Quiz 2
1/31
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
32 Terms
Functions of skeletal muscles
Produce body movements
Stabilize body position against gravity
Regulate organ volume
Move fluids and solid food and wastes in the body
Produce heat
Skeletal muscles
Muscles of skeleton (attached to bones)
Diaphragm
Parts of esophagus and eye
External anal sphincter
Voluntary and reflex control
Properties of muscle tissue
Electrical excitability
Contractility
Extensibility
Elasticity
Muscle fiber
Cellular unit of skeletal muscle
Each fiber contains thousands of tubular structures called myofibrils (highly organized contractile proteins)
Fibers bound together in fasciculi
Parts of the skeletal muscle organization
Myofilaments (actin & myosin) → myofibrils → muscle fibers → fascicles → skeletal muscle
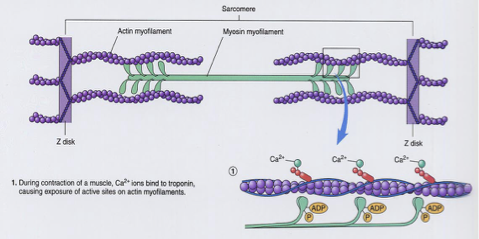
Sarcomeres
Contractile apparatus of SKM made up of thick (myosin) + thin (actin) myofilaments arranged in interdigitating arrays
Contractile proteins associated with muscle fiber
Actin
Myosin
Regulatory proteins associated with muscle fiber
Help form myosin-actin cross bridges
Troponin
Tropomyosin
Structural proteins associated with muscle fiber
Titin
Dystrophin
Myomesin
Nebulin
NMJ
Specialized chemical synapse that links motor nerve impulses to release acetylcholine onto nicotinic receptors which initiate SKM activation
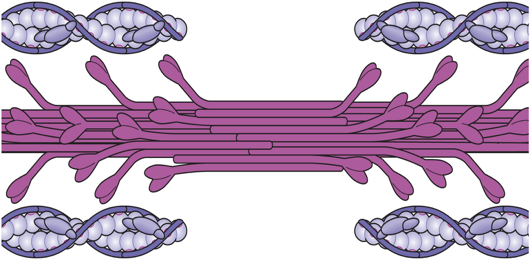
Myofilaments of SKM
Myosin is assembled into thick filaments → S2 region of the molecule is flexible & tail region is stiff
Actin-binding sites are located on globular myosin heads, which also contain light chains with ATPase activity
Thin (actin) filaments are formed from G-actin monomers into helical F-actin strands → associated with troponin-tropomyosin complex to form the functional actin filament

Muscle contraction of SKM
Nerve impulse arrives at end of motor nerve axon (somatic nerves) causing Acetylcholine(ACh) release into synapse via exocytosis
ACh floods across synaptic gap and attaches to receptors on sarcolemma
Permeability of sarcolemma changes and Na+ enters cell
Muscle impulse (AP) is triggered
Muscle impulse travels via transverse tubules (T-tubules) throughout muscle cell = T-tubule depolarization
Ca2+ diffuses from SR into myoplasm → binds to troponin on actin
Myosin heads binds to actin forming cross bridges
Cross-bridges pull thin filament (power stroke), ADP and P released from myosin
New ATP binds to myosin, releasing linkages
ATP splits which provides power to “cock” the myosin cross-bridges
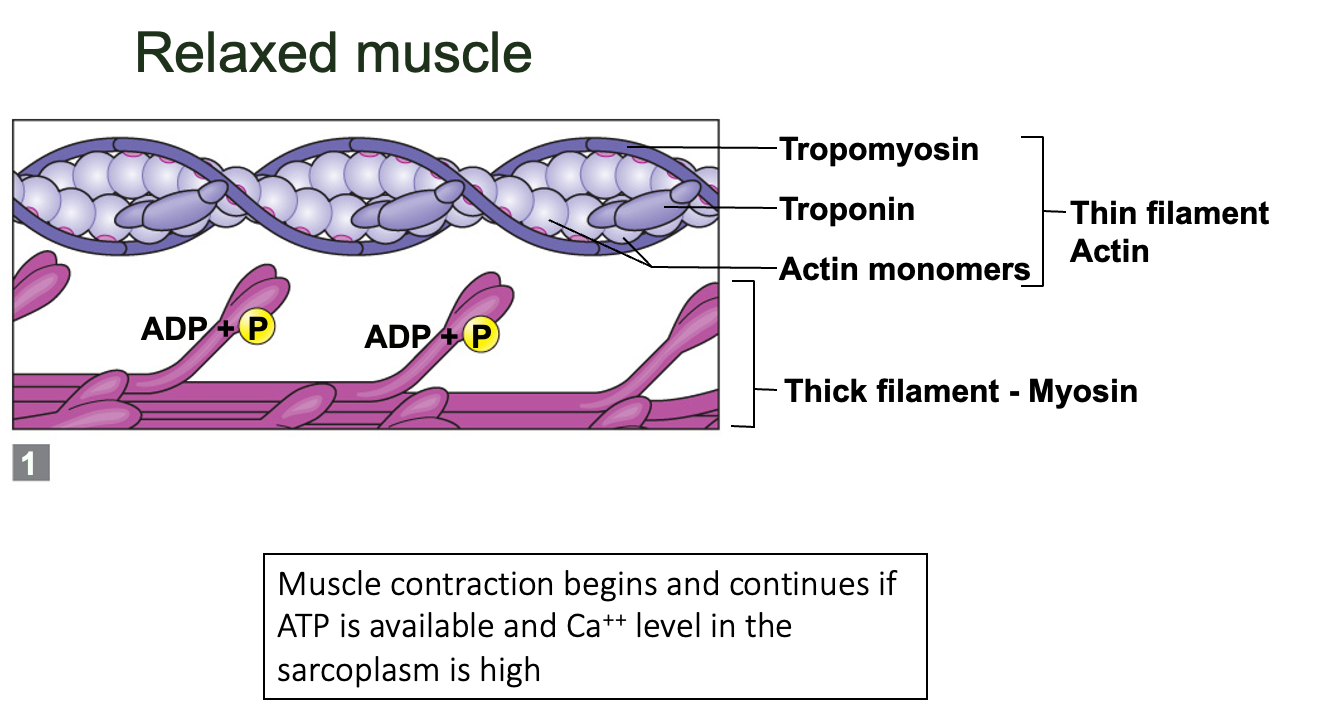
SKM Excitation
Nerve impulse arrives at axon terminal
Triggers release of Ach by exocytosis
ACh diffuses across synaptic cleft
ACh binds to receptors on muscle motor end plate
Sarcolemma becomes more permeable to Na+
Na+ triggers release of muscle action potential
Muscle action potential travels along outside of sarcolemma and into T-tubules
APtriggers Ca++ release from SR
Ca++ binds to troponin on thin filament → releases allosteric inhibition of tropomyosin on actin
Tropomyosin is pulled aside, revealing binding sites
Myosin links to & pulls actin to contract muscle
SKM Relaxation
Acetylcholinesterase decomposes ACh in synapse
Action potential (impulse) ends
SR actively pumps Ca++ back into SR
Tropomyosin moves back to cover binding sites
Myosin heads detach
Muscle fiber returns to its longer resting length
SKM cross-bridge cycle
Produces force and shortens sarcomere
Requires ATP and is activated by increase in intracellular Ca2+
Interdigitation
Trigerred and controlled by the entrance of Ca2+ ion into a protein called troponin located on actin filament
When Ca2+ exits, bridges are uncoupled → relaxing the filaments which lengthen
↑ Ca2+ → ↑ muscle contraction
↓ Ca2+ → ↓ muscle contraction
Too much Ca2+ → muscle fails
Motor unit summation
Summed force: Total force generated in whole SKM due to activation of both motor units to produce a stronger muscle contraction
Total force: simple spatial summation of twitches from two motor units
First, a brief partial tetanus is created in the first motor unit (temporal summation) → additional motor units are recruited, increasing muscle force

Regulating contractile force of SKM
Varying the number of motor units stimulated (spatial summation)
By increasing the frequency of activation by motor neurons (temporal summation)
Temporal summation can summate force and produce tetany
Twitches
Brief, singles contractions of muscle fibers in response to a single stimulus
Smooth muscle
Myogenic contractions: can both contract and relax actively on its own via ANS unlike SKM
Contraction and relaxation can be tonic, graded or phasic and is controlled by direct chemical and physical stimuli, as well as receptor-mediated activation by neurotransmitters, hormones or chemical ligands
Relaxtion is active and not just the absence of contraction → associated with lowering cytoplasmic Ca2+
Exhibit single or summed twitch contractions
Produce graded responses in form of smooth increments in contraction or relaxation rather than the “all-or-off” characteristic of SKM
No visible striations
Contain thick and thin filaments but different than SKM
Fewer myosin filaments than SKM → slower contraction and greater economy of energy usage (begins to contract 50-100ms after being excited and remains contracted for 1-3 sec) & longer contraction (30 times longer than single SKM contraction)
Can maintain same tension of contraction as SKM at less than 1% of energy cost
Visceral SM: can be physically and electrically coupled allowing activation to spread from cell-to-cell
Vascular SM: contains more multiunit type SM that are innervated cell by cell
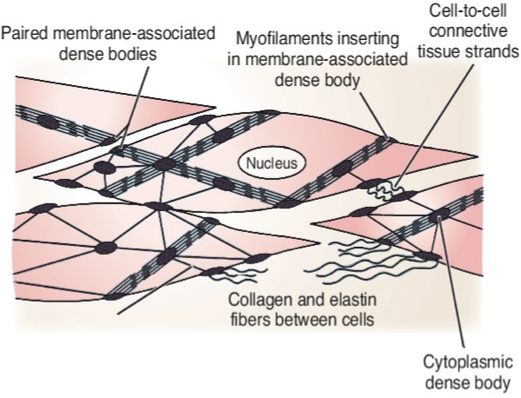
Smooth Muscle myofilament organization
1:16 ratio of thick to thin filaments (1:2 ratio in SKM)
Tropomyosin associated w/ thin filaments but no troponin present
No sarcomeres - thick and thin filaments are collected into budles that correspond to myofibrils
Contain non-contractile intermediate filaments that attach to dark-staining dense bodies that are distributed throughout the cell and occasionally anchored to the sarcolemma
Dense bodies
Serve as attachment points for thin filaments of SM
Counterparts of Z lines in SKM
Intermediate filament-dense body network forms strong, cable-like intracellular cytoskeleton → harnesses pull generated by sliding of SM myofilaments during contraction
Smooth muscle sheets
At least 2 SM sheets are present and oriented at right angle to each other
Longitudinal layer runs with long axis of organ
Circular layer runs around circumference of organ
Cyclic contraction and relaxation of these layers allows lumen of organ to alternately constrict and dilate for peristalsis
Contraction of SM in rectum, urinary bladder and uterus helps those organs to expel their contents
Where is SM found?
GI tract
Bladder
Blood vessels
Uterus
Tracts of respiratory, urinary and reproductive system
Eyes (iris)
Skin (erect hair)
SM innervation
Lacks highly structured NMJ of SKM
Instead, innervating nerve fibers approach SM fibers → release Nts into synaptic cleft of SM cells via bulbous endings called varicosities
Contraction of SM
Adjacent SM cells exhibit slow, synchronized contractions
Whole sheet responds to stimulus in unison → reflects electrical coupling of SM cells by gap junctions
Whereas SKM cells are electrically isolated from one another (each stimulated to contract by its own NMJ)
Gap junctions coordinate changes in membrane potential and intracellular Ca2+ between adjacent SM cells
Ca2+ binds to thick filaments rather than thin filaments as in SKM
Myosin ATP-ase activity is 1/10th that in SKM, even in optimal conditions
Pacemaker cells
Specialized SM cells
Act as “drummers” once excited, to set contractile pace for entire sheet of SM
Self-excitatory membranes → can depolarize spontaneously in absence of external stimuli
However, both rate and intensity of SM contraction may be modified by neural and chemical stimuli
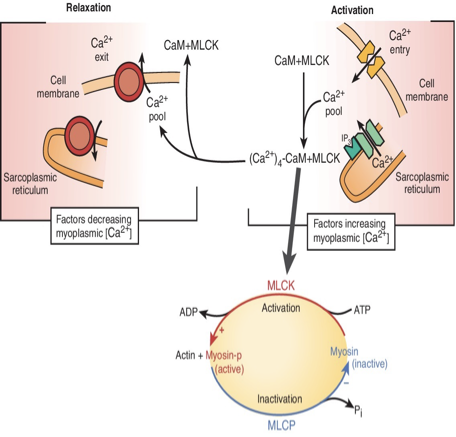
Mechanism of contraction in SM
Actin and myosin interact by sliding filament mechanism
Rise intracellular Ca2+ ion levels (final trigger for contraction)
Sliding process is energized by ATP
Reaction pathways in regulation of cross-bridge cycle in SM
Activation begins when cytoplasmic Ca2+ levels are increased and Ca2+ binds to calmodulin → activates myosin light-chain kinase
The kinase catalyzes phosphorylation of light chain in myosin head, changing it to an active form
Phosphorylated myosin head increases affinity for active sites actin (thin filaments) → cross-bridge cycling → initiates contraction but at slower rate than SKM
When Ca2+ levels reduce, it leaves calmodulin → kinase is inactivated → myosin light-chain phosphatase dephosphorylates myosin, inactivating it
Cross-bridge cycle stops and muscle relaxes
SM tone
Ability of SM to maintain tension for a prolonged period while using relatively small amounts of ATP (important to overall body homeostasis)
Small arterioles and over visceral organs are routinely called on to maintain a moderate degree of contraction (without fatiguing)
Since energy requirements of SM are low, it can generate adequate ATP to support its contractile activity even in absence of O2 → occurs via anaerobic pathways
SM regulation of contraction
AP generated by binding of neurotransmitter molecules to membrane receptors → release of Ca2+ ions into sarcoplasm
Not all neural signals result in SM activation and not all SM activation is result of neural signals
Can generate their own AP by influx of Ca2+ ions
Source of cytosolic Ca2+ ions in SM cells
Extracellular space through voltage-gated calcium channels and
Intracellularly via release from sarcoplasmic reticulum