chapter 22 - exam 3
1/30
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
31 Terms
nephron
basic functional unit of the kidney; filters blood, removes waste, and regulates water and electrolytes
steps of nephron function - step 1
Glomerular Filtration:
As blood moves through the glomerulus and Bowman’s capsule, water and electrolytes leave the blood and enter the proximal tubule. At this stage, the fluid (called glomerular filtrate) is very dilute but contains electrolytes, glucose, and waste products.
steps of nephron function - step 2
Proximal Tubule:
Here, about 60% of water is reabsorbed back into the blood. As the filtrate continues moving through the nephron, electrolytes like sodium and potassium shift between the tubule fluid and the bloodstream.
steps of nephron function - step 3
Loop of Henle:
In this section, urea (a nitrogen-containing waste) is added to the tubule fluid. The fluid now starts to look like urine. The loop of Henle reabsorbs 25% of filtered electrolytes (sodium, chloride, potassium, calcium, and bicarbonate) and 15% of water.
steps of nephron function - step 4
Distal Tubule:
Here, the hormone aldosterone helps the body reabsorb more sodium and water while secreting potassium into the tubule. This step helps the body conserve water and further concentrates the fluid.
steps of nephron function - step 5
Collecting Duct:
In the final stage, antidiuretic hormone (ADH) controls how much water is reabsorbed back into the blood. If the body needs water, ADH increases water reabsorption, producing highly concentrated urine.
pyelonephritis
patho: known as an “upper UTI”, its an ascending infection (bladder to the kidneys), vesicoureteral reflux (urine flows backward from the bladder and into the kidneys) is a common factor
acute: bacteria causes inflammation in kidneys
chronic: repeated infection causing scarring, deformity, and urine reflux creating a cycle of more infections and kidney damage
sx: fever, chills, flank pain, CVA tenderness, hematuria, N&V
dx: urine cultures, intravenous pyelogram (xray)
renal dysfunction
prerenal → before the kidney; lack of blood flow to the kidney that could be due to a hemorrhage, shock, dehydration, etc.
intrarenal → inside the kidney; direct injury to the kidney from potential things like NSAIDS, infections, HTN, DM, autoimmune disorders
postrenal → after the kidney; blockage of urine flow potentially from things like kidneys stones, tumors, enlarged prostate, etc.
acute kidney injury (AKI)
aka acute renal failure
sudden loss of kidney function due to an abrupt insult to the kidneys leading to a low GFR, creatinine, BUN and urine output
etiology:
prerenal → decreased blood flow to the kidneys (most common and reversible if tx early)
instinct → direct kidney damage
postrenal → blocked urine flow
sx: oliguria (<400mL of urine O daily), fluid overload, uremia (waste buildup), electrolyte imbalances, metabolic acidosis
dx: urinalysis, high creatinine, low urine O, high BUN
tx: tx underlying cause, diuretics, electrolyte replacement, dialysis
phases of AKI
kidney insult occurs
oliguric (no urine output) → decreased GFR and high BUN = fluid overload and electrolyte imbalance
diuresis → urine output increases; kidneys are recovering but urine may not filter waste well
recovery → nephrons regenerate or compensate and urine concentration becomes nml over weeks or months
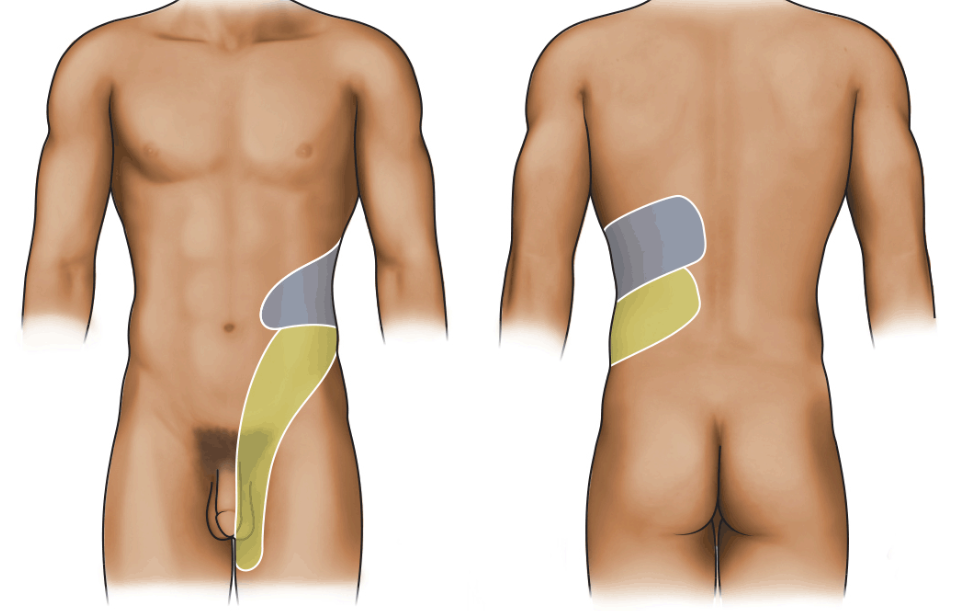
kidney stones (nephrolithiasis) - calcium stones
can be caused by hypercalcemia, oxalate-rich foods, dehydration
parathyroid controls calcium lvl and if calcium is low, the parathyroid will pull more calcium from the bones and the kidneys can’t handle it so calcium calculi form
Flank pain with radiation into the groin, hematuria, and crystalluria are classic signs of nephrolithiasis.
acute glomerulonephritis
CAN BE CAUSED FROM STREP
inflammation of the glomerulus caused by an immune rxn, leading to leaking of blood and proteins into the urine, decreased filtration, and fluid retention
patho: the body responds to infection by making antibodies which will either form immune complexes and deposits in the glomeruli, OR they will mistakenly attack glomerular tissue aka molecular mimicry; the immune complexes lead to inflammation which causes leaky glomeruli = albumin and RBC in urine, low albumin in blood, decreased GFR
sx: HA, elevated BP, proteinuria, hematuria, oliguria, CVA tenderness.
dx: high serum creatinine and BUN, low specific gravity, high protein and RBC in urine
CAN LEAD TO NEPHROTIC SYNDROME
polycystic kidney disease
genetic disorder where fluid filled cysts from in/around the kidneys
patho: mutated genes allows there to be abnml proteins (polycystins) and they grow uncontrollably in the kidney tubules which leads to the formation of fluid filled sacs that compress and damage healthy kidney tissue; overtime, fibrosis (scarring), and loss of fx will occur. the cysts can rupture which stimulates the RAAS system
sx: pain, CVA tenderness, HTN, cysts on other organs, mitral valve prolapse
dx: ct, mri, us
nephrotic syndrome
caused by damage to the glomeruli leading to a LOT of protein loss through urine
patho: damage to the glomeruli happens and protein (especially albumin) leak into the urine which causes low protein in the blood causing water to move into the cells, leading to edema. the liver will try and make more albumin which increases lipid production. loss of proteins like antithrombin increases risk for blood clots
sx: edema in face, HTN, hematuria, proteinuria
dx: proteinuria, hematuria, elevated BUN and creatinine, low serum albumin
good pasture syndrome
autoimmune disease where they body makes antibodies that attack the kidneys and the lungs
patho: antibodies attack the basement membrane of the kidneys (causes glomerulonephritis) and lungs (causes pulmonary hemorrhage). T and B cells are involved and worsen the inflammation; overall damage leads to decreased GFR and o2 exchange in the lungs, inflammation, and bleeding in lungs and kidneys
sx: kidneys ability to filter blood and urine is impacted, decreased o2 exchange in the lungs, chills, fever, malaise, hemoptysis, cyanosis, crackles, HTN
dx: blood tests to check for anti-GBM antibodies and confirm w/ western blot test; UA will show hematuria, proteinuria; BUN and creatinine will be high = kidney fx low
chronic renal failure sx
aka chronic kidney disease
decreased urine output, proteinuria, hematuria, lethargy, confusion (from waste buildup), HTN, hypervolemia, heart failure N&V, anorexia, uremic fetor (ammonia breath), anemia (from decreased EPO), high risk of bleeding, amenorrhea, ED
chronic renal failure patient teaching
diet and fluids → decrease sodium and potassium intake, limit phos. intake, moderate protein intake, maintain fluid balance (avoid overhydration), calcium supp. that contains vit d
sx to report → wt gain or swelling, muscle weakness or irregular heart beat, bleeding/bruising, mental confusion, severe fatigue
lifestyle modifications → stop smoking, exercise regularly, monitor BP, BS and wt daily, get vaccines, prepare for dialysis or replacement
stage 1 CKD eGFR
high or normal
90 - 120 mL per min
stage 2 CKD eGFR
60 - 89 mL per min
stage 3 CKD eGFR
30 - 59 mL per min
stage 4 CKD eGFR
15 - 29 mL per min
stage 5 CKD eGFR
< 15mL per min
no dialysis until GFR is at this rate
pt with chronic hypoxia will often have a higher than normal …
hemoglobin and hematocrit because of constant secretion of erythropoietin
pt with renal failure will have a low….
hemoglobin and hematocrit levels because of deficient erythropoietin
hematuria is often a sign of
renal calculi or infection
serum creatinine is a reliable indicator of
kidney function
oliguria
less than 400 mL of urine output per day or less than 20 mL of urine per hour
hypoalbuminemia, edema, and proteinuria are the three distinguishing features of
nephrotic syndrome
kidney stones (nephrolithiasis) - struvite stones
can be caused by UTI’s from urase producing bacteria (commonly form staghorn calculi which can fill the entire renal pelvis)
kidney stones (nephrolithiasis) - uric acid stones
can be caused from gout, CA treatment, a high purine diet
kidney stones (nephrolithiasis) - cystine stones
can be caused from a genetic defect in cystine reabsorption
failure to absorb amino acids