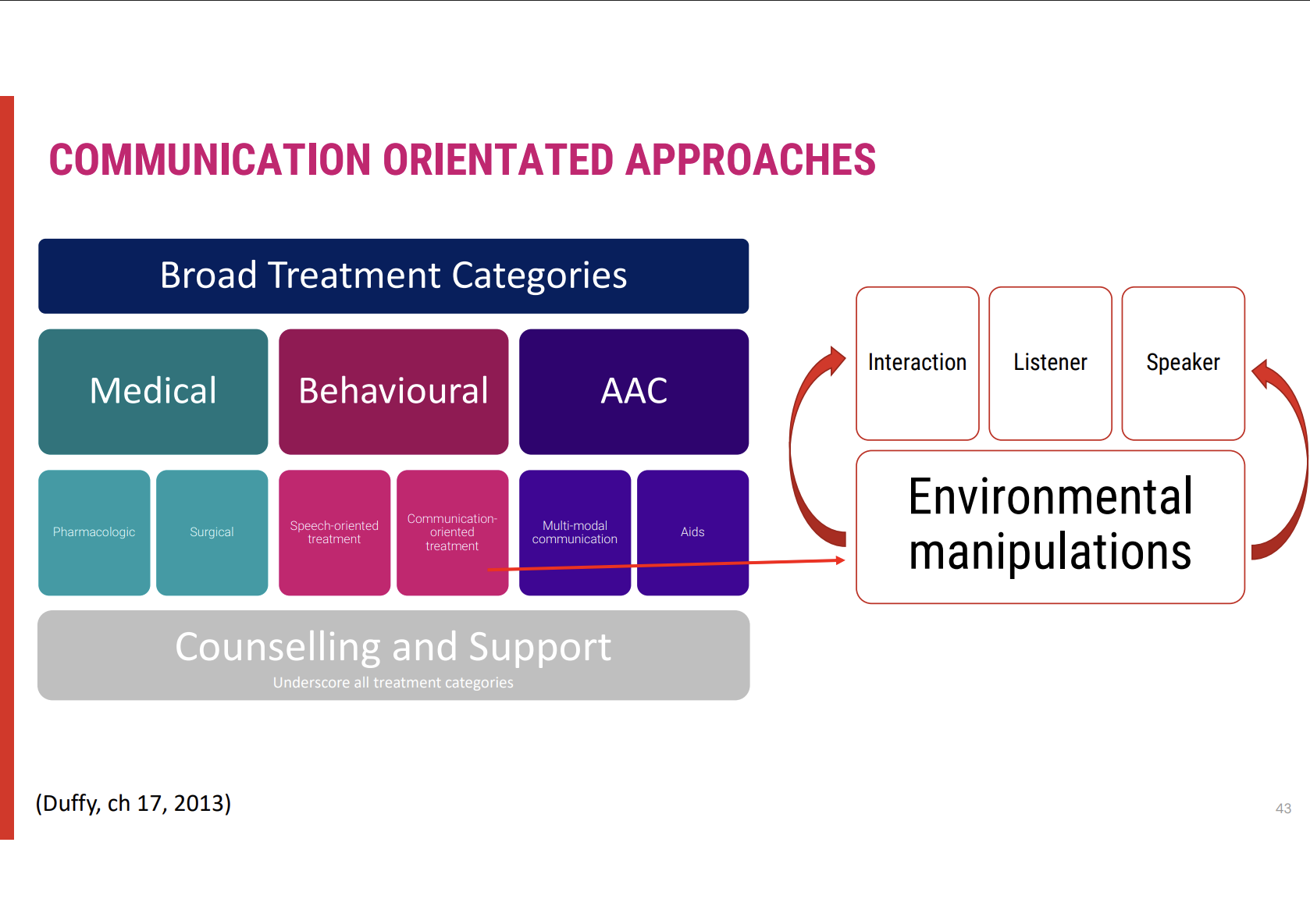
Behavioural Treatment Approaches
1/32
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
33 Terms
Behavioural Management in Motor Speech Disorders
🎯 Goal of Behavioural Management
Maximise communication abilities in individuals with motor speech disorders.
Focuses on speech-oriented and communication-oriented approaches.
🗣 Approaches Based on Severity
Mild impairments: Primarily use speech-oriented approaches to improve articulation, intelligibility, and speech clarity.
Severe impairments: Employ communication-oriented approaches, which may include AAC or compensatory strategies to support communication.
📈 Behavioural Management as Primary Approach
Most common treatment approach for motor speech disorders, adaptable across the spectrum of severity.
Client-Centered Goal Setting in Behavioural Management
🎯 Guiding Factors for Behavioural Approach
Client's goals for therapy are central to determining the appropriate approach.
What is most important to them in relation to communication and overall health?
What are their concerns regarding communication and its impact on daily life?
💬 Collaborative Goal Identification
Through discussions around personal priorities, speech pathologists can collaboratively identify intervention goals that align with the client’s needs and hopes.
Speech-Oriented Approaches: Focus and Goals
Main Focus: Targeting the Motor Speech Disorder
The motor speech disorder itself is the central focus of speech-oriented approaches.
Oromotor examination (OPE) and motor speech evaluation are essential in identifying breakdowns in speech subsystems and setting realistic goals.
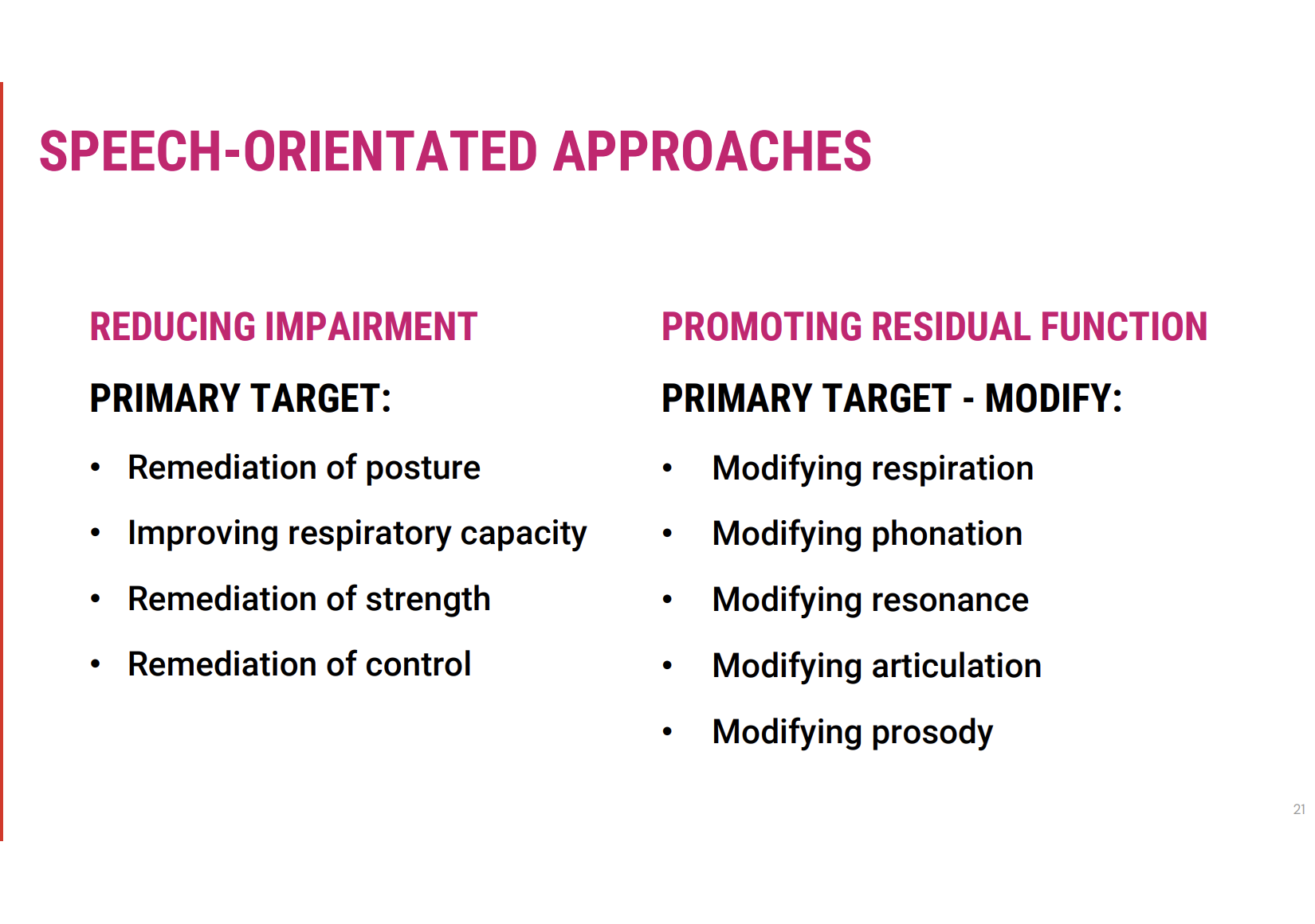
Primary Treatment Goals
Targeting the Impairment
The aim is to reduce the impairment in motor speech to restore function where possible.
Targeting Residual Function
This involves promoting compensatory strategies to make use of any remaining functional speech abilities, without altering the underlying physiology.
Emphasis on Compensation vs. Reduction
Compensation is often prioritised, especially in settings like acute hospitals or inpatient rehab, where quick functional goals are needed.
However, if there is potential to reduce the impairment (e.g., in cases like unilateral upper motor neuron dysarthria following a stroke), restorative goals should also be targeted.
Speech-Oriented Approaches: Detailed Insights
1. Targeting the Impairment: Focus Areas
Reduction of Impairment involves identifying and targeting specific breakdowns in the motor speech systems, which include:
Posture: Improving head and body alignment to support clearer speech.
Respiratory Capacity: Enhancing lung strength and control for better breath support during speech.
Strength and Control: Focus on strengthening oral and facial muscles to improve speech articulation and voice control.
These interventions directly address the domains of respiration, phonation, resonance, articulation, and prosody:
Respiration: Techniques to increase breath support for sustained speech.
Phonation: Targeting vocal cord function to enhance sound production.
Resonance: Modifying speech volume and tone to avoid nasal or breathy speech.
Articulation: Improving clarity of speech through targeted oral motor exercises.
Prosody: Working on intonation and rhythm to restore natural speech patterns.
2. Promoting Residual Function: Modifying Usage
Promoting Residual Function involves adapting the use of remaining functional speech abilities:
No attempt to restore full function, but modifying how the subsystems are used.
For example, in a person with weak respiratory muscles, they may learn to speak more slowly or take strategic pauses to ensure clearer articulation and more efficient communication.
3. Combining Impairment Reduction and Residual Function
Not Mutually Exclusive: Reducing impairment and promoting residual function can complement each other:
Practice and repetition of new speech techniques can not only compensate for lost function but also help regain control in specific motor speech areas.
For instance, a person working on articulation drills to reduce slurring may also naturally increase their control over tongue and lip movements, aiding in clearer speech.
4. Clinical Relevance in Acute Settings
In acute settings like rehabilitation, focusing on compensation may offer immediate functional improvement.
As rehabilitation progresses, there may be greater opportunities to also target and reduce impairments, depending on the individual's recovery potential.
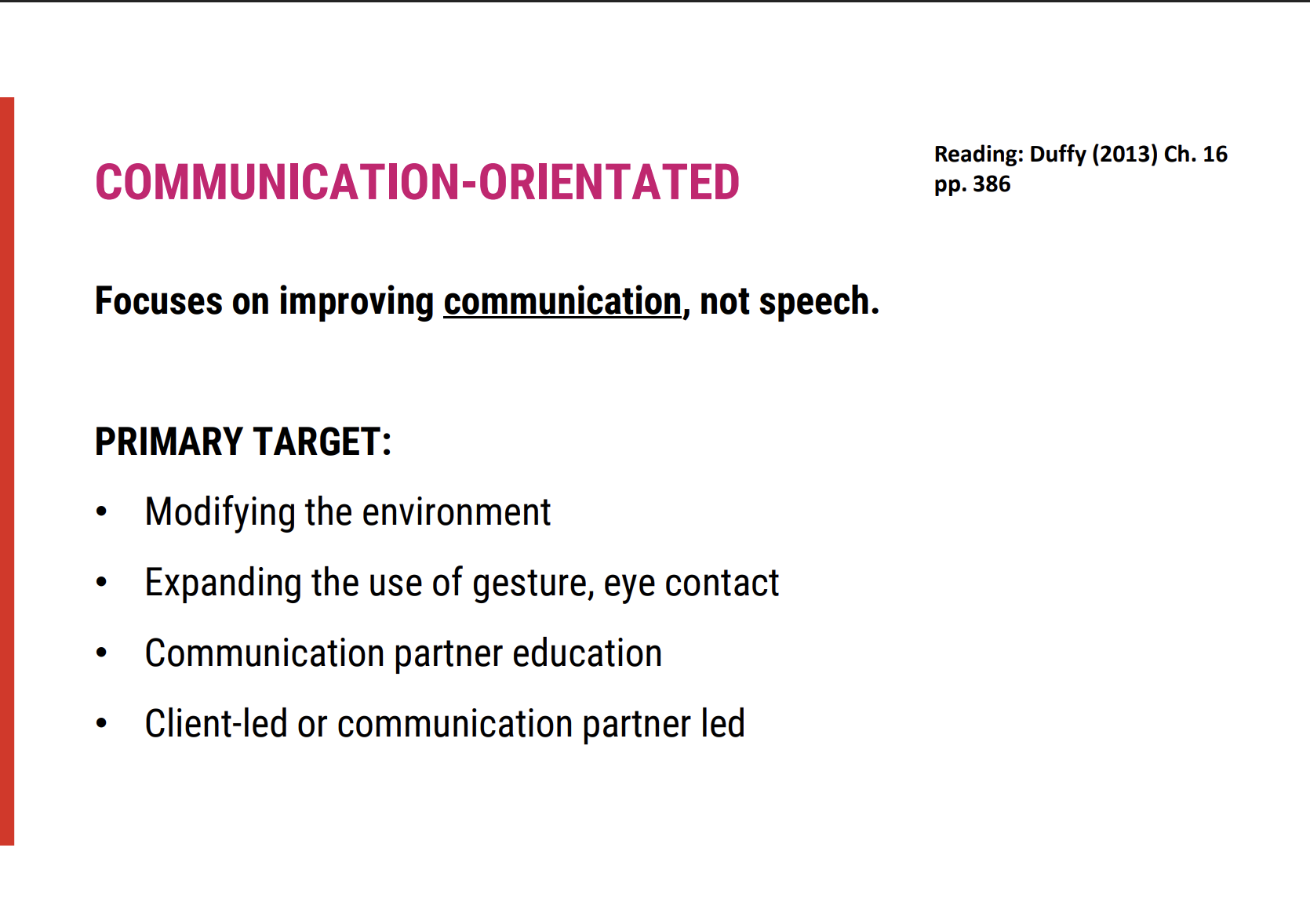
Communication-Oriented Treatment Approach: Detailed Insights
1. Focus on Reducing the Need for Lost Function
Goal: Improve overall communication even if speech mechanisms remain unchanged or continue to deteriorate.
Approach: This strategy does not aim to restore lost speech function but instead focuses on adjustments and adaptations that enhance communication effectiveness.
2. Modifying the Communication Environment
Key Factors to Modify:
Number of Communication Partners: Reducing the number of people involved in conversations to ease communication.
Amount of Noise: Minimising background noise to improve intelligibility.
Physical Distance: Adjusting the distance between the speaker and listener to improve clarity and ease of communication.
3. Enhancing Non-Verbal Communication
Increased Use of Non-Verbal Cues:
Eye Contact: Encouraging the speaker to use eye contact to convey engagement and intention.
Facial Expressions: Promoting the use of facial expressions to enhance understanding, especially in noisy or challenging environments.
Gestures: Encouraging the use of hand gestures or other physical movements to help clarify messages.
4. Teaching Communication Partners
Training Listeners: Educating communication partners about:
Speech Problem Understanding: Helping them understand the nature and cause of the speech disorder.
Preferred Methods: Identifying preferred methods of communication (e.g., visual aids, gestures) that suit the individual in various contexts.
Repairing Communication Breakdowns: Offering strategies for partners to navigate and fix communication issues when they arise (e.g., clarifying misunderstandings or asking for repetitions).
5. Conversation Partner Training
Example of Communication-Oriented Speech Treatment: Training conversation partners to:
Be more patient.
Use appropriate cues (e.g., slow down, focus on key words).
Ensure clarity and mutual understanding in communication, which can be crucial for individuals with significant speech impairments.
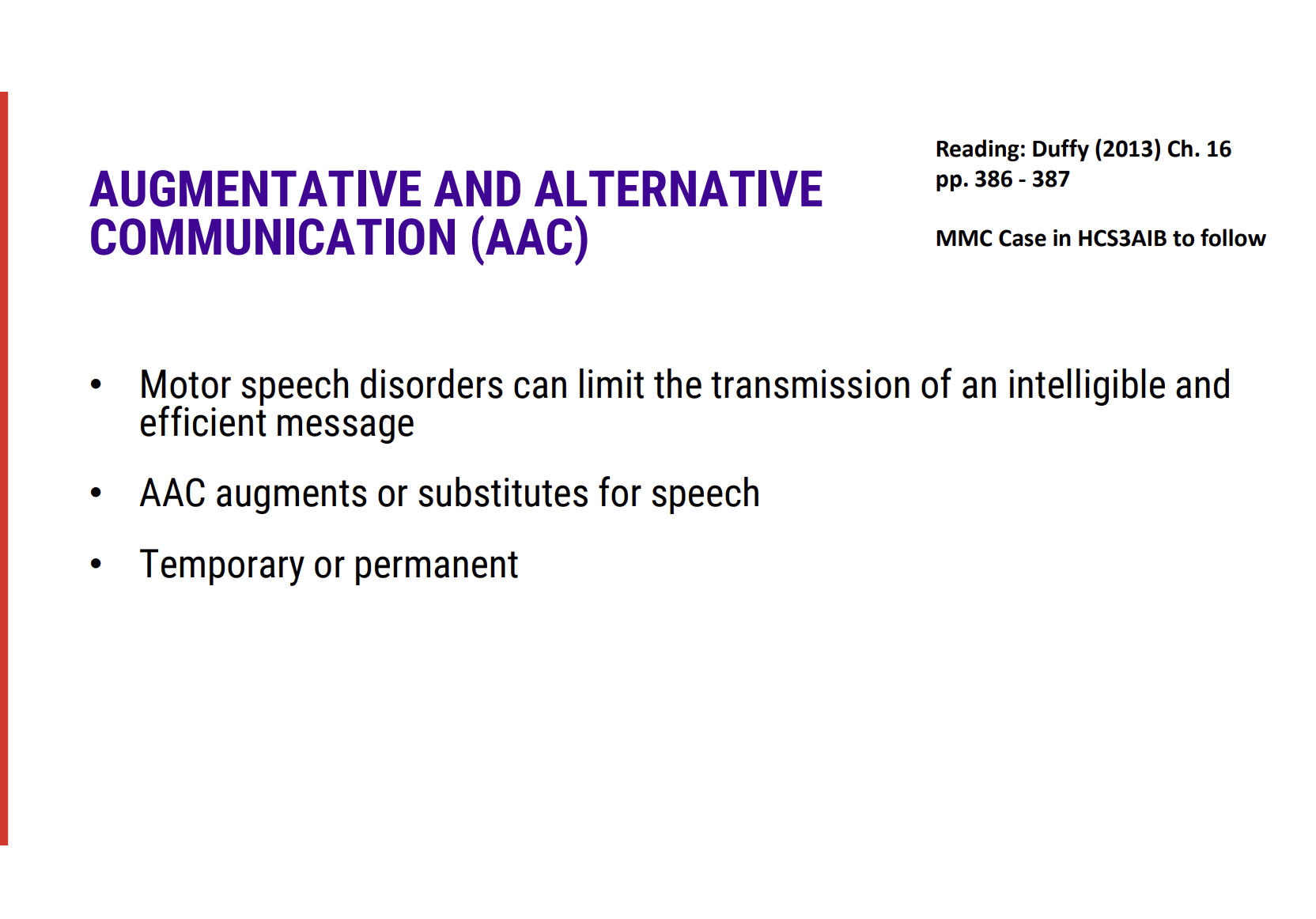
AAC (Augmentative and Alternative Communication) Reminder 📱
Limitations of Motor Speech Disorders: Motor speech disorders can significantly limit speech and gesture transmission, making AAC tools important for communication.
Temporary or Permanent: AAC strategies may be implemented either temporarily or permanently depending on the individual's needs.
Early Introduction: As motor speech deteriorates, it's crucial to introduce AAC strategies early to provide effective communication support
AAC and Motor Speech Disorders
Motor speech disorders can significantly impair an individual's ability to produce clear speech or convey gestures effectively. This often results in difficulties in expressing thoughts and engaging in conversations, making communication challenging for both the individual and their communication partners.
Augmentative and Alternative Communication (AAC) may be needed to supplement or replace speech when it becomes insufficient. The decision to implement AAC could be temporary (for recovery periods, such as after an acute injury) or permanent (in cases of progressive conditions, such as neurodegenerative diseases).
Early introduction of AAC strategies is especially crucial when there is a forecasted decline in speech abilities, such as in progressive disorders like Parkinson's disease or motor neuron disease. Introducing AAC at the right time can help maintain communication and improve quality of life during speech deterioration.
Proactive intervention ensures individuals can adapt more effectively to their evolving communication needs. This allows for smoother transitions to more advanced AAC systems if needed and helps maintain social interactions, participation in daily activities, and overall well-being throughout the course of their condition.
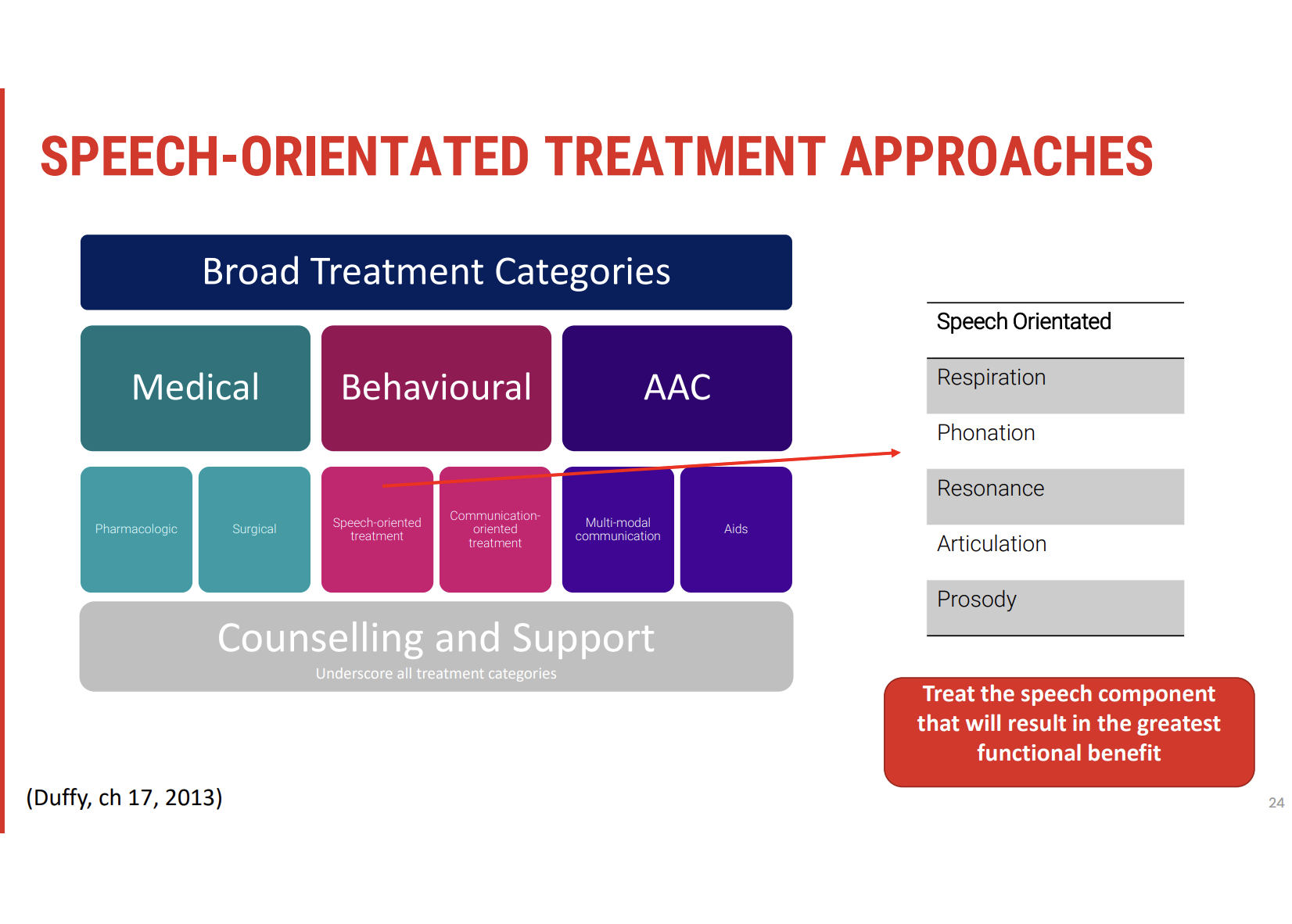
Speech-Oriented Treatment Approaches
When speech-oriented therapy is indicated, the focus shifts to addressing specific breakdowns within the motor speech system. The goal is to restore function and maximize the use of residual abilities to improve speech outcomes.
Key Areas of Breakdown
Respiration
Phonation
Resonance
Articulation
Prosody
Initial Assessment
Oral Motor Examination (OME) and motor speech evaluations are critical for identifying the precise areas of breakdown within these subsystems.
These assessments help determine which areas are most affected and allow for targeted intervention.
Targeting Specific Speech Components
When planning speech-oriented treatment, the focus should be on the area that will provide the greatest functional benefit as quickly as possible.
Alternatively, treatment may aim to provide the greatest support for improvements in other aspects of speech.
This decision is often based on collaborative discussions with the client to identify their priorities, needs, and goals.
Treatment Targets
For each subsystem (e.g. respiration, articulation), specific therapeutic goals are set. This may involve:
Restoring lost function (e.g., improving breathing control for speech production).
Maximizing use of residual function (e.g., using available articulation skills to enhance intelligibility).
Treatment of Respiration Deficits 🫁
Context
The focus is on addressing respiration deficits when they negatively affect speech aspects like phrase length or intelligibility. Key symptoms include:
Short phrases: The person may struggle to complete sentences or thoughts.
Frequent breath breaks: Regularly running out of breath during speech.
Reduced loudness: Difficulty producing strong, clear speech sounds.
Breath voice or harsh-sounding voice: The voice may sound weak or strained.
Treatment Considerations
When respiration deficits impact communication, therapy should focus on improving breath control, strengthening respiratory muscles, and optimizing airflow for speech production. This might involve:
Breathing exercises: To increase control over exhalation and improve phrase length.
Postural adjustments: Improving posture for optimal lung expansion and air support.
Inspiratory muscle training: To enhance breath support for louder and more sustained speech.
Voice therapy: To address breathiness or harsh voice quality, improving resonance and strength.
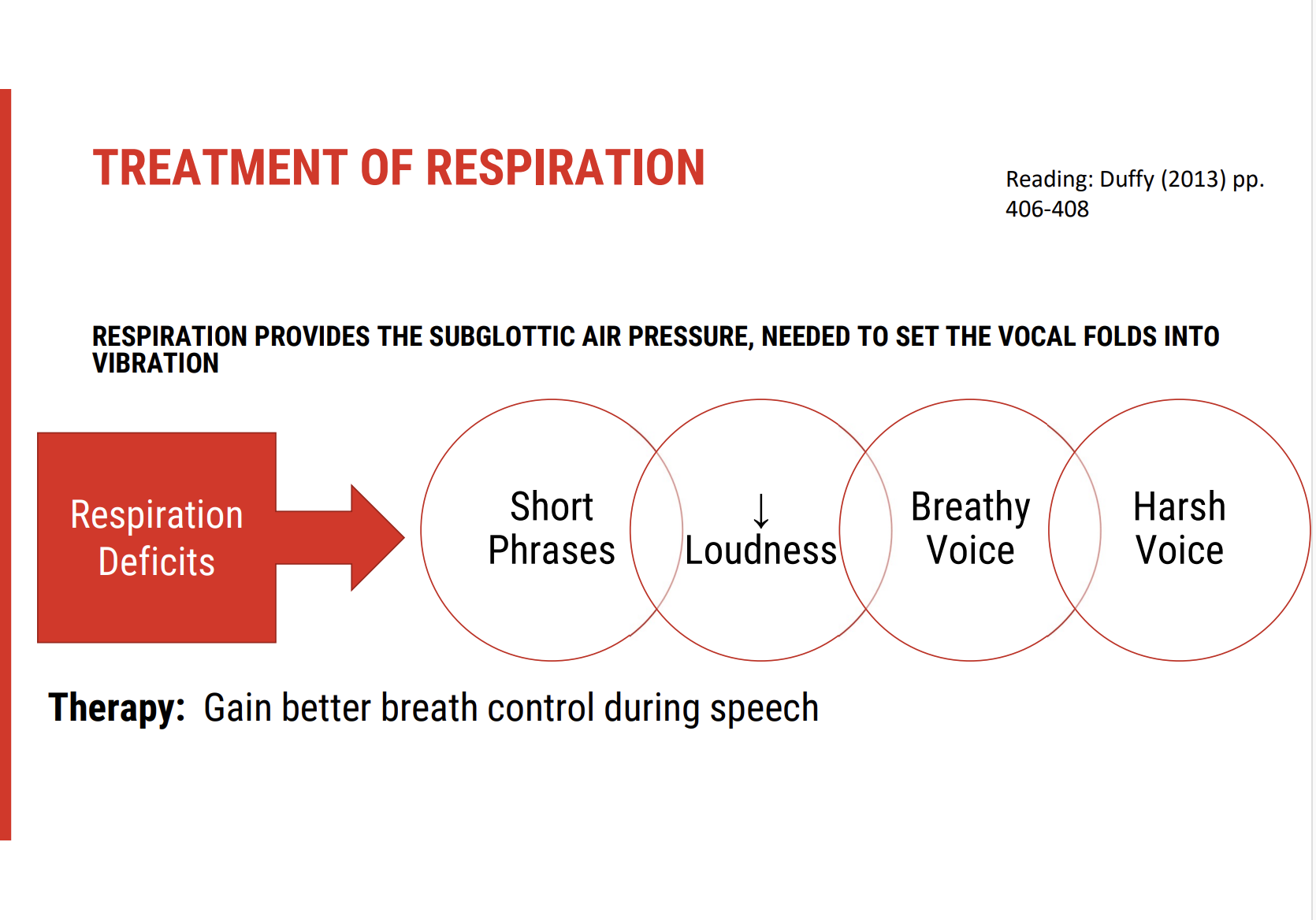
Respiration and Subglottic Air Pressure 🫁
Key Role of Respiration in Speech
Respiration provides the subglottic air pressure essential for initiating vocal fold vibration. Without adequate expiratory drive, speech production is compromised, leading to deficits such as:
Insufficient expiratory drive for speech: Difficulty generating enough air pressure to support speech.
Shallow respiration: Breathing that lacks depth, impacting speech endurance.
Poorly coordinated respiration: Difficulty synchronising breathing with speech.
Respiratory Deficits in Hyperkinetic Dysarthria
In conditions like hyperkinetic dysarthria, deficits may include:
Reduced postural support: Often due to neck injury or other impairments.
Reduced control of expiratory muscles: Leading to inadequate breath support for speech production.
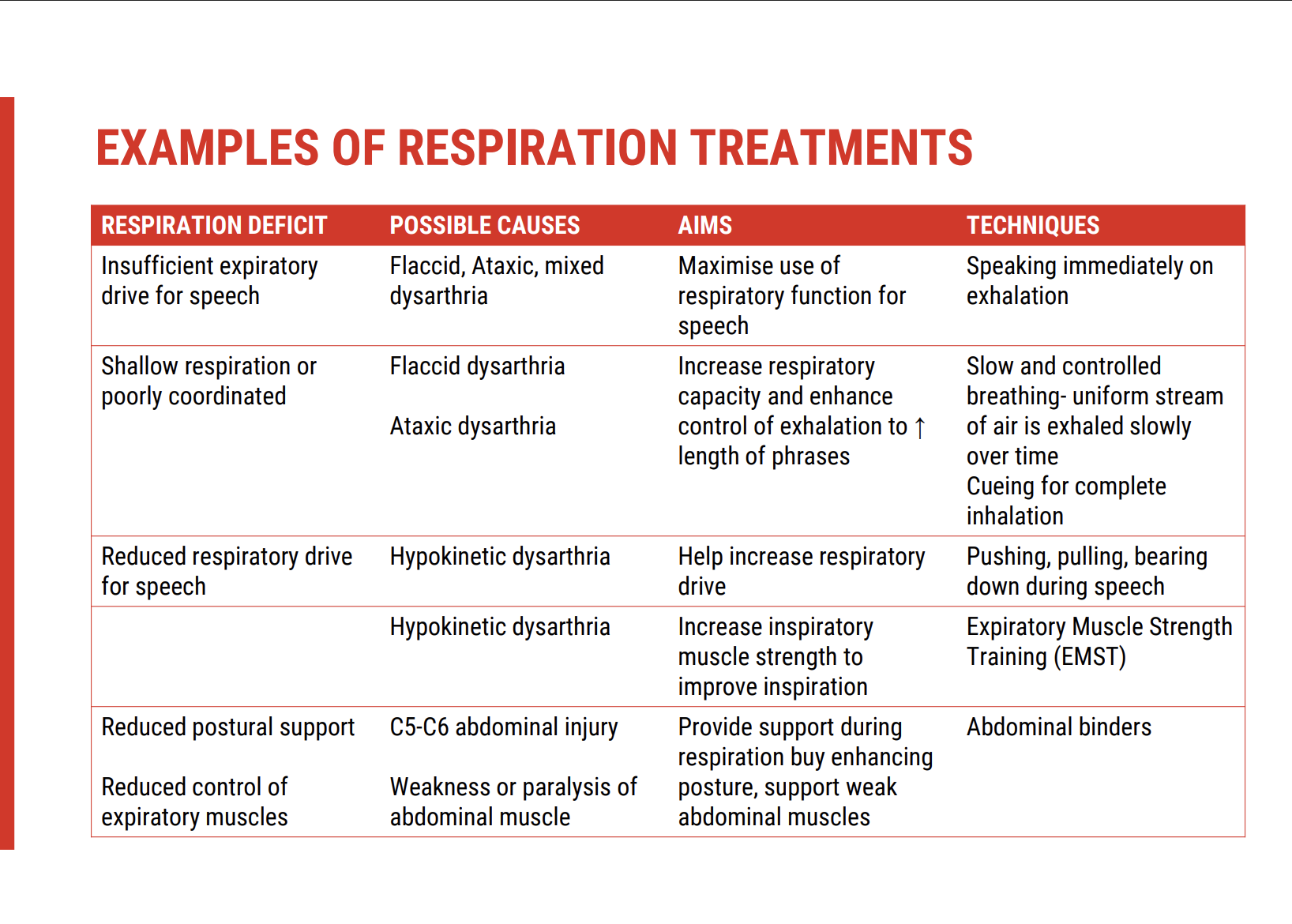
Treatment Approaches Based on Dysarthria Type
The treatment approach should be tailored to the specific type of dysarthria, and can include strategies for restoring or promoting residual function, depending on the underlying aetiology. Common techniques include:
Restoring function: Focusing on improving the individual's respiratory capacity and coordination.
Promoting residual function: Maximising the person's remaining respiratory abilities.
Respiratory Deficits and Communication Impact
When respiratory deficits affect speech, we might see:
Short phrases: Difficulty maintaining speech without taking frequent breaths.
Reduced loudness: Inability to project the voice effectively.
Impaired vocal quality: Voice may be breathy, weak, or harsh.
Non-syntactic breathing: Breaths taken in unnatural places, disrupting natural speech flow (e.g., in the middle of a phrase).
Treatment Techniques for Respiratory Deficits
Effective treatment for these deficits might include:
Speech tasks over non-speech tasks: Speech-focused exercises tend to be more beneficial for improving respiratory function in these cases.
EMST (Expiratory Muscle Strength Training): Though initially introduced for dysphagia, EMST has shown evidence of helping individuals with progressive neurological diseases who experience respiratory weakness.
Strengthening exercises: Focused on enhancing expiratory muscle function to improve speech production.
Goal Setting and Technique Selection
It's important to match the treatment to the specific respiratory deficit and its cause. When setting goals, consider:
The specific deficit: Understand whether the issue is related to breath control, loudness, or quality.
The underlying cause: Is the deficit due to a neurological condition, injury, or another factor?
Appropriate technique selection: Choose the most effective method for supporting the individual's goals and promoting speech function.
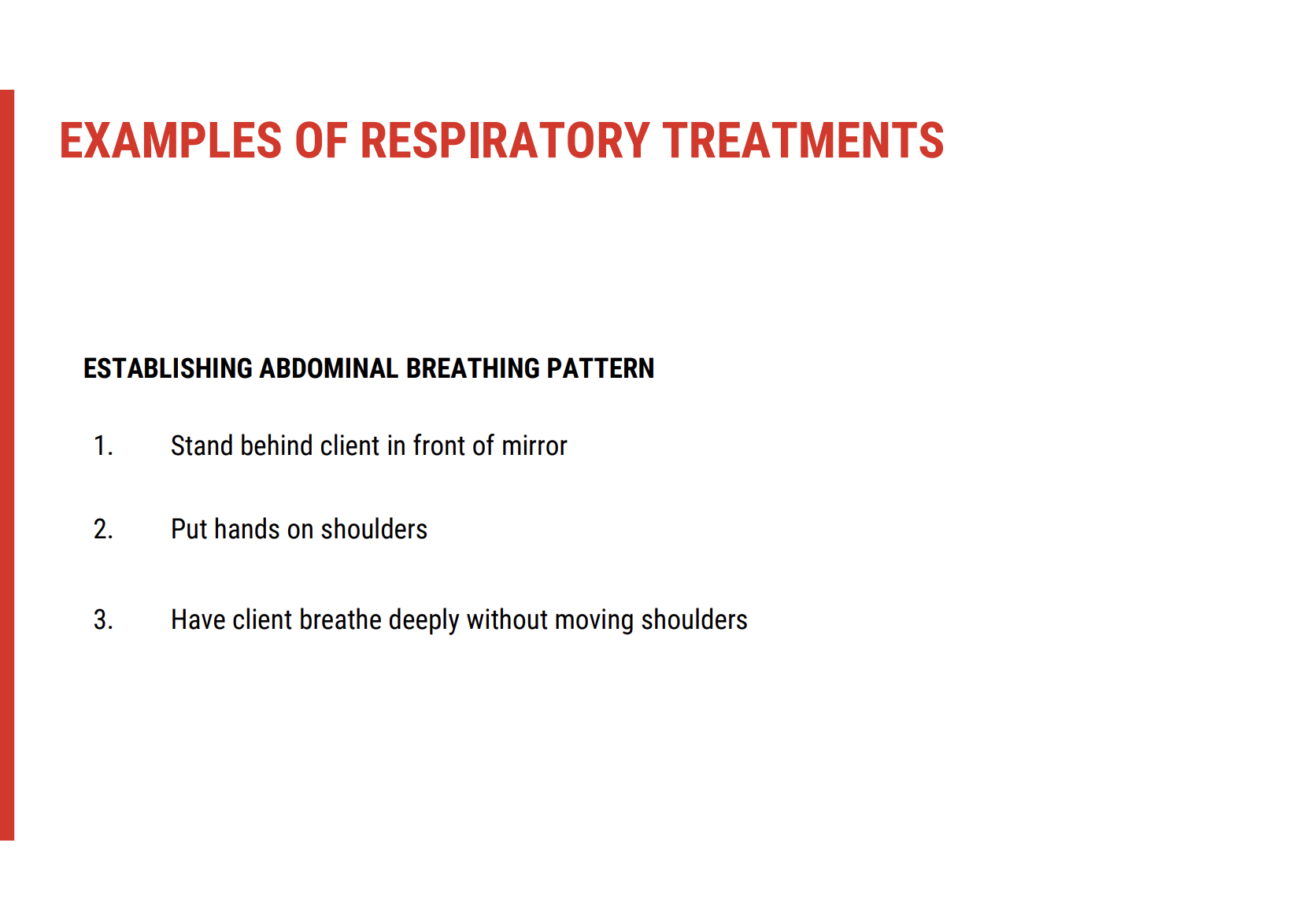
Respiratory Treatment and Voice Approaches 🗣
Focus on Abdominal Breathing Patterns
A key component in respiratory treatment for speech involves teaching clients to establish abdominal breathing. This pattern helps create the necessary airflow for effective voice production.
Mirror Activity:
Have the client observe their torso in front of a mirror.
Encourage them to notice their breathing patterns and describe what they see.
Identifying Breathing Patterns
By focusing on visual feedback, the therapist can help the client identify and correct ineffective breathing strategies.
Clavicular Breathing:
If the client uses clavicular breathing, you’ll observe their collarbone and shoulders rising during inhalation.
This pattern is inefficient for speech production and often indicates shallow breathing.
Correcting Breathing Patterns
Once the client recognises the inefficient pattern, the next step is to shift them to diaphragmatic breathing.
Diaphragmatic Breathing:
Instruct the client to breathe deeply without moving their shoulders.
Focus on using the diaphragm and expanding the belly rather than relying on the chest or shoulders.
Hands-on Support for Visualization
Physical Guidance:
With the client's permission, gently place your hands on their shoulders to help them visualise the movement.
As they practice diaphragmatic breathing, this touch can help them become more aware of shoulder movement and encourage proper breath support.
Respiratory Exercises for Speech Tasks 🗣
Inhalation and Exhalation Control
A key respiratory exercise is teaching the client to control both inhalation and exhalation during speech tasks. This improves breath support and control for effective speech production.
Inhalation and Exhalation Sequence:
Ask the client to breathe in quickly and then breathe out slowly (over a period of 10 seconds).
This exercise simulates the natural breathing pattern needed for speech, where exhalation is slower than inhalation.
Abdominal Breathing with Controlled Durations
Once the client is familiar with abdominal breathing, you can build on this by introducing controlled breathing patterns:
Breathing Exercise (Inhale/Exhale):
Instruct the client to breathe in for three seconds, and then breathe out for six seconds.
This helps develop breath control for longer phrases.
Speech Tasks for Breath Control
Incorporating speech tasks can help improve both the duration and force of the breath used in speech:
Soft-Loud-Soft Exercise:
Ask the client to speak softly, then loudly, and then softly again.
This variation challenges breath control, improving both volume regulation and breath endurance.
Resources for Practice
Video Examples:
Online materials for the week include video examples demonstrating these exercises, providing visual guidance for the client and therapist.
Phonatory Deficits Overview
Phonatory deficits can manifest as issues with vocal quality, often resulting from weak or tight vocal fold reduction. The characteristics of the voice depend on the specific type of dysarthria, and may include:
Breathy voice: The voice sounds airy due to insufficient vocal fold closure.
Harsh voice: The voice sounds rough or strained due to excess tension in the vocal folds.
Strained voice: Difficulty producing smooth, natural sounds, often accompanied by effortful speech.
These deficits interfere with clear and effective speech production and need targeted therapy for improvement.
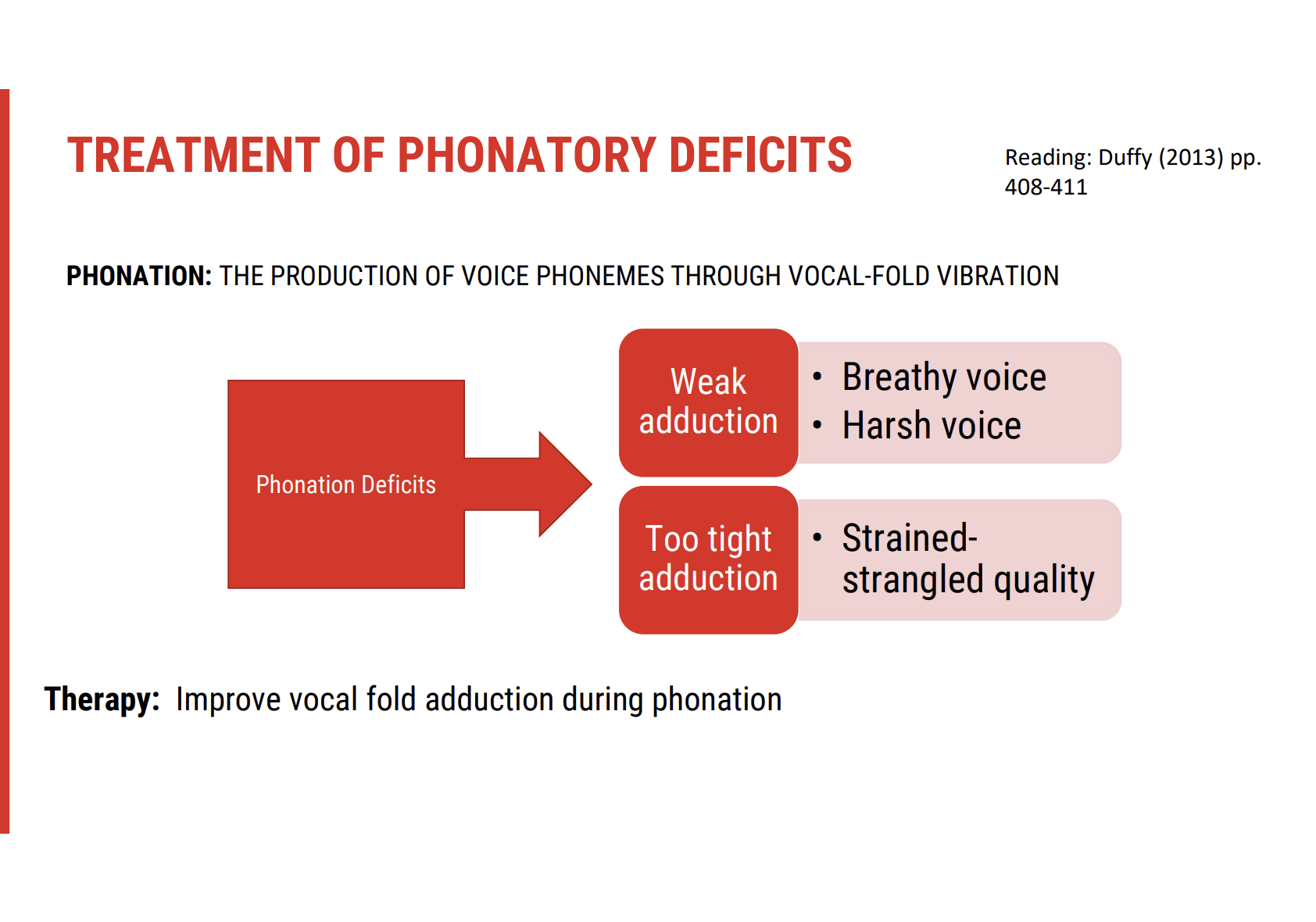
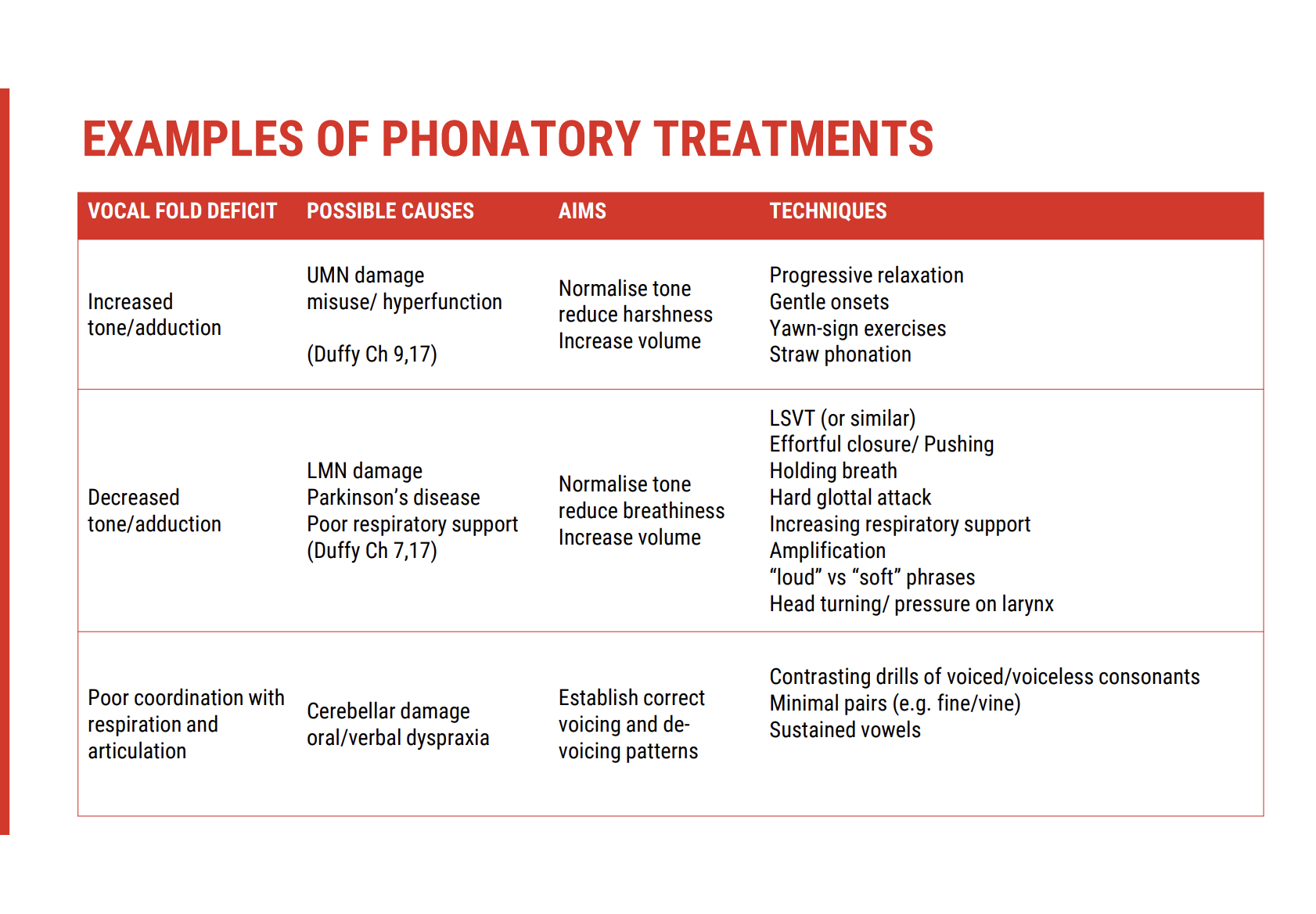
Phonatory Treatments for Dysarthria 🎤
Goal of Phonatory Treatment
The primary aim of phonatory treatments is to improve vocal fold adduction or abduction during phonation. This helps address issues such as breathy, harsh, or strained vocal quality.
Treatment Approaches Based on Specific Impairments
Upper Motor Neuron Damage (e.g., Right-sided Stroke)
Symptoms:
Unilateral facial weakness (often on the left side).
Reduced strength and speed of vocal fold movements, with increased tone.
Resulting harsh voice quality.
Treatment Goal:
Normalise tone, reduce harshness, and improve speech loudness.
Treatment Approaches:
Relaxation exercises: Target muscle systems involved in speech to reduce excess tone.
Straw phonation: Encourages easier vocal fold vibration by using a straw to partially close the mouth, increasing air pressure in the vocal tract.
Lower Motor Neuron Damage (e.g., Basal Ganglia Damage or C5 Level Respiratory Support Issues)
Symptoms:
Decreased tone and poor adduction of vocal folds.
Resulting in a quiet or breathy voice.
Treatment Goal:
Increase loudness and vocal fold adduction for clearer speech.
Treatment Approaches:
LSVT (Lee Silverman Voice Treatment): Focused on increasing loudness.
Pushing strategy: Encourages the client to use a hard surface to push off when speaking, helping increase vocal strength.
Artificial amplification: Using a microphone or speaker to amplify the voice, particularly useful for individuals with cerebellar damage.
Apraxic Changes (Coordination Issues, E.g., Dyspraxia)
Symptoms:
Poor coordination between respiratory and articulation systems.
Short, gasping breaths throughout speech attempts, leading to oral or verbal dyspraxia.
Treatment Approach:
Dyspraxia-focused techniques: Exercises that concentrate on improving respiration and voicing coordination. This approach aims to improve both breath control and motor coordination during speech tasks
Treatment of Phonatory Deficits 🎤
Goal of Phonatory Treatment
The main objective in treating phonatory deficits is to improve vocal fold adduction or abduction during phonation. This helps resolve issues such as breathy, harsh, or strained voice quality.
Treatment Approaches Based on Specific Impairments
Upper Motor Neuron Damage (e.g., Right-Sided Stroke)
Symptoms:
Unilateral facial weakness (typically on the left side).
Reduced strength and speed of vocal fold movements, often with increased tone.
Harsh voice quality due to increased tension in the vocal folds.
Treatment Goal:
Normalise tone, reduce harshness, and improve speech loudness.
Treatment Approaches:
Relaxation exercises to reduce excess tone in the muscles involved in speech.
Straw phonation: Helps facilitate vocal fold vibration by increasing air pressure in the vocal tract, making it easier to phonate.
Lower Motor Neuron Damage (e.g., Basal Ganglia Damage or C5 Level Respiratory Support Issues)
Symptoms:
Decreased tone and poor adduction of the vocal folds.
Resulting in a quiet or breathy voice.
Treatment Goal:
Increase vocal loudness and improve vocal fold adduction for clearer speech.
Treatment Approaches:
LSVT (Lee Silverman Voice Treatment): Focuses on improving loudness.
Pushing strategy: Encourages using a hard surface to push off before speaking to increase vocal strength.
Artificial amplification: Utilising a microphone or speaker to amplify the voice, helpful for those with cerebellar damage.
Apraxic Changes (Coordination Issues, E.g., Dyspraxia)
Symptoms:
Poor coordination between respiratory and articulation systems.
Short, gasping breaths during speech, resulting in oral or verbal dyspraxia.
Treatment Approach:
Dyspraxia-focused techniques: Exercises targeting improved respiration and voicing coordination, helping with motor control during speech tasks.
Exercises for Relaxation and Phonation
Voiceless Sounds:
Focus on relaxing the shoulders and jaw, and take a low breath for support from the stomach muscles.
Voiced Sounds:
Maintain consistent breath support and focus on projecting the voice forward while avoiding tension in the neck.
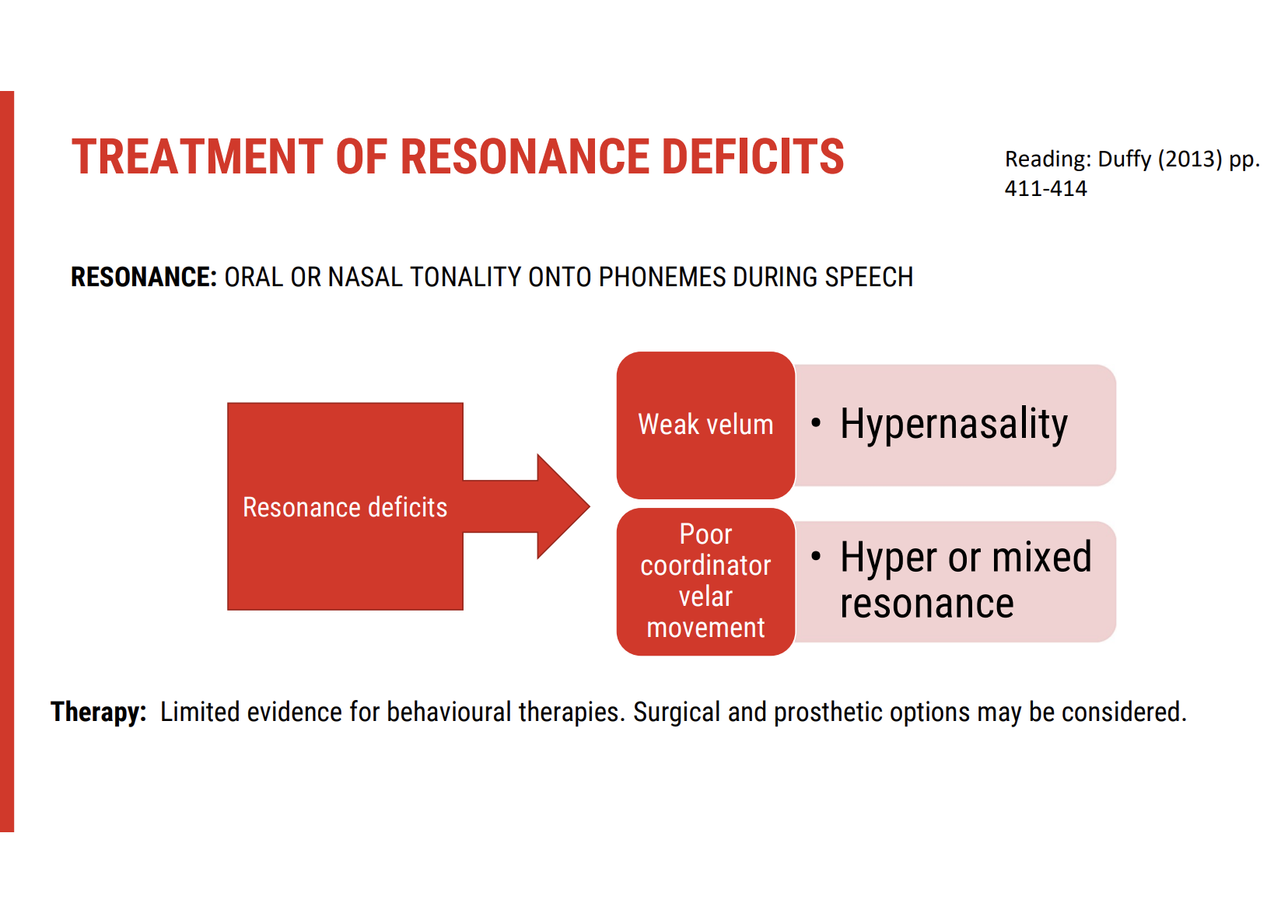
Resonance Deficit Presentation
Resonance issues often manifest as oral or nasal tonality in speech.
This is usually caused by:
A weak velum (soft palate), or
Poorly coordinated velar movement.
Therapeutic Approaches
Behavioural therapy:
Limited evidence supports its effectiveness for resonance disorders.
May be attempted in mild cases or as adjunct support.
Surgical or prosthetic interventions:
More commonly used when resonance deficits are significantly impacting communication or quality of life.
Examples include:
Palatal lift prostheses
Surgical correction of velopharyngeal insufficiency
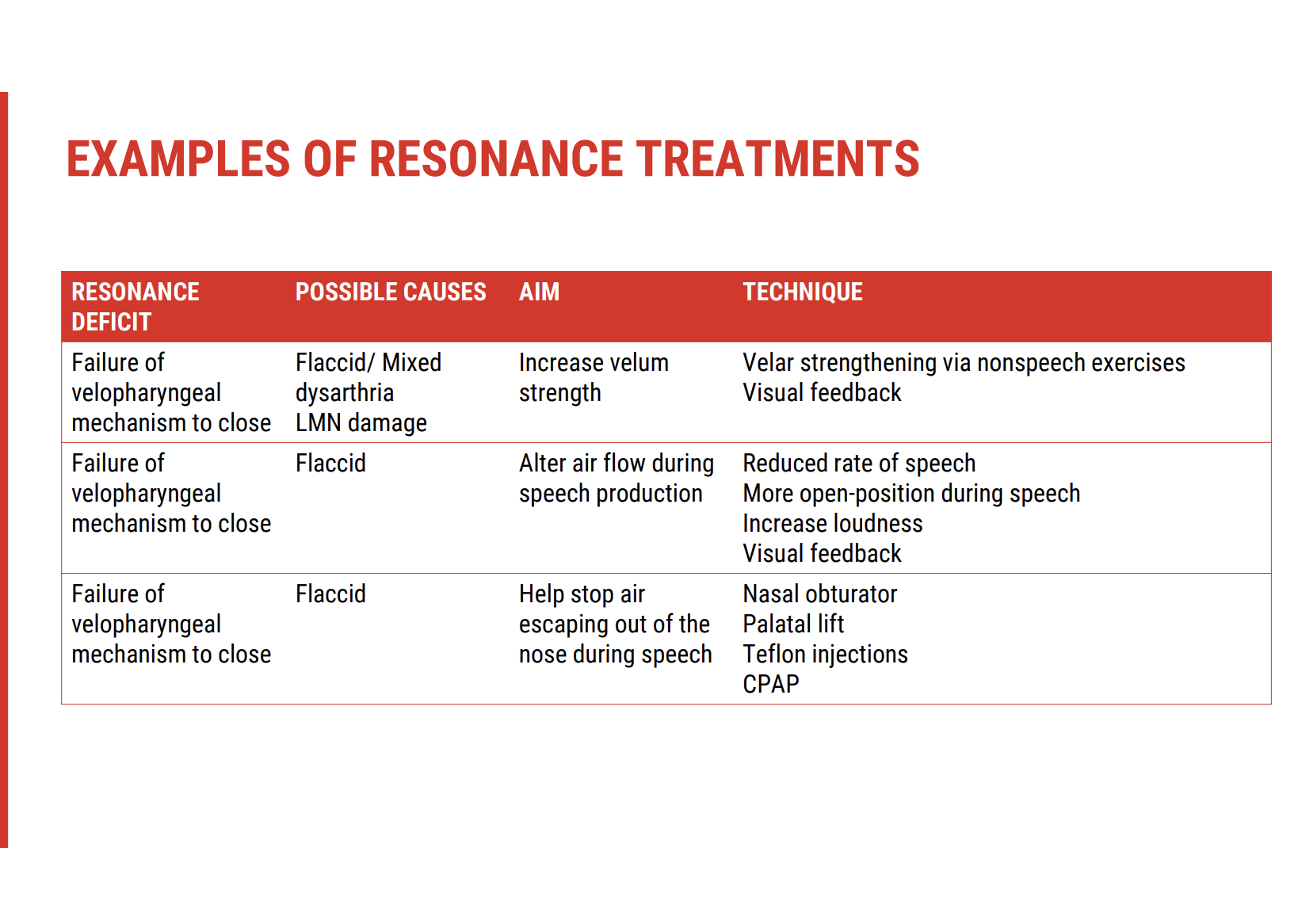
Treatment of Resonance Deficits (continued) 🔊
Speech Strategies for Compensation
While evidence for behavioural therapy is limited, some compensatory strategies can improve intelligibility, even if they don’t directly treat velopharyngeal function.
Useful techniques include:
Reducing speech rate
Over-articulating to enhance clarity
Using visual feedback tools:
Mirror or cold spoon under the nose can help clients detect nasal air emission visually, enhancing self-monitoring.
Emerging and Supportive Therapies
CPAP (Continuous Positive Airway Pressure)
Applied during speech tasks.
Some evidence supports its use for velopharyngeal strengthening, especially in spastic dysarthria.
Prosthetic Management
Palatal Lift Prosthesis
Custom-made device fitted by a dental prosthetist.
Supports the soft palate to improve velopharyngeal closure.
Often more effective than surgery, especially when:
The client is cooperative
The musculature is responsive
Structural anatomy allows a good fit
Clinical Focus
For many clients, compensation is more realistic than restoration.
Improving overall speech clarity, not necessarily velopharyngeal function itself, becomes the primary clinical goal.
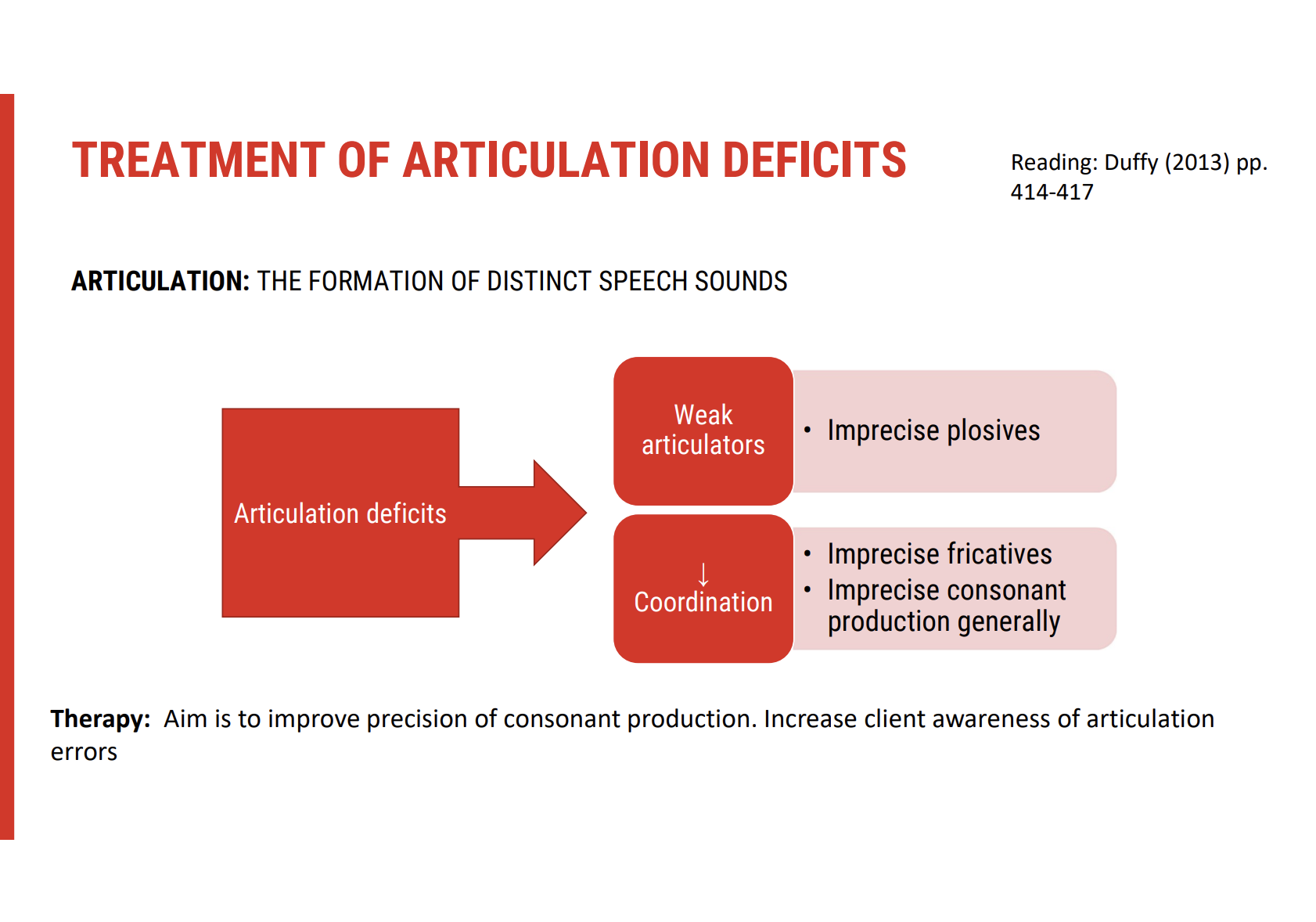
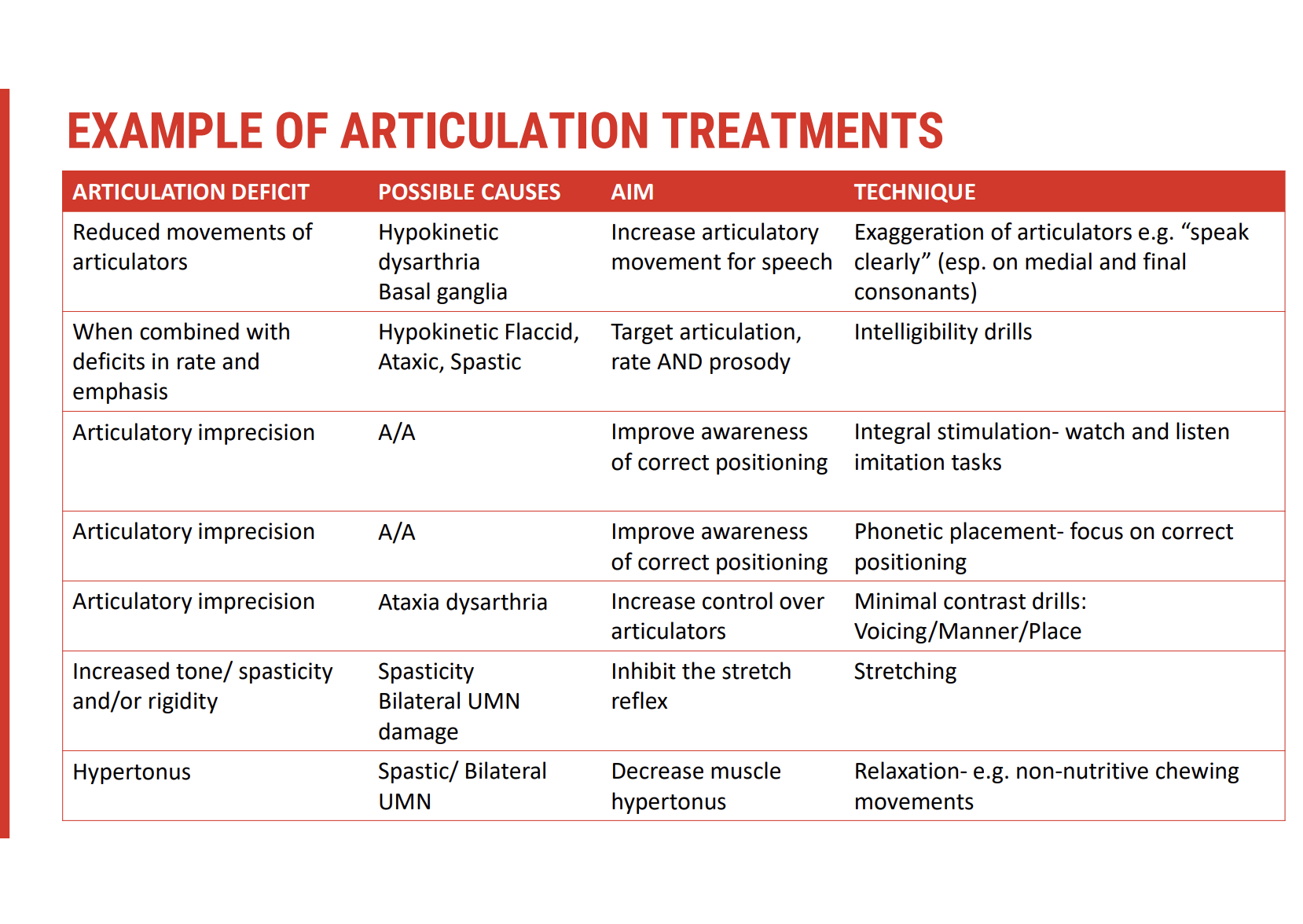
Treatment of Articulatory Deficit
Articulatory Deficit Presentation
Typically observed as imprecise production of:
Plosives (e.g. /p/, /b/, /t/, /d/)
Fricatives (e.g. /s/, /f/, /ʃ/)
Consonant blends
Caused by:
Weakness of articulators (e.g. lips, tongue)
Reduced coordination
Can result from motor execution (strength) or motor planning (skill)
Therapy Goals
Improve consonant precision to enhance intelligibility.
Increase client awareness of articulatory errors through feedback-based tasks.
Tailor therapy to whether the issue is:
Skill-based (e.g. incoordination, apraxia)
Strength-based (e.g. flaccid dysarthria)
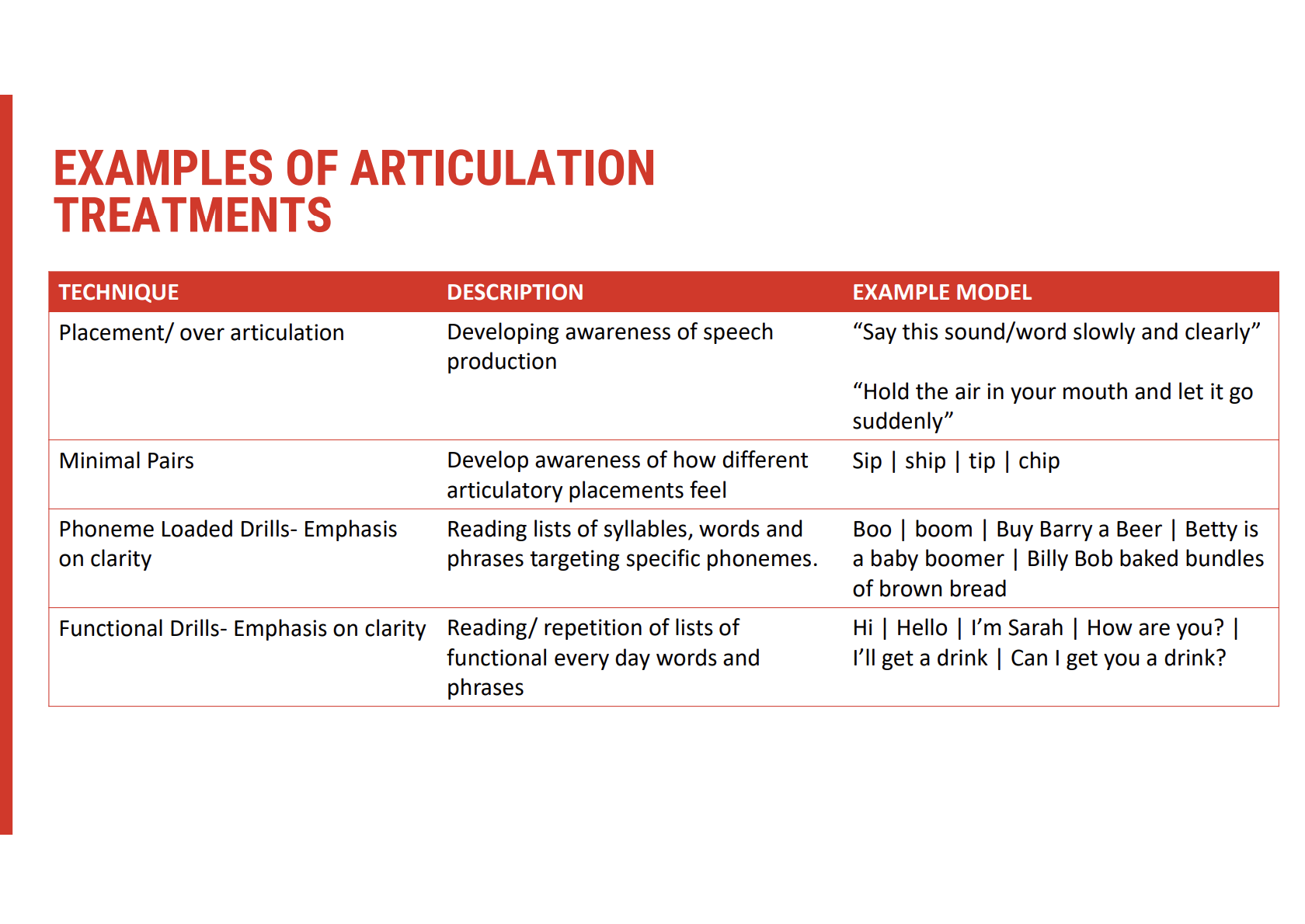
Treatment of Articulatory Deficits 🗣
Speech-Oriented Therapy Approaches
Drill-based practice:
Repeating words and phrases with specific phonetic targets
Often used for strengthening motor patterns
Phonetic Placement Techniques:
Teaching where to place articulators (e.g. lips, tongue) to produce specific sounds
Effective for clients with motor execution issues
Exaggerated Articulation & Minimal Contrast Drills:
Emphasising clear articulation (e.g. /p/ vs. /b/)
Useful for improving perceptual distinctiveness
Apps & Programmes
Apps for articulation and intelligibility support independent practise
Evidence-based structured programs:
Be Clear – Focuses on speech clarity
Speech Atacks ATAX – Tailored for ataxic dysarthria
Motor Learning Principles
Therapy tasks should be:
Meaningful to the client
Relevant to their communication needs
Embedded in functional contexts
Rate Control for Intelligibility
Slowing rate is one of the most effective strategies for improving intelligibility
Techniques include:
Pacing boards or visual cues
Increased pausing time before and during speech
Mindful utterance planning to avoid speech “running together”
Summary of Key Techniques
Intelligibility drills
Phonetic placement instruction
Over-articulation strategies
Minimal pair contrast exercises
Use of apps and structured programmes
Rate reduction strategies
Articulatory Treatment Resources
Supplementary Examples Available
Additional examples of articulation treatments are provided:
In this session (verbal and/or slide-based)
In the online learning module linked with this content
Included Resources
Examples may include:
Video demonstrations
Drill templates
App recommendations
Phonetic placement visuals
Rate control strategy guides
Accessibility
All linked resources are:
Available online
Intended to complement therapy planning
Useful for reinforcing techniques discussed in therapy
Prosody Treatment 🎵
Common Presentations
Reduced articulatory precision and intelligibility due to:
Inappropriate speech rate
Prosodic abnormalities, such as:
Unpredictable tone
Monotone delivery
Equal and excess stress on syllables
Therapy Goals
Improve intonation, rhythmic variation, and appropriate stress in speech
Enhance the naturalness and expressiveness of spoken communication
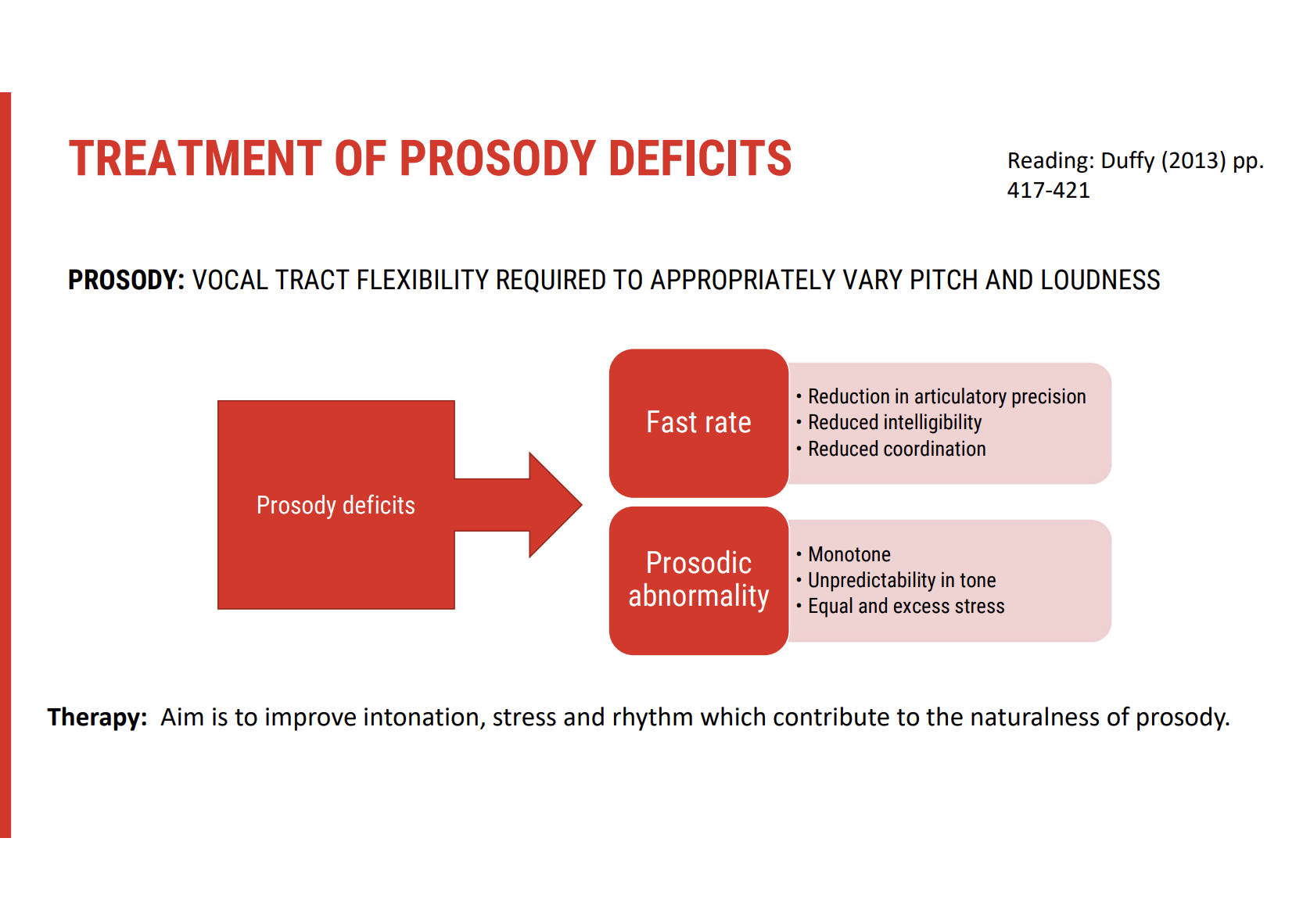
Prosody Treatment Technique
Key Strategies
Contrastive Stress Drills
🔹 Practise emphasising different words in a sentence to change meaning (e.g. "I didn't steal the money" vs "I didn't steal the money").
🔹 Improves intonation, stress control, and clarity.Chunking Utterances
🔹 Teach the speaker to break sentences into natural breath groups.
🔹 Supports rhythm, pausing, and better breath control.Emphasis & Meaning
🔹 Explore how changes in stress alter interpretation and message clarity.Rhythm & Melody Activities
🔹 Use poetry, lyrics, or nursery rhymes to introduce melodic flow.
🔹 Enhances intonation and natural speech patterns.
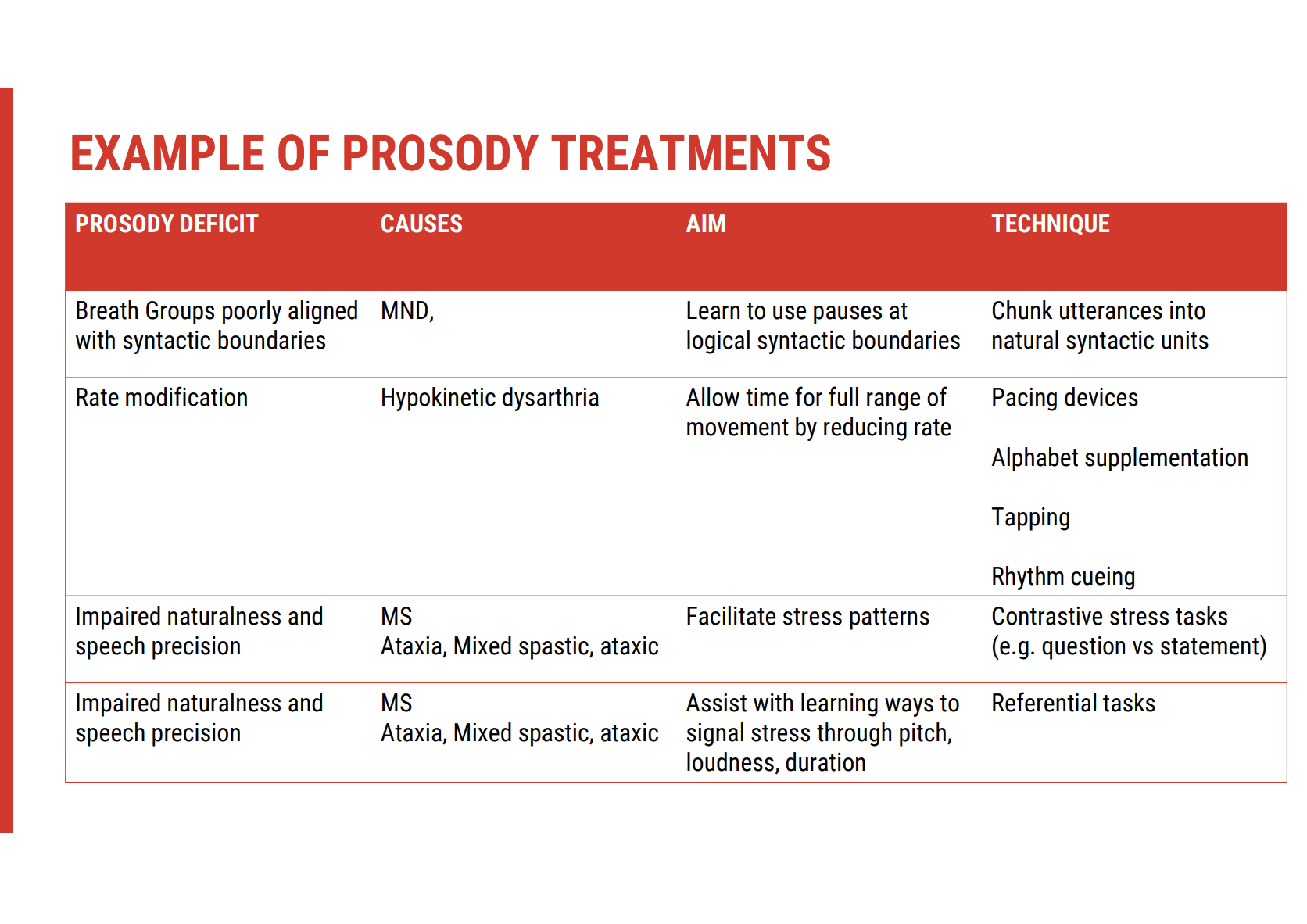
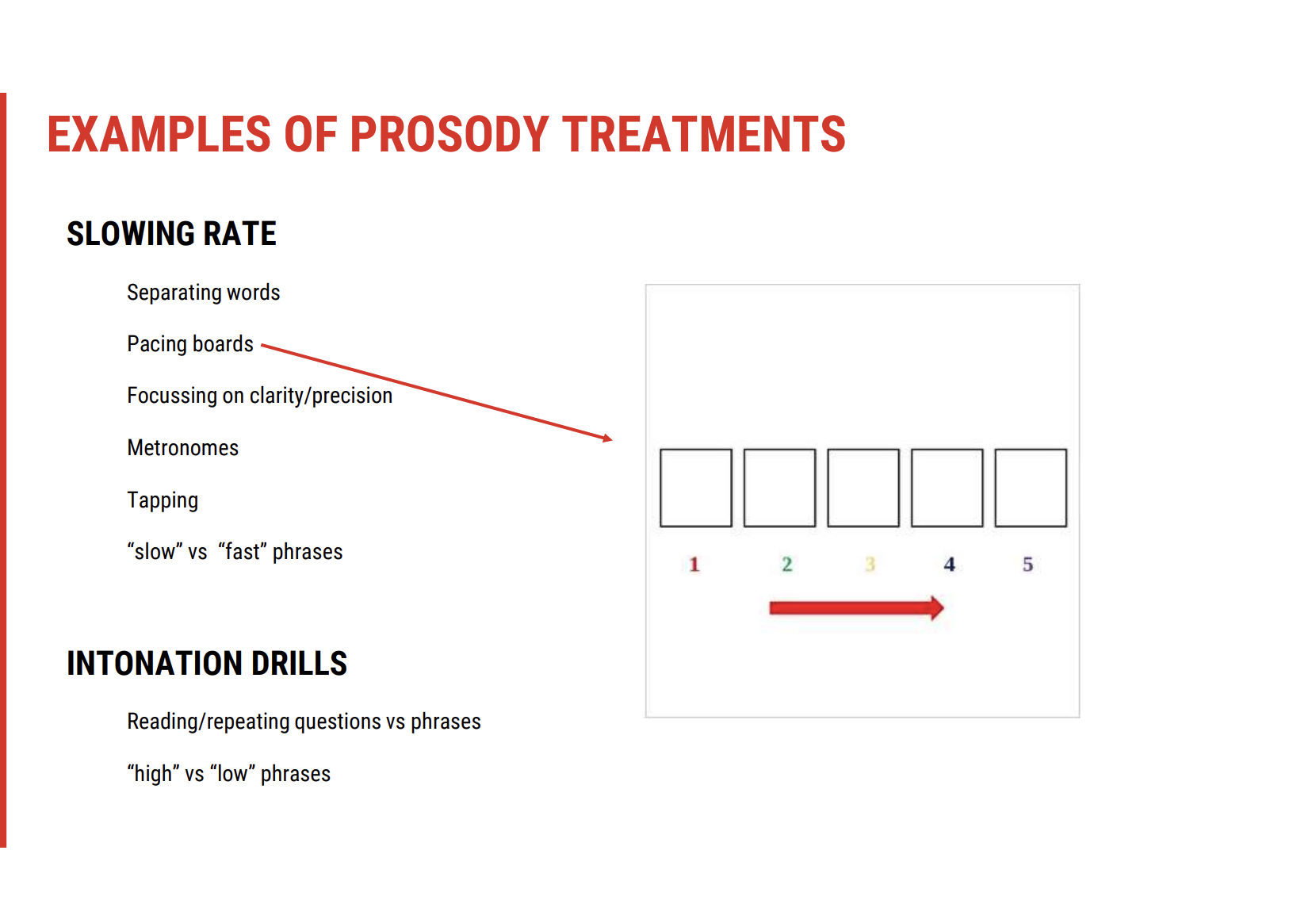
Prosody Treatments (Continued)
Rate Control Techniques
Rationale: A fast speech rate can reduce intelligibility, hinder sound sequencing, and affect prosody clarity.
Treatment Tools
Pacing boards:
🔹 Client touches each space for every syllable spoken.
🔹 Encourages pausing and slowed articulation.Metronomes:
🔹 Set to adjustable rates to regulate timing of syllable production.
🔹 Helps maintain rhythmic speech patterns.Syllable tapping:
🔹 Tapping while speaking supports motor timing and syllable awareness.Rate contrast tasks:
🔹 Practising switching between fast and slow phrases builds rate flexibility and self-monitoring.
Challenges in Prosody Treatment
High cognitive demand:
🔹 Controlling intonation, stress, and rate requires significant attention and motor planning.Generalisation difficulties:
🔹 Skills may be evident in clinic but less transferable to real-world, spontaneous contexts.
🔹 Increased cognitive load (e.g. formulating ideas while speaking) can reduce success outside therapy.
Prosody Treatment Approaches – Enhancing Naturalness & Intelligibility
🎯 Primary Goals of Prosody Therapy
Improve naturalness in speech through intonation, stress, rhythm, and loudness control.
Support intelligibility by controlling speech rate, syllable timing, and emphasis.
Enhance self-monitoring and awareness of how prosodic features influence meaning.
🧠 Why It's Challenging
Requires high-level motor coordination, planning, and cognitive flexibility.
Generalisation is difficult: What works in clinic may break down in spontaneous, real-life conversation due to increased cognitive demands.
Control over prosody often deteriorates outside rehearsed contexts.
🎵 Treatment Strategies & Techniques
🔹 Stress & Emphasis Drills
Contrastive stress practice:
E.g. “She dressed and fed the baby” vs. “She dressed and fed the baby.”
Helps clients understand how emphasis shifts meaning.
Single-word and phrase-level work using minimal pairs or emotional tone changes.
E.g. “Record” (noun) vs. “record” (verb).
🔹 Hierarchical Task Complexity
Progress tasks from simple to complex:
Start with single syllables or short phrases.
Build toward multi-syllabic, sentence-level tasks with stress shifts.
Vary by:
Number of syllables
Complexity of utterance
Semantic context (e.g. neutral vs emotional tone)
🔹 Volume Awareness & Calibration
Loudness drills target hypophonia or monotone presentation:
Clients often lack awareness of how quiet they are.
Therapy focuses on recalibrating what “normal” sounds like.
Use tools like:
Decibel meter apps
Biofeedback software (e.g. LSVT Companion)
🔹 Prosodic Engagement Activities
Use poetry, nursery rhymes, or song lyrics to practice rhythm, melody, and emphasis.
Question/statement intonation exercises:
E.g. “It’s raining?” vs. “It’s raining.”
Conversational role-play:
Practise using pitch variation and pause to convey intention (e.g. “You can have beans or cabbage.”)
🔹 Rate Control Tools (Reviewed)
Pacing boards, metronomes, syllable tapping, alternating fast/slow phrases:
Promote rhythmic speech control.
Improve speech segmentation and prosodic clarity.
🎯 Therapist Tips
Make it meaningful: Embed prosody drills in relevant and real-life tasks (e.g. greeting someone, asking a question, storytelling).
Use audio recordings: Clients can listen back to their speech to increase insight.
Incorporate family or carer feedback: They often notice subtle prosodic improvements or persisting deficits in everyday settings.
Communication-Oriented Treatment Approaches
🎯 Goal of Communication-Oriented Treatment
Focus on improving communication effectiveness rather than restoring speech function.
Adapt to communication challenges even if speech remains impaired or worsens.
Problem-solving environmental and interpersonal factors that enhance overall communication success.
🧠 Key Elements in Communication-Oriented Treatment
🔹 Speaker Strategies
What the patient can do:
Adaptation of speech (e.g. speaking slowly, using clear articulation).
Use of alternative methods (e.g. AAC devices if needed).
Improved vocalisation or gestures to support speech.
🔹 Listener Strategies
What the conversation partner can do:
Active listening: Paying attention and asking clarifying questions if needed.
Providing feedback: Offering verbal or non-verbal cues to confirm understanding.
Creating a supportive listening environment (minimising distractions, ensuring face-to-face communication).
🔹 Interaction Strategies
What both the speaker and listener can do:
Collaborative efforts to ensure effective conversation.
Strategies for turn-taking: Encouraging pauses and checking for comprehension.
Modification of communication style: Ensuring mutual understanding through gestures, writing, or drawing.
🔹 Environmental Manipulations
Optimising the communication environment:
Reduce background noise or visual distractions.
Proper lighting for clear visual communication (if using gestures or lip-reading).
Quiet spaces for better auditory focus during conversation.
🛠 Strategies for Effective Communication
Enhance speaker awareness of how speech may sound to others.
Equip listeners with tools to better understand speech, even if impaired.
Foster a collaborative environment where both speaker and listener actively contribute to communication success.
Modify settings to ensure clarity and reduce external communication barriers.
🎯 Benefits of Communication-Oriented Treatment
Increased confidence in communication despite speech impairments.
Better quality of life through enhanced social interaction.
Mutual understanding between speakers and listeners, improving daily life activities.
Communication-Oriented Treatment (Continued)
Goal of Communication-Oriented Approach
Focus on getting the message across and encouraging positive interactions.
The aim is to improve communication beyond speech alone, especially when the speech itself remains impaired.
🔧 Strategies for Enhancing Communication
🔹 Targeted Adjustments in Communication
Facial Expressions & Eye Contact: Encourage expressive facial communication and effective eye contact to aid understanding.
Distance & Environment: Ensure optimal distance for clear speech and adjust the environment (e.g. lighting, background noise).
Listener Considerations: Educate new listeners (e.g. baristas, shop assistants) about the person's speech difficulties.
🔹 Communication Repair Strategies
Cards to Explain Speech Difficulties: Use a card to explain the condition (e.g. "I’ve had a stroke; I have a speech problem, but I can understand and converse").
Breakdown Management:
Ask for repetitions if something is misunderstood.
Letter boards: Use to identify the first letter of words that are hard to understand.
🔹 Practical Support in the Community
Educate individuals (e.g. community workers, friends) on how to facilitate communication, ensuring smooth exchanges.
🌍 Optimising Communication in Various Settings
Awareness and education for communication partners can dramatically improve understanding.
Encouraging the use of repair strategies like asking for repetition or pointing to letters can prevent frustration and enhance communication flow.
🎯 Benefits of Communication-Oriented Strategies
Improved interactions with community members (e.g. baristas, shop assistants).
Increased participation in daily life activities without focusing on speech restoration.
Reduced frustration by providing tools for managing communication breakdowns.
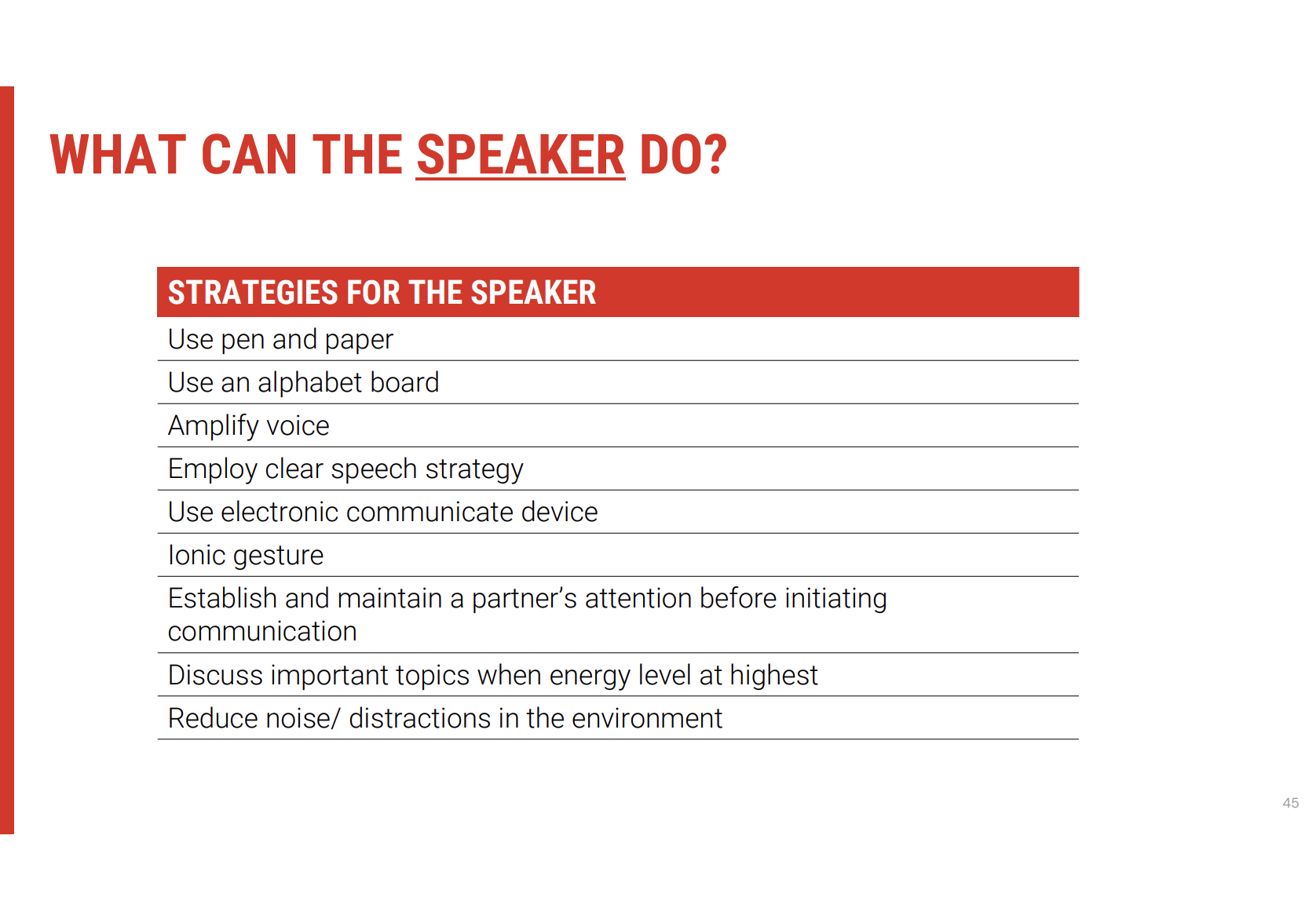
Speaker Strategies for Optimising Communication
🎯 Key Techniques for Speakers to Enhance Communication
🔹 Pen and Paper Use
Shift modality to pen and paper when speech is tiring or unclear, offering an alternative communication method.
🔹 Voice Amplification
Amplify voice to improve loudness and increase communication efficiency, making speech clearer for listeners.
🔹 Clear Speech Strategies
Slow down speech to give full range of articulators time to move, which enhances intelligibility.
Increase awareness of exchanges, focusing on clear articulation and pacing.
🔹 Use of Iconic Gestures
Incorporate gestures to augment speech, improving message transfer and helping listeners better understand.
🔹 Gain and Maintain Partner’s Attention
Draw the listener's attention before starting communication, ensuring they are focused on the conversation.
🔹 Reduce Background Noise
Eliminate or reduce distractions and noise in the environment, ensuring better focus on the message.
🔹 Optimise Communication Environment
Control environment: Ensure quiet, well-lit spaces for easier communication, especially if speech is low or unclear.
🔧 Additional Considerations for the Speaker
Slowing speech and gaining attention can significantly enhance the chances of message reception.
Minimising distractions helps the listener focus on the speaker, especially when loudness is an issue.
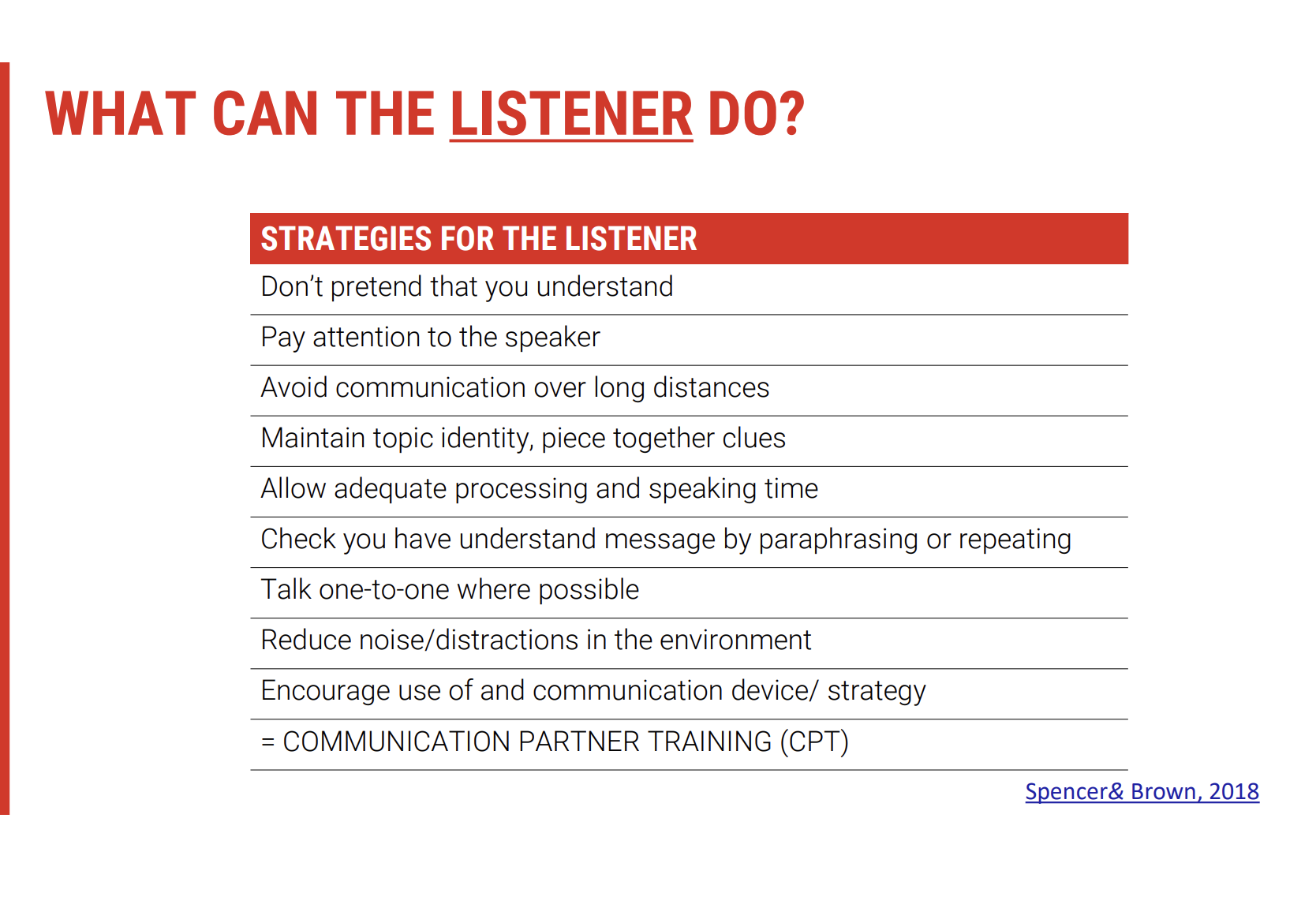
Communication Partner Strategies for Optimising Engagement
🎯 Coaching Caregivers & Communication Partners
🔹 Role of Communication Partner Training
Training for caregivers and family members is vital to improve communication effectiveness.
Clinical Practice Guidelines for Stroke Management recommend caregivers receive training from a speech pathologist to improve communication skills and help the person with communication difficulties engage optimally.
🔹 Goals of Communication Partner Training
The training aims to enhance communication strategies, enabling both the individual with communication difficulties and their communication partners to interact effectively.
This involves providing caregivers with tools to better support the person, reducing frustration and improving quality of interactions.
🛠 Key Components of Communication Partner Training
Interventions include:
Strategies for adjusting communication approaches.
Training in recognising and responding to communication breakdowns.
Non-verbal communication cues, such as eye contact and body language.
Techniques to improve conversation flow and understanding.
🔹 Frequent Reinforcement of Strategies
Regular reminders of these techniques throughout treatment can help embed them into daily routines and improve long-term outcomes.
📘 Reference to Prior Learning
Many of these strategies have been previously introduced in earlier modules or subjects, so they can be reinforced during the coaching sessions as a reminder to caregivers.
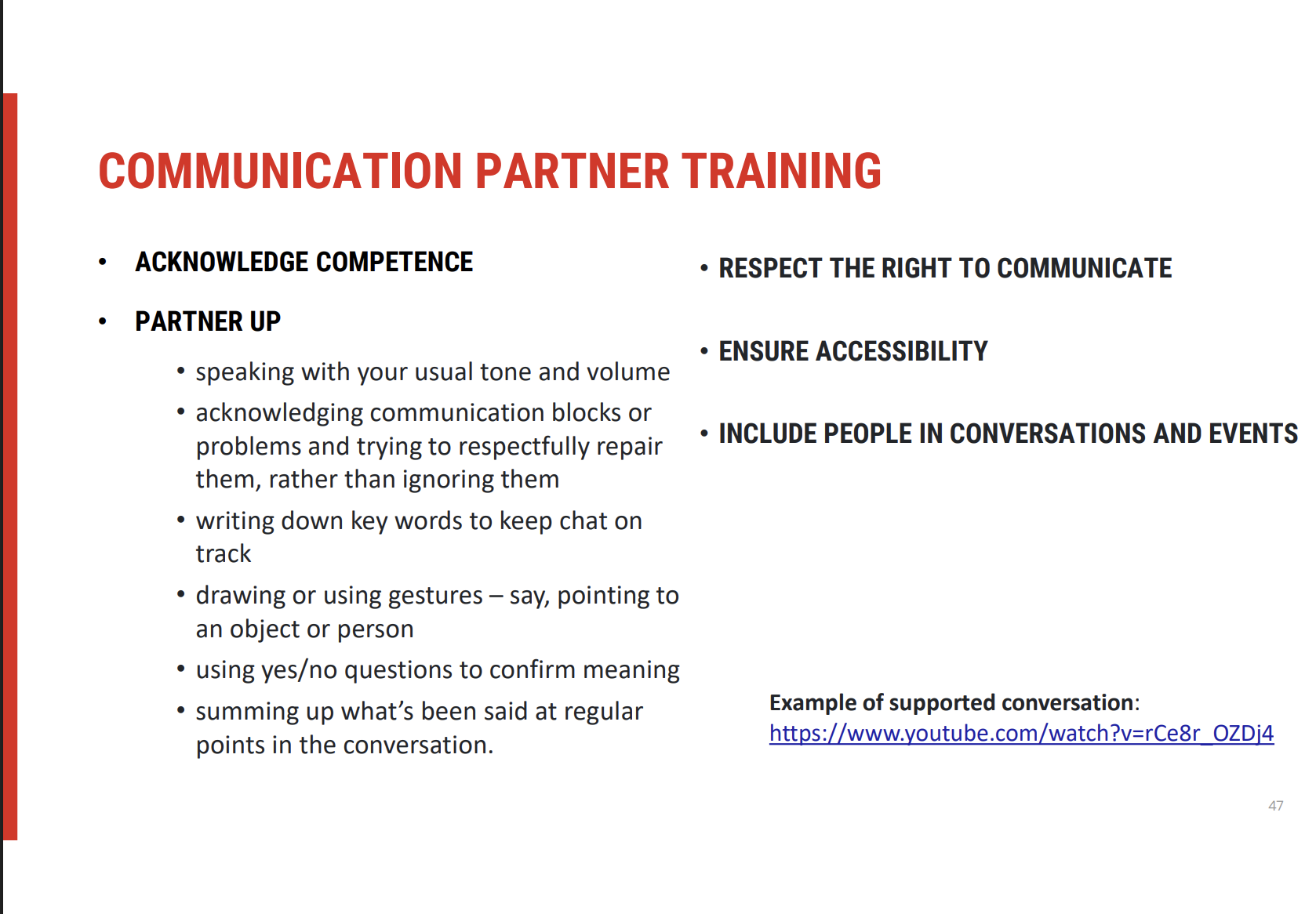
Fundamental Principles of Communication Partner Training
🎯 Key Principles for Effective Communication
🔹 Acknowledging Competence
It's crucial to recognise the person’s competence, regardless of their speech disorder.
Respecting intelligence and maintaining dignity sets the stage for more productive and respectful conversations.
🔹 Partnering Up
Communication is a shared responsibility: both the speaker and the communication partner have a role in ensuring effective interaction.
Evidence supports that when communication partners are trained and provided with strategies, it leads to better conversations and less frustration.
🛠 Core Strategies in Communication Partner Training
🔹 Effective Communication Techniques
Use usual tone and volume: maintaining normal conversational habits.
Acknowledge communication blocks instead of ignoring or pretending to understand.
Writing down key words can help maintain focus.
Drawing or gesturing to aid understanding.
Summing up important points regularly to keep track of the conversation.
🌍 Human Right to Communicate
🔹 Communication as a Human Right
Communication is fundamental to human experience, linking to identity, personal expression, and quality of life.
Without effective communication, individuals can experience significant quality of life challenges.
🔹 Ensuring Accessibility
Adjustments to language may be needed to accommodate individuals with communication difficulties.
This can include slowing down speech, simplifying information, or modifying how information is presented.
Inclusion is key: Ensuring the person is included in conversations, events, and activities provides them with the opportunity to practice and improve communication skills.
💡 Impact of Inclusion
Inclusion not only provides practice but also enhances social engagement, helping individuals feel valued and improving their overall communication confidence.
Offering choices and allowing the person to express their preferences encourages autonomy and supports effective communication.
Communication-Oriented Approaches: Shared Responsibility
🎯 Shared Responsibility for Communication
Communication-oriented approaches emphasise that the responsibility for modifying and adapting communication is shared between both the speaker and the communication partner.
The clinician plays a key role in supporting both the speaker and the listener to facilitate the entire communication exchange.
🛠 Facilitating Effective Communication: Speaker & Listener Roles
🔹 Key Strategies for Clinicians:
Scheduling Important Interactions: Ensuring that time is set aside for essential conversations.
Identifying Optimal Communication Times: Knowing when speaking is easiest or hardest for the person and tailoring communication strategies accordingly.
🌟 Optimising the Environment
🔹 Key Environmental Considerations:
Minimising Noise & Distractions: Creating a quieter environment for better clarity and focus.
Establishing Optimal Lighting: Ensuring proper visibility for non-verbal cues (e.g., facial expressions).
Seating Arrangements: Positioning participants comfortably to promote effective communication.
Maintaining Eye Contact: Encouraging appropriate eye contact to aid attention and understanding.
📝 Repairing Communication Breakdowns
Identifying Breakdowns: Recognising when communication has failed or is unclear.
Repair Strategies: Establishing what works and what doesn’t work to fix misunderstandings.
💡 Summary of Approaches for Motor Speech Disorders
These communication and speech-oriented behavioural strategies help improve the interaction between individuals with motor speech disorders and their communication partners.
The focus is on cooperative communication, creating favourable environments, and using repair strategies when needed to ensure successful interactions.