Male genital & urinary pathology
1/73
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
74 Terms
Congenital abnormalities
defects are quite common, about 1% of all male births
Cryptorchidism
hypospadias
espispadias
Hypospadias and Epispadias
Urethra opens into ventral surface (underside) of penis
more common: 3 in 1,000 live born males
Urethra opens onto dorsal (upper sect) surface of penis
uncommon: 1 in 100,000 live born males
more severe associations than hypospadias
both result in partial urinary obstruction that predisposes to infection
have defective ejaculation that may reduce fertility
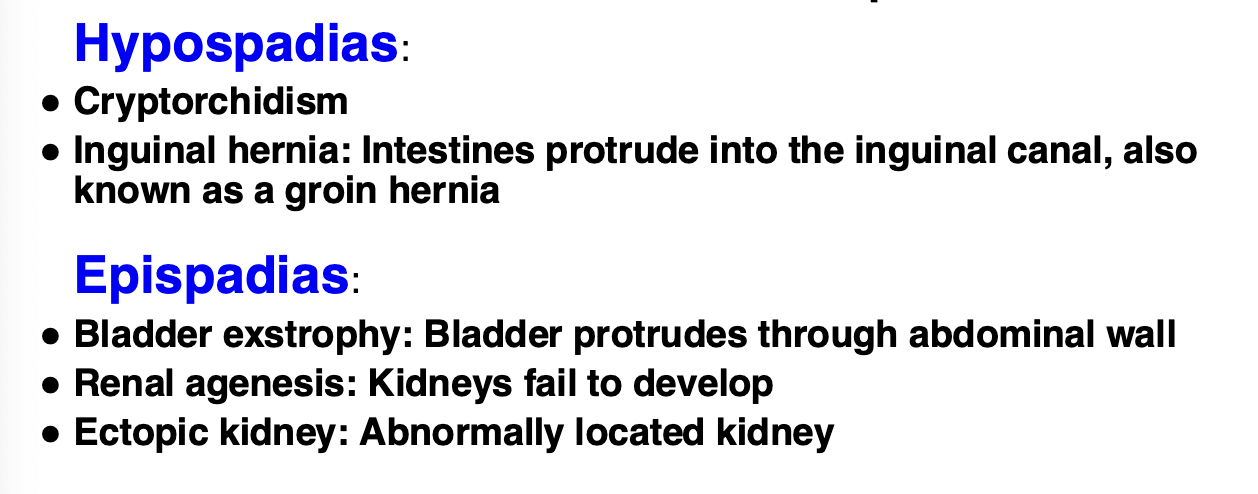
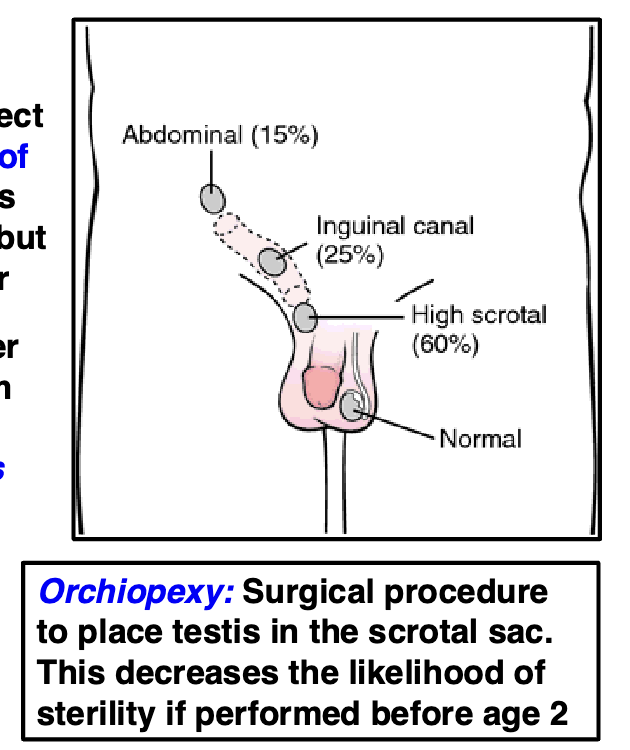
Cryptorchidism
absence of one or both testicles from the scrotum
most common development defect in male GU tract
affects over 3% of full-term newborns
in most cases testes will descend by 3 months, but 1% are still undescended at 1 yr
sperm production requires a lower temp
testes descend from the abdomen into the scrotum in utero or shortly after birth
testes not descended into scrotal sac greatly increases infertility
increases risk of testicular cancer later in life
Characteristics of STDs
caused by many different organisms
individuals may suffer from more than 1 STD at a time
initial symptoms almost always occur at site of infection
disease symptoms almost always clinically more apparent in males
infections usually cause systemic disease
infection transmitted from mother to child in utero or during birth
Herpes
caused by HSV
HSV-1 usually caused “cold sores” in mouth/lips
both types produce life-long infection, but virus usually remains dormant
drugs can reduce outbreaks
active genital herpes produces painful blisters at infection site
Bacterial STD infections
syphilis: a corkscrew-shaped bacteria (spirochete)
chlamydia: obligate intracellular bacerium, very common STF
Gonorrhea: bacterium, very common STD
Trichomonas: parasite
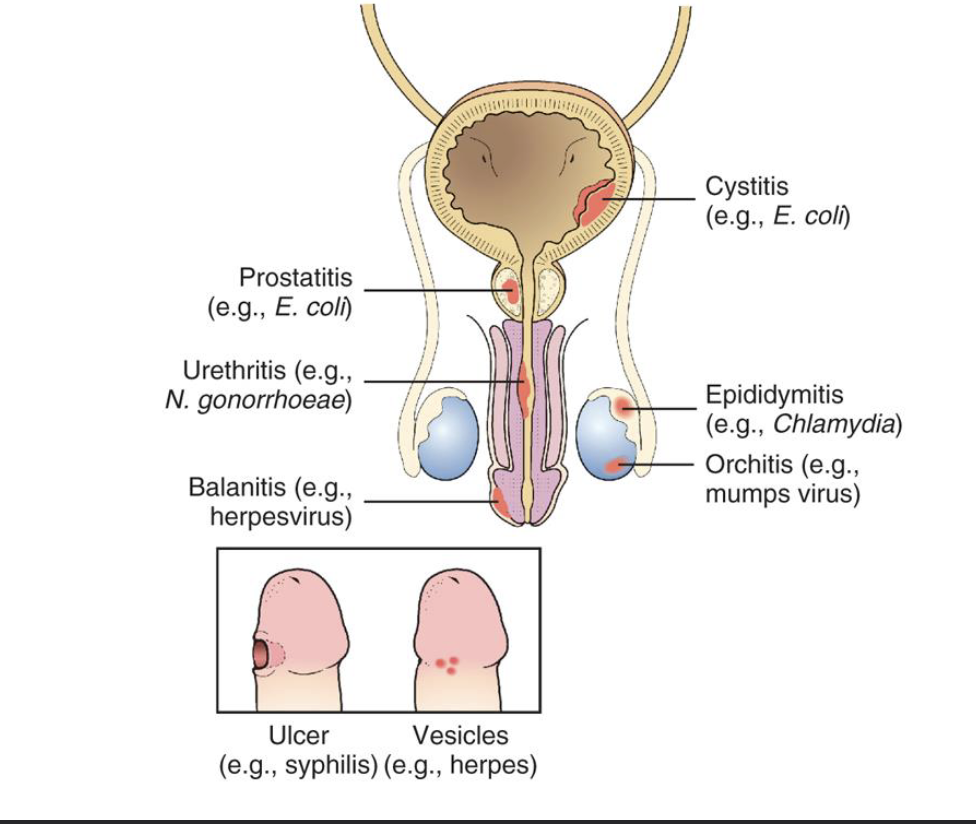
bacterial infections cause Urethritis: inflammation of urethra, often with a discharge of a purulent exudate (pus)
co-infection with more than 1 STD is common!
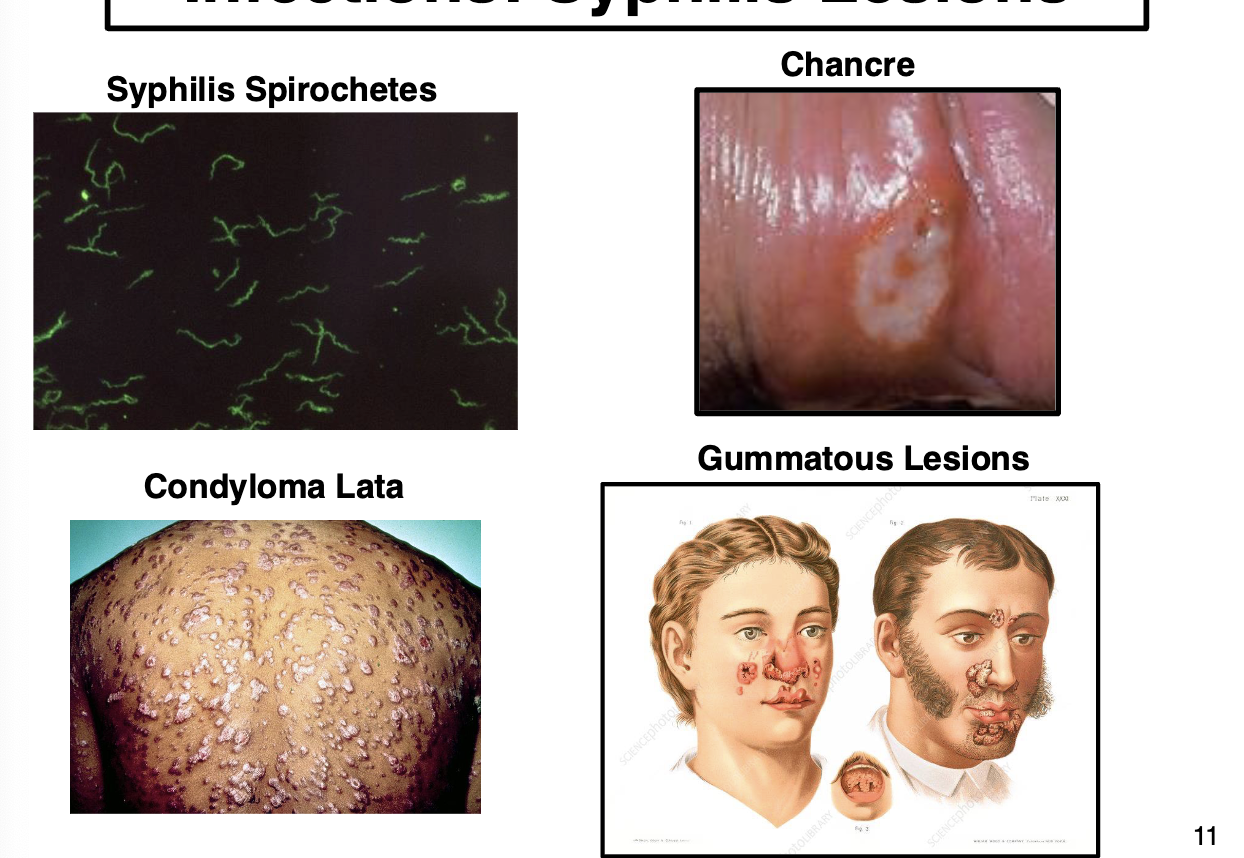
Syphilis
caused by Treponema pallidum. Infection has 3 distinct stages if not treated
Primary syphilis: characterized by a chancre, a solitary painless ulceration at site of infection, appear ab 1-3 weeks after exposure, may persist for 3-6 weeks w/o treatment
secondary syphilis: characterized by a systemic spread of spirochetes and a skin lesion known as Condyloma lata, multiple slightly raised lesions, appear 2 months to 2 yrs after infection
tertiary syphilis: rare, characterized by a lesion known as Gumma, soft and rubbery non-cancerous growth filled granulomas, appears 2-20 yrs after infection, can be very disfiguring. Can also involve ❤ and CNS
Balanitis
inflammation of the head and foreskin of the penis
largely idiopathic but known association with genital herpes
affects 11% of adult men and 3% of children
much more common in uncircumcised males
Orchitis
inflammation of the testes
usually associated viral infections (mumps)
Prostatitis
inflammation of the prostate gland
usually an acute illness with fever, back pain, dysuria and other urination problems
usually infection with GN uropathogens, E. coli is a frequent cause
location of the prostate males inflammation/infection of this gland a painful lesion
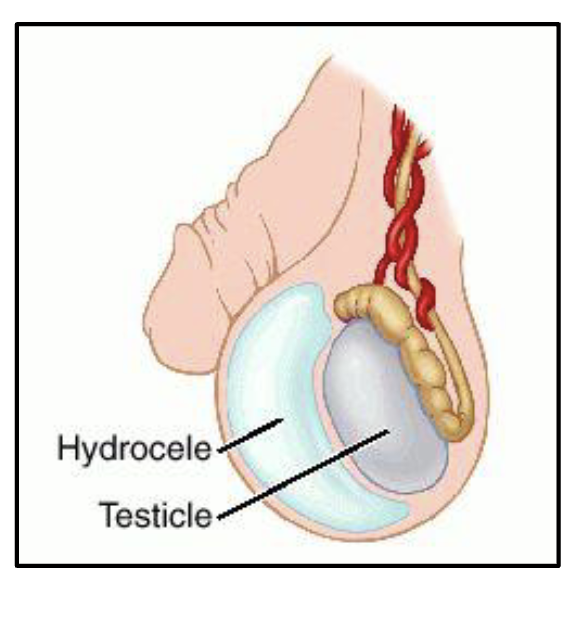
Hydrocele
Accumulation of fluid around a testicle, this is relatively common
caused by fluid secreted from the tunica vaginalis
a simple method of diagnosing a hydrocele vs a tumor is to shine a strong light through the enlarges scrotum
hydrocele will usually allow light to pass
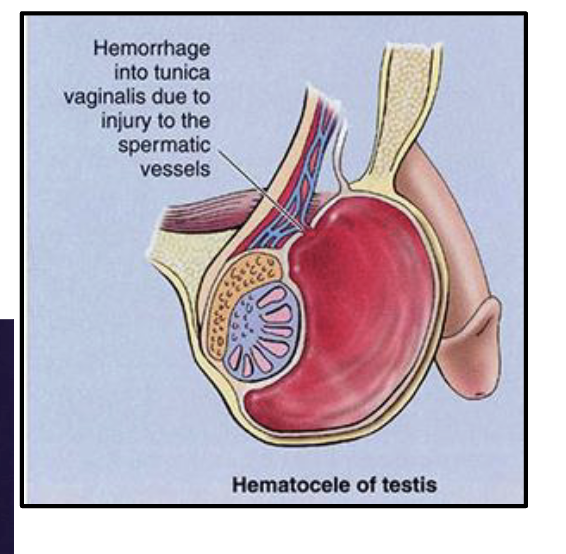
Hematocele
collection of blood in the tunica vaginalis caused by trauma to testes
more painful than a hydrocele
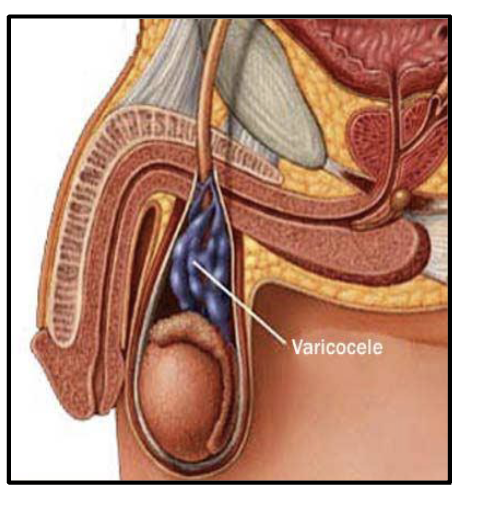
Varicocele
abnormal enlargement of the venous plexus of the scrotum (pampiniform plexus) which drains the testicles
cause:
defective valves
compression of vein
usually harmless but may affect infertility
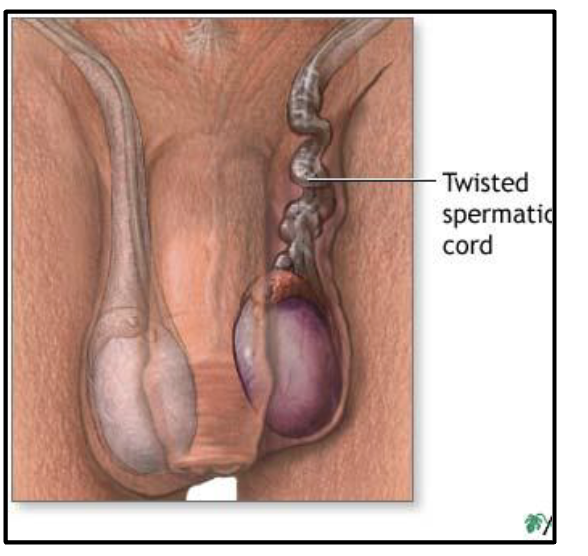
Testicular torsion
a urologic surgical emergency
very painful condition
delay in diagnosis and treatment can lead to infarction and loss of the testicle
requires surgery, time is key factor for preservation of testicle:
<6 hrs -90%
12 hrs - 50%
24 hrs - 10%
>24 hrs - 0%
Benign Prostatic Hyperplasia (BPH)
increase in size of prostate due to glandular hyperplasia
highest in males of African lowest in males of East Asian
BPH does NOT predispose to prostate cancer
causes multiple symptoms relating to urination, increased size may obstruct urethra and increase infection risk
Male genital tract tumors
penis: squamous cell carcinoma of skin (HPV may be a cause)
prostate: adenocarcinoma
testis: cancer of young men, incidence peaks ages 24-45
testicular cancers respond well to chemotherapy and have a 5-yr survival rate >90%
Rule of 90’s for testicular cancer: 90% age 25-45, 90% germ cell tumors, 90% malignant, 90% curable
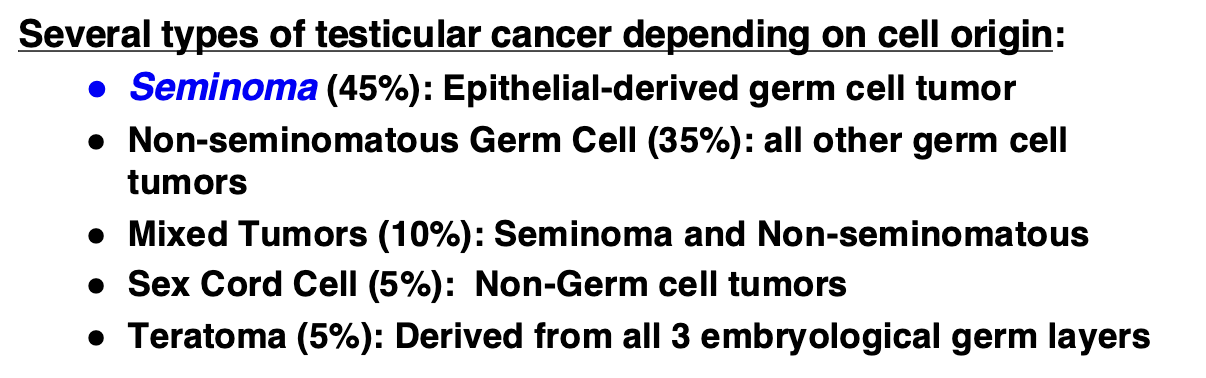
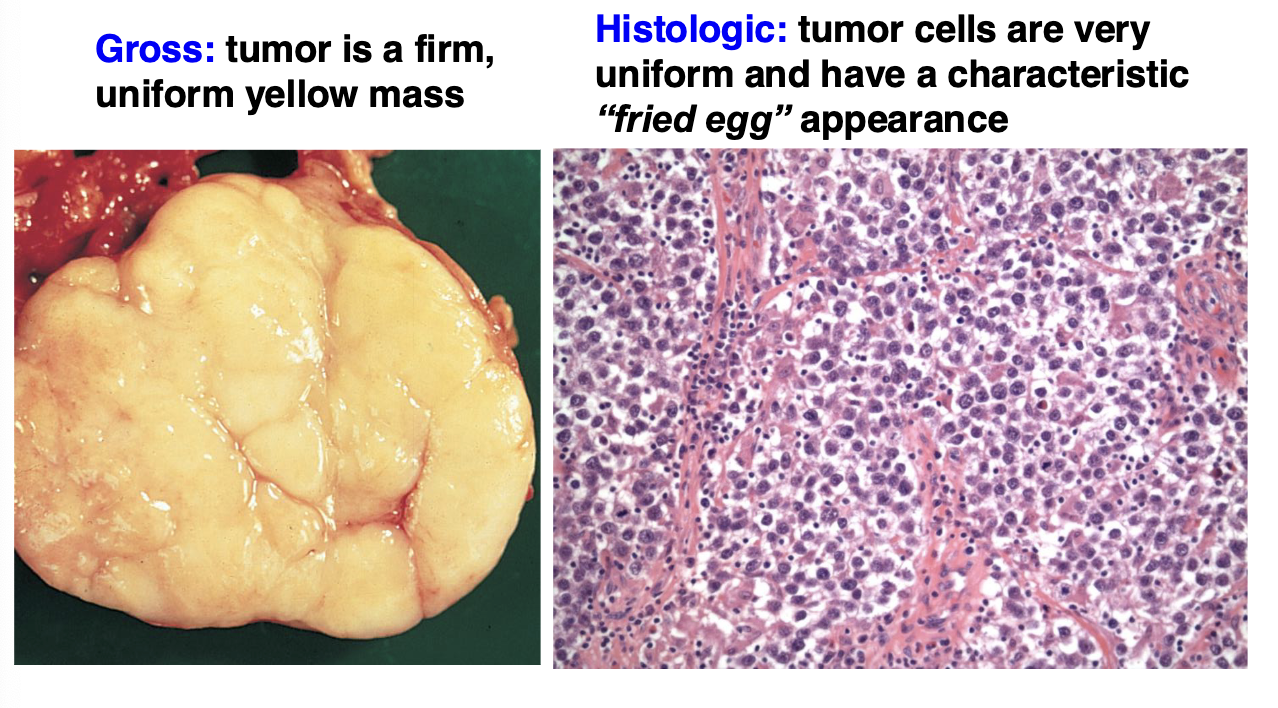
Testicular seminoma
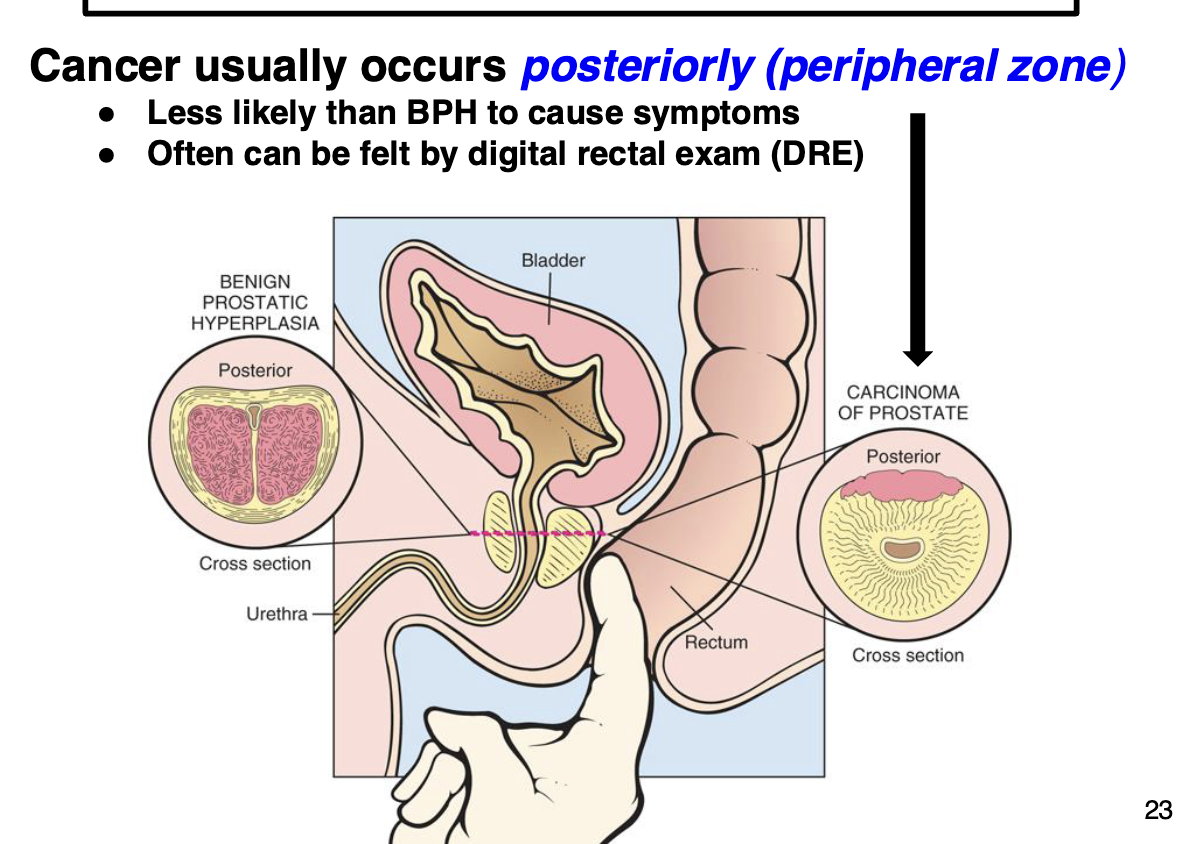
Prostatic adenocarcinoma
most common male cancer (non-skin) in the US
2nd leading cause of cancer-related deaths in males
incidence increases with age (cancer of old men), but incidence and mortality rates in US are declining
no specific symptoms, usually clinically silent, urinary symptoms sometimes can mimic nodular hyperplasia (BPH)
some men may present with severe back pain due to metastasis to vertebral bone (most often with aggressive form)
treatment for localized (non-metastatic) cancer is effective
Neuroendocrine carcinoma
aggressive prostate cancer variant that is R to treatment
metastasizes early in disease and has poor survival
ab 1% of total prostate cancer cases
Prostate specific antigen (PSA)
protein produced by cells of the prostate gland
blood test measures circulating levels of PSA
FDA has approved of PSA blood test along with digital rectal exam (DRE) to screen for prostate cancer in men 50 and older
PSA test is also approved to monitor patients with a history of prostate cancer for recurrence
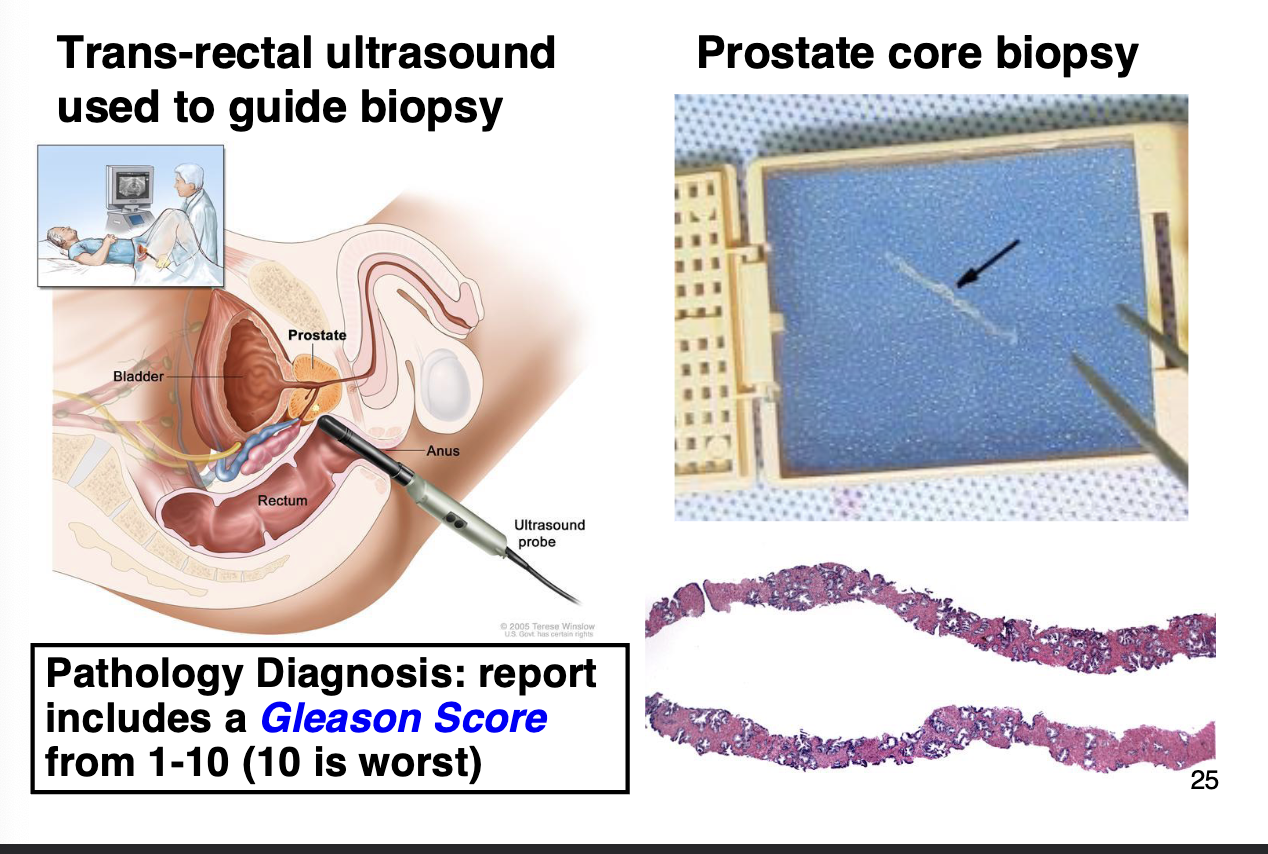
Prostate cancer diagnosis
Cystitis
inflammation of the urinary bladder
many causes including UTI, trauma (catheter), kidney stones, collateral dmg radiation or chemo
most caused by ascending infection with fecal bacteria (E. coli)
more common in females, children, elderly, individuals confined to bed
acute cystitis caused by UTI is very effectively treated with short course of antibiotics
Carcinoma of the urinary bladder
4 types depending on cell from which the cancer developed
primary cause is cigarette smoking and/or occupational exposure to chemicals
peak incidence ages 55-80, more common in males (M:F = 3:1)
less invasive and less prone to metastasize than other cancers
surgical resection is preferred treatment
most tumors (70-75%) are low grade with good prognosis
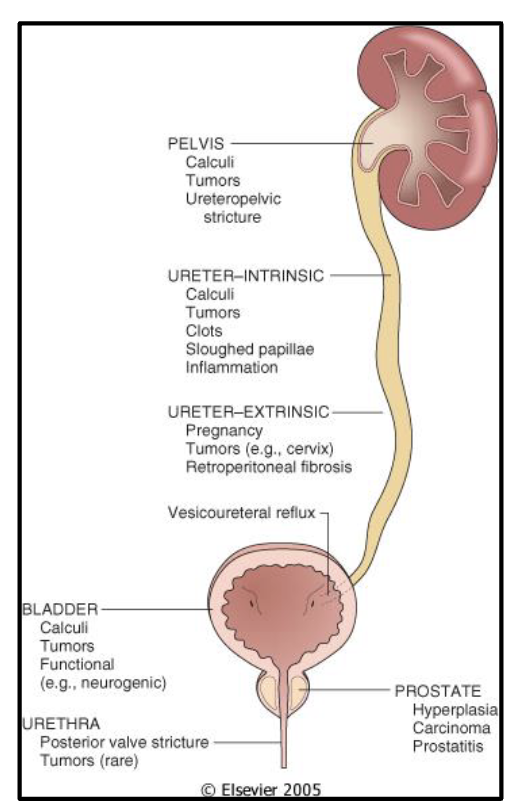
Urinary tract obstructions
any obstruction will predispose to an infection (usually bacterial)
urinary tract can be obstructed by many processes
in each case infection is a potential complication
Congenital: Ectopic kidney
kidney is located in an abnormal position
there are several different variants depending on location
usually doesn’t cause issues
less often, the ectopic kidney may cause problems such as urine blockage, infection, or urinary stones
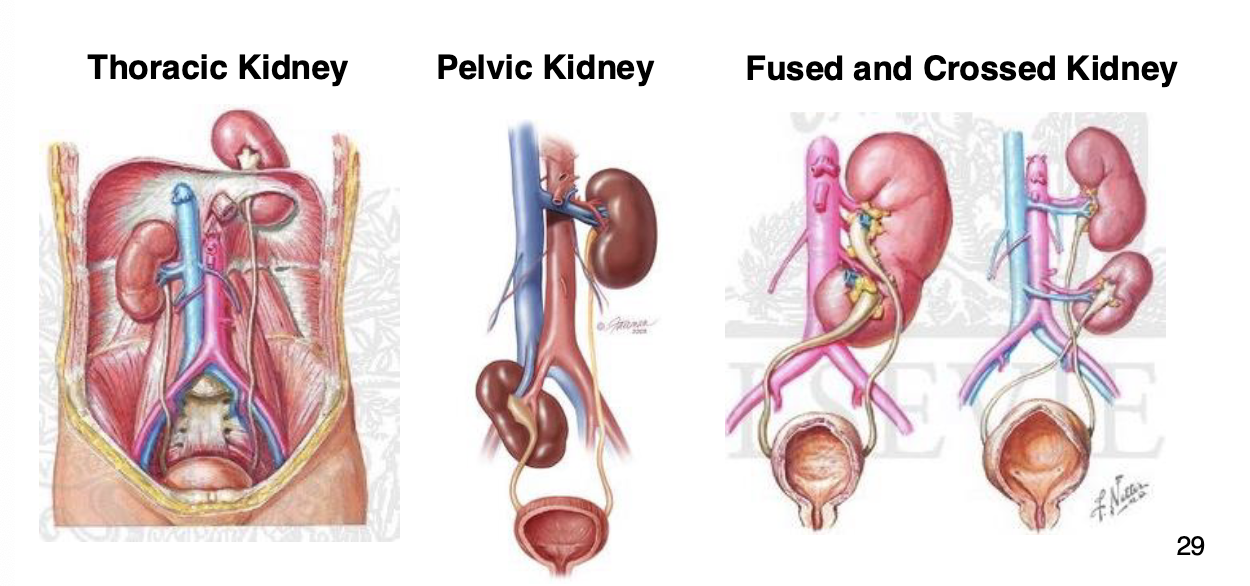
Congenital: horseshoe kidney
both kidneys are fused tgt at the midline as a single organ
associated with chromosomal defects: Turner syndrome (one X chromosome) Edwards syndrome (Trisomy 18)
can also occur as an isolated anomaly in about 0.1 to 0.2% of the general population
usually asymptomatic
Congenital: Dysplastic kidney
AKA Multicystic dysplastic kidney (MCDK)
malformation during fetal development resulting in disorganized architecture of the cortex and medulla
usually only 1 kidney, often with minimal clinical impact
degree of abnormality (cysts) will determine kidney function
multiple cysts often cause urinary tract obstruction

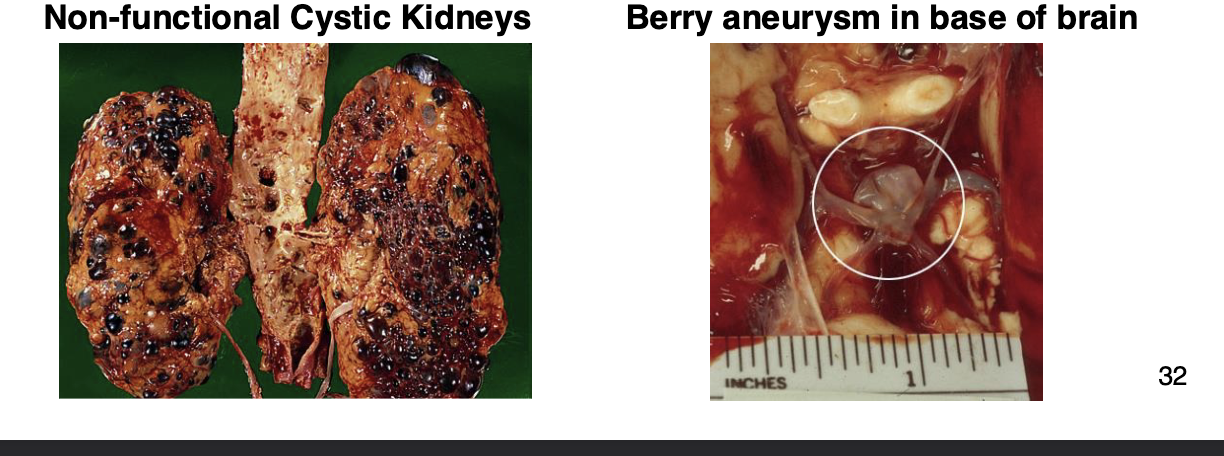
Hereditary: Autosomal dominant polycystic kidney disease (ADPKD)
common inherited disorder: affects 1 in 500 persons
disease usually presents in the early-mid 40’s with hypertension and urinary problems (infections, hematuria)
cysts lead to renal failure, 10-15% of ADPKD are on dialysis
ab 1/3 of ADPKD have berry aneurysms in the brain, Brain hemorrhages account for up to 10% of deaths in ADPKD patients
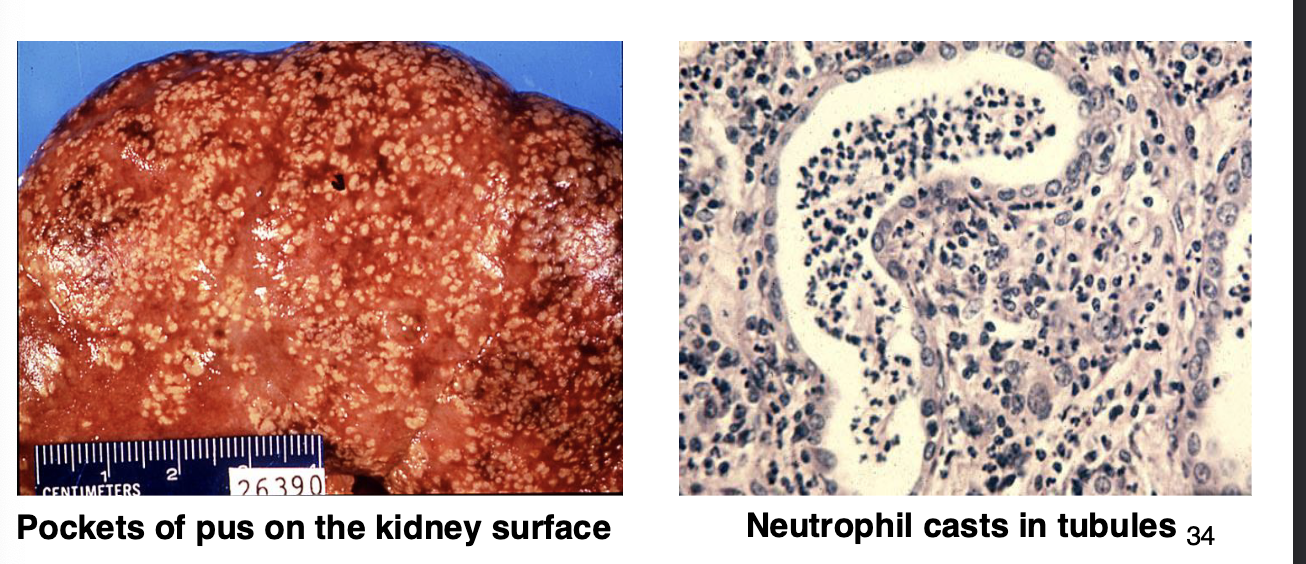
Pyelonephritis: Kidney infection
inflammation triggered by a bacterial infection
infection can involve renal parenchyma, calyces or pelvis
over 80% of infections arise from an ascending UTI with fecal bacteria (E. coli and others). UTI involving kidney is a complicated UTI and is more difficult to treat
10% are caused by a blood infection due to bacteremia, often with Staphylococcus (IV drug use)
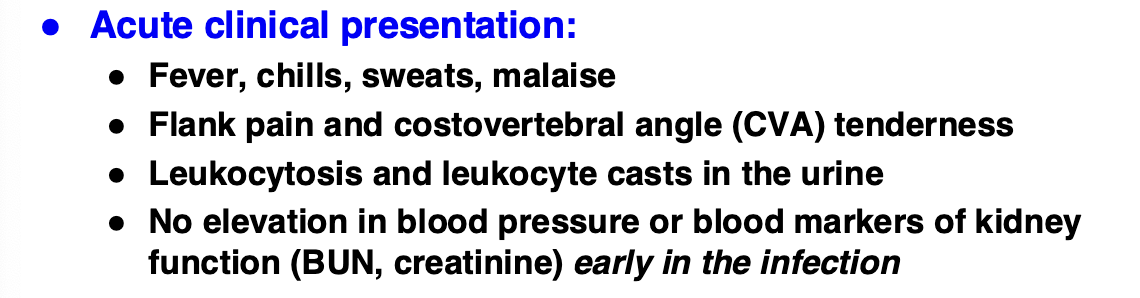
Acute pyelonephritis
critical that antibiotic treatment is prompt and complete
acute pyelonephritis can progress rapidly to sepsis and death
chronic pyelonephritis: may develop in persons with a structural defect of the kidney, very difficult to treat, results in destruction of the kidney
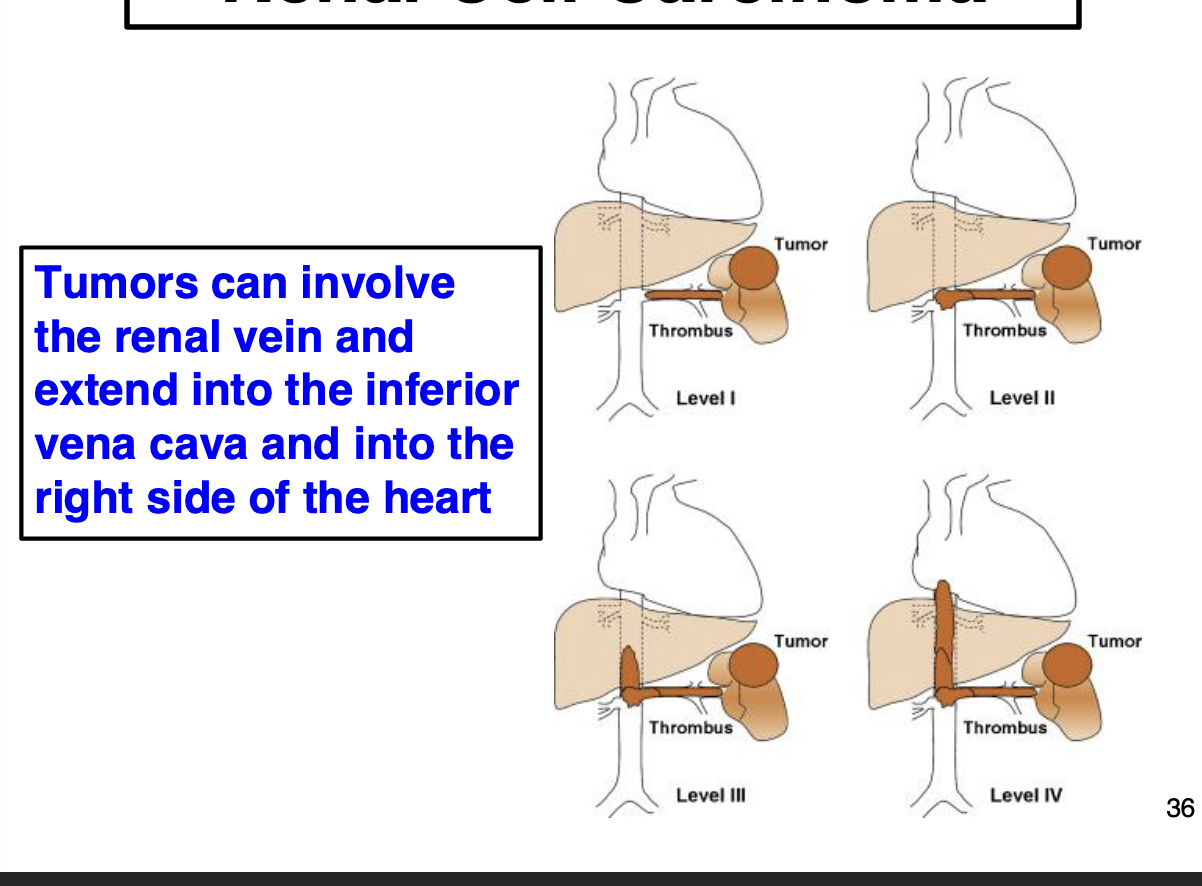
Renal cell carcinoma
tumors may arise anywhere in the kidney, but more often it affects the hilum
tumors are spherical solid masses, which can vary in size (often large)
characteristic color: bright yellow-gray-white
necrosis and hemorrhage are common
can invade extend into renal vein and inferior vena cava
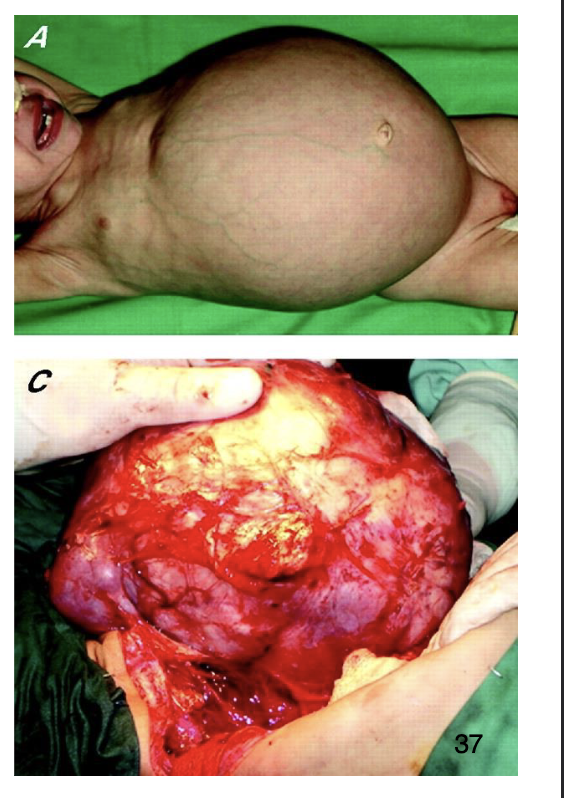
Wilms tumor (Nephroblastoma)
most common kidney tumor of childhood (ages 2-5)
90% are sporadic, less than 10% associated with WT1 or WT2 mutations
Presents as large abdominal mass
responsive to surgery and chemotherapy, 90+% cure rate
increases risk of developing other cancers (leukemia)
Kidney disease related to blood (ends with emia)
Azotemia: accumulation of nitrogenous wastes in the blood: creatinine and blood urea nitrogen (BUN)
Uremia: azotemia with clinical signs of kidney disease
Hyperkalemia: elevated blood potassium lvls (can cause sudden cardiac arrest)
Kidney disease relate to urine (ends with uria)
Anuria: no production of urine (<50ml in 24 hrs)
Dysuria: pain during urination
Hematuria: blood in the urine
Oliguria: decreased urine production (<400ml in 24hrs)
Polyuria: excessively increased production of urine (as in diabetes)
Proteinuria: protein (largely albumin) in the urine
Pyuria: pus in urine
Major kidney functions
removal of waste products and foreign substances
regulation of plasma ion composition: sodium, potassium, calcium, magnesium, chloride, bicarbonate, phosphates
regulation of plasma volume
regulation of blood pH (acid-base balance)
secretion of renin: regulates BP
secretion of Erythropoietin: stimulates erythrocyte production
activation of vitamin D: converts the stable 25-hydroxyvitamin D to the active steroid hormone 125-dihydroxyvitamin D
The nephron
functional unit, ab 1 million per kidney
Nephron = Glomerulus (filtering unit) + Tubule (collects filtrate)
kidney can only function normally with only 25% of total filtering capacity (functional nephrons)
Glomerular blood supply
glomerular capillary bed is the only one to have arterioles on both sides
blood enters glomerulus via the afferent arteriole →
branches into extensive capillary network →
capillaries converge to form the efferent arteriole (E for exit, A before E)
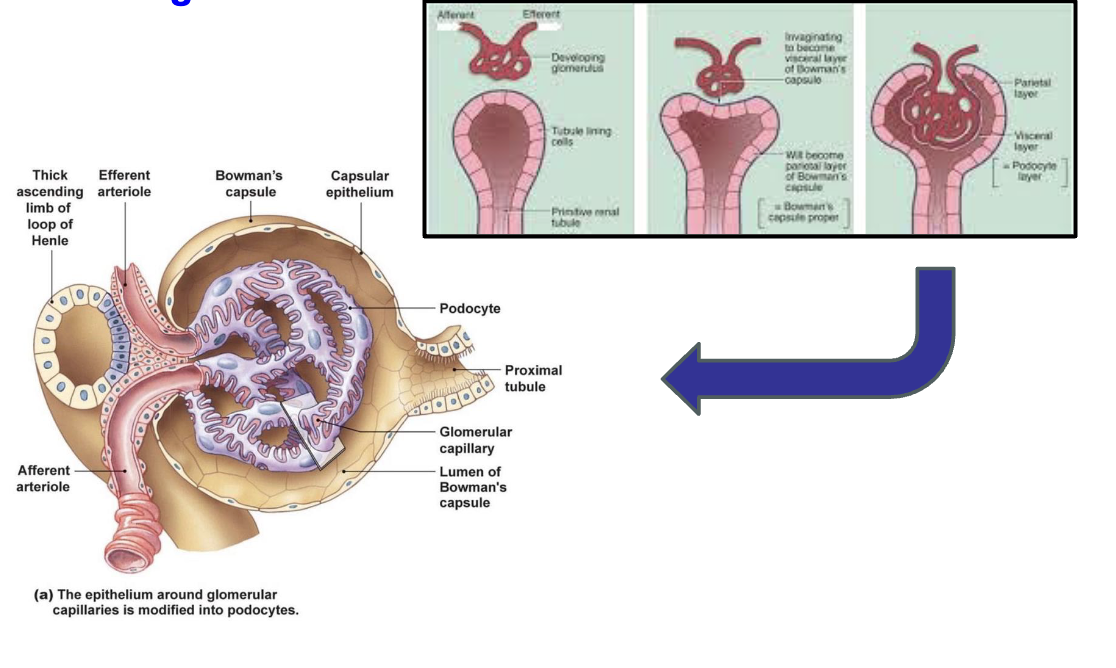
Glomerulus: development
during embryological development, arterioles “push” into the tubules
additional cell types are created and mature into functional glomerulus
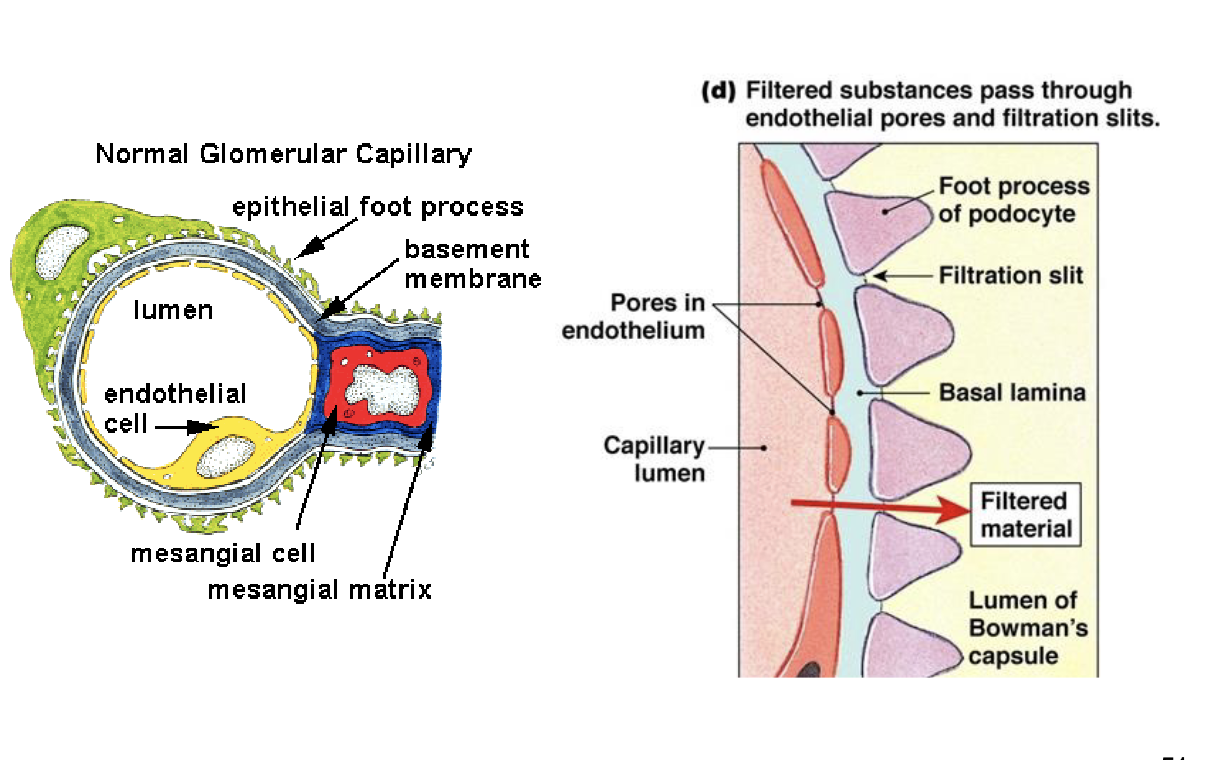
Endothelial cells (EC)
specialized type known as fenestrated endothelial cells
they line the capillary loops, have large pores in their cytoplasm that function as the 1st part of the glomerular filtration barrier
Glomerular basement membrane (GBM)
specialized basement membrane (thicker with diff connective tissue proteins) that separates endothelial cells from the podocytes (both cell types make the GBM)
This GBM functions as the 2nd part of the glomerular filtration barrier
Podocytes (glomerular epithelial cells)
large specialized epithelial cells with long cytoplasmic extensions that form “foot processes” that wrap the GMB and ECs
foot processes of adjacent podocytes interdigitate to form slit pores
function as the 3rd part of the glomerular filtration barrier
Bowman’s space
after blood is filtered through the glomerular filtration barrier the filtrate is captured in this space before entering the proximal convoluted tubule
bowman’s space is continuous with the proximal tubule
Mesangial cells & mesangial matrix
function as “maintenance” cells of the glomerulus
both cells and matrix tgt function as an “anchor” to hold the capillary loops tgt and maintain integrity of the glomerulus
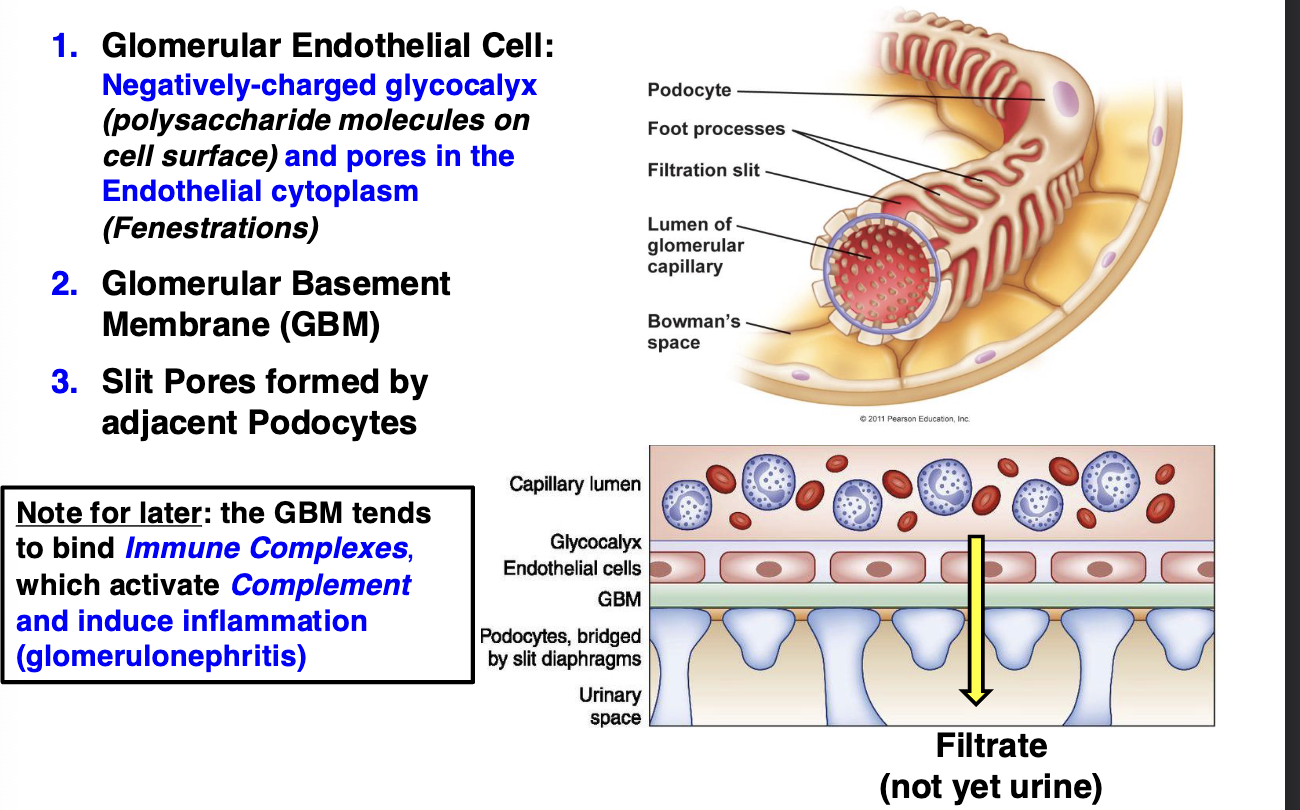
Glomerular filtratoin barrier
Glomerular endothelial cell: negatively-charged glycocalyx (polysaccharide molecules on cell surface) and pores in the endothelial cytoplasm (fenestrations)
glomerular basement membrane (GBM)
slit pores formed by adjacent podocytes
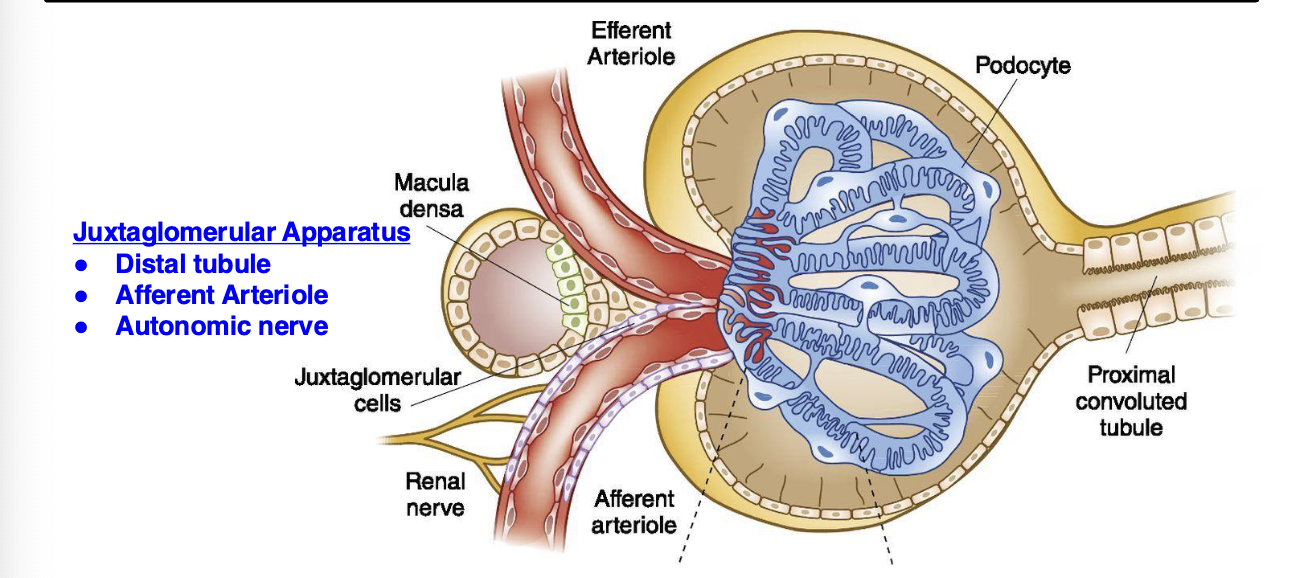
Glomerulus: blood pressure regulation
afferent arterioles adjacent to distal tubule can dilate or constrict based on the composition of the filtrate
this regulates BP
if BP is too low, juxtaglomerular cells secrete renin
results in arteriole constriction to increase BP and tubules retains/reabsorbs salt from filtrate
Nephron tubules
Proximal tubule: reabsorption of many molecules (including proteins) in the filtrate back into blood. Proximal tubule epithelial cells also activate vitamin D
Loop of Henle: water and salt reabsorption
Distal tubule: concentrates filtrate, BP regulation
collecting ducts: at this point filtrate is now urine
Calyx
Pelvis
Ureter
Urinary bladder
Glomerulonephritis
Inflammation of glomeruli
not a single disease but broad term used to refer to many types of inflammatory conditions that most often affect both kidneys
children: 95% is primary kidney disease
adults: 60% primary disease 40% secondary to diabetes
Causes of glomerulopnephritis
immune-mediated
metabolic
circulatory
methods of classification:
clinical syndrome: nephritic vs nephrotic
glomerular pattern: proliferative vs. non-proliferative
Causes of glomerular pathology
Immune-mediated: most significant mediator of glomerular damage
abnormal immune response to infections and autoimmune diseases are major causes
involves both immune complexes and anti-GBM antibodies that activate complement, which then will recruit and activate neutrophils that damage the glomeruli
Metabolic: diabetes induces a specific type of glomerular disease. Kidney failure is the major cause of death in diabetics
Circulatory: anything that reduces BF to the kidney that can lead to renal failure
disseminated intravascular coagulation (DIC) often triggered by bacterial sepsis is a major cause
Clinical presentation of glomerular injury (nephritic)
Azotemia: nitrogenous wastes in blood
Hematuria: blood in urine
Hypertension: high BP
Oliguria: decreased urine production
Clinical presentation of glomerular injury (nephrotic)
edema: generalized edema due to water retention
Proteinuria: protein (mostly albumin) in the urine
hyperlipidemia: increased lipids in blood (this is variable and not always observed in the nephrotic syndrome)
Nephritic syndrome
Glomeruli are “clogged” due to inflammation and glomerular hypercellularity: resulting in decreased filtration
decreased filtration causes oliguria and azotemia
kidney will increase BP (hypertension) for filtration
increased BP forces RBCs through damaged glomerular filtration barrier (hematuria)
nephritic syndrome diseases have increased cells in the glomerulus (hypercellularity) and are classified as Proliferative
nephrotic syndrome
glomerular filtration barrier is damaged “leaky” so that protein is lost in the urine (proteinuria) faster than can be replenished
loss of protein in the blood (hypoalbuminemia) decreases the oncotic pressure in the microvasculature, allowing fluid to accumulate in tissues (edema): generalized edema
there is a compensatory increase in proteins and lipoproteins by the liver, but lipoproteins (main lipid carriers) are not lost in the urine so there often is hyperlipidemia
usually do not have increased # of cells in glomerulus, classified as non-proliferative
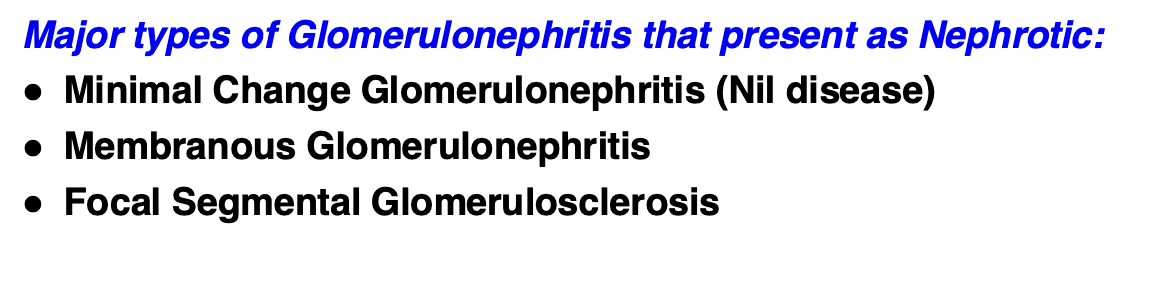
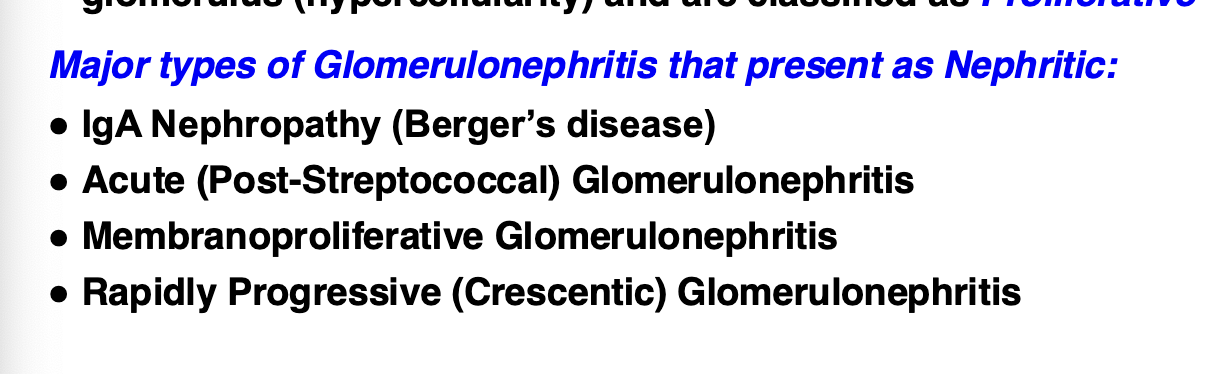
Diagnosis of glomerular disease
must use special lab techniques for precise diagnosis of the type of glomerulonephritis, which will determine treatment
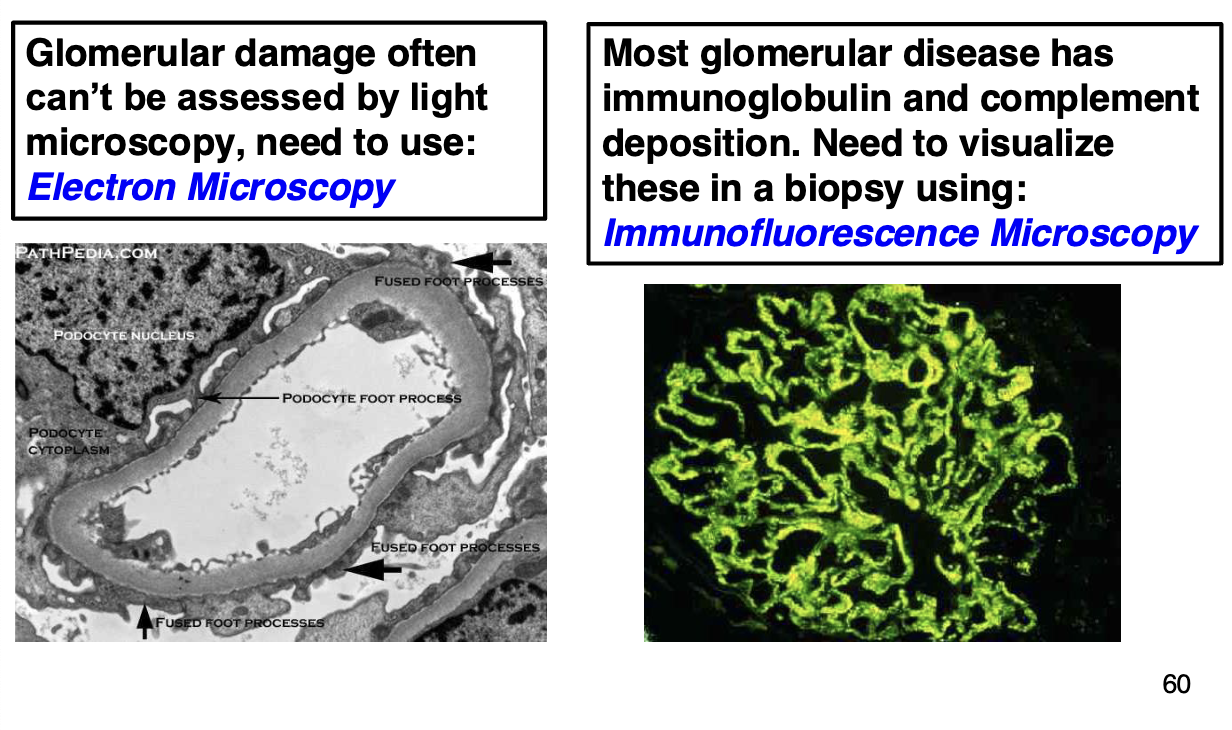
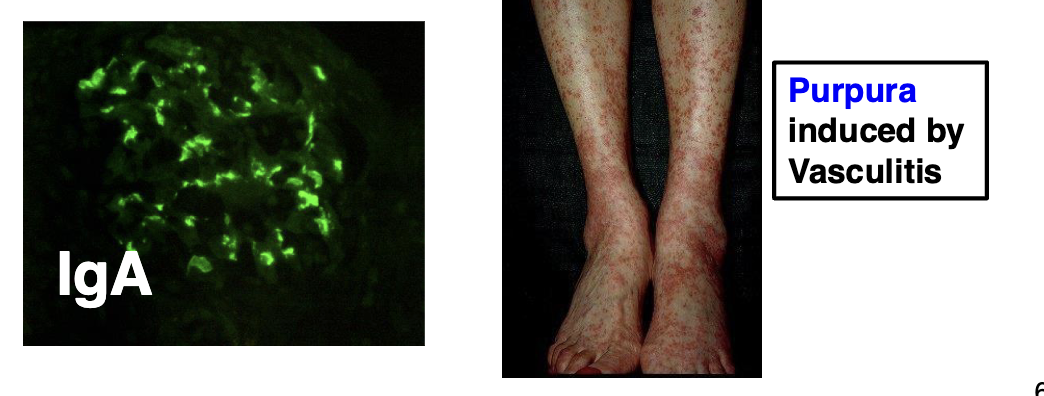
Nephritic: IgA nephropathy
most common form of glomerulonephritis world-wide, mainly affects young adults (16-35)
characterized by glomerular deposition of IgA antibodies and complement
most causes are idiopathic, but may occur after flu-like illness, also occur in association with a type of small-vessel vasculitis
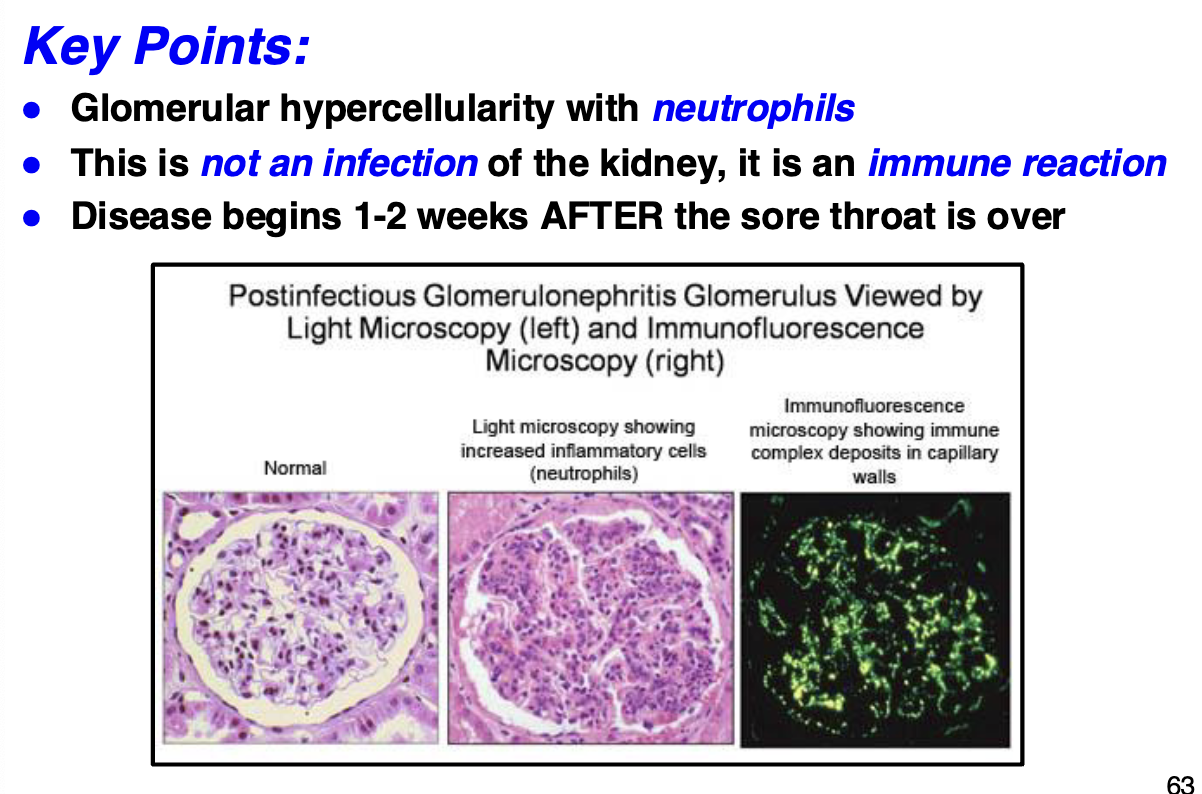
Nephritic: acute glomerulonephritis
disease prototype is post-infectious glomerulonephritis usually after group A B-hemolytic streptococci infection
usually in children, in ab 1-3% cases this occurs ab 1-2 weeks after strep throat infection
prompt antibiotic treatment can prevent possible kidney damage
95% recover, 5% progressive to chronic renal disease
glomerular inflammation caused by an autoimmune reaction of to glomerular (self) antigens (anti-glomerular IgG antibodies)
immune complexes induce Type III hypersensitivity reaction and activate complement, that recruit neutrophils
glomerular histology shows diffuse proliferation of glomerular cells and presence of neutrophils
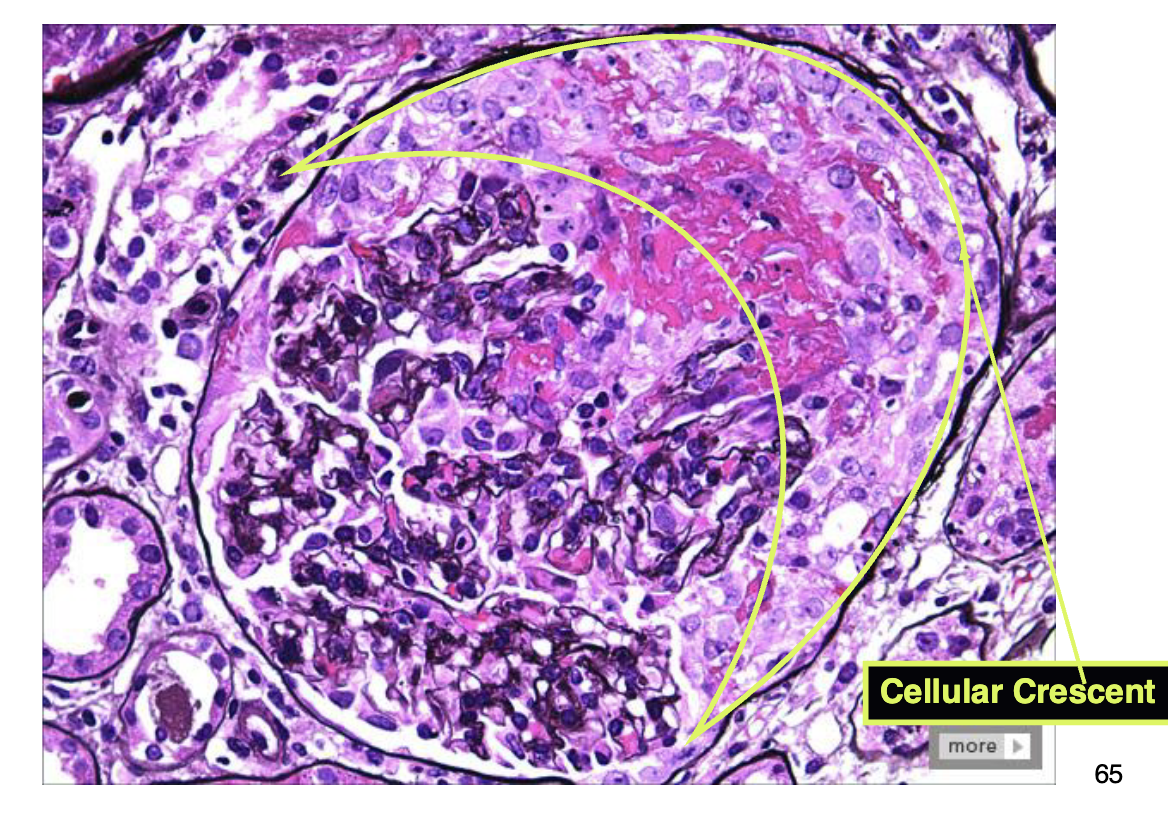
Nephritic: rapidly progressive (Crescentic) Glomerulonephritis (RPGN)
rapid and progressive destruction of glomeruli, can result in renal failure within weeks to months
the classic histologic picture is presence of crescents (hypercellularity with fibrin) in the glomeruli which obliterate Bowman’s space
many causes, often autoimmune diseases, example is Goodpasture’s syndrome: anti-GBM (also affects lungs)
grossly, kidneys are swollen, pale with “flea-bitten” petechial hemorrhages on the kidney surface
only treatment is dialysis and kidney transplant
Nephritic: membranoproliferative glomerulonephritis (MPGN)
MPGN accounts for 10-20% of glomerulonephritis cases in children and young adults
presents as mixed nephritic/nephrotic syndrome
many causes, post-infectious reaction and/or autoimmune diseases
the classic histologic pictureL thickening of GBM, proliferation of glomerular cells and presence of neutrophils
complement activation plays a major role in MPGN pathogenesis
slowly progressive unremitting course that eventually requires transplant (50% of cases 10 yrs after diagnosis)
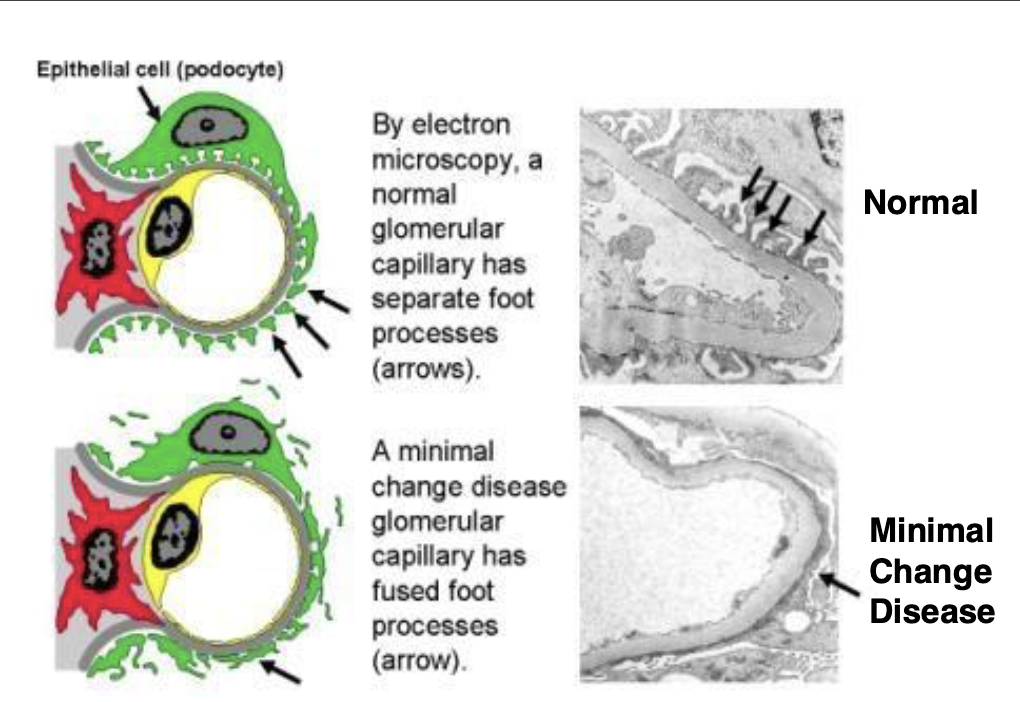
Nephrotic: minimal change glomerulonephritis
Also known as Nil Disease since no abnormalities found by light microscopy, requires electron microscopy to see pathology
Occurs mainly in children (2-6 years old) and is most common
kidney disease of childhood, generalized edema (anasarca) is the most prominent clinical sign
Relatively benign disease that doesn’t progress to renal failure
Unknown cause, there are NO immune complexes or complement activation
By light microscopy glomeruli appear normal, but electron
microscopy shows fusion of the podocyte foot processes
Corticosteroid therapy is effective, long-term prognosis is good
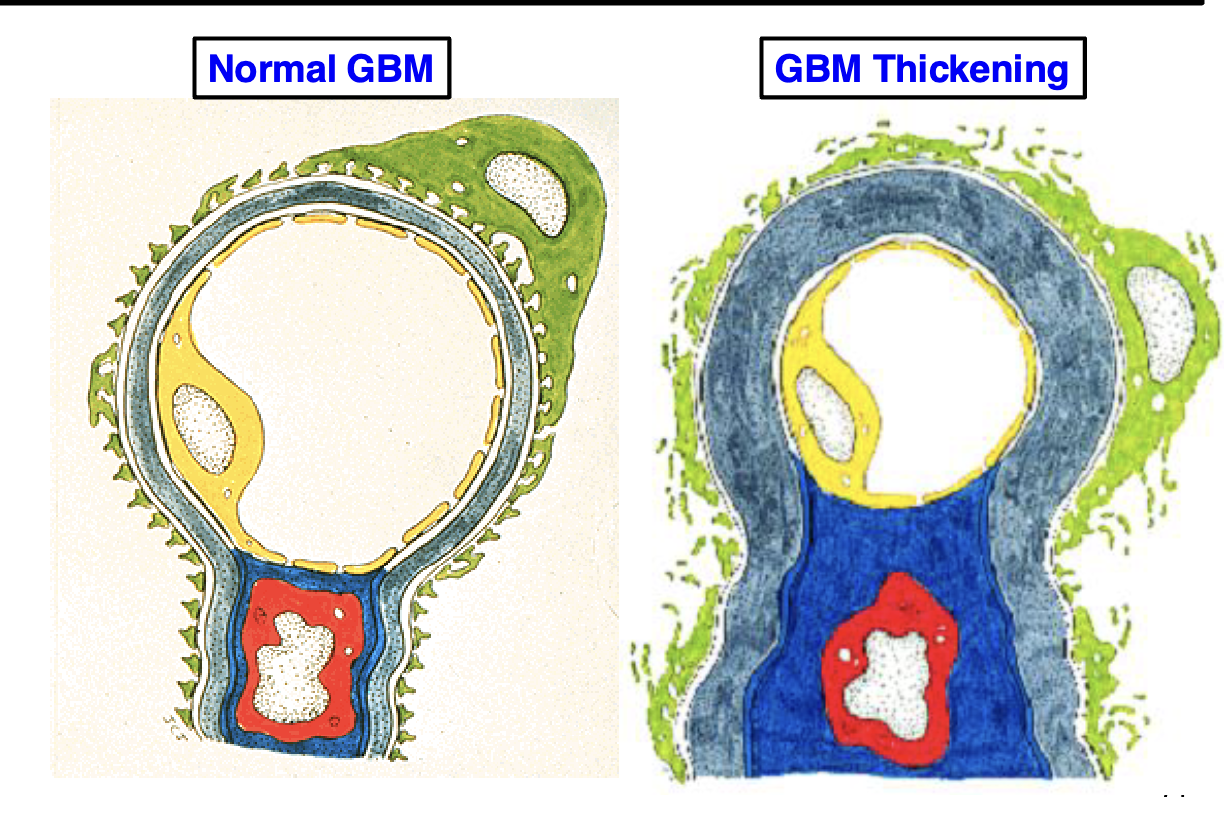
Nephrotic: membranous gelomerulonephritis
Most common cause of primary kidney disease in adults, most often persons in their 50’s and 60’s
Usually idiopathic, but can occur as a secondary reaction to autoimmune diseases (SLE), cancers, reaction to drugs
Glomerular pathology is characterized by thickening of the glomerular basement membranes and leakiness of the glomerular capillaries
Corticosteroid therapy is somewhat effective, but 50% have a slow progression to renal failure
Nephrotic: Focal segmental Glomerulosclerosis (FSGS)
Most common cause of adult proteinuria in the U.S.
Usually idiopathic, but can occur in association with autoimmune diseases (SLE), IV drug abuse, HIV infection
Increased collagen deposition affects only a portion of each glomerulus (segmental) and is focal
Less than 50% of glomeruli are affected
HIV nephropathy: a more severe variant of FSGS associated with HIV infection
Most persons progress to renal failure 5 to 10 years after diagnosis
Acute interstitial nephritis:
somewhat common, many cases could be sub-clinical
toxins (plant and fungal-derived) and certain drugs (antibiotics and NSAIDS) are known to trigger
possibly an allergic type reaction since serum IgE is increased and the kidney lesions have a large # of eosinophils
usually self-limiting, but severe cases may need dialysis while the tubules regenerate
Chronic interstitial nephritis
similar to acute but with a slow insidious onset
increased collagen deposition in the interstitial tissue surrounding tubules results in fibrosis causing renal failure
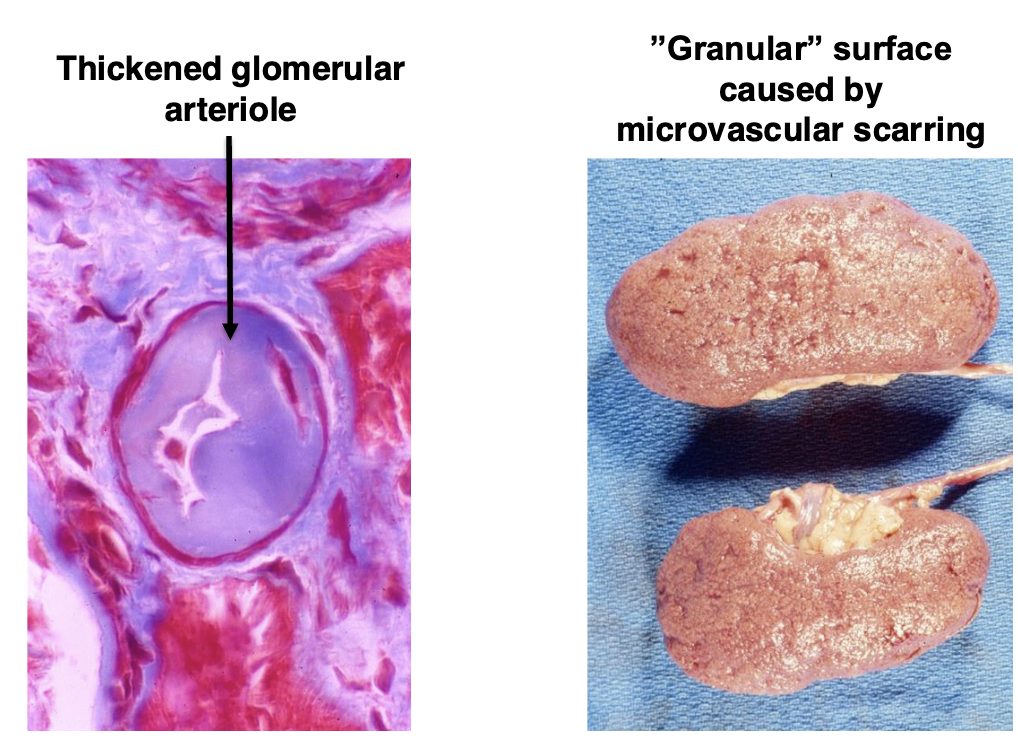
Hypertension
kidney can cause
kidney is a major target of dmg due to hypertension
perhaps most common cause of renal disease
2 major types:
essential hypertension (benign)
hypertensive crisis (malignant)
Essential hypertension
The typical common form of hypertension, >95% cases
Chronic and modest elevations in blood pressure
Stage 1 hypertension: 130-139/80-89 Stage 2: >140/90
Chronic hypertension causes kidney arterioles to thicken to cope with the increased arterial pressure
Arteriole thickening reduces blood flow and causes:
Shrunken kidney
Microvascular scarring with ”granular” surface
Hypertension may also lead to:
Cardiac hypertrophy (enlarged heart)
Atherosclerosis
Retinopathy
Strokes
Hypertensive crisis
Rare form of hypertension, less than 5% of cases, also called Malignant Hypertension (older term)
More acute than essential, presents as severe and rapid rise in blood pressure to greater than 180/120
This is a Medical Emergency, need to treat ASAP, may lead to rapid kidney failure and stroke
Very high pressures can cause hemorrhages in kidneys, brain and eyes
Kidney shows hemorrhage from damaged vessels with “flea-bitten”/ petechial hemorrhages (very similar to severe damage in RPGN)
Diabetes
diabetic are the largest group on dialysis and most end-stage renal disease patients are diabetics
fluctuations in blood glucose levels damage glomerular basement membranes and blood vessels
diabetic nephropathy
basement membrane becomes thickened and leaky
progressive kidney disease caused by arteriosclerosis of capillaries
increase in mesangial matrix
Nodular glomerulosclerosis (Kimmelstiel-Wilson disease)
kidney disease specific to long standing diabetes mellitus (type 1)
characterized by nephrotic syndrome, diffuse glomerulosclerosis and nodules of mesangial matrix
Systemic Lupus Erythematosus (SLE)
autoimmune disorder with antibodies against nuclear antigens
Immune complexes form and deposit in the kidney
Between 50 and 80% of SLE patients will develop Lupus Nephritis: Nephrotic syndrome characterized by a “full house” pattern of immunofluorescence staining of glomeruli (positive staining for all antibodies and complement proteins)
Several variants, but may cause renal failure
Amyloidosis
amyloid is insoluble aggregates of certain types of proteins that deposit in organs/tissues and interfere with function
deposits of amyloid in glomeruli cause a nephrotic syndrome
size of kidney increases due to deposits
can cause renal failure
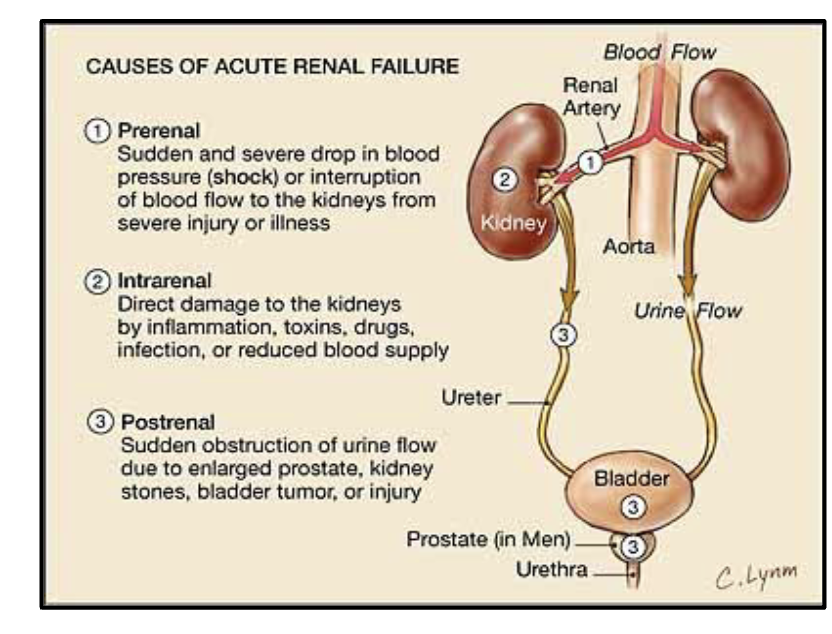
Acute renal failure
many causes:
trauma, shock, hypotension: reduces renal BF
acute infections/sepsis
acute toxicity from drugs/poisons or foods containing toxins
massive urinary outflow obstruction
problems when kidneys stop functioning
water retention and generalized edema
uremia
electrolyte imbalance: potassium can’t be excreted, and levels increase in the blood (hyperkalemia) which can cause arrhythmias and asystole
Chronic renal failure
AKA end stage renal disease
Azotemia and Uremia: Uric acid crystals may deposit on the tongue or eyelids, persons may give off an odor of urine
GI tract: Constipation, Diarrhea, Nausea and Vomiting
CNS: Muscle weakness, Headache, Retinal Damage, Delirium, Convulsions, Coma
Cardiovascular: Pericarditis, Anemia, Hypertension, Pulmonary Edema
Treatment needs to start early to minimize systemic affects
Once damage reaches a certain point, loss of function becomes
progressive, dialysis or transplant are the only options
Kidney transplantation
Hyperacute Rejection: Rejection is immediate due to pre-formed antibodies to endothelial cells, this usually is prevented by careful pre screening prior to transplant
Acute Rejection: Most common type, usually occurs in first 6 months due to T cells sensitized to donor kidney antigens
Chronic Rejection: Causes are not clear and difficult to manage and may require 2nd transplant