterized by cycles of binge eating and compensatory behaviors (e.g. self-induced vomiting)
Typically have normal or slightly above average body mass
Commonalities between Anorexia and Bulimia
Disordered food intake
Distorted body image
Compulsive exercise
Purging behavior
Strong genetic component
More common in Western societies
Almost 10x more common in women than in men
Possibly organized by lack of prenatal androgens and activated by pubertal hormones
Hormones and Eating Disorders
Leptin (Decreases appetite)
Anorexia
Very low in anorexic patients
Leptin treatment does not reverse low body mass
Androgens
Females of opposite-sex twins are exposed to more prenatal androgens than females of same-sex twins
Highest to lowest rates of disordered eating: (least to most prenatal androgens)
Females of same-sex twins
Females of opposite-sex twins
Males of opposite-sex twins
Males of same-sex twins
Emotional and binge eating peak during mid-luteal phase
Progesterone is highest and estrogens are relatively high