6. Red Blood Cell Metabolism
1/18
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
19 Terms
Blood Components
55% Plasma, 45% RBCs, <1% WBC’s and platelets
General characteristics of RBCs
Function
Abundance in blood
Organelles
Function: transport oxygen and contribute to buffering of the blood
The most abundant cell in blood —> compared to WBCs and platelets
Has no organelles, as they are lost during differentiation
Red Blood Cell Metabolism General Overview
_________ RBCs contain no ______________ ____________, thus metabolic pathways are forced to occur in the ___________
Because they lack ________,the only way RBC’s can generate ATP is through _________, as they convert ________ into ___________
ATP of RBCs is used for what 3 things?
RBCs _________ contains enzymes for _____________ and _________ of damage done by __________ _________ _________ , they get these enzymes from the ______ pathway
Mature RBCs contain no intracellular organelles, thus metabolic pathways are forced to occur in the cytoplasm
Because they lack organelles ,the only way RBC’s can generate ATP is through glycolysis, as they convert pyruvate into lactate
ATP of RBCs is used for ion transport, phosphorylation of membrane proteins and priming of glycolysis reactions
The RBC’s cytosol contains enzymes for prevention and repair of damage done by reactive oxygen species , they get these enzymes from the PPP pathway
Pentose Phosphate Pathway/ Hexose Monophosphate (HMP) Shunt —> Quick review
What route does it bypass?
What glycolysis precursor does it start and which one does it end with?
What electron carrier does PPP generate and what is it used for?
PPP breaks down what type of biomolecule?
What are the two phases? Which one generates the electron carrier molecule mentioned before
Which stage is irreversible
What molecule does the oxidative phase start and end with, how many electron carriers are formed
What is the crucial enzyme needed for the oxidative phase, what happens when it is deficient?
What molecule does the Non-Oxidative phase start and end with?
Bypasses the first stage of glycolysis
Starts with glucose-6-phosphate and ends with fructose-6-phosphate
PPP generates NADPH, which is used in nucleotide biosynthesis, Fatty acid synthesis and cholesterol biosynthesis
PPP breaks down carbohydrates/sugars
The two phases are oxidative and non-oxidative; NADPH is generated in the Oxidative phase only
The irreversible stage is the Oxidative one
Oxidative phase starts with glucose-6-phosphate and ends with ribulose-5-phosphate; 2 NADPH are produced
The enzyme is glucose-6-dehydrogenase, if it is deficient it can cause hemolysis/hemolytic anemia because there is no NADPH for glutathione to detoxify ROS
The non-oxidative phase starts with ribulose-5-phosphate and ends with fructose-6-phosphate
Rapoport- Luebering Shunt —> occurs only in RBC’s
Steps
Why is the function of this in metabolism
What pathway is the initial molecule shunted from
Because of this shunt, what happens to net ATP produced from glyolysis?
1,3-bisphosphoglycerate (1,3BPG) — mutase → 2,3BPG
—phosphatase→ 3-phosphoglycerate
The function is to produce 2,3GPG to: moderate oxygen binding, stabilize the deoxy form of hemoglobin and facilitate oxygen release to tissues
1,3-BPG is shunted from glycolysis
Because a step is skipped (would generate 2 ATP), the second stage of glycolysis only generates 2 ATP, which brings the net ATP of glycolysis to 0 when you subtract the 2 ATP from the preparative stage
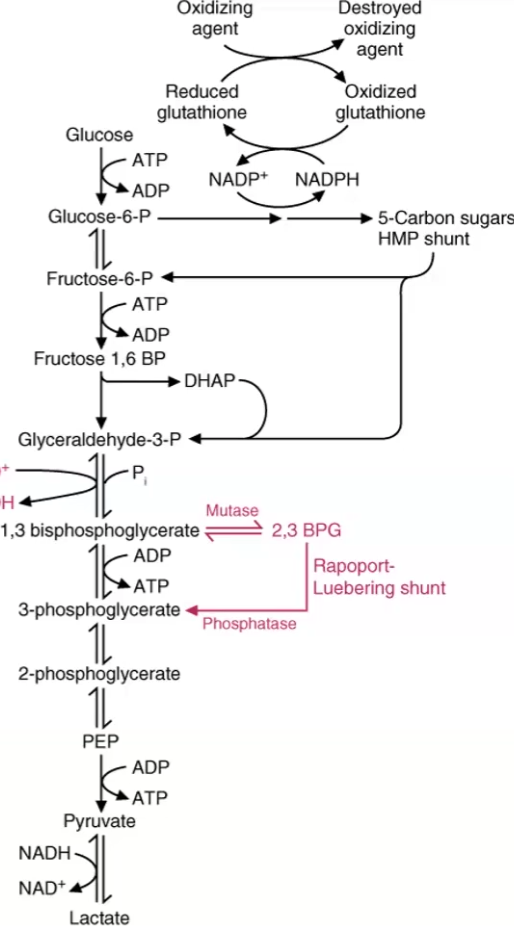
If RBC’s can only produce ATP from glycolysis, they cannot undergo The e’ Transport system or TCA….. how do they use the NADH produced by glycolysis?
NADH reduces Cytochrome b5, which converts Fe3+ (ferric, deoxy) of hemoglobin into Fe2+ (ferrous, oxy)

What is the lactate produced by RBC’s used for?
The Cori cycle in the liver turns lactate into glucose through gluconeogenesis
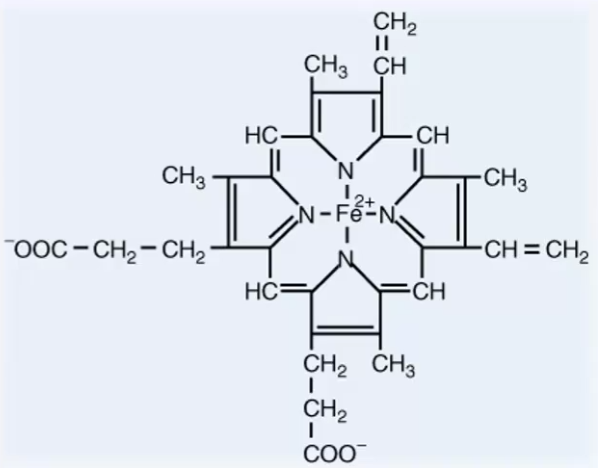
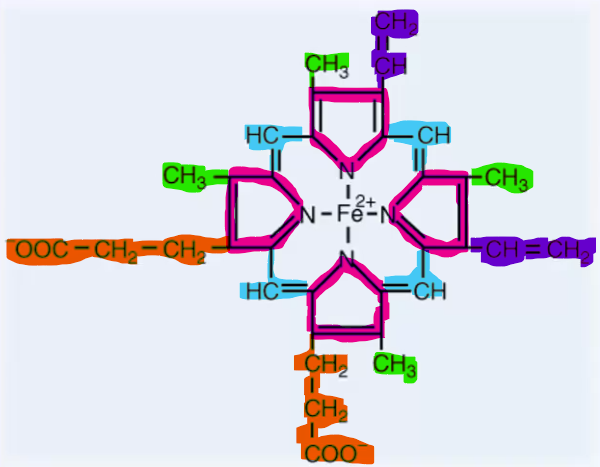
Heme structure: describe groups, order and main structure
Heme is the main ____________ found in the body and forms _____________, ____________ and the ____________
4 Pyrrole rings connected by 4 methylene bridges
8 side chains on pyrrole rings: 4 methyl (M) groups, 2 vinyl (V) groups, 2 propionate (P) groups
Order: MVMVMPPM
Heme is the main porphyrin found in the body and forms hemoglobin, myoglobin and the cytochromes
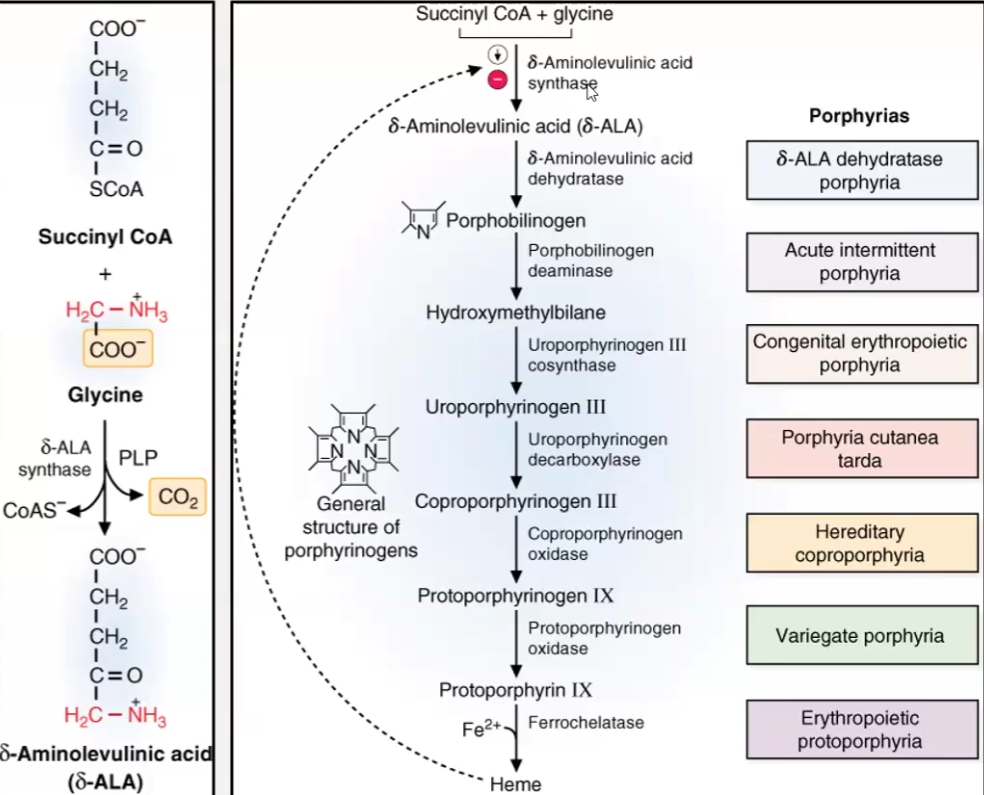
Heme synthesis:
3 steps
Requirements of the step 1 enzyme
Allosteric inhibitors
glycine + succinyl-CoA — delta aminolaevulinic acid synthase→ delta aminolaevulinic acid (delta-ALA)
Condensation reaction where glycine is decarboxylated
Enzyme requires pyridoxal phosphate (PLP) —> Pyridoxine (Vit B6) —> deficiencies cause microcytic hypochromic anemia (RBCs that are smaller and thus have less heme)
Allosterically inhibitor: Heme
2 molecules of delta-ALA —delta ALA dehydratase→ porphobilinogen (a pyrrole)
4 pyrrole rings condense to form a chain and then a series of porphyrinogens
Deficiencies in the enzymes used in all these steps are all different types of Porphyrias
Iron is added
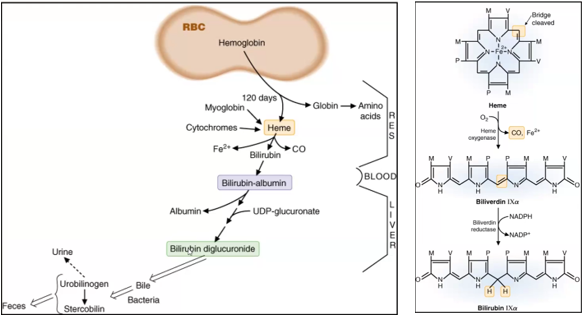
Heme degradation occurs when _____ reach the end of their life at approximately _____ days and they are _____________ by the cells of the ___________________ __________
Steps of Heme Degradation
Heme degradation occurs when RBC’s reach the end of their life at approximately 120 days and they are phagocytosed by the cells of the reticuloendothelial system
Steps of Heme Degradation
Hemoglobin → Heme + Globin
Globin —> Amino acids
Heme → Bilirubin
Heme → Biliverdin
methylene bridge is broken
Catalyzed by heme oxygenase
CO2 and iron released
Biliverdin → Bilirubin
Center methylene bridge reduced (double bond to single bond)
Catalyzed by Biliverdin reductase
NADPH needed from PPP
Bilirubin → Bilirubin-albumin
Bilirubin is being carried in the blood by albumin
Bilirubin-Albumin → Bilirubin diglucuronide → bile
Conversion to bilirubin-diglucuronide allows excretion by the liver as bile
Sources of Iron
Iron is obtained from the _____, the daily amount for men and post-menopausal women is ____, while for pre-menopausal women it is _________ due to menstruation
The average US diet contains _____, but only ______% is normally absorbed
Are iron deficiencies common or uncommon?
Iron in meats is in the ______ form, which is _______ absorbed, and iron in plants is in the _______ form, which is _____ absorbed
Vitamin ___ can ________ the uptake of non-heme iron from the digestive tract
Iron is obtained from the diet, the daily amount for men and post-menopausal women is 10mg, while for pre-menopausal women it is 15mg due to menstruation
The average US diet contains 10-50mg, but only 10-15% is normally absorbed
Are iron deficiencies are common
Iron in meats is in the heme form, which is readily absorbed, and iron in plants is in the non-heme form, which is not readily absorbed
Vitamin C can increase the uptake of non-heme iron from the digestive tractF
Iron transport
Iron is absorbed in the __________ state
Iron is then ________ to the __________ state by the enzyme ____________
Iron is carried in the blood as _______ by the protein ______________
_____ + Apotransferrin= ____________ _________
Transferrin binds to __________ _________ on the cell surface and is _________, then it is __________ to _____ and released into the __________ by iron transporter __ ( ____ )
Deficiency in ________ leads to __________ _________ ________ ________
Once in the cytoplasm, iron is ________ to necessary ________
Excess iron is ______ back into ______ and binds to __________ for _____-term storage in the _______, _______ and bone __________.
_______ + Apoferritin = _________ complex
Iron can be drawn from ________ stores for cells that require iron such as __________ that use it to synthesize ____________
About __mg of iron is lost per day in feces, urine, sweat, skin and menstruation
Iron is absorbed in the ferrous (Fe2+) state
Iron is then oxidized to the ferric (Fe3+) state by the enzyme ferroxidase (ceruloplasmin)
Iron is carried in the blood as Fe3+ by the protein Apotransferrin
Iron + Apotransferrin= Transferrin complex
Transferrin binds to transferrin receptors on the cell surface and is internalized, then it is reduced to Fe2+ and released into the cytoplasm by iron transporter I ( DMT-I)
Deficiency in DMT-I leads to refractory hypochromic microcytic anemia
Once in the cytoplasm, iron is shunted to necessary enzymes
Excess iron is oxidized back into Fe3+ and binds to Ferritin for long-term storage in the liver, spleen and bone marrow.
Iron + Apoferritin = Ferritin complex
Iron can be drawn from ferritin stores for cells that require iron such as reticulocytes that use it to synthesize hemoglobin
About 1mg of iron is lost per day in feces, urine, sweat, skin and menstruation
Red Blood Cells
Under a microscope, RBC’s appear as a red ____ with ______ central area
The shape facilitates _____ _________ across cell membrane
The shape facilitates RBC’s to ________ across capillaries with small __________ to deliver oxygen to tissues
They can ______ and ________ to travel restricted spaces
The _____ determines the viability of RBC’s because they have to pass its small _____ diameter, thus the RBC must be highly _________ to pass through
Damaged cells become _________ in the _____ and destroyed by ___________
Under a microscope, RBC’s appear as a red discs with pale central area
The shape facilitates gas exchange across cell membrane
The shape facilitates RBC’s to travel across capillaries with small diameter to deliver oxygen to tissues
They can shrink and expand to travel restricted spaces
The Spleen determines the viability of RBC’s because they have to pass its small 3 micrometer diameter, thus the RBC must be highly deformable to pass through
Damaged cells become trapped in the spleen and destroyed by macrophages
Red Blood Cells
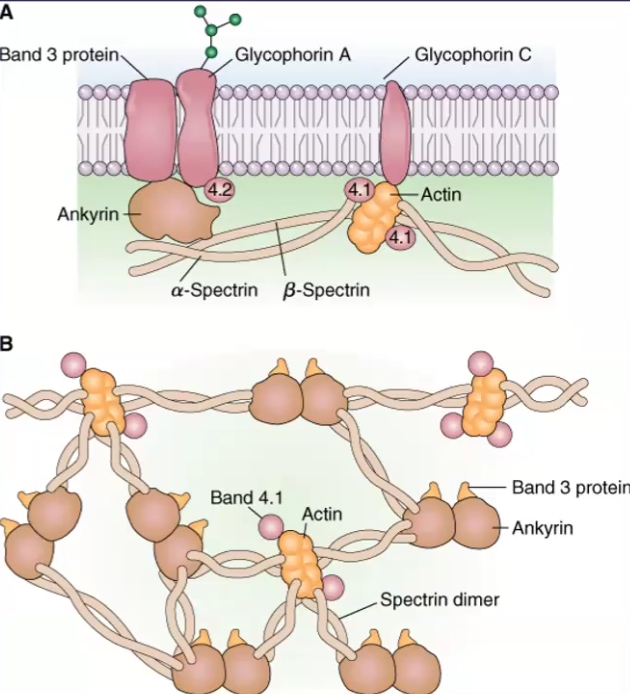
RBC deformability lies in its shape, but also the _________ of the proteins that make up the membrane
These proteins are on the ___________ side of the membrane
List the proteins and their function
Spectrin is the ________ of the membrane and are the ones responsible for altering ____ when the cell is subjected to _________ stress
_______ RBC’s cannot synthesize new membrane proteins or lipids to use for ___________ detoxification
Defect in these membrane proteins can result in _________ ________
When RBC’s lose their deformability, they can ____ in response to stress, get trapped and ________ or be malformed and become a ________
RBC deformability lies in its shape, but also the organization of the proteins that make up the membrane
These proteins are on the cytoplasmic side of the membrane
List the proteins and their function:
Spectrin: heterodimer alpha or beta subunits that wound around each other → looks like strings
Actin and Band 4:1: bind at the ends of Spectrin dimers and can connect multiple of them
Ankyrin and Band 4.2 anchor Spectrin to the membrane
Spectrin is the cytoskeleton of the membrane and are the ones responsible for altering shape when the cell is subjected to mechanical stress
Mature RBC’s cannot synthesize new membrane proteins or lipids to use for glutathione detoxification
Defect in these membrane proteins can result in hemolytic anemia
When RBC’s lose their deformability, they can lyse in response to stress, get trapped and destroyed or be malformed and become a spherocytes
Hematopoesis
All cell lineages descended from _____________ _______ cells found in ______ __________
The population of hematopoietic stem cells is ___ per ____ bone marrow cells
RBC’s come from the same lineage as ________ and their shared characteristic is that they lack a _________
All cell lineages descended from pluripotent stem cells found in bone marrow
The population of hematopoietic stem cells is 1 per 105 bone marrow cells
RBC’s come from the same lineage as platelets and their shared characteristic is that they lack a nucleus
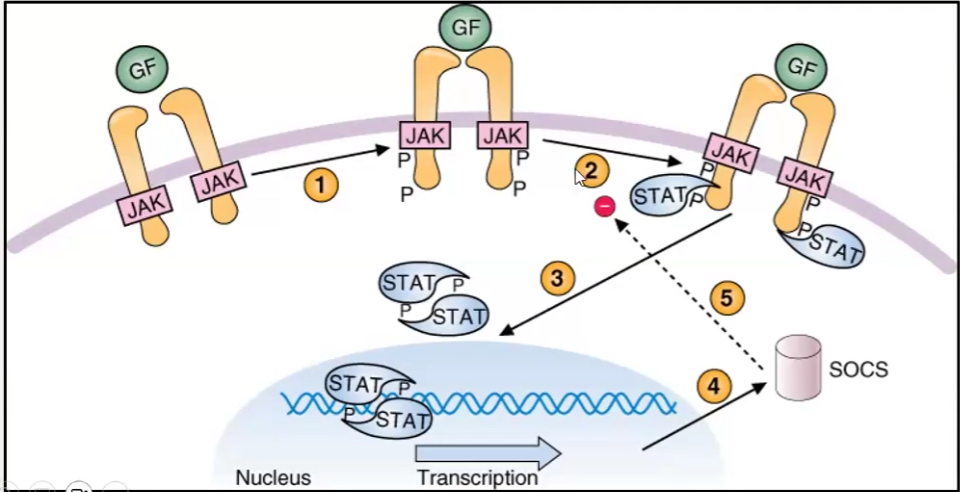
Hematopoiesis Cytokines
What cells support the development of progenitor cells?
How do they support?
Stromal cells: fibroblasts, endothelial cells, adipocytes and macrophages
Things done for support:
Secrete Growth Factors
Growth Factors are recognized by Cytokine receptors and cause receptor aggregation
JAK’s phosphorylate cytokine receptor, making it active
STAT proteins bind to activated receptor and are phosphorylated to initatiate gene transcription
SOCS (silencer) inhibits this mechanism
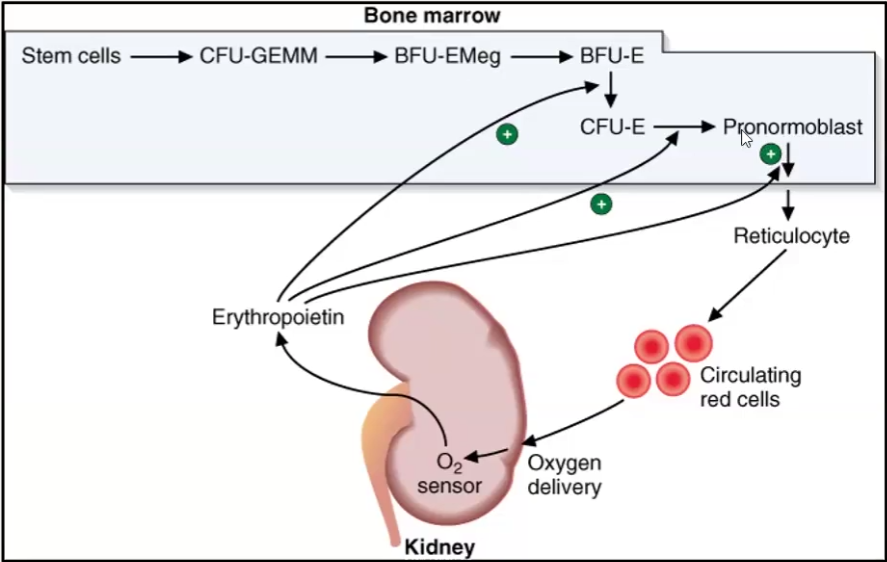
Erythropoiesis
RBC production is regulated by the ______ of oxygen delivery to tissues
In response to reduced tissue oxygenation, the _________ releases hormone called ___________ that stimulates ____________ and replication of ___________ progenitors
Describe the order of maturation of RBCs
RBC production is regulated by the demand of oxygen delivery to tissues
In response to reduced tissue oxygenation, the _________ releases hormone called ___________ that stimulates ____________ and replication of ___________ progenitors
Describe the order of maturation of RBCs:
Stem cell
Mixed Myeloid Progenitor Cell (CFU-GEMM) → gives rise to granulocytes megakaryotes and monocytes
BFU-E (burst forming unit-erythroid)
CFU-E (colony-forming unit-erythroid)
Pronormoblast → first recognizable RBC precursor
Reticulocyte → forms after 4 rounds of division and still has organelles
RBC → no organelles
Anemia
When hemoglobin concentration falls below normal values, the patient is classified as _______
Anemias can be classified by cell sizes: what are the size classes?
Anemias can also be classified in hemoglobin concentration, what are the concentration classes?
When hemoglobin concentration falls below normal values, the patient is classified as anemic
Anemias can be classified by cell sizes: what are the size classes?
Normal → Normocytic
Small → Microcytic
Large → Macrocytic
Anemias can also be classified in hemoglobin concentration, what are the concentration classes?
Normal → Normochromic
Low → Hypochromic
Types of Anemia
Types of Nutritional Anemias
Causes of Hemolytic Anemia
Regular Anemias
Microcytic and Hypochromic → impaired hemoglobin synthesis → iron deficiency, thalassemia, lead poisoning
Macrocytic, normochromic → Impaired DNA synthesis → B12 deficiency or folic acid deficiency, erythroleukemia
Normocytic. normochromic → RBC loss → acute bleeding, sickle cell disease
Nutritional Anemias
Iron deficiency → Smaller (Microcytic) and Paler (Hypochromic)
Vitamin B12 or Folate deficiency → Macrocytic/Megaloblastic Anemia
These nutrients are needed for DNA synthesis
Causes bigger and lesser blood cells produced because they cant divide
Hemolytic Anemias are due to deficiency in the following enzymes:
Pyruvate kinase
G6P dehydrogenase