Reproductive System Test
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
65 Terms
Gonadotropin-releasing hormone (GnRH)
Origin: Produced by the hypothalamus.
Target: Acts on the anterior pituitary gland.
Effect(s): Stimulates the release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the anterior pituitary.
Follicle-stimulating hormone (FSH)
Origin: Produced by the anterior pituitary gland.
Target: Acts on the ovaries in females and the testes in males.
Effect(s): In females, it stimulates the growth and maturation of ovarian follicles and promotes estrogen secretion. In males, it stimulates sperm production (spermatogenesis).
Luteinizing Hormone (LH)
Origin: Produced by the anterior pituitary gland.
Target: Acts on the ovaries in females and the testes in males.
Effect(s): In females, it triggers ovulation and promotes the formation of the corpus luteum, which produces progesterone. In males, it stimulates the interstitial cells of the testes to produce testosterone.
Testosterone:
Origin: Produced primarily by the testes in males and in smaller amounts by the ovaries and adrenal glands in females.
Target: Acts on various tissues, including the reproductive organs, muscles, bones, and other tissues.
Effect(s): Facial hair, deepening of the voice, and muscle growth. It also plays a role in sperm production and libido in both males and females.
Inhibin:
Origin: Produced by the ovaries in females and the testes in males.
Target: Acts on the anterior pituitary gland.
Effect(s): Inhibits the secretion of FSH from the anterior pituitary gland, helping to regulate the production of sex hormones and gametes (eggs and sperm).
Prolactin:
Origin: Produced by the anterior pituitary gland.
Target: Acts primarily on the mammary glands.
Effect(s): Stimulates milk production (lactation) in females after childbirth. It also has other functions, including playing a role in the reproductive system, metabolism, and behavior.
Oxytocin:
Origin: Produced by the hypothalamus and released by the posterior pituitary gland.
Target: Acts on the uterus and mammary glands.
Effect(s): Stimulates uterine contractions during childbirth and promotes the ejection of milk from the mammary glands during breastfeeding. It also plays a role in social bonding and emotional behavior.
Estrogen:
Origin: Produced primarily by the ovaries in females, with smaller amounts produced by the adrenal glands and testes in males.
Target: Acts on various tissues throughout the body, including the reproductive organs, bones, and brain.
Effect(s): Breast development and widening of the hips. Menstrual cycle, fertility, and bone health.
Progesterone:
Origin: Produced primarily by the corpus luteum in the ovaries in females, with smaller amounts produced by the adrenal glands and testes in males.
Target: Acts on the uterus and other reproductive tissues.
Effect(s): Prepares the uterine lining for implantation of a fertilized egg and helps maintain pregnancy. It also plays a role in regulating the menstrual cycle and has effects on the breasts and other tissues.
Human chorionic gonadotropin (hCG):
Origin: Produced by the placenta during pregnancy.
Target: Acts on the ovaries and corpus luteum.
Effect(s): Supports the production of progesterone by the corpus luteum during the early stages of pregnancy, helping to maintain the uterine lining and support the developing embryo.
Human placental lactogen:
Origin: Produced by the placenta during pregnancy.
Target: Acts on various tissues, including the mammary glands and maternal metabolism.
Effect(s): Stimulates mammary gland development and milk production in preparation for breastfeeding. It also plays a role in regulating maternal metabolism and nutrient supply to the fetus.
Relaxin:
Origin: Produced primarily by the corpus luteum in the ovaries during pregnancy, and also by the placenta and other tissGues.
Target: Acts on various tissues, including the uterus and pelvic ligaments.
Effect(s): Relaxes the uterine muscles and pelvic ligaments, helping to prepare the body for childbirth. It also plays a role in softening and widening the cervix and pubic symphysis during pregnancy and labor.
GnRH (Female):
Origin: Hypothalamus
Target: Anterior Pituitary
Effects: Production and release of FSH & LH
FsH (Female):
Origin: Anterior Pituitary
Target: M - Sustentacular cells (testis)
F - Follicles (ovary)
Effects: Production of ABP
Follicle growth & estrogen production
Estrogen:
Origin: Follicles (Ovaries)
Target: Brain and Endometrium (Uterus)
Effects: Low E: Inhibit release of gonadotropins
High E: Stimulate release of LH (FSH)
High E+P: Inhibits cycle restart
Thickens the endometrium (Endometrium produces progesterone receptors)
Spermatogonium and Primary Spermocyte
Spermatogenesis begins with the division of spermatogonia, which are diploid stem cells found in the seminiferous tubules of the testes. These cells undergo mitosis to produce more spermatogonia and some primary spermatocytes.
Primary spermatocytes are the result of mitotic division of spermatogonia. They are diploid cells that undergo the first round of meiotic division (meiosis I) to produce two secondary spermatocytes.
Secondary spermatocyte and Spermatids:
Secondary spermatocytes are haploid cells resulting from the first meiotic division of primary spermatocytes. They then undergo the second round of meiotic division (meiosis II) to produce haploid spermatids.
Spermatids are haploid cells resulting from the second meiotic division of secondary spermatocytes. These spermatids are immature and round in shape.
Spermatids
Spermiogenesis is the process by which spermatids mature into spermatozoa. This transformation involves significant structural changes. During this phase, the round spermatids develop a tail and become elongated.
Spermatozoa:
also known as sperm cells, are the mature male gametes produced at the end of spermiogenesis. They are specialized cells with a head containing the nucleus, a midpiece containing mitochondria for energy production, and a flagellum (tail) for motility.
Retrograde Ejaculation:
Semen flows backward into the bladder instead of exiting through the penis during ejaculation, often due to muscle or nerve dysfunction. Can cause infertility.
Erectile Dysfunction:
Inability to achieve or maintain an erection for sexual intercourse. Can result from physical or psychological factors.
Testicular Cancer:
Cancer that develops in the testicles, typically affecting younger men. Symptoms include testicular lumps, swelling, or discomfort.
Prostate Cancer:
Cancer occurring in the prostate gland, common in older men. Symptoms may include difficulty urinating, blood in urine or semen, and pelvic pain.
STD’s:
Bacterial Infections: Examples include Gonorrhea, Chlamydia, and Syphilis.
Viral Infections: Examples include HIV, HSV (Herpes), and HPV.
Primordial Follicles (A):
immature ovarian follicles containing a primary oocyte surrounded by a single layer of flattened cells. They are dormant until they are activated during the reproductive cycle.
Primary Follicles (B):
Primary follicles are activated primordial follicles that have started to grow. They consist of a primary oocyte surrounded by a layer of granulosa cells.
Secondary Follicles (C):
larger than primary follicles and contain a primary oocyte surrounded by multiple layers of granulosa cells. They also have a fluid-filled space called an antrum.
Graafian (Vesicular or Mature) Follicles (D):
mature ovarian follicles ready for ovulation. They are characterized by a large fluid-filled antrum and a bulging follicle wall. The primary oocyte within the Graafian follicle completes meiosis I, resulting in the formation of a secondary oocyte and a polar body.
Corpus Luteum (E):
forms from the remnants of the Graafian follicle after ovulation. It secretes progesterone and estrogen, which help maintain the uterine lining during the menstrual cycle in preparation for possible implantation of a fertilized egg.
Corpus Albicans (F):
If fertilization does not occur, the corpus luteum degenerates into the corpus albicans, a small, scar-like structure. This marks the end of the ovarian cycle for that month.
Ovarian cycle (follicular/luteal phases):
Follicular phase: Development of ovarian follicles until ovulation.
Luteal phase: Formation of the corpus luteum after ovulation.
Ovarian hormones (estrogen/progesterone):
Estrogen stimulates uterine lining growth.
Progesterone maintains the uterine lining.
Uterine (menstrual) cycle (menstrual/proliferative/secretory phases):
Menstrual phase: Shedding of uterine lining.
Proliferative phase: Growth of uterine lining.
Secretory phase: Preparation of uterine lining for potential pregnancy.
Pelvic Inflammatory Disease (PID):
Infection of female reproductive organs, often caused by STIs.
Symptoms: pelvic pain, abnormal discharge, fever.
Can lead to infertility if untreated.
Breast Cancer:
Malignant tumor in breast tissue, most common cancer in women.
Risk factors: age, genetics, hormones, lifestyle.
Symptoms: breast lump, changes in breast or nipple.
Treatment: surgery, chemotherapy, radiation, hormone therapy.
Cervical Cancer:
Cancer in cervix, often caused by HPV infection.
Symptoms: abnormal bleeding, pelvic pain.
Detected through Pap smears and HPV testing.
Treatment: surgery, radiation, chemotherapy.
Somatic cells:
Make up the body tissues and organs.
Are diploid (have two sets of chromosomes).
Undergo mitosis for growth, repair, and maintenance.
Examples include skin, muscle, and nerve cells.
Germ Line cells:
Give rise to gametes (sperm and egg cells).
Are haploid (have one set of chromosomes).
Undergo meiosis to produce gametes.
Found in the reproductive organs (ovaries and testes).
Mitosis:
Makes identical copies of cells for growth and repair.
Happens in normal body cells.
Makes cells with the same number of chromosomes as the parent cell.
One division, four stages.
Meiosis:
Makes sex cells (sperm and eggs) for reproduction.
Happens only in reproductive organs.
Makes cells with half the number of chromosomes as the parent cell.
Two divisions, each with four stages.
Explain three way meiosis differs between egg and sperm production: (1)
Number of Cells Made:
Eggs: One egg cell is made from each round of meiosis.
Sperm: Four sperm cells are made from each round of meiosis.
Explain three way meiosis differs between egg and sperm production: (2)
When it Happens:
Eggs: Meiosis starts before birth but pauses until puberty, then continues monthly.
Sperm: Meiosis starts at puberty and continues throughout life.
Explain three way meiosis differs between egg and sperm production: (3)
Size and Nutrients:
Eggs: One big egg gets most of the nutrients, while three small cells get very little and break down.
Sperm: All four sperm cells get equal amounts of nutrients and are the same size.
Anatomy of the Male system,:
Testes
Ducts
Epididymis
Ducts (Vas) Deferens
Ejaculatory Duct
Urethra
Accessory Glands
Seminal Glands
Prostate
Bulbourethral Glands
Penis
Functions of Male System:
Epididymis: Sperm Maturation
Vas Deferens: Carries sperm from testes to ejaculatory duct
Ejaculatory Duct: Where seminal vesicle joins vas deferens to urethra
Penile Urethra: Delivers sperm to the vagina
Functions of Male System: (Glands + Sperm Production)
Semen = sperm + products of accessory glands
Extra fluids support and nourish the sperm
Accessory Glands
Seminal Gland: (60)
Seminal Glands: Alkaline to neutralize acidity of vagina
Fructose to nourish sperm
Prostate Glad: (30)
Activates and protects sperm
Bulbourethral Gland: (10)
Mucus to neutralize acidity of urine and urethra
Semen content:
Transport medium
Fructose
Antibiotic chemicals to protect
Chemicals that facilitate and activate sperm movement
Describe ANS control over male erection and ejaculation:
Erection: Enlargement and stiffening of penis
From engorgment of erectile tissues of penis
PS ANS
Ejaculation:
Propulsion of sperm from male duct system
Reproductive ducts and glands empty into urethra
Muscular movements:
Penis bulbocavernosus muscles rapidly contract
S ANS
Describe sperm structure, including flagellum, midpiece, and acrosome.
Head:
Contains the genetic material (like a blueprint) and a special cap called the acrosome that helps it break into the egg.
Midpiece:
Acts like a power plant, providing energy for the sperm to swim.
It's packed with tiny energy factories called mitochondria.
Tail (Flagellum):
This is the tail that helps the sperm swim.
It moves like a whip, pushing the sperm forward towards the egg.
Female Reproductive Anatomy:
Ovaries
Fallopian Tubes
Uterus
Vagina
Mammary Glands
Supporting Structures
Describe alterations to the ovarian/menstrual cycles during pregnancy:
Ovarian Cycle:
During pregnancy, ovulation (the release of an egg from the ovary) typically stops.
This means that the ovarian cycle, which includes follicular development, ovulation, and the formation of the corpus luteum, is interrupted.
Menstrual Cycle:
Menstruation, which is the shedding of the uterine lining (period), stops during pregnancy.
Without menstruation, the typical phases of the menstrual cycle, including menstruation, the proliferative phase (building up the uterine lining), and the secretory phase (preparing for potential implantation), are disrupted.
In simple terms, pregnancy puts the ovarian and menstrual cycles on hold. Ovulation stops, and there is no menstrual bleeding because the body is focused on supporting the growing baby instead.
List the steps of sperm penetration:
Sperm Transport:
Navigating the Uterus and Fallopian Tubes:
Penetration of Cervical Mucus:
Migration to the Egg
Fertilization:
Describe the roles of hyaluronidase:
Breaking Down Barriers:
Hyaluronidase is produced by the acrosome, a structure at the tip of the sperm.
It helps the sperm break down a substance called hyaluronic acid, which is found in the outer layer of cells surrounding the egg.
Facilitating Sperm Movement:
By breaking down hyaluronic acid, hyaluronidase helps create pathways for the sperm to swim through.
This allows the sperm to navigate through the protective layers surrounding the egg more easily.
In summary, hyaluronidase acts like a molecular "key" that helps unlock barriers around the egg, allowing sperm to reach and fertilize it.
List the major events in each trimester of gestation.
First Trimester
Cleavage from blastocyst
Implantation (hyaluronidase)
Placenta forms
Embryo begins to develop
Second Trimester
Organ system development
Body shape and proportions change
Third Trimester
Rapid growth and adipose deposition
Organ system becomes fully functional
Blastocyst:
It's like a tiny ball of cells formed from the fertilized egg.
The outer part will become the placenta, and the inner part will become the baby.
Implantation:
This is when the blastocyst attaches to the wall of the uterus (like sticking to it).
It happens around a week after fertilization.
It's important because it's how the baby gets nutrients from the mother.
Gastrulation:
After implantation, the cells in the blastocyst start to rearrange.
This rearrangement creates different layers that will become the different parts of the baby's body.
It's like the first steps in building the baby's body plan.
Functions of Placenta:
Exchange of nutrients, metabolic gases and wastes
Umbilical Arteries
Deoxygenated blood to the placenta
Umbilical Vein
Oxygenated blood from the placenta
List the difference between dizygotic twins, monozygotic twins, and chimerism:
Dizygotic (Fraternal) Twins
Fraternal Twins
Monozygotic (Identical) Twins
Identical Twins
Chimerism:
Chimerism can occur in twins or in individuals who are not twins.
presence of genetically distinct cells within a single individual
List and define the three stages of labor:
Dilation stage
Cervix widens
Expulsion stage
Delivery of infant
Placental state
Delivery of placenta
Home fertility:
a tool used by individuals or couples trying to conceive to predict the most fertile days in a woman's menstrual cycle. It detects the surge in luteinizing hormone (LH) levels in urine, which occurs shortly before ovulation.
Home pregnancy:
A home pregnancy test is a tool used by individuals to detect pregnancy. It works by detecting the presence of human chorionic gonadotropin (hCG) hormone in urine, which is produced by the placenta shortly after implantation of the embryo in the uterus.
List and describe the main points of contraception where contraceptives play a role.
Contraception is the act of preventing pregnancy. This can be a device, a medication, a procedure or a behavior. Contraception allows a woman control of her reproductive health and affords the woman the ability to be an active participant in her family planning.
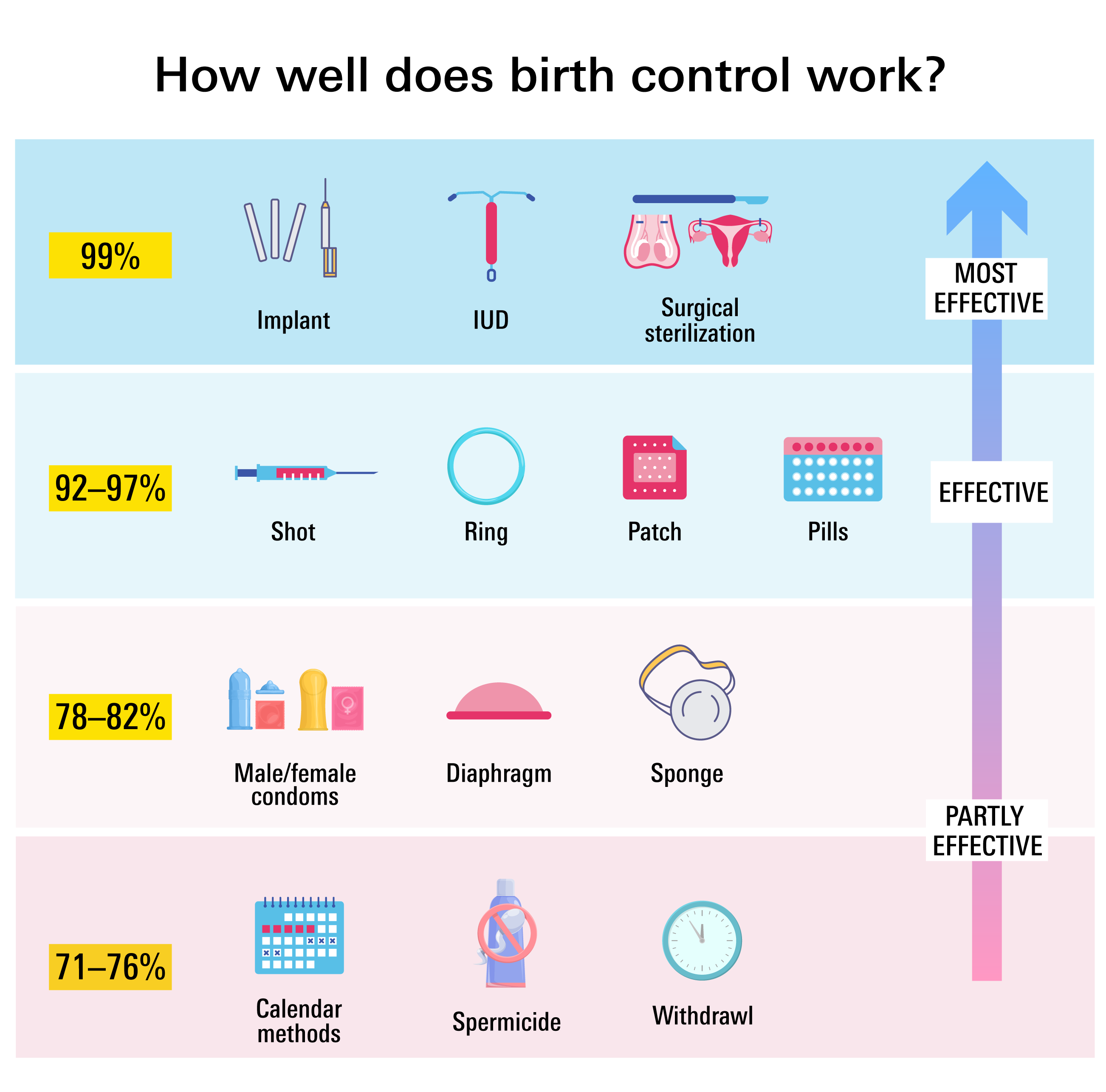
Compare the effectiveness of different types of birth control.
Ectopic pregnancy:
Implantation of embryo outside uterus