Gait training and walking recovery after SCI
1/70
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
71 Terms
PROM UE
need to be WNL, esp shoulder extension
scapula needs to move
LEs PROM needed
-hip: 0-10 ext and full flexion
-HS length: 0-110 for KAFO or reciprocating gait orthosis (RGO) users
-knee: full extension
-ankle: 0-10 DF
-needed to attain “para-stance”
in para stance position
-GRF needs to be posterior of hip for the hip extension moment
With sufficient ankle DF, hip extension, & lumbar extension PROM, pt leans into anterior hip’s Y ligaments for stability.
for fxnal gait, pt needs to have 5/5 throughout UEs
-scapulae must be stable and mms strong
-for traditional “para-gait”
-50 dip rule
true MMT will help with bracing specifications
-do not rely on ASIS alone
—all mms need to be tested
-particularly important for pts with AIS C & D
other MSK considerations
Lumbar flexibility to achieve para-stance
Leg length discrepancy
Scoliosis
Orthopedic fixation
Body shape/size
Length of time since onset of injury
May require osteoporosis screening (DEXA scan) if its been 4-6 months since WBing
sensory considerations
-body awareness
—including proprioception/kinesthesia
-p!
-light touch
-deep pressure
-need more than AIS testing
—for where you need to perform skin checks, harnesses
interdisciplinary team assesses spasticity
caused by upper motor neuron lesion
interfere w mobility/standing/ambulating
spasticity PROS
-maintain mm bulk
-circulatory fxn
-postural control
-prevent weight gain
-may be indicative of recovery potential
spasticity CONS
PROM changes
interfere w orthosis use
-cause areas of increased pressure
-donning
other examinations for standing or gait
-BP for upright tolerance
-motivation: attendance; compliance w self PROM, skin checks and protection, bowel/bladder management
-cost/funding sources
-balancing gait w other therapy goals: transfers, WC mob, bed mobility, etc
Shepherd Center SCI Program: Criteria for Long Leg Bracing Program
Patient has desire to ambulate with specific and realistic goals
Patient within 10% of ideal body weight
PROM within following limits:Hip Ext (5 degrees), Knee Flex/Ext (WNL), Ankle DF (5 degrees), Passive SLR (110 degrees)
Skin intact
Stable cardiovascular and pulmonary systems (MD cleared)
Patient must be able to stand in parallel bars for 60 min with stable BP/joints
T12 and below (higher considered if all other criteria met)
50 body-weight dips
PT session compliance, must complete PT training before KAFO prescription
Independence with all transfers/WC mobility
WC propulsion: 1 mile in less than 20 min
Patients L2 and higher must be >6 months post-injury
Caregiver identified for assistance and training
SCIM III (like FIM)
-power wc → manual wc → dependent walking → independent walking
WISCI-II (like 10mWT)
Area of assessment
Functional mobility & gait
Amount of physical assistance needed as well as devices required
can tell insurance that they are progressing
functional scale
SCI-FAI
assesses functional wlaking ability i amb individuals with SCI
-qualitative data
-participation
evaluation: cardiopulmonary comorbities
autonomic dysreflexia
take vital signs
hypertension/hypotension
smoking
DM, hypoglycemic
CAD
evaluation: integumentary
putting my eyes on them
so you can figure out what might have caused it
evaluation: cognitive and psychological
-TBI, concussion
-anxiety and depression, sleep and wake cycles, fatigue, motivation
PT diagnosis
-neuro classification (ASIA)
-force production
-fractionnated movement
Prognosis: predict potential recovery based on exam dat, evidence, and clinical judgment
Complete vs incomplete
Predict optimal level of improvement in function
Paralyzed Veterans of America (PVA) Guidelines for Expected Outcomes based on level of injury
ASIA Impairment Scale
Somers textbook
ASIA A progniosis
3% ambulate
ASIA B prognosis
50 ambulate
ASIA C prognosis
75 ambulate
ASIA D prognosis
95%
canadian calculator for ambulation prognosis
L3 myotome, S1 dermatome, age at injury
POC: determine which intervention route or routes you will use, consider risks and benefits
Compensatory movement patterns
Recovery of normal movement patterns
Risks
Fracture: proximal femur and tibia
Overuse: UE/LE; Especially consider shoulders and CTS with para-gait
Cost/benefit ratio of energy expenditure
Consider the benefits: Psychological; Physiological
standing/walking functional level
standing only; walking for exercise; functional amb (household and community)
equipment
Assistive devices
Orthoses
Electrical stimulation
Robotics
-lokomat
-rewalk
-EKSO
recommendations/referrals
-medical intervention: spasticity, surgery
-continuum of care
AIS A C1-C8
inadequate voluntary motor function for functional ambulation
PVA guidelines state that standing/ambulation require total assist
AIS A T1-T12
varying trunk and pelvic control
abdominals lowest functioning mm group
sensory deficits
HKAFO/RGO for children & some adults for exercise/household ambulation with assistive device
Supervision-Min assist(T1-T8) or mod indep (T9-T12) with KAFOs for exercise/household ambulation with assistive device (walker or crutches)
T1-T8 modified independent in parallel bars
Difficulty with uneven surfaces
Wheelchair for functional mobility
AIS A L1
CAN HIP HIKE, CAN PROGRESS THE LIMB FORWARD
-pelvic control: QL
-sensory deficits
-KAFO: exercise/household amb w AD (crutches)
-WC: functional mob
AIS A L2
use less heads hip relationship
-hip control: iliopsoas
-sensory deficits
-KAFOs: functional household amb w AD (crutches)
-WC: functional mob
AIS A L3
-knee control: quads
-sensory deficits
-AFOs/KAFOs for household amb w potentional for functional comm amb w AD (usually ccrutches)
-may continue to use WC in community
AIS A L4-5
Knee and some foot control – anterior tibialis
Sensory deficits
RX: AFOs – Good potential for functional community ambulation with assistive device (crutches or cane)
incomplete injuries
-very complicated
-case by case basis
-level of injury (ASIA)
-AIS classification
-age, body habitus, resources, etc
techniques to gain PROM
-self or assisted PROm
-cruciate (crucifixion, open up chest) positioning for UEs
-mobs (talocrural mob)
-standing program
-serial/inhibitory casting
spasticity management
-watching HS, hip flexors, PFs
-oral meds
-neurolytic injections
-botox injections
-intrathecal baclofen pump trial/placement
theoretical benefits of standing
Maintain PROM/prevent contractures
Regulate bowel and bladder
Decrease spasticity/clonus
Improve strength (of what?)
Decrease risk of pressure sores
Increase circulation
Compensate for impaired autonomic response to position change (ie. BP issues – orthostatic hypotension)
Psychological/emotional benefits
Prevent or slow osteoporosis process* (remains controversial)
No evidence to support that static standing will promote return**
stall bars standing frame
working on trunk control
KAFO Pre-gait and functional training
-training braces (KLUNKERS)
-allows assessment of pt’s ability and training prior to ordering
-not customized
-difficult to control amount of DF
-heavy/ugly
other options besides KAFOs for lower SCIs
trial orthoses
ace wraps/theraband/taping
casting/bivalves
KAFO pre-gait and functional training: education and donning/doffing
•Re: overuse of shoulders for those without LE return
•Skin considerations
KAFO pre-gait and functional training: donning/doffing
•Short vs. long sitting
•Under (skin checks) vs. over clothing (no WRINKLES)
balance in “para-stance”
•Ankles dorsiflexed – fixed
•Knees extended
•Hips extended, leaning into Y ligament
•Lumbar extension
•Begin in the parallel bars with KAFOs
•Poor balance vs. orthotic modification
•Working within base of support and setting limits to allow patient with complete (para-stance) or incomplete SCI to recover balance
patients with complete SCI
push-ups, jack knife
pts with incomplete SCI
strengthening/forced use activities
all pts need to train these activities
-WC sit to/from stand practice
-WC frame and footrest type
Para-stance/Tripod position
•Drag to: Most inefficient, for weakest patients &/or early training
•Swing to
•Swing through: Fastest, requires most strength and guts
4-point vs. 2-point reciprocal
Most efficient per unit of time, but…
guarding the patient w complete SCI
Guard from back once up
•Prevention of accidental jack knife: hand at the back & on the shoulder
guarding pt w incomplete SCI
Position self where needed for patient stability & best body mechanics
FALLING & FLOOR TO STAND
Remember to remove assistive device out of the way for patients with complete injuries Hamstring length
For patients with incomplete injuries, discuss gait assistive devices for safety vs. full potential
How to simplify the task? part-whole training
ramps
Remember toe clearance for all levels of injury & bracing levels when going up.
Remember that floor “drops” from beneath feet when descending.
Where will hips tend to “fall” when in orthoses with fixed ankle joints?
curbs and stairs
Direction for patients with B KAFOs
—Forwards method
—Backwards method: Descending backwards with a railing for fatigue & safety reasons
Other techniques for lower level and/or incomplete injuries
—Step over step
—Step-to method
Environmental constraints of curbs versus stairs?
—stairs: small space
ASSISTIVE DEVICES: practice with walkers and crutches
Parallel bars
Walker
Crutches
—Lofstrands vs axillary?
Walking stick or NDT pole
1 or 2 canes
Walker vs Lofstrand crutches
—Environmental constraints?
—Shoulder joint forces?
—Gait characteristics?
more force through lofstrand or walker?
lofstrand
orthoses
An orthosis may not & probably won’t return the patient to prior functional level: Discuss expectations
An orthosis is a tool, like a cane or crutch, that they must learn how to use effectively
Never underestimate the importance of cosmesis.
Components: Remember that there are dozens of ankle & knee joints on the market.
The best joint to use may be the one with which your orthotist is familiar.
Consider availability/expense (time, money) of orthotist & materials for maintenance & repairs.
Teamwork: Ask questions if the orthotist is more experienced OR learn together.
Few people post SCI continue to use their KAFOs long term
3 out of 40 continued to use (30 complete/10 incomplete injuries)
•Of those no longer using:38% - too time consuming to don/doff
22% - fear of falling
19% - impractical due to inability to use hands for other things
•Of those still using:Used max of 1x/week
•Of 10 patients issued standing frames, all 10 used at least 1x/month
paradigm shift in SCI rehab
Historically, the prevailing assumption has been that the CNS is incapable of repairing itself.
Clinical decision-making has been guided by expected outcomes & the degree of motor/sensory loss demonstrated by a patient. Refer back to Scheets neuro class system, PT 6032.
Compensation with braces & assistive devices, as well as teaching new movement strategies has been the gold standard for SCI rehabilitation.
BUT…Independent function does not equal recovery.
Activity based plasticity of neurons has been well known for more than 100 years
There is evidence that the spinal cord is capable of learning & controlling walking in animals with transected spinal cords.
Lovely et al (1986) Cats with transected cords demonstrated hind limb stepping in absence of supraspinal input
CPGs
Cats increased cadence & step length appropriately as treadmill speed was increased
•Possible interpretations: Spinal cord has a capacity to respond to afferent input (i.e. increased treadmill speed)
Hodgson, et al (1994)
Task specificity
Cats with completely transected cord
2 groups; Standing and Stepping
Each group learned the task for which it was trained, but could not perform the alternate task.
AIS A Human Studies
Human spinal cord interprets limb loading during stepping independent of supraspinal influence (EMG activity increases with higher limb loading).
Human spinal cord interprets velocity afferent input (EMG amplitude increases with faster stepping speeds), independent of supraspinal influence.
Subjects with “clinically complete” SCI can generate stepping patterns on treadmill, but cannot sustain it (3-10 steps).
The use of partial body weight support
Decreases biomechanical & equilibrium constraints.
Allows for repetitive practice of complex gait cycles.
But we have to be careful with how much we unload, as we know that loading increases EMG amplitudes, right?
BWST systems benefits
Provide earlier intervention to ↓ secondary complications
Provide task specific training, sensory input, and repetition
Minimize compensation
↑ LE weight-bearing, ↓ UE weight-bearing
Promote good trunk, pelvic, and limb kinematics
Promote upright posture and balance
–20-40 min of cumulative stepping in 1-hr session
manual BWST training advantages
Fall-free environment
•Patient is more active, esp. at hips and trunk
•Allows for manual facilitation by trainer
•Allows for active arm swing
•Can use FES and/or orthotics
•Manual facilitation
manual BWST disadvantages
•Requires up to 3-4 trainers.
•Patients with severe spasticity can be very difficult
•Trainer fatigue and experience level (injuries) can alter results
•Inconsistent seating systems for the trainers
•Weight limit: 250 lbs
clinical considerations prior to locomotor training w BWST
Spinal stability
Stabilization device used
Clearance from ortho / neurosurgery
Weightbearing status
Lower limbs
Upper extremities
Joint PROM (ankylosis, fusion, casts)
Balance
comorbities
pain
CV status: metabolic demands, fatigue, ortho hypotension
pulm status: need for oxygenation, ventilation, suctioning; contra w rib fxs, pneumothorax
skin: contra w sacral or ischial wounds
urologic/GI: timing B&B, caution with indwelling catheters
MSK: some residual LE strength, spasticity, avoid musculo-tendinous injuries (i.e. sprains)
body habitus: weight limit is ~250 lb for most bWS systems and 297 lb for Lokomat.
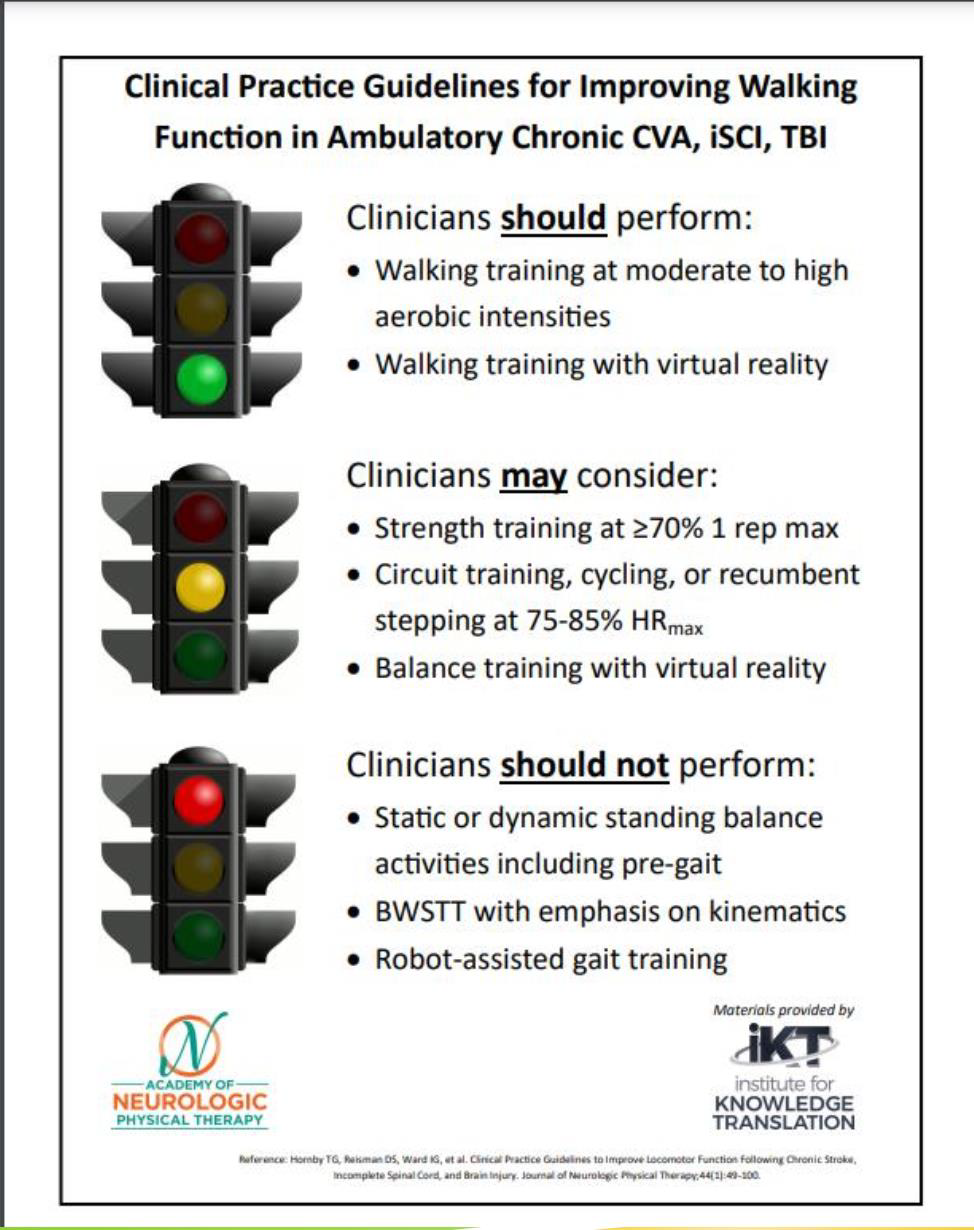
CPG for improving walking
neuromodulation after SCI
Peripheral stim
NMES/FES
TENS
Spinal cord stim
Epidural electrical stim (EES)
Transcutaneous electrical spinal stim (TESS)
Brain stim
Transcranial direct current stim (tDCS)
Transcranial magnetic stim (TMS)
DBS (deep brain stimulation?)