GP- platelet disorders, hemostasis, and coagulation
1/42
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
43 Terms
disorders of hemostasis are common in what animals?
dogs
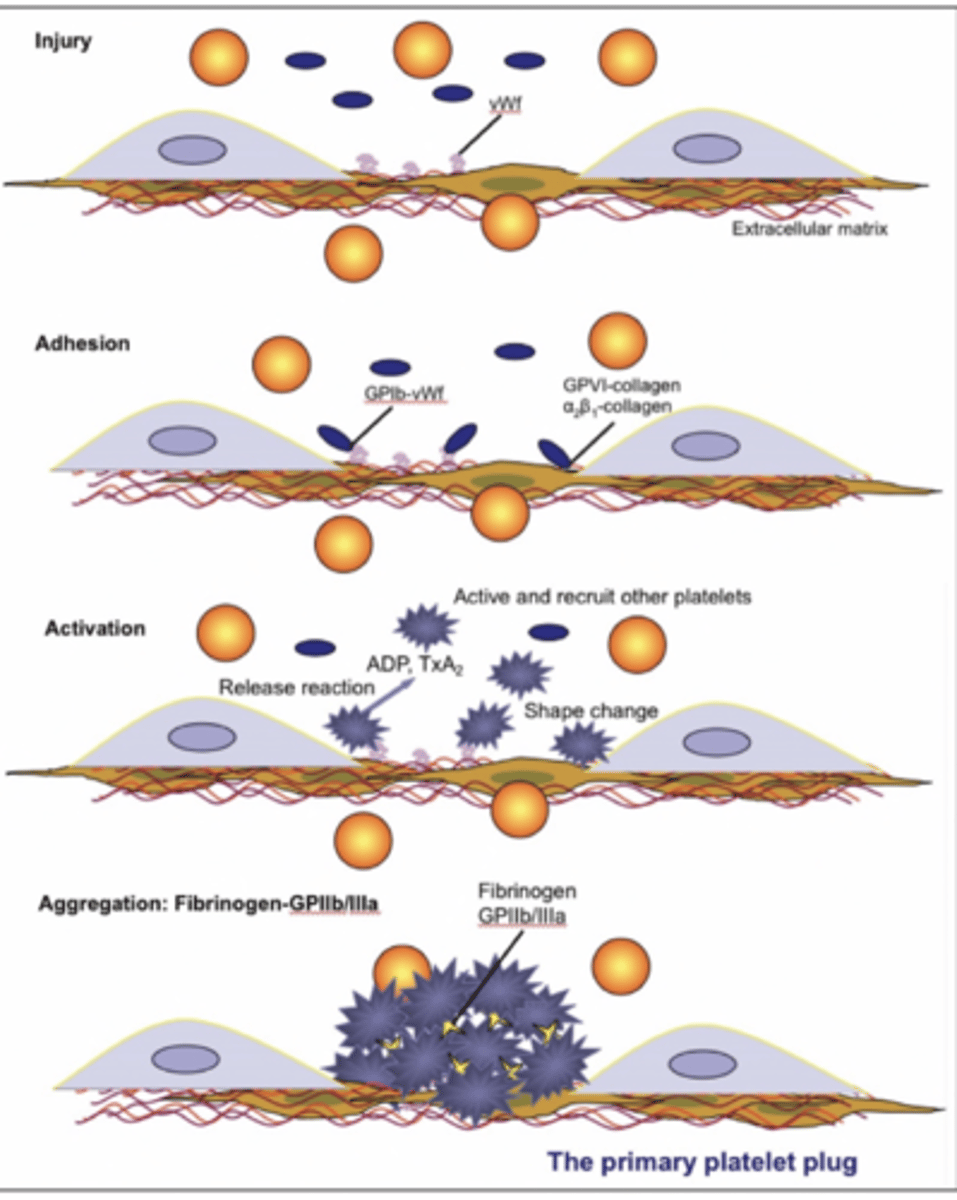
what is primary hemostasis?
the first step of hemostasis, where the vessels constrict and the platelet plug is formed
the endothelial damage causes the exposure of collagen, attracting platelets. the von willebrand factor allows the platelets to adhere to collagen.
what is secondary hemostasis?
the second step of hemostasis, where the platelet plug is turned into a clot.
both the intrinstic and extrinsic pathways work towards the activation of factor X, which combines with proaccelerin to be able to convert prothrombin to thrombin, which converts fibrinogen to fibrin
the products of fibrinolysis are...
FDP and D dimers
activators and inhibitors of coagulation and fibrinolysis are normally in dynamic balance, but a failure of this equilibrium can result in....
abnormal bleeding OR risk of intravascular coagulation (thrombosis)
what is antithrombin III?
a natural anticoagulant produced by hepatocytes to prevent excessive clot formation
what roles do protein C and protein S have with coagulation?
they inhibit certain coagulation factors
they are dependent on vitamin K, so an animal with vitamin K deficiency will cause them to not work,
what are the main regulators of fibrinolysis?
PA inhibitor (impairs tPA)
antiplasmins (impair plasmin)
thrombocytopenia and thrombocytosis are bleeding disorders that affect ______ hemostasis. (primary/secondary)
primary
what may cause an individual to have thrombocytopenia?
increased use:
DIC
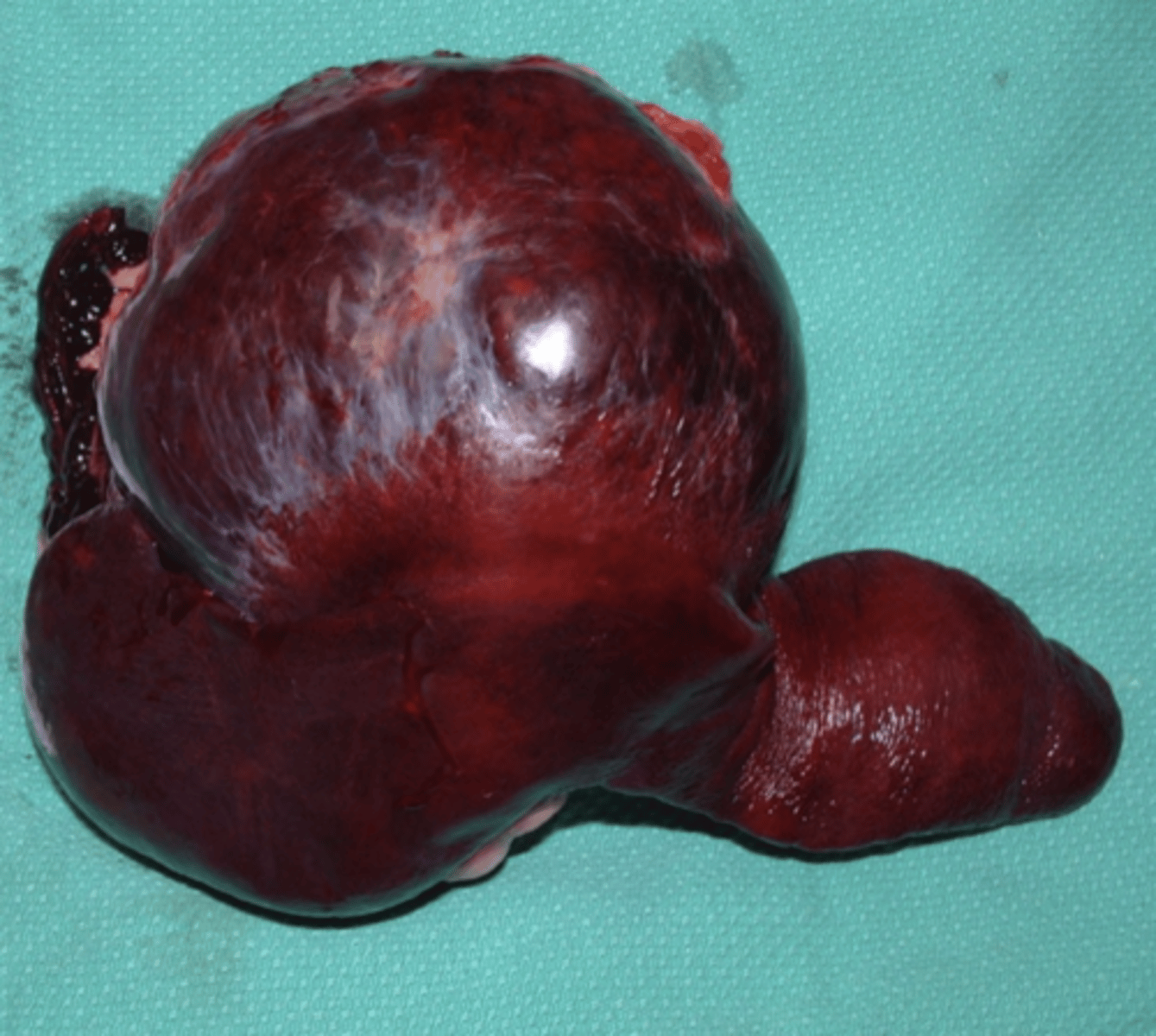
hemangiosarcoma
congenital
increased destruction
immune mediated
ehrlichiosis
vasculitis
low production
BM disease
what is thrombocytopathy?
a normal number of platelets, but they do not work
what are the reasons an animal might have thrombocytopathy?
hereditary
von willebrand disease
acquired
drugs
secondary to another disease (cushings, ehrlochiosis, renal disease, liver disease, etc)
do clotting factor deficiencies impact primary or secondary hemostasis?
secondary
what might cause the low production of platelets?
bone marrow disease
what can cause the increased destruction of platelets?
immune-mediated problem
ehrlichiosis
vasculitis
what can cause the increased use of platelets, leading to thrombocytopenia?
DIC
hemangiosarcoma
what are reasons an animal may not make enough clotting factors?
vitamin K deficiency (malnutrition, rodenticide)
congenital disease
liver failure
why might an animal abnormally use more clotting factors, leading to their deficiency?
DIC
what are the clinical signs of an animal with thrombocytopenia or thrombocytopathy?
petechiae
ecchymosis
mucous membrane and skin bleeding
hematuria
epistaxis
immediate bleeding after venipuncture

what are the clinical signs of an animal with a coagulation problem (clotting factor deficiencies)?
muscle and joint bleeding
bleeding into body cavities
hematomas
delayed bleeding after venipuncture
if an animal comes in with lots of petechiae, ecchymosis, and epistaxis, they probably have a problem with what part of hemostasis?
primary hemostasis
thrombocytopenia or thrombocytopathy
if an animal comes in with hematomas, muscle and joint bleeding, and hemothorax, they probably have a problem with what part of hemostasis?
secondary hemostasis
clotting factor deficiency
how can we diagnose a problem with primary hemostasis (thrombocytopenia/thrombocytopathy)?
-platelet count (with a machine)
-looking at platelet morphology (with a blood smear)
-bone marrow examination
-platelet function tests, like mucosal bleeding time
why is it important to perform a platelet count before surgery?
because if the animal has thrombocytopenia, surgery might cause a lot of unwanted bleeding, so we try to avoid it
why is the machine less reliable than a blood smear when doing a platelet count?
because if there are aggregations of platelets, it doesn't count these, so the platelet count will be very low
what numbers of platelets indicate thrombocytopenia?
<100-150 x10^3/L (with machine)
<3 per field (with blood smear)
what is mucosal bleeding time? what does it measure?
it is the time taken to stop bleeding after an incision made with a lancet on the upper lip, vaginal mucosa, or toenail cuticle
it tells us how well the platelets are working
the incision should stop bleeding after:
dogs- <4-5 min
cats- <2.5 min
horses- <10-14 min
if we perform a mucosal bleeding time test on a dog and it takes 6 minutes to stop bleeding, what is our conclusion?
he has a platelet problem: thrombocytopenia or thrombocytopathy. dogs should take 4-5 min to stop bleeding
if we perform a mucosal bleeding time test on a cat and it takes 2 minutes to stop bleeding, what is our conclusion?
his platelets are working normally
if we perform a mucosal bleeding time test on a horse and it takes 20 minutes to stop bleeding, what is our conclusion?
he has a platelet problem: thrombocytopenia or thrombocytopathy. horses should take 10-14 min to stop bleeding
how can we diagnose a secondary hemostasis disease?
with laboratory tests with machines:
prothrombin time
activated partial thromboplastin time
fibrinogen
thrombin time
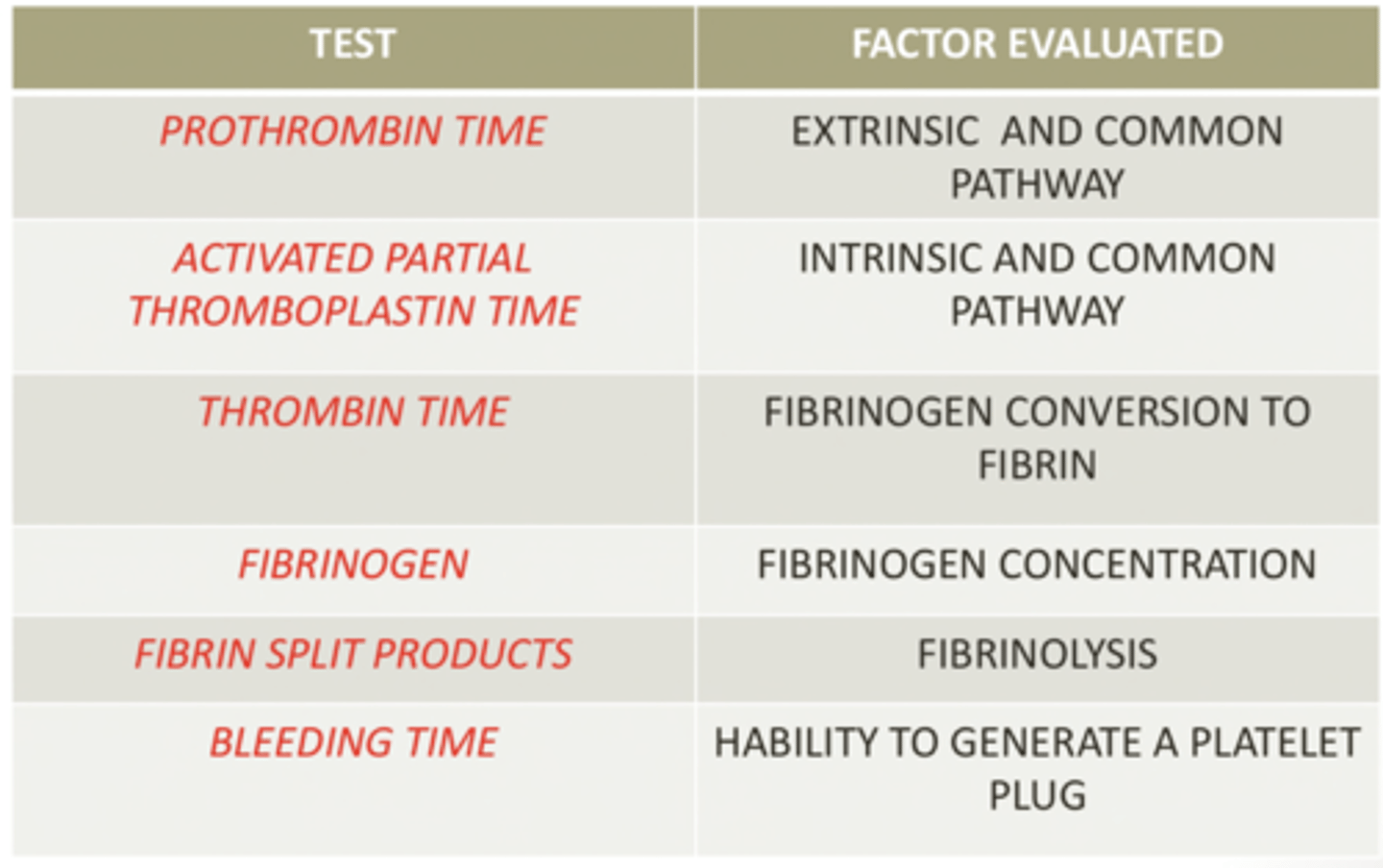
which coagulation pathway does an activated partial thromboplastin time test evaluate?
intrinsic and common
what is von willebrand disease?
a congenital defect, causing the inability of platelets to adhere to a vascular injury. it is common in dobermans
is von willebrand disease a thrombocytopenia, thrombocytopathy, or clotting factor defect?
thrombocytopathy- there are normal numbers of platelets, but they cannot adhere properly
what is hemophilia A?
a sex linked factor VIII deficit (only males are asymptomatic)
what problems with coagulation does a vitamin K deficit cause?
a deficit in factors II, VII, IX, and X
problems with secondary hemostasis
why might an animal have a vitamin K deficiency?
ingestion of rodenticides- they have warfarin and brom adiolone, which inhibit vitamin K, causes GI issues, and damaged blood vessels, so the animal internally bleeds but cannot clot to stop the bleeding
liver disease or inflammatory bowel disease- cause problems in digesting vitamin K
how is rodenticide poisoning treated?
induce vomiting (if it was ingested recently)
activated charcoal (absorbs undigested poison in stomach)
oral vitamin K for 1 month
what is DIC?
disseminated intravascular coagulation
a problem with primary and secondary hemostasis, in which there is a widespread activation of the clotting cascade. this causes blood clots in the circulation, causing hypoxia and therefore organ damage. clotting factors and platelets are used up, so the animal internally bleeds more as well.
it is usually caused by an underlying condition like infections, sepsis, neoplasia, vascular disorders, toxins, pancreatitis

how can a hemangiosarcoma cause DIC?
it causes the release of factor X
this is common in german shepherds
how can pancreatitis cause DIC?
it causes tripsin activation, which causes endothelial damage, plasminogen activation, and activation of factors X and II
how is DIC treated?
heparin (anticoagulant)
blood transfusion
how do the laboratory tests of an animal with DIC appear?
low fibrinogen
thrombocytopenia
low antithrombin
schistocytes