fungal infections
1/94
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
95 Terms
What are fungi?
Fungi are eukaryotic, and obtain their nutrition from their environment. They occur worldwide, and may be environmental, commensal or pathogenic.
Non-photosynthetic (cannot generate their own food) not autotrophs
Obtain nutrients by absorption (secretion of digestive enzymes)
Structural features of fungi -celll membranes and cell walls
Fungi contain chitin in their cell walls (polymer of N-acetylglucosamine)
Fungi contain ergosterol in their plasma membrane
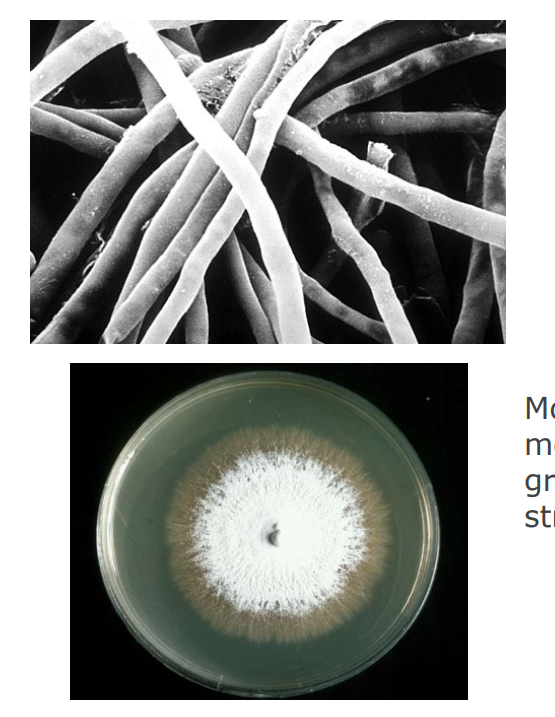
hyphae structural features - mycelium
Sometimes comprised of a mycelium: a large mass of hyphae (singular: hypha) Hyphae: structures produced by apical extension which have parallel sides

Features of human fungal pathogens 4
1. Growth at 37 degrees - human core temperature but Majority of fungi cannot survive, prefer 18-34 C
2. Ability to avoid/resist immune clearance • Required for persistence in the host
3. Lysis of human tissue and absorption of products • Acquisition of nutrients is essential
4. Locomotion through or around host barriers • Dissemination through the host
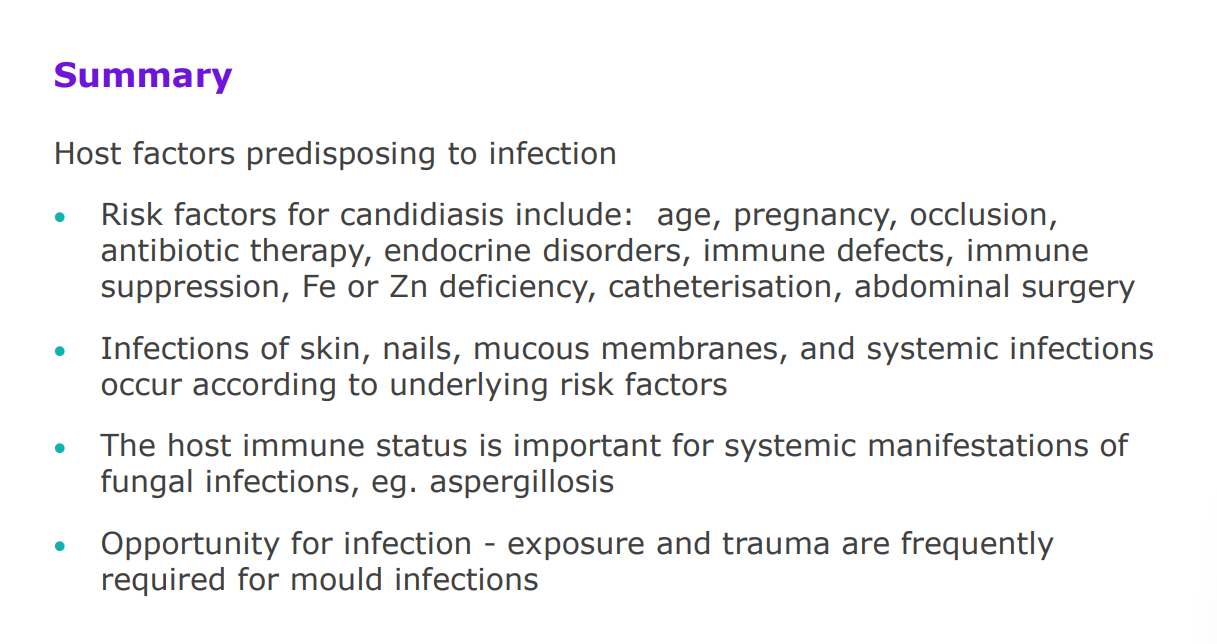
Factors which predispose to fungal infection
Age (infancy and elderly)
endocrine disorders - diabetes
Defects in cell-mediated immunity
Cancer treatment (chemotherapy)
Drug addiction
Use of antibiotics, corticosteroids, immunosuppression
Use of medical plastics (especially intravenous catheters: biofilms)
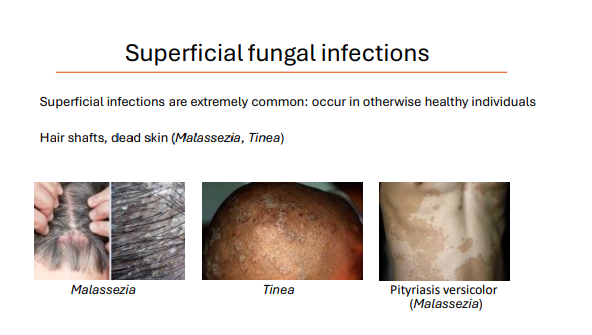
Superficial fungal infections - hair shafts and dead skin
Superficial infections are extremely common: occur in otherwise healthy individuals
Malassezia
Pityriasis versicolor (Malassezia)
tinea
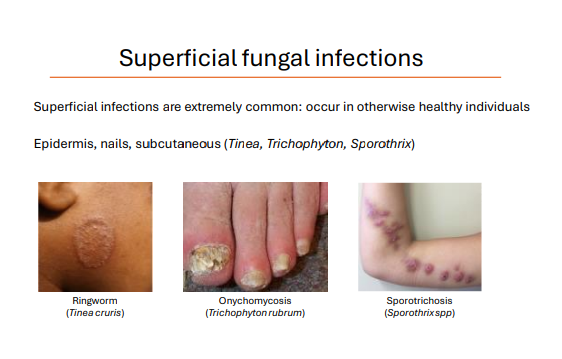
Superficial fungal infections - nails, epidermis, subcutaneous
Superficial infections are extremely common: occur in otherwise healthy individuals
Ringworm (Tinea cruris)
Onychomycosis (Trichophyton rubrum)
Sporotrichosis (Sporothrixspp)
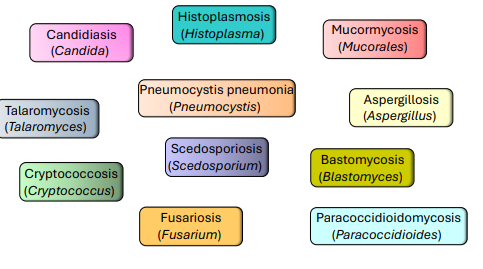
Fungal diseases of the immunocompromised
Most fungal pathogens cannot cause serious disease in immunocompetent people
immunocompromised examples
Use of corticosteroid inhalers
Chemotherapy
Solid organ transplants
Low CD4+ cell count (HIV/AIDS)
Neutropenia - low neutrophil count
Systemic diseases in the immunocompromised
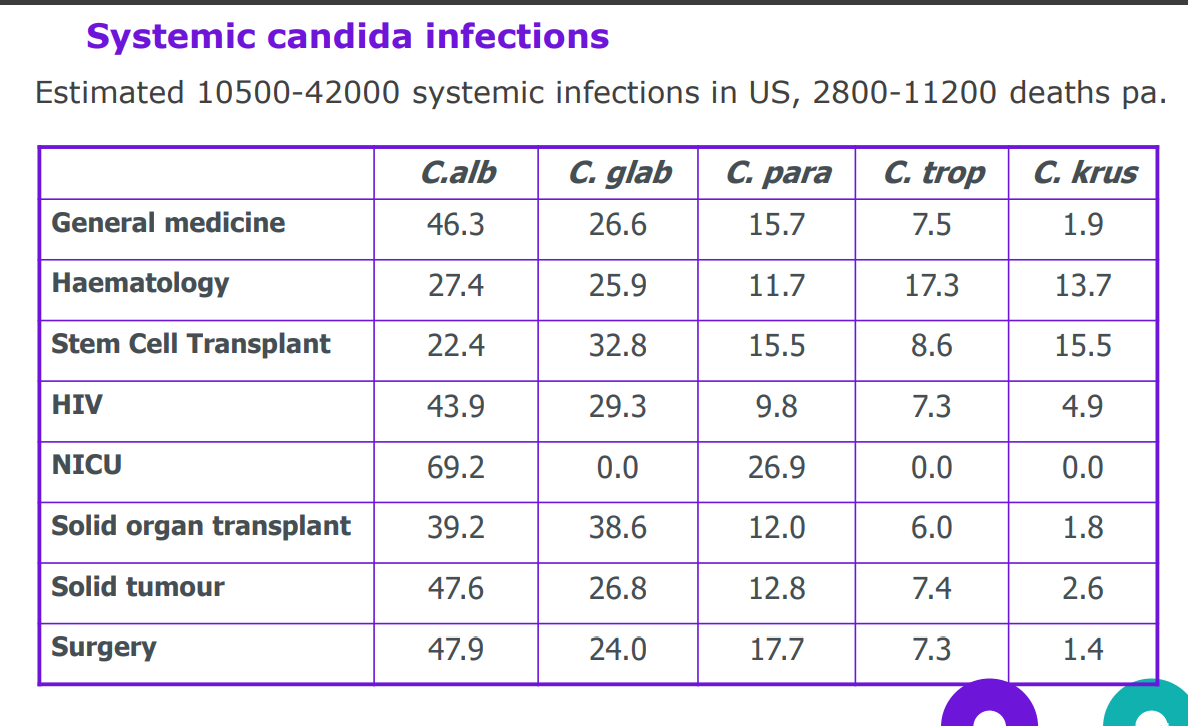
candida albicans
Yeast: approx 60% carriage rate in the human population
Can be commensal (typically GI tract) or pathogenic
200,000 deaths and >150 million mucosal infections annually
50% of HIV and 90% of AIDS patients: oral infections
75% of all healthy women: vaginal candidiasis - can cause disaese in healthy people
Systemic infections can occur in immunocompromised individuals and are often fatal
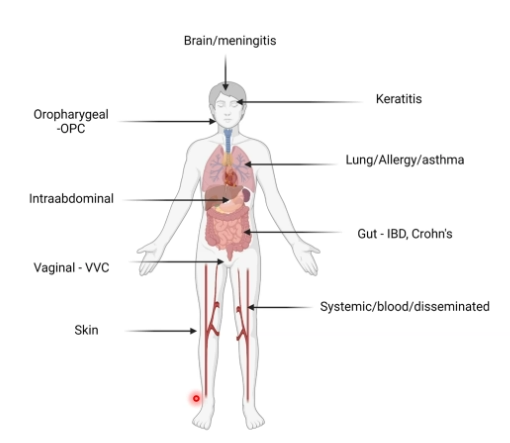
Candida infections target all tissues and organs
Candidiasis (i.e., albicans, glabrata, auris)
Caused by Candida species (i.e., albicans, glabrata, auris)
Synonymous with mucosal infections (e.g., oral thrush)
C. auris is highly resistant to antifungal therapy
candidiasis
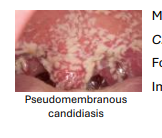
- Pseudomembranous candidiasis
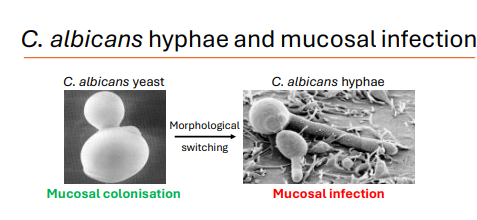
Morphological switching facilitates C. albicans infection C. albicans secretes a range of virulence factors
Forms biofilms readily
Immunosuppression is a strong predisposing factor to candidiasis
candida infections target all tissues and organs
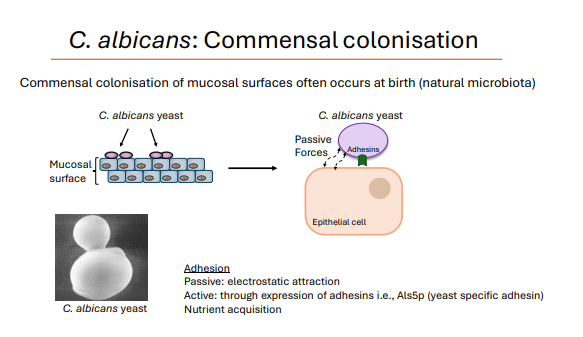
C. albicans: Commensal colonisation
Commensal colonisation of mucosal surfaces often occurs at birth (natural microbiota)
Adhesion Passive: electrostatic attraction
Active: through expression of adhesins i.e., Als5p (yeast specific adhesin)
Nutrient acquisition
C. albicans morphological switching
under certain conditions - it can change morphology - eg immune suppression
Defective immunity:
Fungal overgrowth
Yeast-to-hypha transition (morphological switching)
Tissue invasion
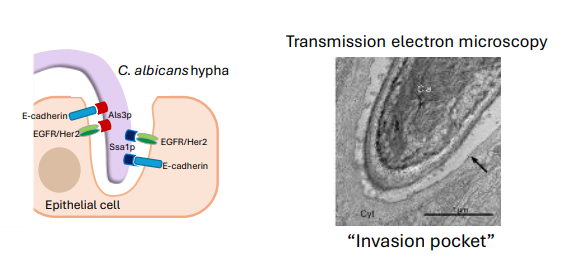
how do C. albicans hyphae create tissue damage?
Create an “invasion pocket”
Damage cells and tissues by secreting virulence factors
Breach mucosal barriers and invade underlying tissues
C. albicans hyphal invasion pocket formation 2 options
Active penetration of hyphae (fungus driven) - tugor pressure pushes through the tissue
Receptor-induced endocytosis (host driven)
C. albicans virulence factors
C. albicans hyphae secrete virulence factors to facilitate pathogenicity
Lipases/Phospholipases (lipids)
Secreted Aspartyl Proteinases (proteins)
Candidalysin: Cytolytic peptide toxin (damages tissues and activates immune responses)
Oral manifestations of candidiasis
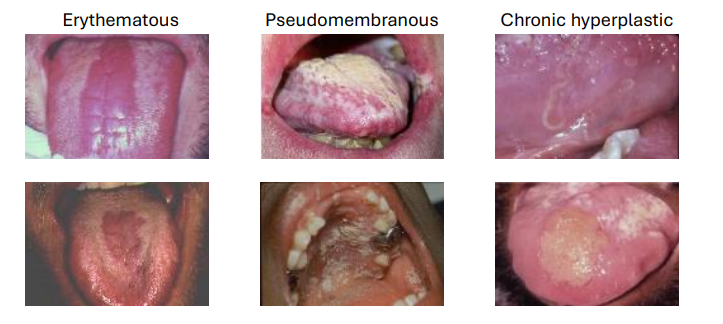
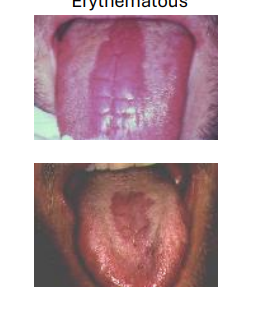
Erythematous candidiasis

pseudomembranous candidiasis
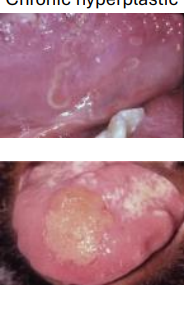
chronic hyperplasic candidiasis

angular cheilitis - candidiasis
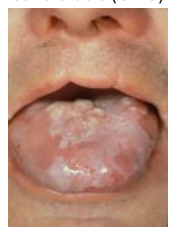
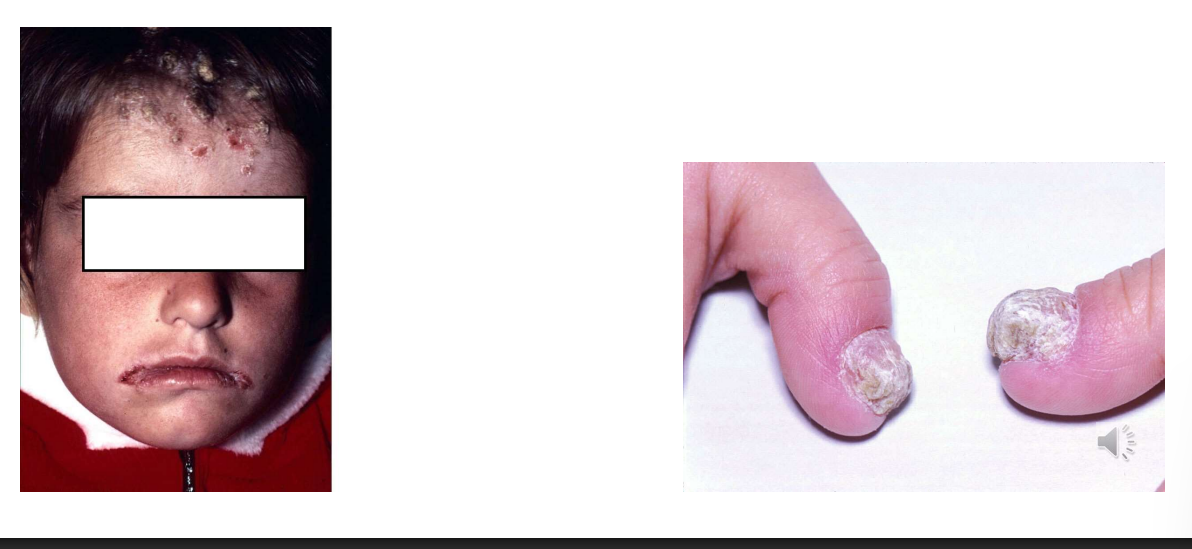
Chronic mucocutaneous candidiasis CMC
Genetic predisposition (mutations which cause a defective T-helper 17 (Th17) immune response) Infection of the nails is also common with CMC
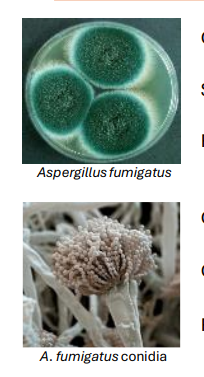
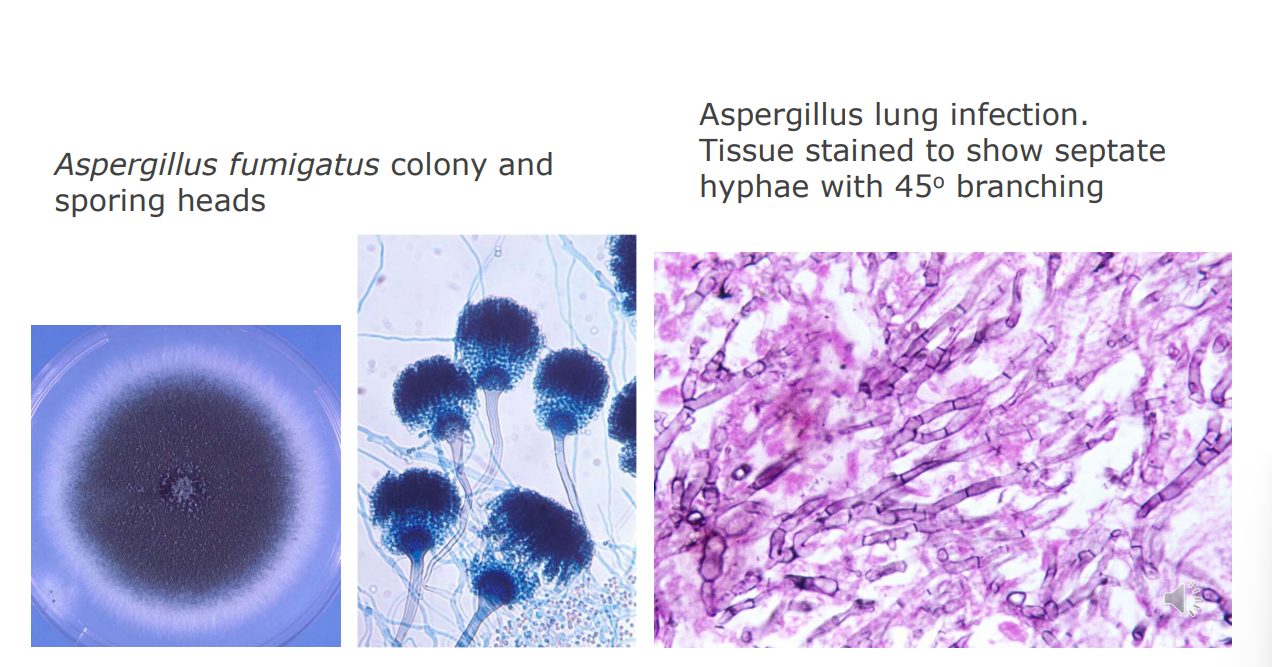
Invasive Aspergillosis (IA) - BACKGROUND
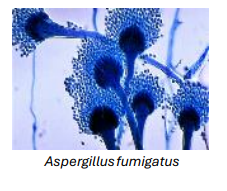
Caused by Aspergillus species (i.e., fumigatus, flavus)
Soil-dwelling saprophytic mould (EXOGENOUS )
Releases conidia/spores (spores; 2–3 μm) into the air
Conidia are inhaled deep into the lung - respiratory epithelium
Conidial swelling, germination, and hyphal growth
Respiratory infections in patients with compromised immunity
Invasive Aspergillosis (IA) - CLINICAL FEATURES
Growth of Aspergillus in the lung - big as a tangerine
Physical obstruction
Secretion of hydrolases (proteases, phospholipases)
Production of mycotoxins: secondary metabolites - bad impacts on the human body
Gliotoxin (detectable in serum of IA patients) → Inhibits neutrophil/macrophage function
Severe infections can become systemic
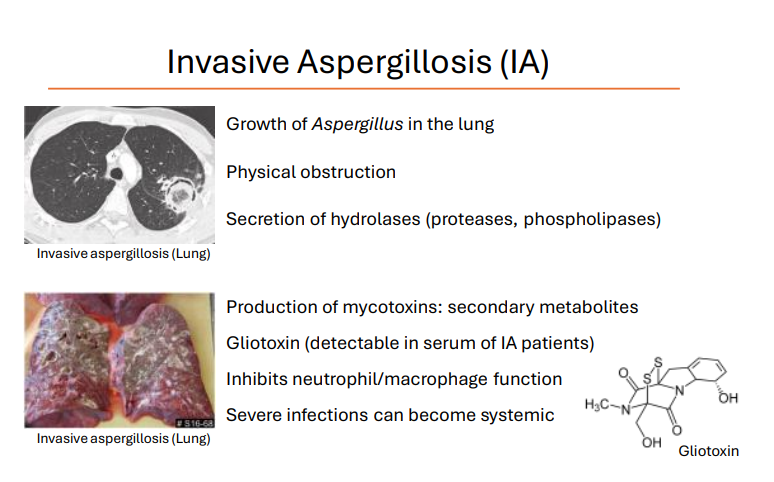
Gliotoxin
(detectable in serum of IA patients) → Inhibits neutrophil/macrophage function
Allergic Bronchopulmonary Aspergillosis (ABPA)
immune-mediated reaction against A. fumigatus antigens
Hypersensitivity following colonisation of lung - immune mediated
ABPA most commonly complicates the course of patients with asthma and cystic fibrosis
Cutaneous hypersensitivity to A. fumigatus antigen, elevated IgE
Blood and sputum eosinophilia (overproduction)
lower infection →Bronchiectasis (widening of airways, persistent cough, phlegm)
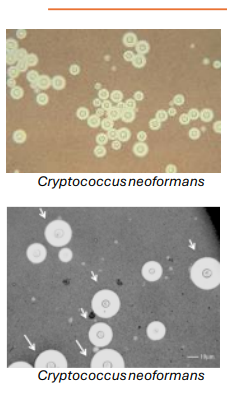
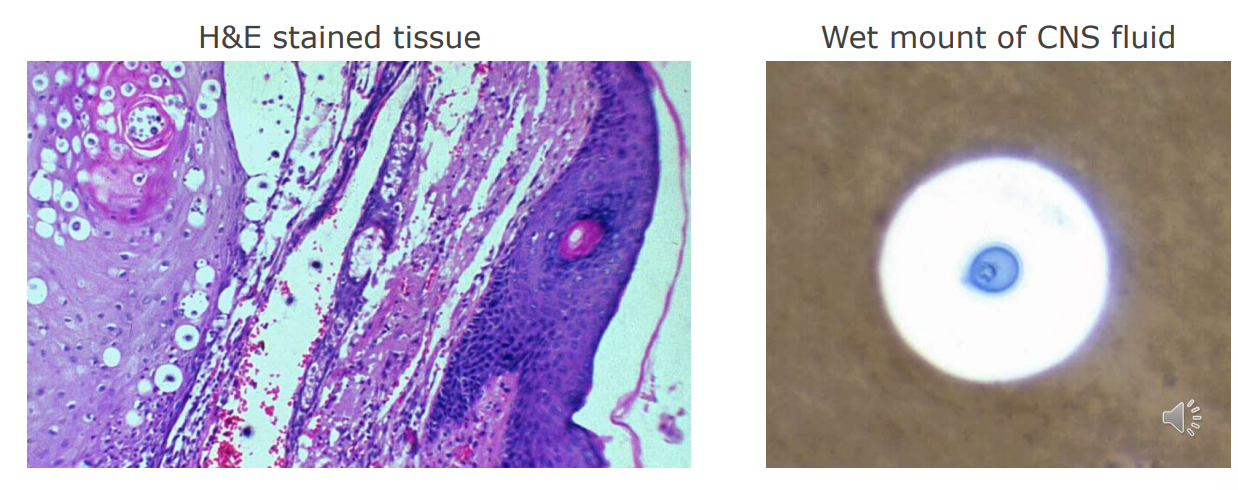
Cryptococcosis
Caused by Cryptococcus species (i.e., neoformans, gattii)
Found in soil, pigeon droppings (yeasts are inhaled)
Thick polysaccharide capsule (reduces phagocytosis)
Cryptococcus can persist within phagocytes
Diverse morphologies: titan cells- big (arrows) – but no hyphae
Infects the lungs and central nervous system (brain/spinal cord)
Cryptococcosis - lung infections
Respiratory distress
Pneumonia-like symptoms
Dissemination to the brain
Cryptococcosis - brain infection
Brain infection (Cryptococcal meningitis):
Acquired from the lung
Fungus crosses the blood-brain barrier
Headache, sensitivity to light, nausea, confusion/behavioural changes

Pneumocystis pneumonia
Caused by Pneumocystis jirovecii
Causes lung infections (fever, shortness of breath, hypoxemia, non-productive cough)
Associated with severe immunodeficiency AIDS-defining disease in USA (CDC, 1981)
Incidence of Pneumocystis pneumonia is reduced with HAART therapy for HIV/AIDS (not always available)
Also occurs with solid organ transplantation/use of corticosteroids)
Several aspects of pathogenesis are poorly understood
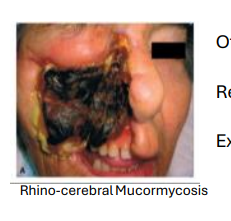
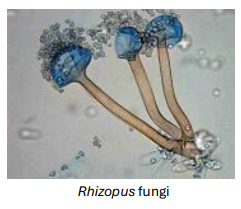
Mucormycosis
Caused by fungi in the phylogenetic order Mucorales
Common examples include Rhizopus delemar, R. oryzae
Predisposing factors include:
Diabetic ketoacidosis (elevated ketones in blood)
Neutropenia (low neutrophil counts)
Mucormycosis can be:
Cutaneous
Rhino-orbital/Cerebral
Pulmonary/systemic

Rhino-cerebral mucormycosis
Often has life-changing impact
Systemic mucormycosis has a mortality rate of ~90%
Requires surgical intervention/reconstruction
Extensive antifungal therapy
Covid-19-Associated Mucormycosis
in patients who have had covid - 2021
Mucoricin
Extremely stable protein toxin
Associated with, and shed from R. delemar hyphae
Mucoricin causes:
Organ damage
Necrosis (ribosome inactivation: depurination of ribosomal RNA)
Haemorrhage and vascular leakage
Immune cell infiltration
all subsequent cards are from last years lecture
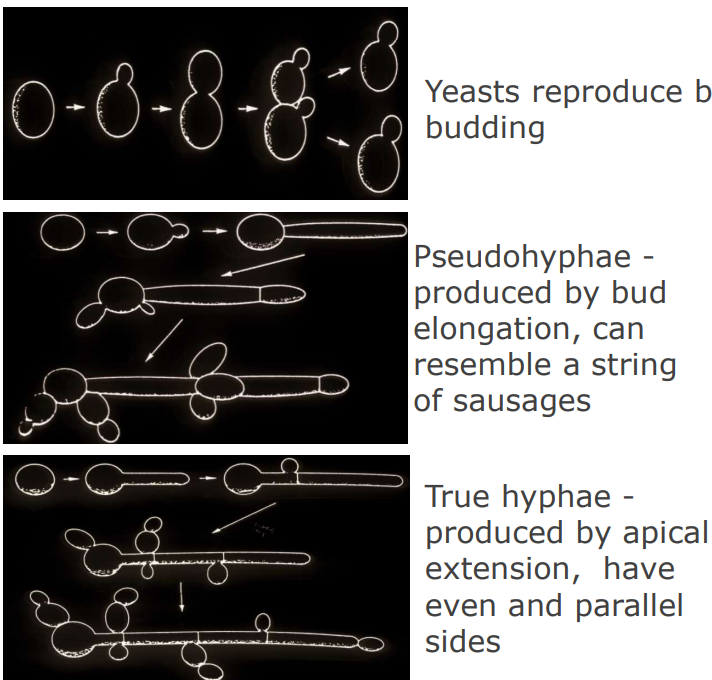
the main characteristics of yeast are 3
unicellular
reproduce by budding
some may produce hyphae and pseudohyphae
what are the main characteristics of moulds ? 3
multicellular - linked
reproduce using specialized spore structures
produce hyphae
what are the structures produced by yeasts?
buds
pseudo hyphae
true hyphae
Pseudohyphae
yeasts - Pseudohyphae - produced by bud elongation, can resemble a string of sausages
true hyphae
yeasts - True hyphae - produced by apical extension, have even and parallel sides
how can you describe the colonies yeast form?
what do moulds produce?
true hyphae
Mould hyphae form a colony on solid media that is round, sub-surface growth occurs and special spore structures may be on the surface (agar) - spores - distributed by air or water
It is possible to distinguish mould and yeast infections in tissue by microscopy (example using fluorescence stain)
in moulds - hyphae are true and parallel and regularly septate
in candida infected skin - budding yeasts, pseudohyphae, true hyphae
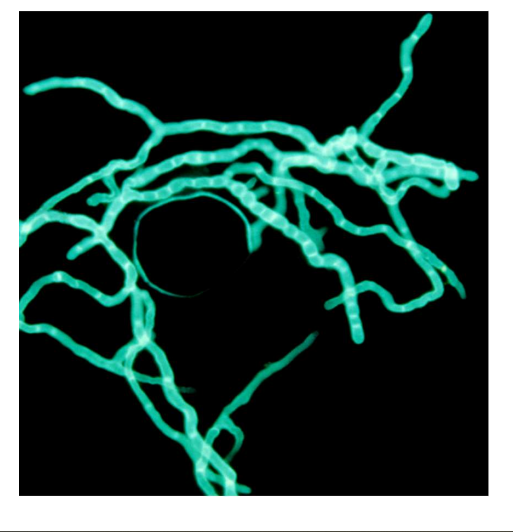
mould infection
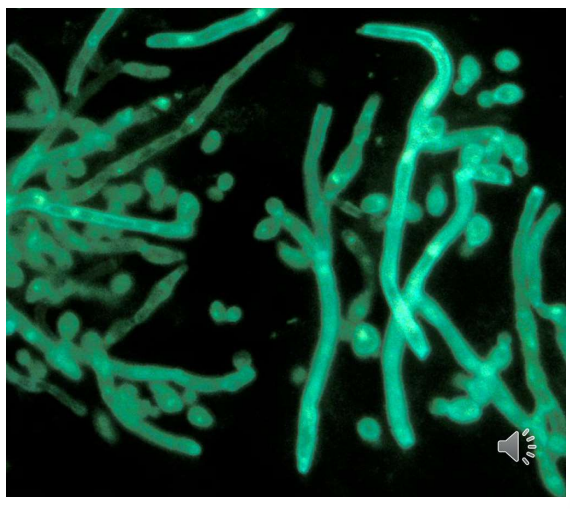
yeast infection
are there any commensal yeasts?
yes
Candida albicans - GI tract, oral
Other Candida species may be found in the GI
Malassezia - Skin
are there any commensal moulds?
no
Factors predisposing to candidiasis 8
Age - infancy, elderly
Endocrine disorders
Defects in cell mediated immunity
Cancer
Drug addiction
Drug therapy -antibiotics (removes competition), corticosteroids, immunosuppression
Surgery
Intravenous catheters - biofilm formation
Candidiasis
Candida species are commensal to GI tract, most infections arise from endogenous flora
Commonest causes: Candida albicans C. glabrata, C. tropicalis, C. parapsilosis, C. krusei
Occasionally exogenous sources implicated - eg. hospital outbreaks, and the commonest cause of these is C. albicans.
Latest nosocomial problem is Candida auris. Colonises readily, persists in environment, highly resistant to antifungals

candidiasis - Acute pseudomembranous, detachable plaques

candidiasis - Chronic pseudomembranous, AIDS persistent

candidiasis - Chronic mucocutaneous candidiasis
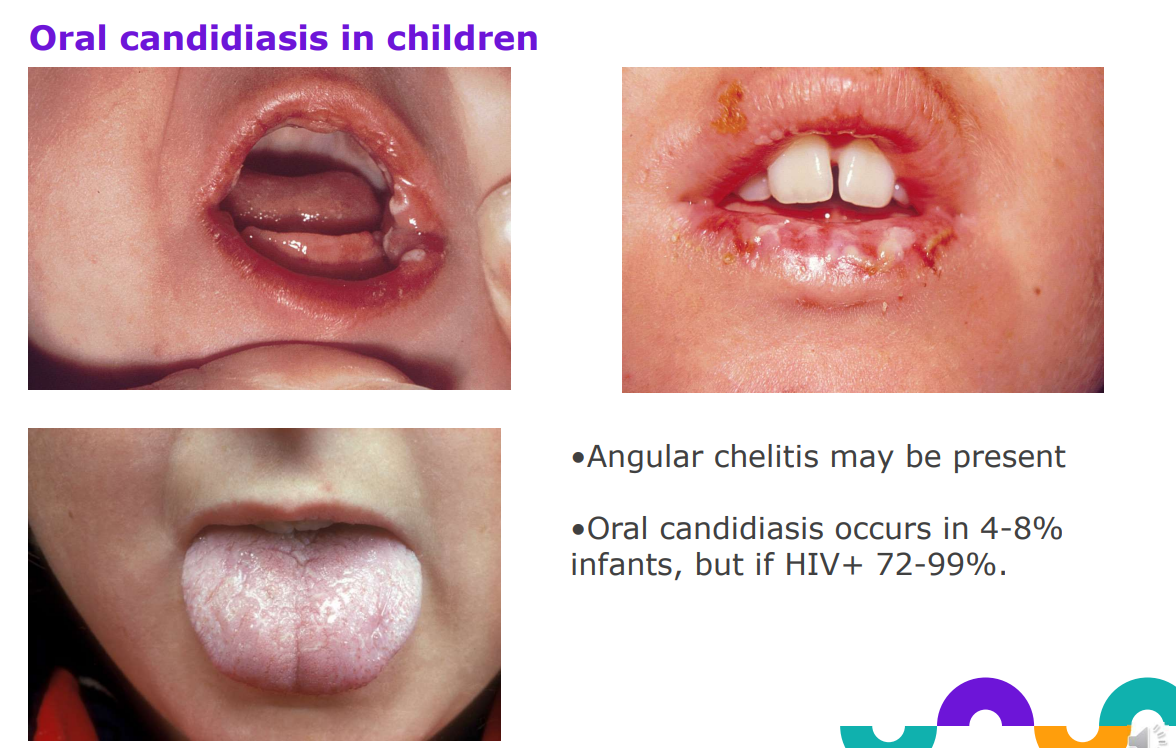
Oral candidiasis in children
Angular chelitis - corner infection may be present
Oral candidiasis occurs in 4-8% infants, but if HIV+ 72-99%.
Superficial infections caused by Candida albicans

predisposing factors for intertrigo candidiasis
obesity and diabetes


predisposing factors for Fingerweb / finger nail candidiasis
occlusion and wetness, carriage of candida.
Candidiasis - nappy dermatitis
Buttocks, perianal, groin.
Erythema, scaling, satellite lesions
1o or 2o invader?
Association with faecal carriage of C. albicans - abrasion, urine and faeces → candida can get in

Chronic mucocutaneous candidiasis
Presents in childhood or infancy, recurrent oral, skin, nail infection.
Skin lesions crusted on face and scalp - “candida granuloma”
Immunological abnormalities involved, not characterised CMC may be inherited, associated with hypoparathyroidism or hypoadrenalism, hypothyroidism, or idiopathic
Systemic candidiasis - predisposing factors
age
antibiotic treatment
abdominal surgery
immune suppression
catherisation
prolonged hospitalization
systemic candidiasis - sites affected
blood, lungs and internal organs, skin
systemic candidiasis - endogenous and exogenous sources
C.albicans is an opportunist
Endogenous source– resulting from predisposing factors
Exogenous source – outbreaks can occur in wards with severely debilitated hosts, uncommon
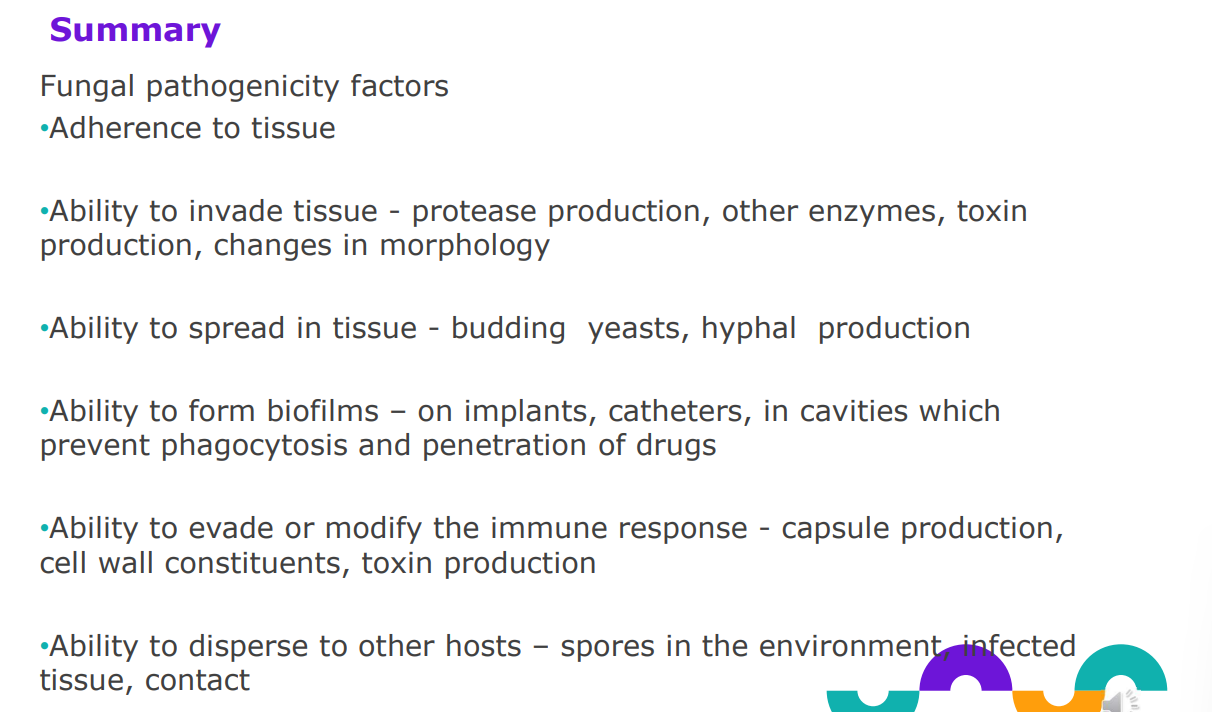
How does Candida albicans cause infection? 7
ability to adapt to changes in the environment
ability to adhere to different surfaces
production of destructive enzymes
Changes in cellular morphology
Production of biofilms
Evasion of host defence mechanisms
Toxin production
candida - ability to adapt to different environments
eg. pH. Sites include mouth, GI, vagina, skin
candida - Ability to adhere to different surfaces
Surface molecules bind to: iC3b, fibrinogen, fibronectin, laminin, epithelial cells , bacterial coaggregation with Streptococci and Fusobacteriumspecies
candida - Production of destructive enzymes
Secreted aspartyl proteinases, phospholipases, hyaluronidase, degrade extracellular matrix proteins, etc enabling invasion
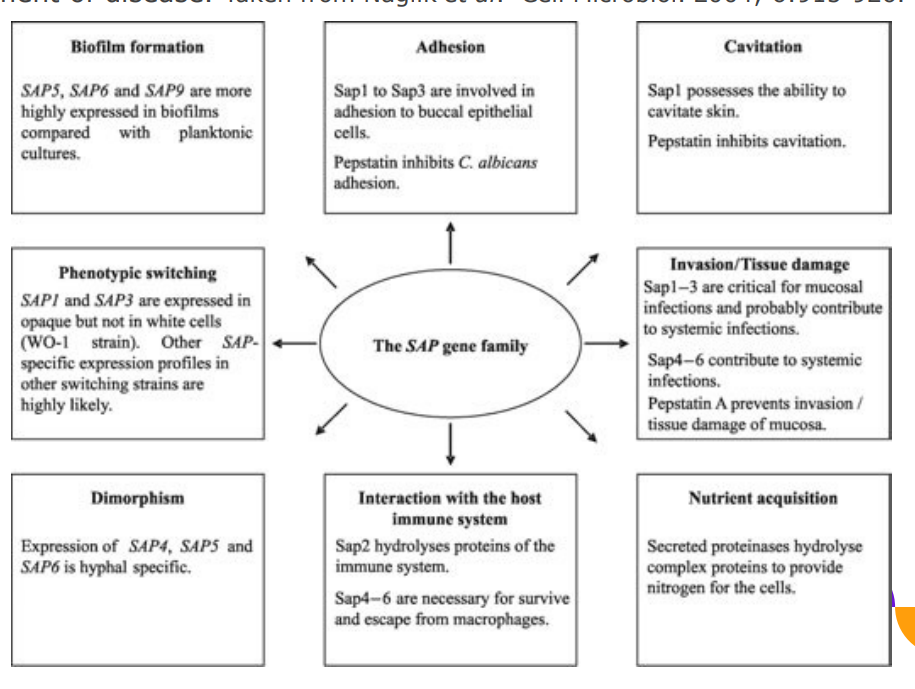
candida pathogenicity - Secretory aspartyl proteases SAP
Secretory aspartyl proteses (SAPs) have roles in adherence, invasion and development of disease.
can turn on different proteases depending on what theyre doing
candida - changes in cellular morphology
Yeast, hyphae, pseudohyphae
candida - production of biofilms
Offers protection from environment, phagocytosis, and antifungals
candida - evasion of host defence mechanisms
Block oxygen radical production and degranulation of PMN, kill monocytes. Cell wall components may have immunomodulatory effects, may stimulate cytokine release, may activate complement cascade
candida - toxin production
Candidalysin is a cytolytic peptide toxin secreted by C. albicans during hyphal invasion. Damages tissue and activates the immune response
Cryptococcosis
A chronic, subacute to acute pulmonary infection resulting from inhalation of cryptococcus yeasts.
On dissemination, the yeast shows a predilection for the CNS and cryptococcal meningitis occurs. Systemic spread may result in skin lesions, and infection of bone and internal organs may occur
Cryptococcosis - distribution, risk factors and causative organism
Distribution - worldwide especially associated with bird droppings (eg. pidgeon)
Causative organism Cryptococcus neoformans
Risk factors - HIV/AIDS
Cryptococcus gattii
and related species can also cause infection of mostly immune competent hosts. This species is associated with trees and soil and is endemic to certain regions. eg. Vancouver Island, Canada
Cryptococcus infection - yeast or mould?
Cryptococcus exists only in the yeast form, no hyphae produced.
cryptococcosis - major virulence factor
Major virulence factor: capsule is protective, prevents phagocytosis. melanin is immunomodulatory
capsuled microbes likely cause meningitis
Mould infections
No commensal mould to the human body.
Infections always exogenously acquired.
examples showing different pathogenicity mechanisms and relationships with the host
Dermatophytes - what is it and the source
mould infection
Common
superficial infection,
sources include human, animal and soil, healthy host
Aspergillus - what is it and what’s the source?
mould infection
Uncommon,
systemic infection
environmental source
immune compromised host or predisposing factors underlie disease
What factors predispose to mould infection? 5
History of trauma to site of infection (cutaneous and subcutaneous)
Host immune status - can determine the extent of disease, duration, outcome
Underlying disease – may influence susceptibility to certain types of infection
Exposure to a source
Portal of entry
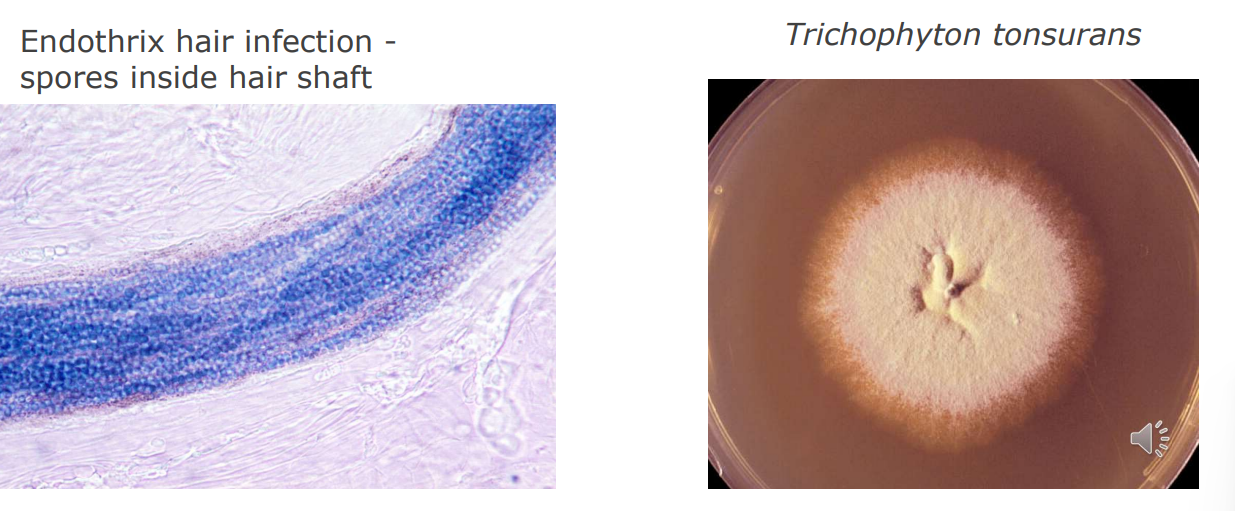
Dermatophyte infections - what is there substrate? ring worms
Dermatophytes are a family of mould/fungi that use keratin as a substrate
Species can infect skin, nail and hair
Clinically dermatophyte infection is referred to as
tinea
Dermatophyte infections- facts
Infections result from contact with a source Affect healthy and immune compromise people
Commonest cause of human mould infection
Commonest cause of skin and nail infection is Trichophyton rubrum.
Species are linked to primary hosts – humans, animals or soil

Dermatophyte infections - Tinea capitis
In UK cities the commonest form is spread anthropophilically - person to person . Clinical presentations may be sub-clinical to kerion. Often fine scaling, mild erythema, patchy alopecia. Hairs break at skin level -black-dot alopecia.
Highly contagious among pre-pubescent children.
Practice good hygiene and disinfect chairs and headrests.
Tinea capitis - risk factors
age – most infections before puberty (mid teens). Uncommon in adults. Sebum production is inhibitory to fungal growth.
contact with infection - relevant history of exposure to source (human, animal, soil)
minor trauma to inoculate - scratching, hair dressing, barbers, sharing hats / towels etc
affects healthy hosts. Not more common in immune compromised hosts, but infections may be more florid
Pathogenicity mechanisms for tinea 6
Adherence: adhesins, enzymes (subtilisin in M. canis), fibrillar projections on fungal cell surface
Invasion: phospholipases, subtilisins, metalloproteinases, carboxyproteinases, serine proteinases etc. Complex process regulated by protein content and pH.
Utilise keratin: proteins in the cornified layers of skin are rich in disulphide bridges. Dermatophytes use a sulphite pump to reduce the disulphide bond in proteins which are then cleaved. Subtilisins and metalloproteasess can digest these proteins, and aminopeptidases and carboxypeptidases digest further to form peptides and amino acids
Manipulation of the immune response - cell wall mannans suppress lymphoproliferative activity → from plants → worse symptoms
Host adaptation - zoophillic species produce more protease than anthropophilic species - less IL-1α was induced by T. rubrum than T. mentagrophytes andT. tonsurans elicits a lower cytokine release from keratinocytes than animal species
Asymptomatic or minor infection that is ignored → increases spread
Aspergillus infections - Aspergillosis
environmental moulds - leaves
Causes systemic disease following inhalation of spores.
Type of disease is determined by host status. Commonest causes: Aspergillus fumigatus, A. flavus, A. nidulans, A. niger, A.terreus.
All are referred to as species complex as each comprises closely related organisms that are only distinguished genetically
Aspergillus infections
Allergic aspergillosis - temporary presence of aspergillus in respiratory tract, healthy host. Agricultural link, or exposure to large nos. spores
Aspergilloma - colonisation of pre-existing cavities (TB), fungal ball in lung, predisposing factors for lung cavitation but may otherwise be healthy
Invasive aspergillosis - pulmonary focus, dissemination possible, immune compromised host
Systemic aspergillosis - lungs, brain, other organs, immune compromised host
Cutaneous aspergillosis
Cutaneous aspergillosis – primary infection due to skin damage (healthy or immune compromised). - secondary manifestation due to disseminated disease.
Risk factors – trauma, neonate, immune compromised host. A. fumigatus, A flavus commonest
A. flavus causes aflatoxicosis due to ingestion of toxin produced in contaminated foods (peanuts), healthy host

Invasive aspergillosis
zygomycosis