10 - Motor Systems 1
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
65 Terms
steps in voluntary goal-directed movements?
decision to move
identification and location of target
knowledge of position of limbs, body
formation of plan of action
execution of plan and action - control of both proximal and distal segments
(unconscious after the task is learned)
hierarchal vs parallel distributed processing in motor system
once thought as hierarchical, now considered as parallel descending systems
numerous regions of the central nervous system are required to plan and execute motor skills - there are series of parallel systems linking various motor areas of cortex more directly with spinal motor circuits
where are the motoneurons located in the spinal cord and brainstem?
spinal cord - predominantly L IX
brainstem - cranial nerve motor nuclei are in abducens, trochlear, oculomotor; hypoglossal, trigeminal motor, facial motor, nucleus ambiguus, spinal accessory
what does a motor unit innervate?
group of muscle fibers called a muscle unit - all contract together
review: muscle innervations, myotome levels and peripheral nerve innervation
—
why is lower motor neuron an inaccurate term?
much descending input goes to interneurons which help with coordinated function of motor units/muscles
there are motor neuron pools - distal/proximal, flexor/extensor
what are the central pattern generators? what do they do?
interneurons
create coordinated, multisegmental rhythmic cyclical motor activities - basic rhythm patterns
where do interneurons receive input from?
supraspinal centers for modulation to environmental conditions and sensory receptors that give feedback back to spinal cord
what else provides input to motor related interneurons and motoneurons (to a lesser extent)?
sensory, descending pathways, collaterals from motoneurons - agonists, antagonist
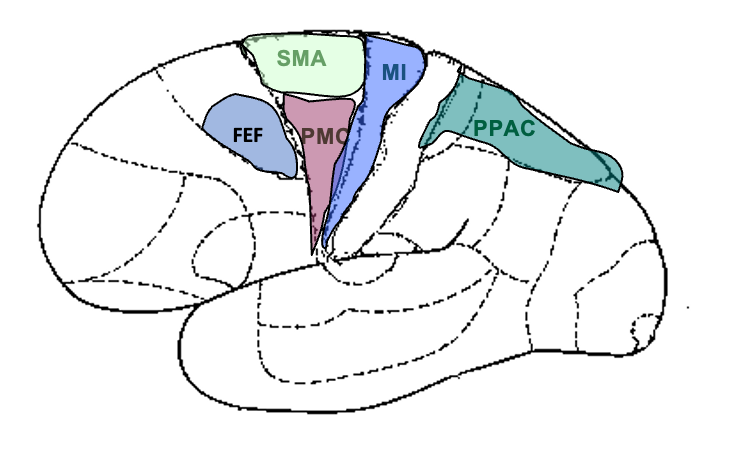
PMC vs SMA
PMC: more important for learning, planning, control of movements requiring visual or other sensory input (external info)
SMA: more important for initiation, planning, control of movements based on learned patterns, activity of SMA decreased as movement patterns become more automatic (internal info)
what are the primary motor tracts? where do they terminate?
corticospinal
vestibulospinal
reticulospinal
rubrospinal
tectospinal
*terminate primarily on interneurons
what part of the cerebrum controls motor activities?
M1, M2 (PMC, SMA), PPAC, cingulate gyrus
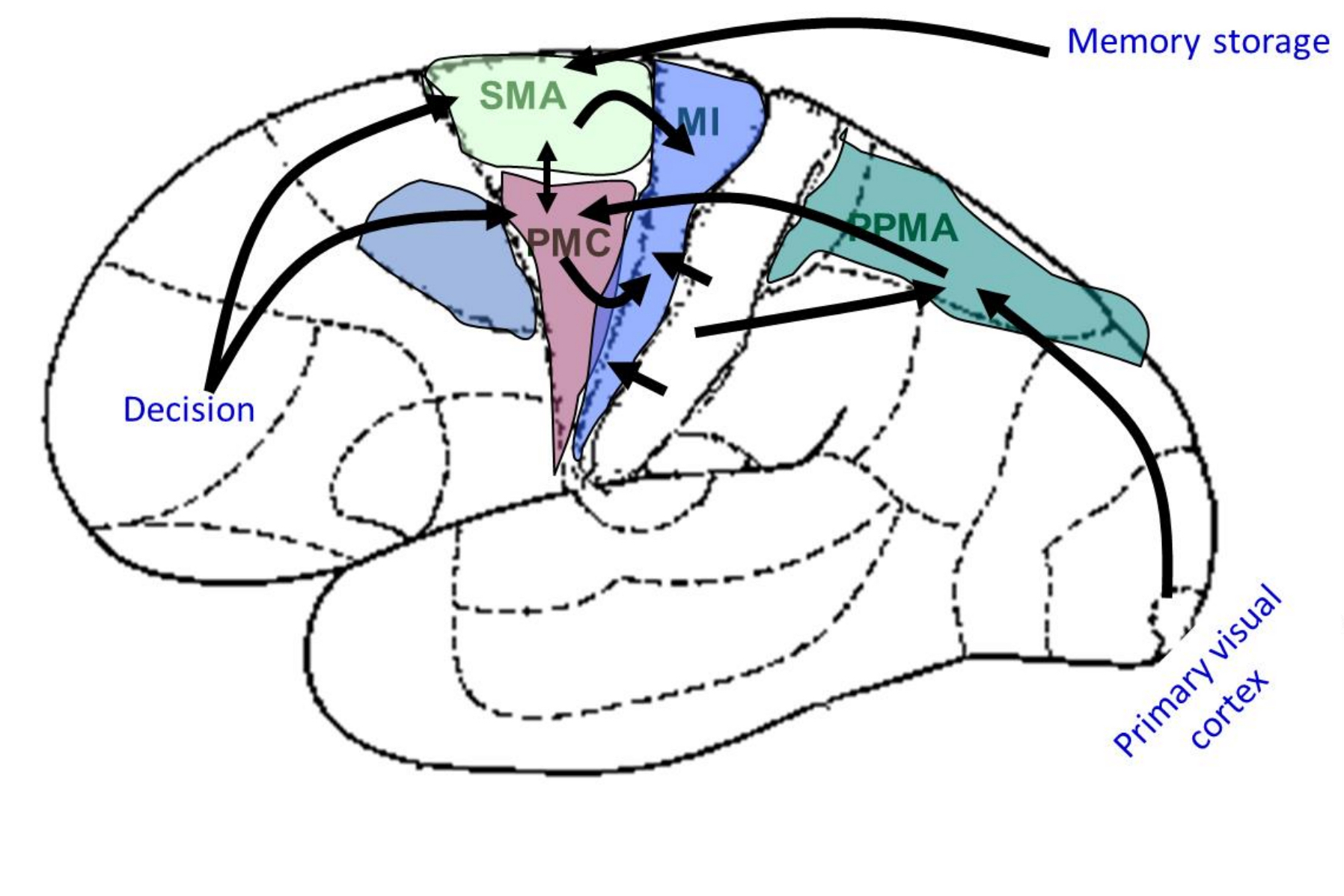
the cerebral cx interacts with the cerebellum and basal nuclei. what are the pathways?
M1: cerebral cx → pontine nuclei → cerebellum via middle cerebellar peduncle → thalamus (VL/VPL) → cerebral cx
SMA: cerebral cx → neostriatum (basal nuclei) → globus pallidus → thalamus (VA/VL) → cerebral cx
what brodmann’s area is the SMA?
area 6
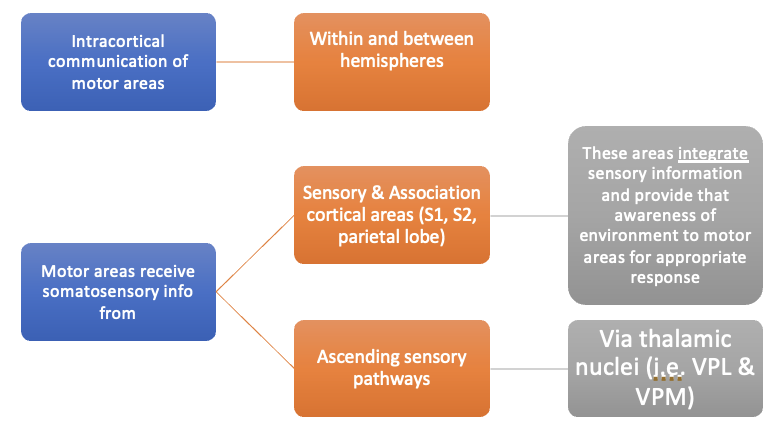
what are the general afferents to motor areas?
intracortical communication of motor areas within and between hemispheres
sensory and association cortical areas, ascending sensory pathways
what sensory input are the the cerebellum and basal nuclei responsible for?
cerebellum - motor planning, smoothing ongoing movements, assist in motor learning, posture, balance, equilibrium
basal nuclei - motor planning and execution, scaling amplitude and velocity of movements
what does M1 do?
executes specific well defined motor responses - stimulation of individual cells or small groups of cells. simple and stereotypical, discrete movement of individual muscles especially distal muscles
populations of neurons code for force of contraction and movement of direction
where is the source of projection fibers and corticospinal tract in M1?
layer V
preMC and SMA function
involved in planning of movements especially more complex movements, possible role in motor learning
goal oriented movements, movements planned based on memories, movements requiring interlimb coordination
initial phase of movements
control of proximal and axial muscles
what do secondary motor areas send major efferents to?
M1, reticular formation, spinal cord
what lobe is responsible for random finger movements? planned and execute in specific order? movement that is planned but not executed?
M1
M1 and SMA
SMA
M1 isolated lesion results in?
paresis of contralateral voluntary movements, usually starts as flaccid limbs and may become spastic - often regain some movement of proximal limb segments but distal muscles may remain paralyzed
synergistic contractions - lack independent control
lesion to the secondary motor areas results in?
apraxia - difficulty appropriately using the limb during purposeful tasks despite ability to move limbs
automatic limb movement preserved but purposeful movement usually impaired
what does the PPAC do?
motor planning functions - preparation for movement guided by sensory stimuli, collate input from sensory systems (visual, somatosensory cx, vestibular), create map of space, computation of limb and body trajectory
initiation of movement
motor related efferents are primarily to secondary motor areas
PPAC sensory functions?
integrates somatosensory, visual, auditory, and vestibular systems
interpretation and use of sensory info, planning and guiding movements based on sensory inputs, use of tools, ability to attend to sensory stimuli
PPAC deficit?
sensory deficits - various agnosias, inability to associate tactile and visual images
difficulty attending to contralateral world
motor deficits - inability to perform simple skilled tasks and difficulty with visually and tactilely guided movements
non-dominant hemisphere lesion has greater consequences than dominant
what does the cingulate gyrus do?
in monkeys has a small contribution to the corticospinal tract, projection to M1, possible role in movements that have a motivational or emotional component
what parts of the cortex are responsible for eye fields? what are their functions in relation to eye movement?
frontal, supplemental, parietal
coordination of eye movements and visual tracking, voluntary override of visual reflexes (rectus lateralis)
example of pathways
what are descending fiber paths from motor areas? (6)
corticospinal, corticonuclear, corticostriatal, corticorubral, corticoreticular, corticopontine
(many of these pathways also have fibers originating in non-motor regions of the cortex)
lateral vs medial system of descending motor control pathways, what pathways?
lateral: primary effect on motoneurons of more distal muscles - includes lateral corticospinal and rubrospinal
medial: primary effect on motoneurons of more proximal and axial muscles often bilaterally - includes anterior corticospinal, vestibulospinal, reticulospinal, tectospinal. control/modulation of balance, proximal stability head position, etc
origin of corticospinal tract
pyramidal cells
30% from M1
30% from secondary motor areas
40% from parietal regions (SI, PPAC, SII, cingulate gyrus)
course of corticospinal tract?
lateral CSp Tr: layer V of motor cortices → posterior limb internal capsule → crus cerebri → basilar pons → pyramidal decussation → anterior horn of SC (LVII, VIII, XI)
anterior CSp Tr: same as lateral, but does not decussate in pyramid, some may decussate farther down tract
somatotopically arranged
does the corticospinal tract synapse on interneurons or direct motorneurons?
more synapses to interneurons but some direct to motoneurons esp distal muscles
review: anterior and lateral corticospinal tract terminate on the _____ and _____ muscles respectively
proximal, distal
review: the anterior corticospinal tract is bilateral/unilateral. It does/doesn’t decussate in the pyramidal decussation.
bilateral, doesn’t
motor functions of the corticospinal tract?
controlled, integrated, coordinated movements, esp distal muscles in extremities (lateral corticospinal), initiation/modulation of central pattern generators
T/F the corticospinal tract carries sensory fibers from SI and SII.
T, some fibers travel in the corticospinal tract to the spinal cord posterior horn and intermediate region; modulates sensory transmission
where do collaterals of the corticospinal tract go to?
reticular formation - pons, medulla
inferior olivary nucleus - cerebellar inputs
vascular supply of internal capsule, midbrain, medulla, spinal cord
internal capsule - lenticulostriate a. off MCA
midbrain - post cerebral a.
medulla - anterior spinal a.
spinal cord - arterial vasocorona
where does the red nucleus receive input from?
ipsilateral motor areas of cerebral cortex, cerebellum (4, 5, some 5, 7)
pathway and function of the rubrospinal tract?
ipsilateral motor areas of cerebral cortex and cerebellum → red nucleus and immediately crossover in midbrain→ synapse on axons that travel to the contralateral cervical spinal cord → synapse primarily on MN of flexors
primarily influences contralateral UE flexor motoneurons, supplement the corticospinal
function of medial motor systems?
control of proximal and axial muscles
balance
orientation of head
vestibular nuclei parts
superior, lateral medial, inferior
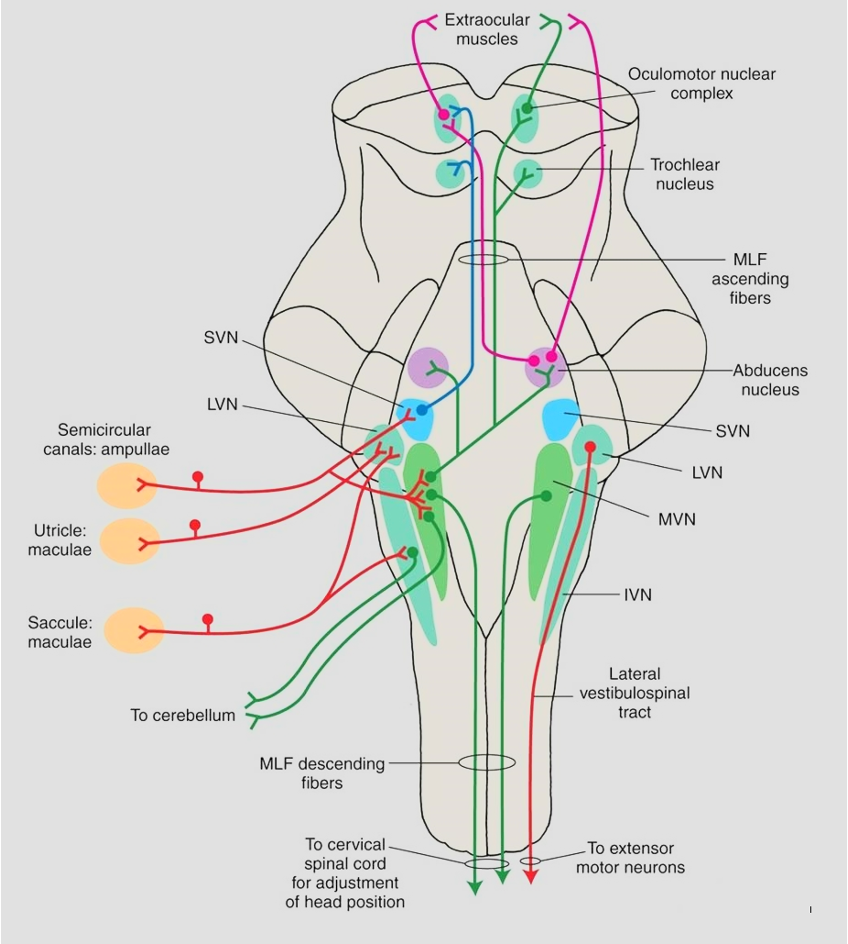
what are reflex adjustments of the vestibular system and what are the inputs to vestibular nuclei?
axial and LE muscles respond to changes in head position relative to gravity
vestibular apparatus (CN VIII), cerebellum
pathway and function of the lateral vestibulospinal tract
lateral vestibular nucleus → lateral vestibulospinal tract → ipsilateral anterior spinal cord gray area → synapse on motoneurons
postural adjustment (trunk and LE in response to vestibular apparatus input), maintain balance
generally, the lateral vestibulospinal tract produces (EPSP/IPSP) on motoneurons that control ____ and _______ on the spinal cord.
EPSP, axial, LE extensors
pathway and function of medial vestibulospinal tract
medial vestibular nucleus → descends bilaterally via the medial longitudinal fasciculus → terminates in cervical and upper thoracic spinal cord only (LVII and VIII)
influences neck musculature, reflex adjustments like head position in response to activity in vestibular apparatus
is the lateral vestibulospinal tract ipsilateral or bilateral? medial vestibulospinal tract?
ipsilateral, bilateral
pathway of reticulospinal tract
pontine reticular nucleus → pontine reticulospinal tract → terminate intermediate and anterior SC (LVII and VIII) mostly ipsilaterally (some bilaterally)
reticulospinal tract functions
control and modulate motor activity, influence motoneurons of paravertebral muscles and limb extensors
involved in providing background for primary movements - posture (stabilizes scapula and spine for UE movement), balance
alter γ-MN activity (alter muscle spindle sensitivity) - modulate muscle tone and maintain posture
modulation of sensory info, especially noxious
types of reticulospinal tracts and where they terminate
pontine (medial)
medullary (lateral)
both terminate in intermediate and anterior spinal cord (LVII and VIII), influence neurons supplying paravertebral and limb extensor muscles
T/F the reticulospinal tract travels the entire length of the spinal cord.
T
function of pontine reticulospinal tract
predominantly excitatory effect on motoneurons
function of medullary reticulospinal tract
predominantly inhibitory effect on motoneurons
what does the reticular formation do? where does it receive input from?
control and modulate motor activities, modulate sensory information
receives from corticoreticular (motor regions of cerebral cortex), cerebellum, collaterals of sensory paths, spinoreticular tract of ALS
pathway and function of tectospinal tract
superior colliculus → axons to the contralateral ventral cervical spinal cord → terminate in LVI, VII of cervical levels
involved in reflex movements of head and neck in response to visual, auditory, and painful stimuli
review: superior colliculus function
integration of visual, somatosensory info
pathway of corticonuclear tract
M1 layer V of face motor cx → genu of internal capsule → crus cerebri medial to corticospinal tr → fibers project bilaterally in pons and medulla → nuclei of motor cranial nerves
*similar to corticospinal tract (parallel)
what are the cranial nerve motor nuclei?
V, VII, XII, Nucleus Ambiguus (IX and X), accessory nucleus
what are the terminations of the corticonuclear tract? what are the functions?
trigeminal: bilateral equally; muscles of mastication
facial: upper face is bilateral, lower face is contralateral; muscles of facial expression
nucleus ambiguus: uvula and soft palate is mostly contralateral; larynx, pharynx, upper esophagus is bilateral
hypoglossal: primarily contralateral to genioglossus; tongue
spinal accessory: primarily ipsilateral; trapezius, SCM
oculomotor, trochlear, abducens: from frontal and parietal eye fields, not face motor cortex
what happens if there is a lesion in the UMN facial motor cortex? LMN (facial n.)?
UMN - central seven, only lower face affected, contralateral
LMN - Bell palsy, both upper and lower face affected, ipsilateral
what happens if there is a lesion to facial motor cortex that affects pathways to nucleus ambiguus and hypoglossal nucleus?
nucleus ambiguus - uvula moves to side of lesion
hypoglossal nucleus - tongue moves opposite side of lesion
typical signs with lesion of corticospinal tract and other descending tracts
paralysis or paresis - initially flaccid but often develop spasticity/hypertonicity
hyperreflexia and possibly clonus
Babinski sign
Synergistic movements patterns of groups of muscles
what is spasticity/hypertonicity?
increased resistance to passive stretch, velocity dependent, clasped knife effect