Circulatory Disturbances - Hemorrhage & Thrombosis
1/78
Earn XP
Description and Tags
Pathology - Lec 13 - Exam 2
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
79 Terms
What are the 2 disorders of hemostasis?
hemorrhage → extravascular blood loss
thrombosis → inappropriate formation of intravascular clots
What are the 2 mechanisms of hemorrhage?
hemorrhage by rhexis → ruptured vessel
hemorrhage by diapedesis → RBC squeeze through intact vessel walls
T/F: The appearance of hemorrhage depends on cause, location, and severity.
TRUE
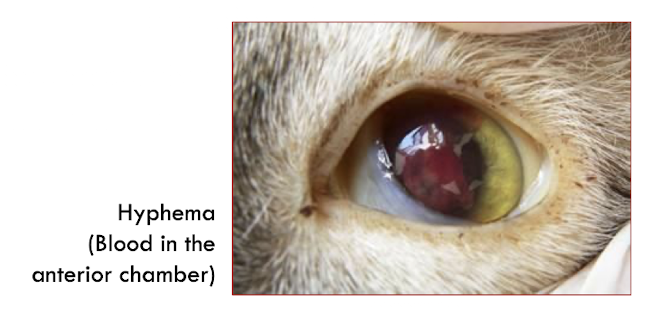
Hemorrhage is characterized by what?
size
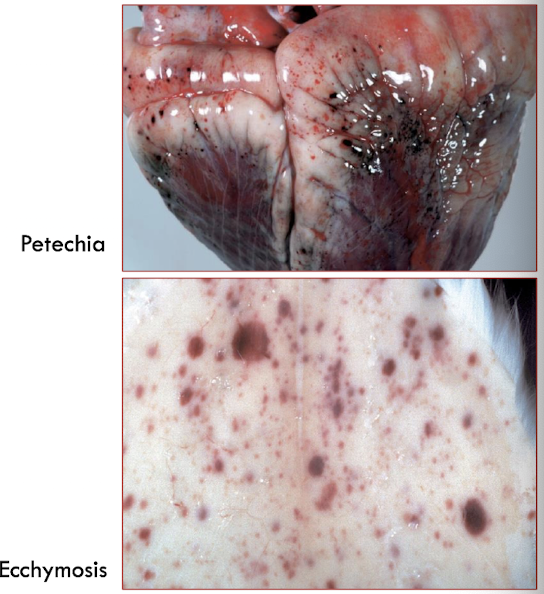
What are the 3 different classifications of hemorrhage based on size (from smallest to largest)?
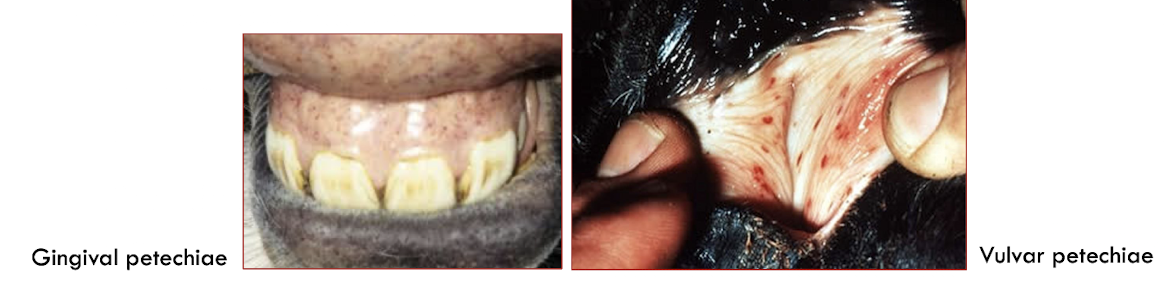
petechia → 1-2 mm
purpura → 3 mm - 1 cm
ecchymosis → 1-3 cm
What is suffusive hemorrhage?
larger contiguous areas of hemorrhage
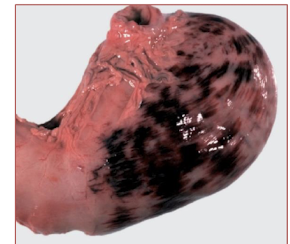
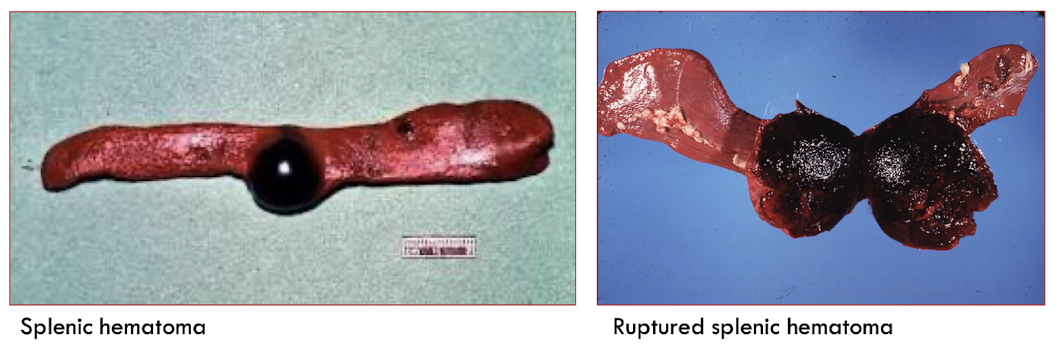
hematoma
occurs in a focal, confined space
A hematoma grows until what?
pressure exerted by extravascular blood matches the pressure of blood within the injured vessel or the vessel is sealed by hemostasis
T/F: Hematomas are always life-threatening.
FALSE - can be insignificant or rupture & potentially cause death
Which classifications of hemorrhage have a diapedesis mechanism?
petechiae & ecchymoses
What are the 2 major causes of hemorrhage by diapedesis?
minor defects in otherwise intact blood vessels (endothelial damage)
defects in 1o hemostasis (platelet defects, von Willebrand disease)
What are the 2 major causes of hemorrhage by rhexis?
trauma
extensive damage to vessel integrity by infectious agent (invasive fungi)
Hemorrhage occurs due to abnormal function or integrity of what?
endothelium and blood vessels
platelets
coagulation factors
What are the causes of hemorrhage via blood vessels?
trauma
inflammation
infectious disease
genetic disorders
nutritional disorders
Hemorrhage in relation to blood vessel trauma is caused how? Examples?
physical disruption of blood vessel wall
ex) subdural hematoma, aural hematoma, iatrogenic hemorrhage (surgery)
What is an example of blood vessel hemorrhage due to inflammation?
Feline Infectious Peritonitis (FIP) → type III hypersensitivity rx (FIV also type IV)
What is an example of blood vessel hemorrhage due to infectious disease?
epizootic hemorrhagic disease → vasculitis & hemorrhage due to endothelial injury
What is an example of blood vessel hemorrhage due to genetic disease?
Ehlers-Danlos Syndrome/ Dermatosparaxis → hereditary collagen dysplasia (fragile skin ± blood vessels)
What are is nutritonal disorder that can lead to blood vessel hemorrhage?
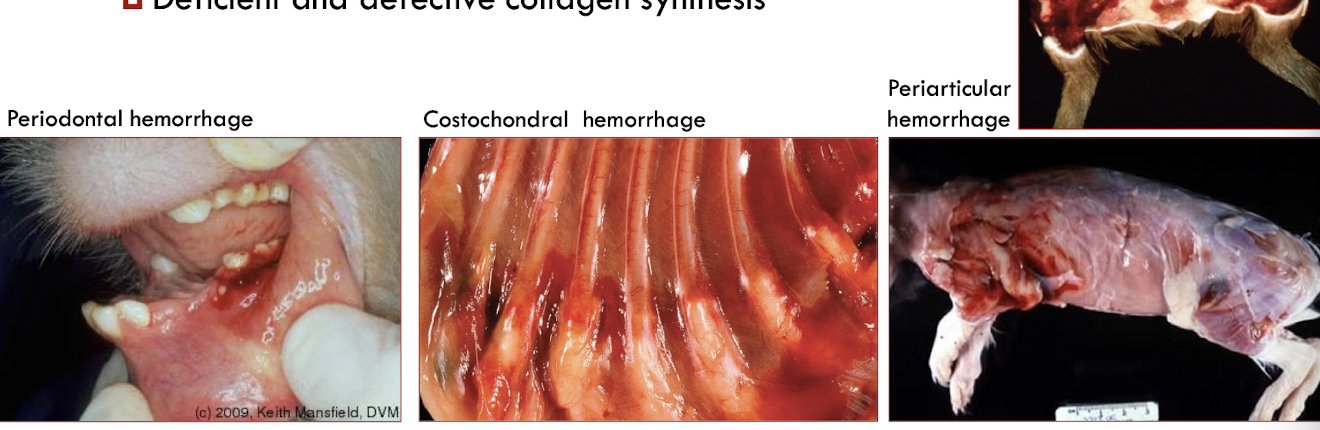
Vitamin C deficiency → scurvy
What purpose does ascorbic acid (vit C) serve?
serves as an enzyme cofactor
Species such as guinea pigs, primates, cetaceans, some bats, birds, and fish require a _________ source of Vitamin C. Why?
dietary
deficiency of L-gulonolactone oxidase (coverts L-gulonolactone to L-ascorbic acid)
Ascorbic acid serves as an enzyme cofactor for what? What are these required for?
prolyl and lysyl hydroxylases
required for the hydroxylation of proline & lysine during procollagen synthesis
What does a deficieny in hydroxylysine and hydroxyproline cause?
impaired function of intermolecular collagen cross-links
A vitamin C deficiency causes what?
deficient & defective collagen synthesis → bone, connective tissue, blood vessels (capillary fragility)
Vitamin C is also required for the synthesis of which important substances?
dopamine, norepinephrine, epinephrine, carnitine, wound healing, conversion of cholesterol into bile acids. antioxidant
What 2 platelet issues can cause hemorrhage?
decreased platelet numbers
abnormal platelet function
thrombocytopenia
decreased numbers of platelets
What are some things that can cause thrombocytopenia?
decreased production
increased destruction
increased use
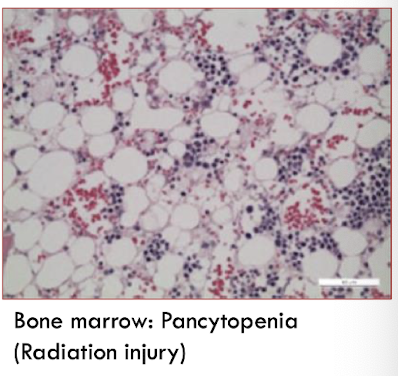
Decreased production of platelets leading to hemorrhage is due to what? Examples?
megakaryocyte damage or destruction
radiation, estrogen toxicity, cytotoxic drugs, viral diseases (parvo)
Increased destruction of platelets leading to hemorrhage is due to what? Examples?
immune mediated
drug rxn, viral diseases (EIA)
Increased use of platelets leading to hemorrhage is due to what? Examples?
diffuse endothelial damage or generalized platelet activiation
DIC
thrombocytopathy
decreased function of platelets
hereditary thrombocytopathy
deficiency of surface receptors → von Willebrand disease
acquired thrombocytopathy causes
NSAIDS (aspirin)
renal failure → uremia
Cause of hemorrhage?
decreased concentration of coagulation factors
Decreased concentration of coagulation factors can either be ________ or __________.
hereditary
acquired
What are the 2 categories of acquired coagulation factor decrease?
decreased production
increased use
What are the hereditary coagulation disorders?
X-linked hemophilias (A & B)
autosomal factor deficiencies
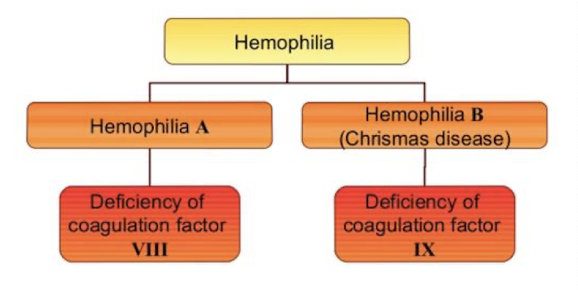
T/F: Clincial signs vary with hereditary coagulation disorders.
TRUE
Causes of decreased production leading to acquired coagulation disorders?
liver disease (dec synthesis)
vitamin K deficiency (dicumarol in moldy sweet clover, warfarin, sulfaquinoxaline)
Causes of increased use leading to acquired coagulation disorders?
disseminated intravascular coagulation (DIC)
thrombosis =
mechanisms involved in the formation of a thrombus in an injured blood vessel
thrombus
an aggregate of platelets, fibrin, & other blood elements formed on a vascular wall
What are the 2 types of thrombi?
physiological → normal hemostasis, rapidly resolved
pathological → persistent or inappropriate
What is Virchow’s Triad?
vascular injury → inflammation
altered blood flow → stasis or turbulence
hypercoagulability → inherited or acquired
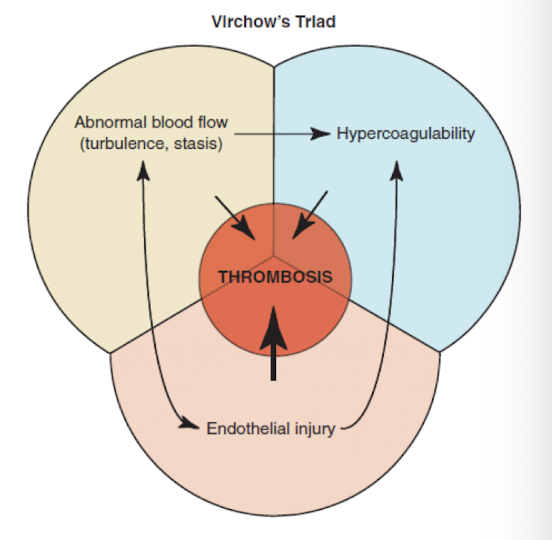
T/F: Alterations to endothelium (vascular injury) is the most important of aspect of Virchow’s Triad in vet med.
TRUE
What are the possible alterations to the endothelium leading to vascular injury?
increased production of procoagulant substances
decreased production of anticoagulant substances
What are some causes of vascular injury?
trauma, vasculitis, metabolic disorders, neoplasia
What happens when the endothelium is injured?
exposure of subendothelial collagen
release of TF (III)
platelet adherence & activation
local depletion of prostacyclin and tissue plasminogen activator
normal laminar blood flow
cells flow centrally in the blood vessel separated from the endothelium by a thin layer of plasma
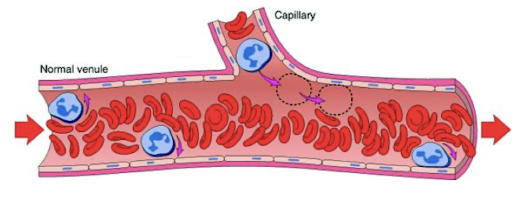
How does normal blood flow affect platelets?
keeps platelets away from endothelium preventing them from sticking
What can lead to stasis of blood flow?
heart failure (systemic)
vascular obstruction or dilation (local)
Slow rate of blood flow favors what?
accumulation of activated CoAg factors
contact of platelets with the endothelium
T/F: Turbulence does not disrupt laminar blood flow.
FALSE
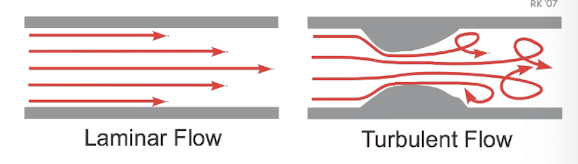
What does turbulence favor?
platelets interacting more with the endothelium
mixing of blood = more CoAg factor interaction
physical damage/ activation of the endothelium
When is turbulence the greatest?
where vessels branch
at a narrowing of the vessel lumen
at sites of venous or lymphatic valves
Hypercoagulability reflects what?
an increase or decrease in the concentration of activated hemostatic proteins
What are the 2 categories of hypercoagulability?
increased activation
decreased degredation
What is the most common cause of hypercoagulability?
INFLAMMATION
also: stress, surgery, neoplasia, pregnancy, renal disease
How does renal diease contribute to hypercoagulability?
loss of Antithrombin III and Protein C & S
What determines the gross appearance of thrombi?
dependent on underlying cause, location, & composition
What is the key point regarding thrombi?
they are ALWAYS attached to the vessel/ heart wall
The shape and appearance of arterial thrombi is determined by what?
rapid flow in arteries/ heart
Arterial thrombi are usually initiated by what?
endothelial damage → point of attachment
Arterial thrombi are composed primarily of what?
platelets and fibrin
Gross appearance of arterial thrombi:
dull, tan to red-gray
± vessel occlusion
tail extends down stream
laminated appearance
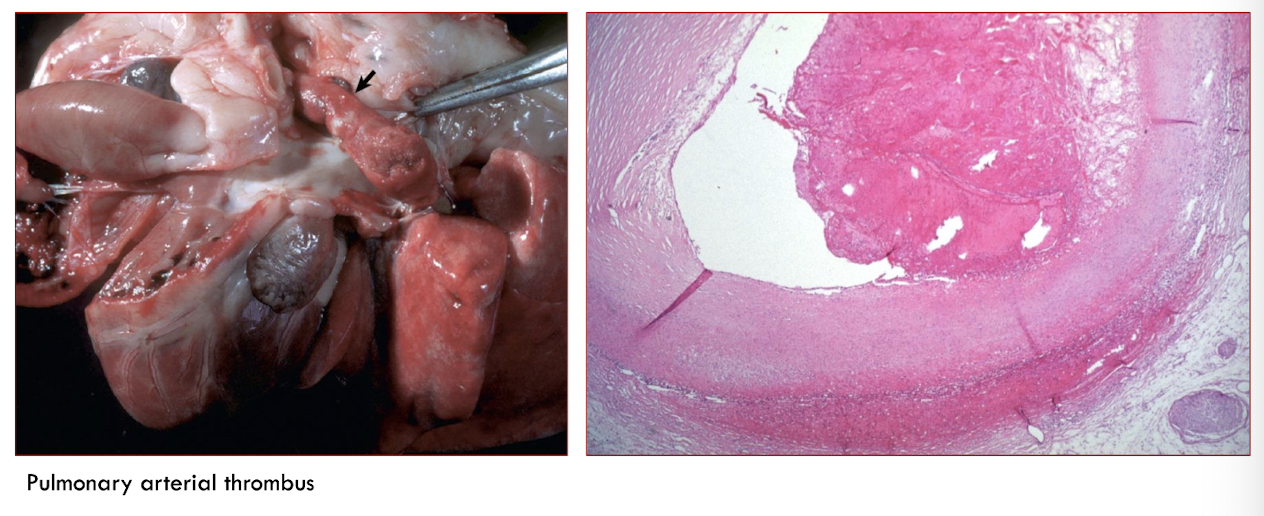
Lines of Zahn
alternating layers of platelets, interspersed by fibrin intermixed with erythrocytes and leukocytes
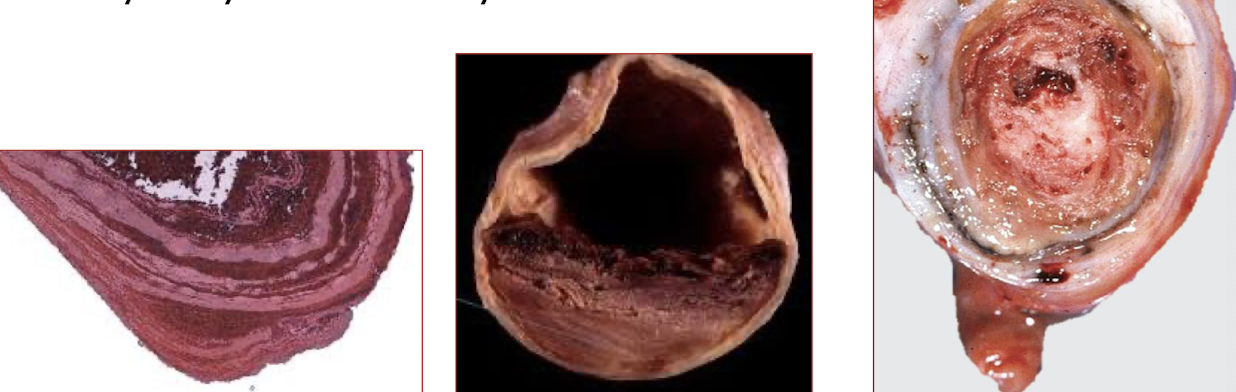
T/F: Lines of Zahn are characteristic of venous thrombi.
FALSE - arterial thrombi
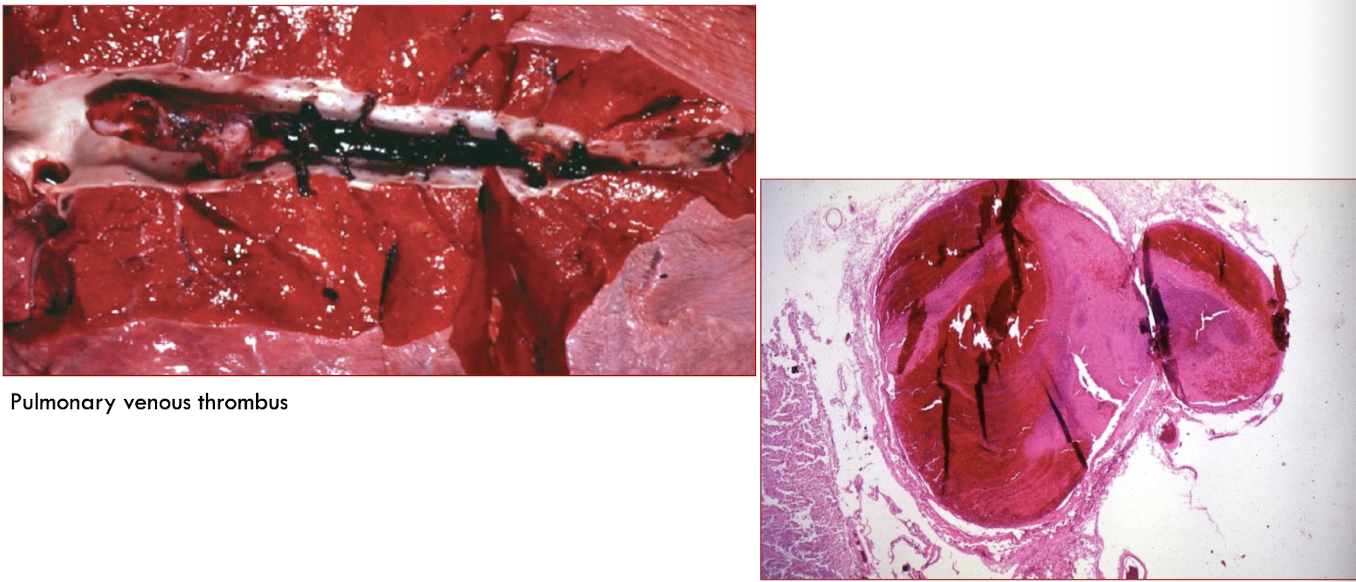
Venous thrombi often occur where?
in areas of stasis → increased activation of CoAg factors + reduced clearance
Low blood flow allows incorporation of _______ into a venous thrombus.
RBCs
What makes up a venous thrombus?
loose meshwork of platelets, fibrin, RBCs, and WBCs
gross appearance of venous thrombi:
gelatinous, soft, glistening
dark red
almost always occlusive → molded to wall
often extend upstream from point of origin
T/F: The point of origin of venous thrombi may be difficult to determine.
TRUE
Characteristics of postmortem clots:
softer
do NOT have point of attachment
do NOT have associated lesions
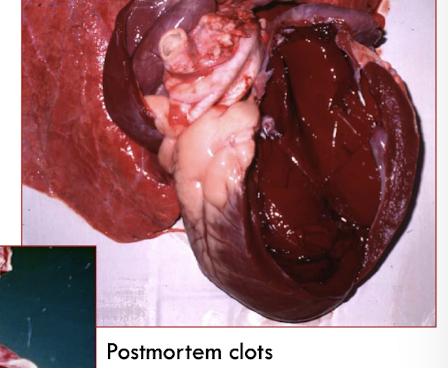
Gross appearance of postmortem clots:
current jelly: dark red
chicken fat: yellow
Significance of a thrombus is determined by what?
location & ability to disrupt perfusion in a dependent tissue
Significance of a thrombus based on size:
small vs large
non-occlusive vs occlusive
Significance of a thrombus based on rate of formation:
slow vs fast
Other determinants of thrombi significance:
method of resolution or repair
number of vessels affected