The Temporomandibular Joint
1/222
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
223 Terms
What are the components of the TMJ?
A temporal component and a mandibular component
What are the components of the temporal portion that contribute to the TMJ?
Mandibular fossa, and articular eminence
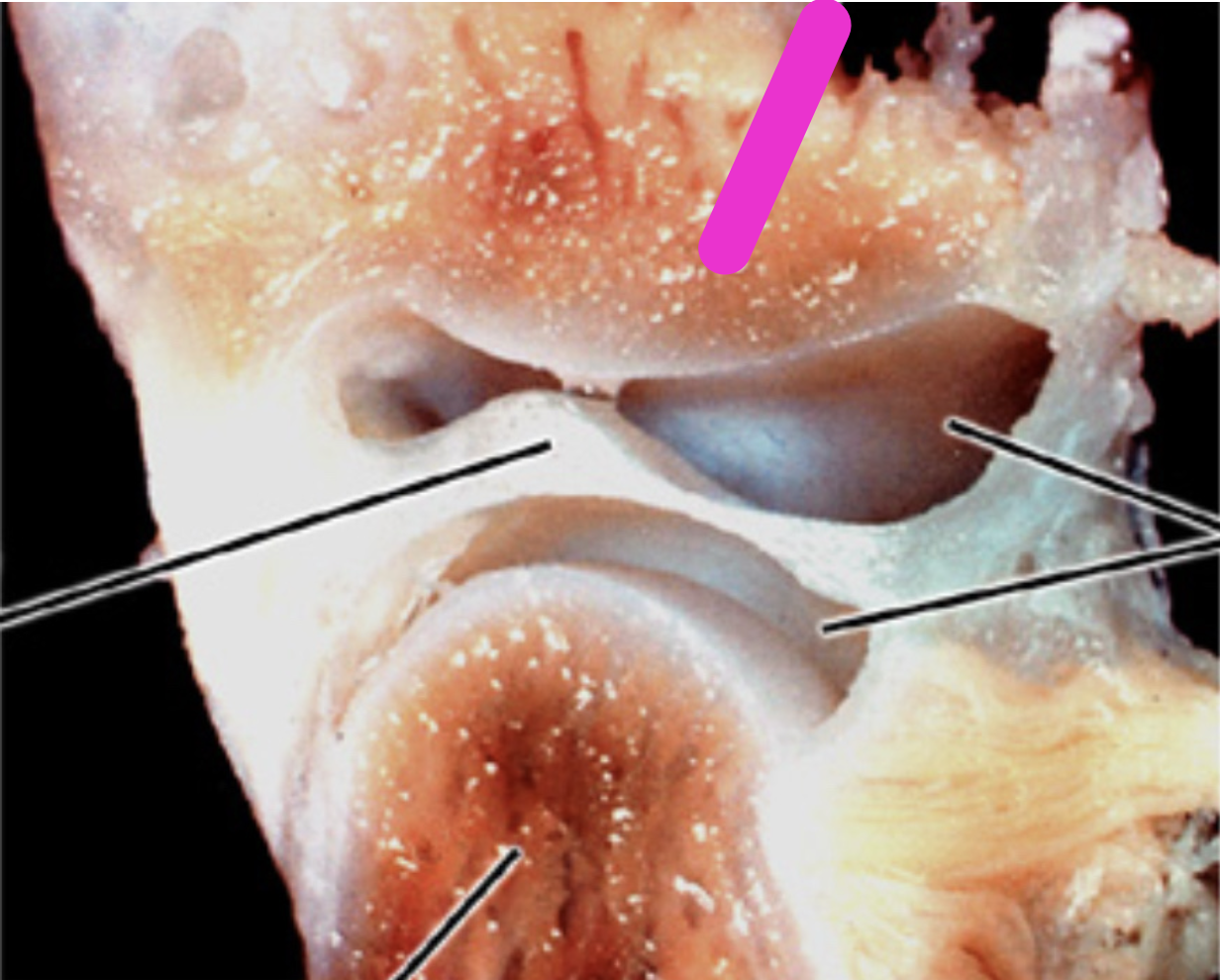
Identify the structure
Articular eminence
Identify the structure
Synovial cavity
Identify the structure
Articular Disc
Identify the structure
Condyle
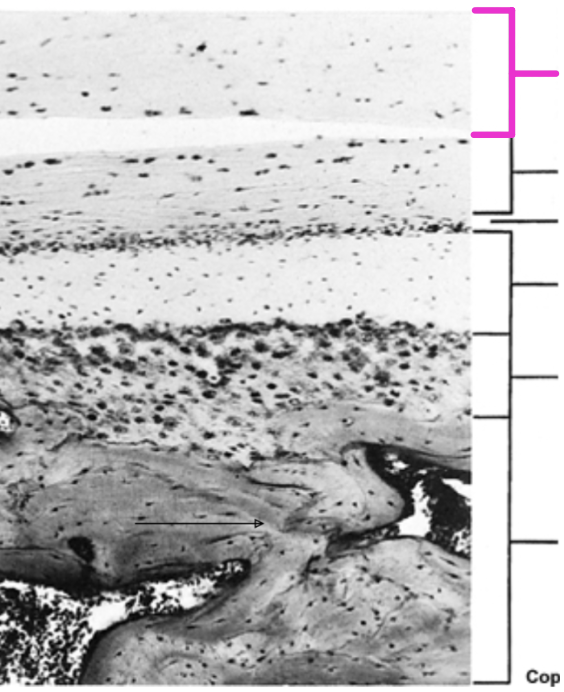
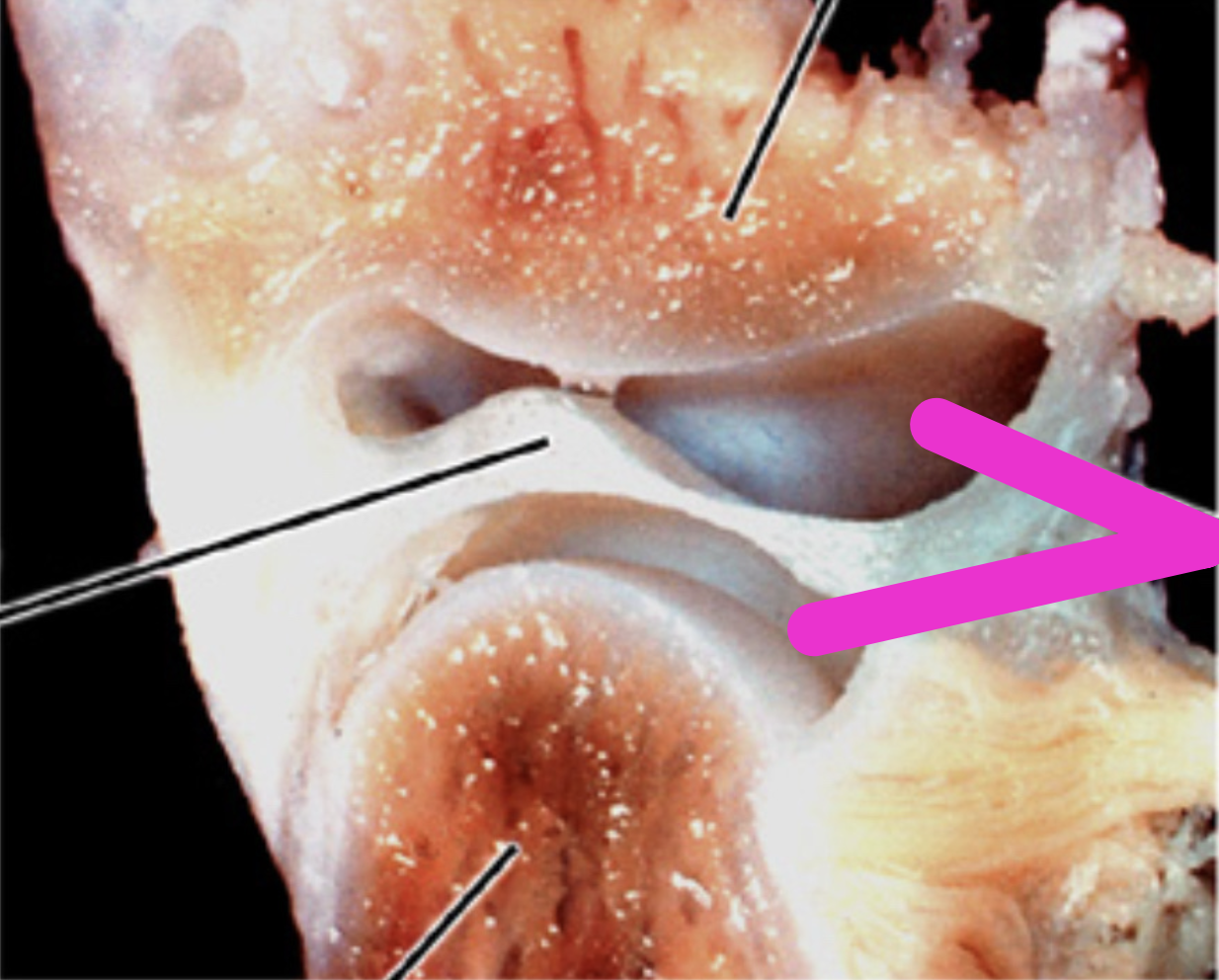
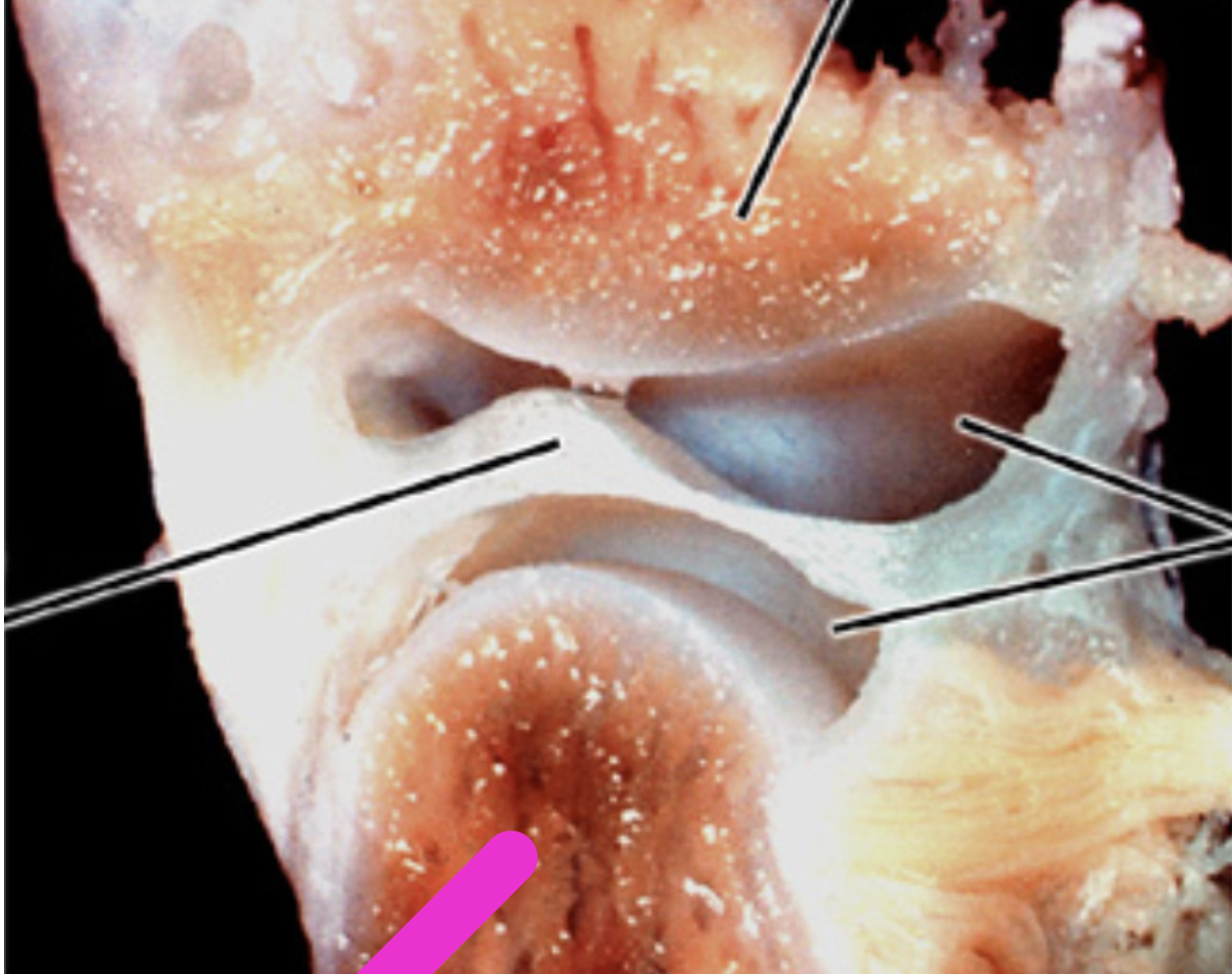
Identify the histological structure of the adult mandibular condyle
Articular Disk
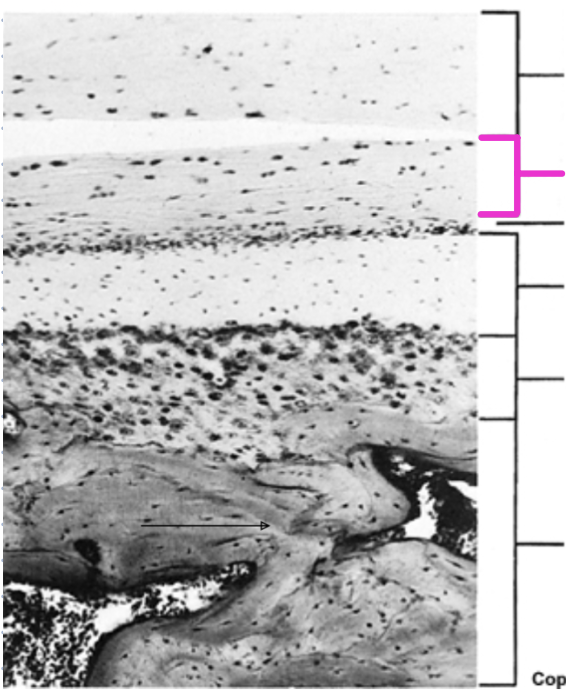
Identify the histological structure of the adult mandibular condyle
Articular Zone
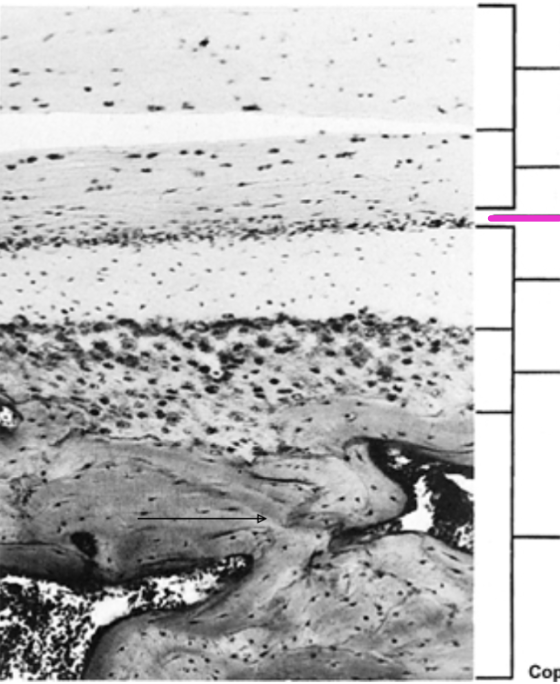
Identify the histological structure of the adult mandibular condyle
Proliferative Zone
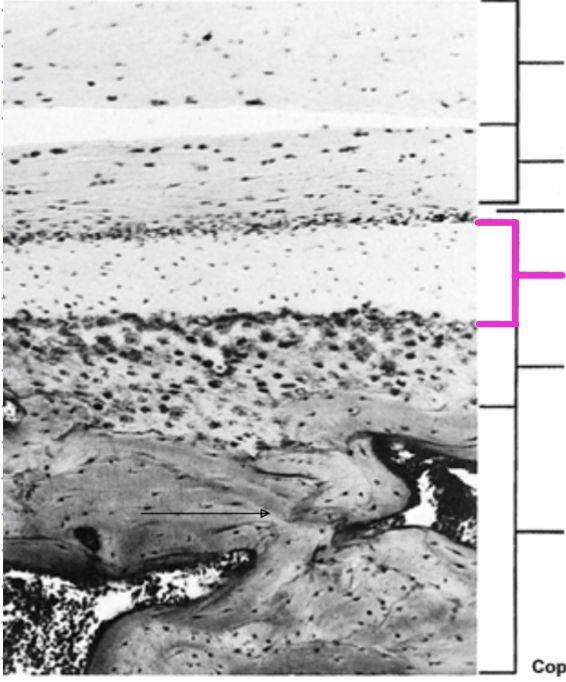
Identify the histological structure of the adult mandibular condyle
Fibrocartilaginous
Identify the histological structure of the adult mandibular condyle
Calcified cartilage
Identify the histological structure of the adult mandibular condyle
Subarticular bone
Histologically, what is the difference between mandibular fossa and articular eminence?
The mandibular fossa does not have a cartilage layer, the articular eminence has the same layers as the mandibular condyle (including cartilage)
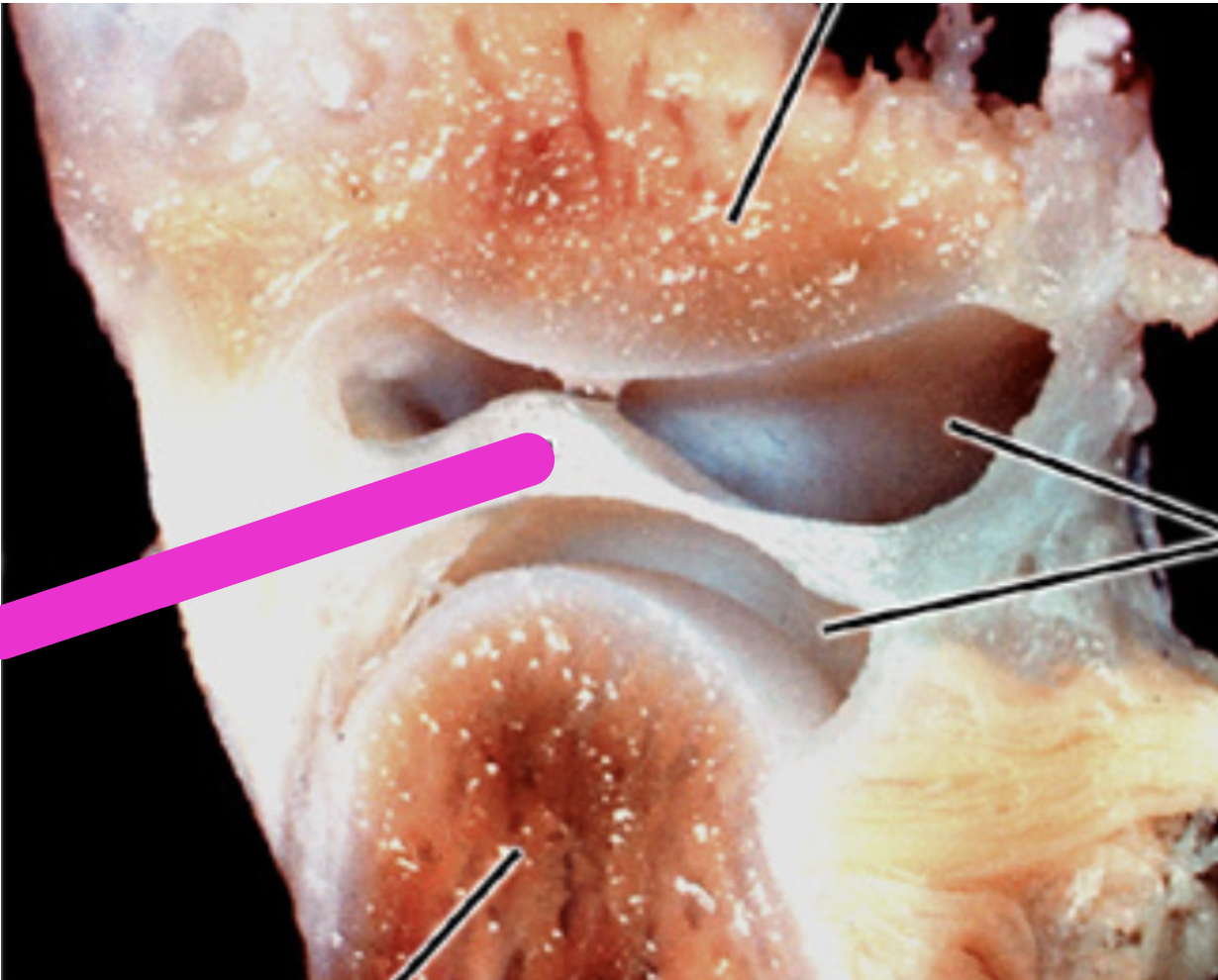
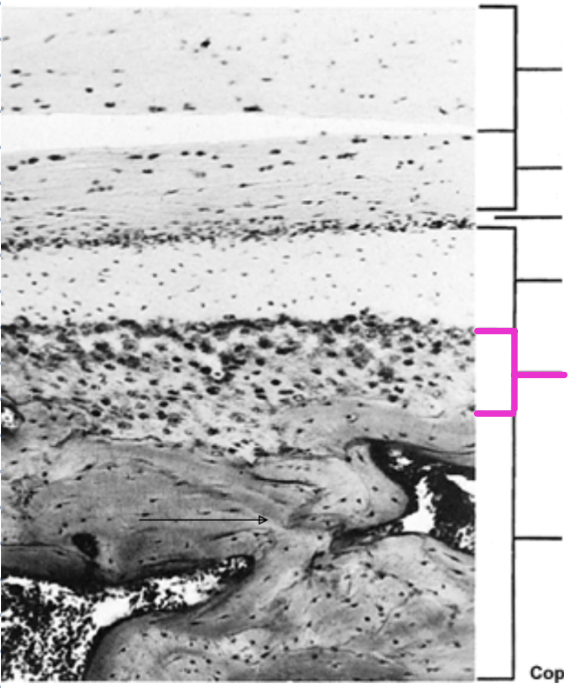
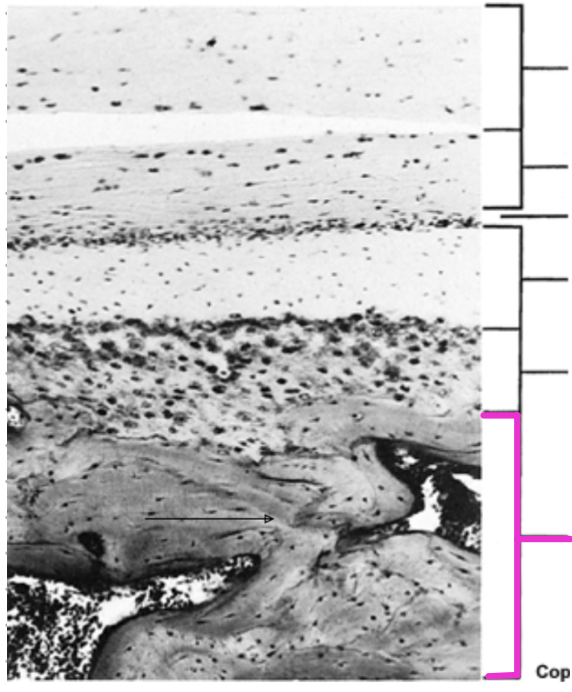
Layers of the mandibular fossa
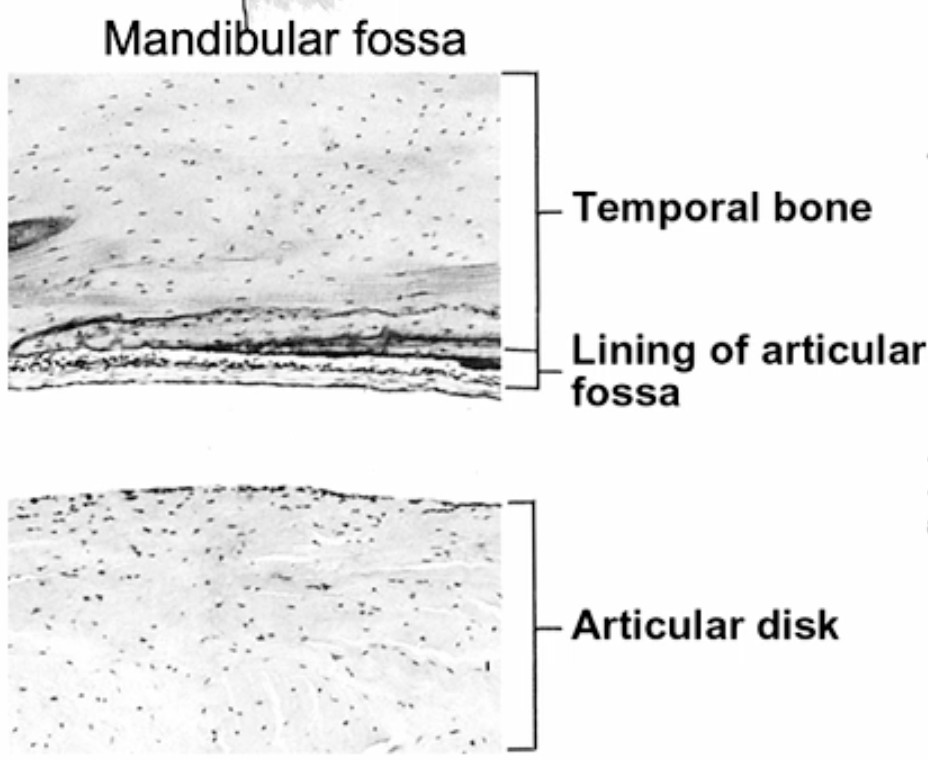
Layers of the Articular Eminence
The lining of the articular fossa
Is basically periosteum
What components make up the soft tissues of the TMJ?
Capsule
Articular disc
Ligaments
What does the capsule of the TMJ do and where does it attach?
The capsule surrounds the joint and attaches to the neck of the condyle and the temporal bone
What lines the inner part of the TMJ capsule?
The synovial membrane
How is the articular disc related to the TMJ capsule?
The articular disc is continuous with the capsule at its edges
What ligaments are associated with the TMJ?
Collateral ligaments and the lateral temporomandibular ligament
Where do the lateral and medial collateral ligaments of the TMJ attach?
The lateral collateral ligament attaches the disc to the lateral pole of the condyle; the medial collateral ligament attaches the disc to the medial pole of the condyle
What is the TMJ ligament and where is it located?
A structure on the lateral side of the joint that stabilizes the TMJ
What are the two parts of the TMJ ligament?
Outer oblique ligament: runs from the articular tubercle to the neck of the condyle
Inner horizontal ligament: runs from the articular tubercle to the lateral pole of the condyle
Why is there a lack of medial ligament reinforcement in the TMJ?
Because the medial side is already reinforced by bone
What is the connection formed by the lateral ligament of the TMJ?
Connects the zygomatic arch to the neck of the condyle
Image of the TMJ ligaments
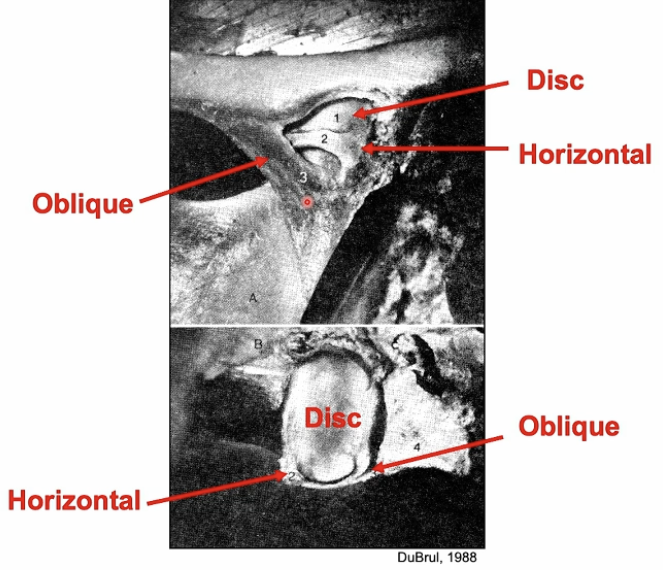
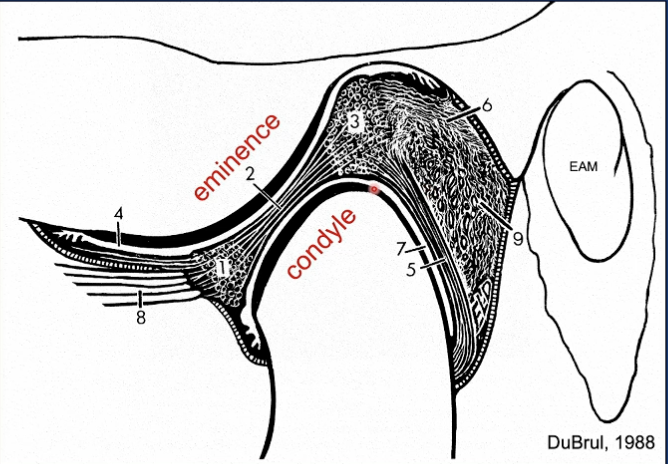
Identify structure 1
Anterior band
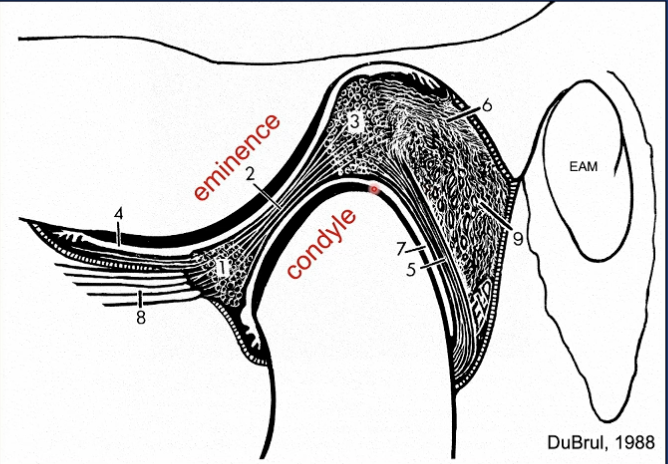
Identify structure 2
Intermediate band
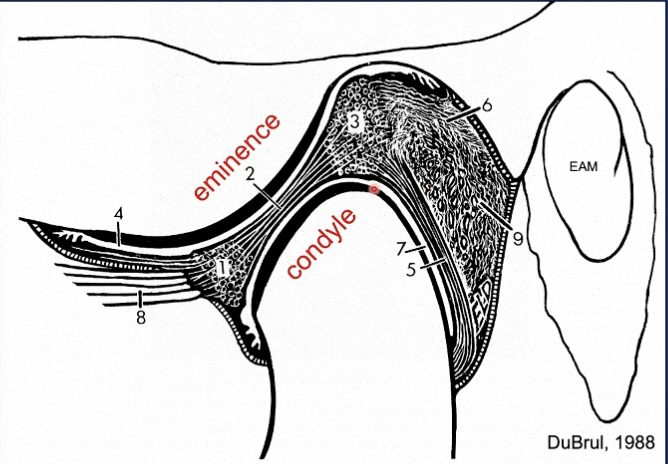
Identify structure 3
Posterior band
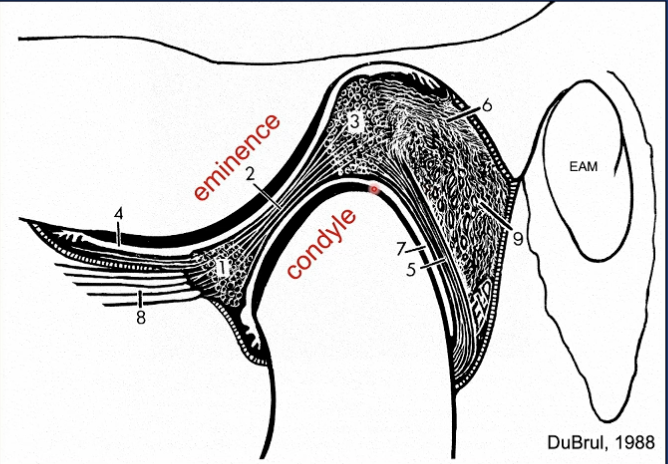
Identify structure 4
Superior joint cavity
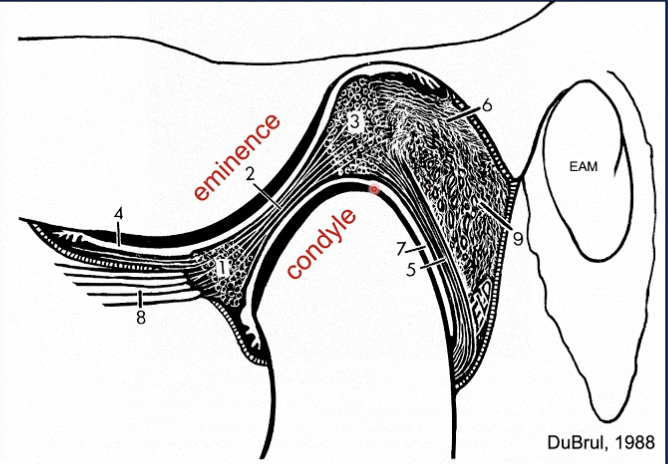
Identify structure 5
Inferior lamina
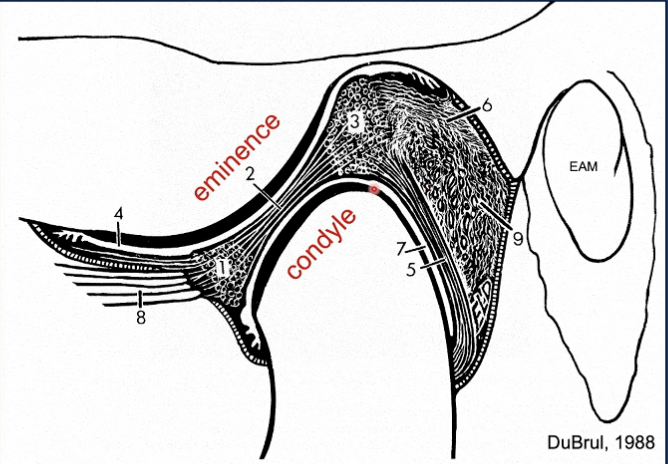
Identify structure 6
Superior lamina

Identify structure 7
Inferior joint cavity
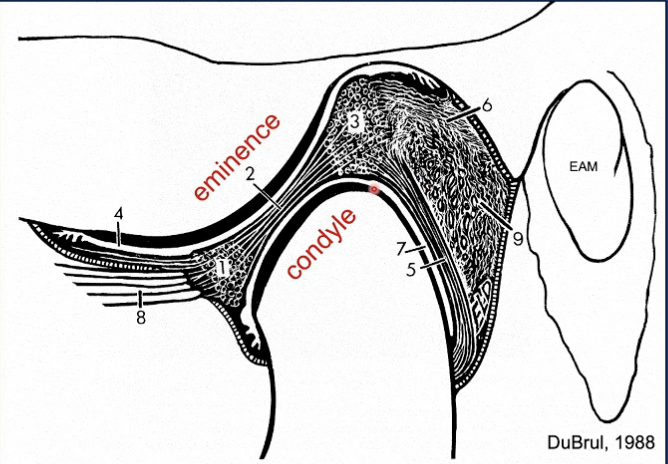
Identify structure 8
Lateral pterygoid
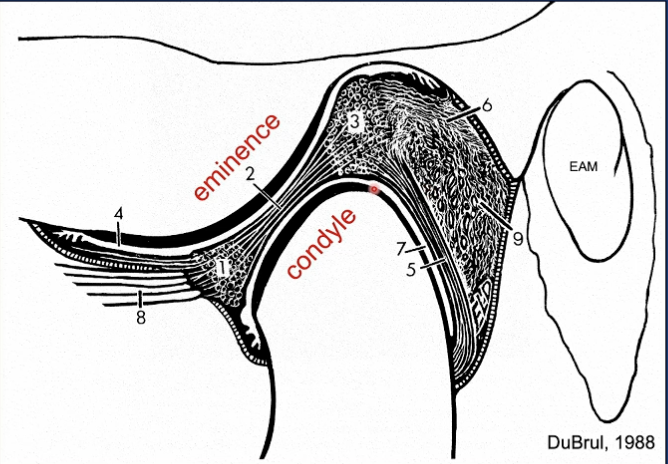
Identify structure 9
Retrodiscal pad
What does the superior lamina attach to?
The temporal bone
What does the inferior lamina attach to?
The neck of the condyle
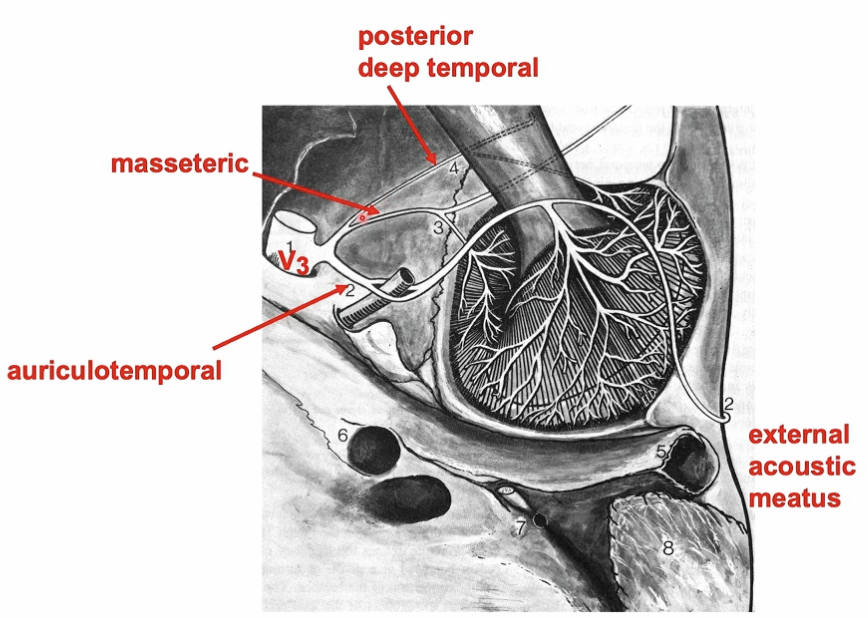
The auriculotemporal nerve is a branch of
V3 - Trigeminal
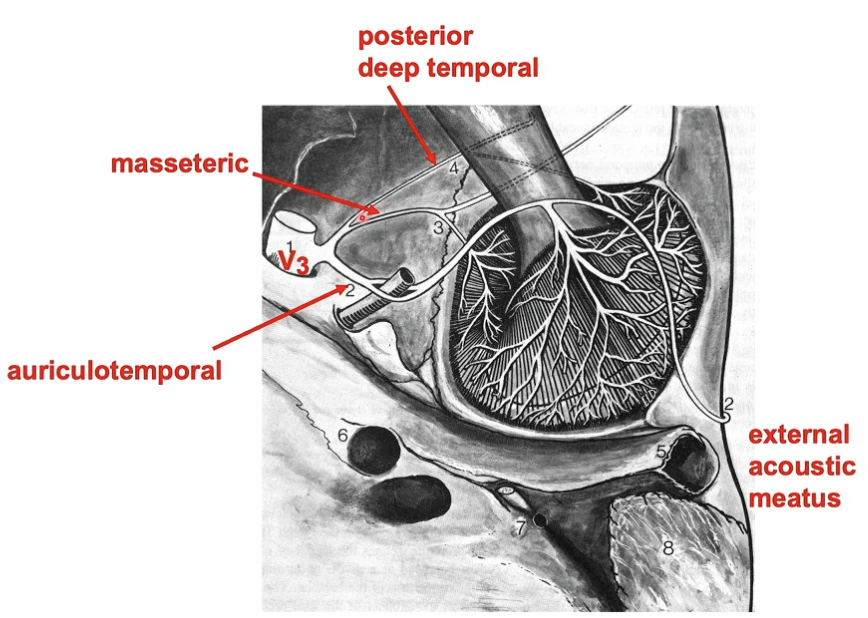
Where does V3 leave the skull?
Foramen ovale
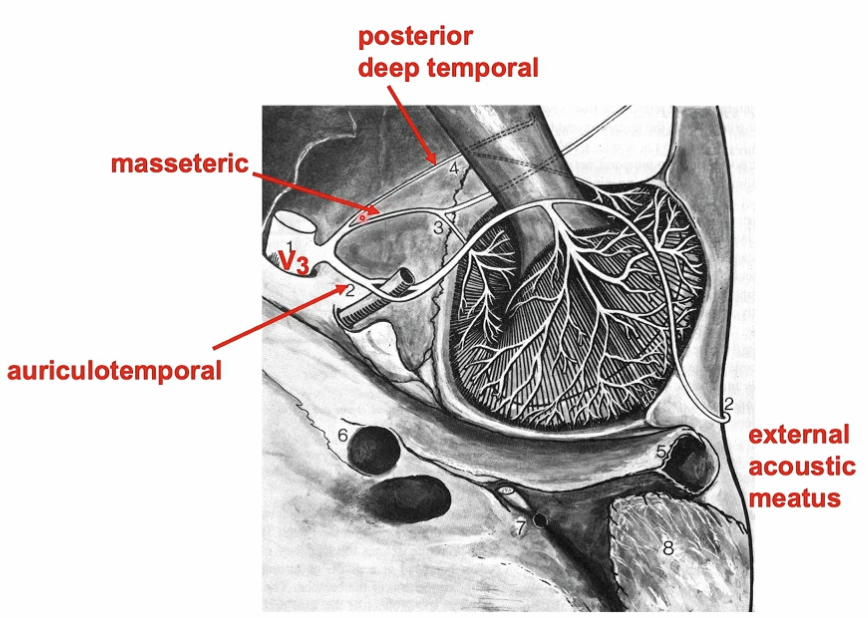
Which division of the trigeminal nerve are the masseteric and posterior deep temporal nerves part of?
V3 (the mandibular division of the trigeminal nerve)
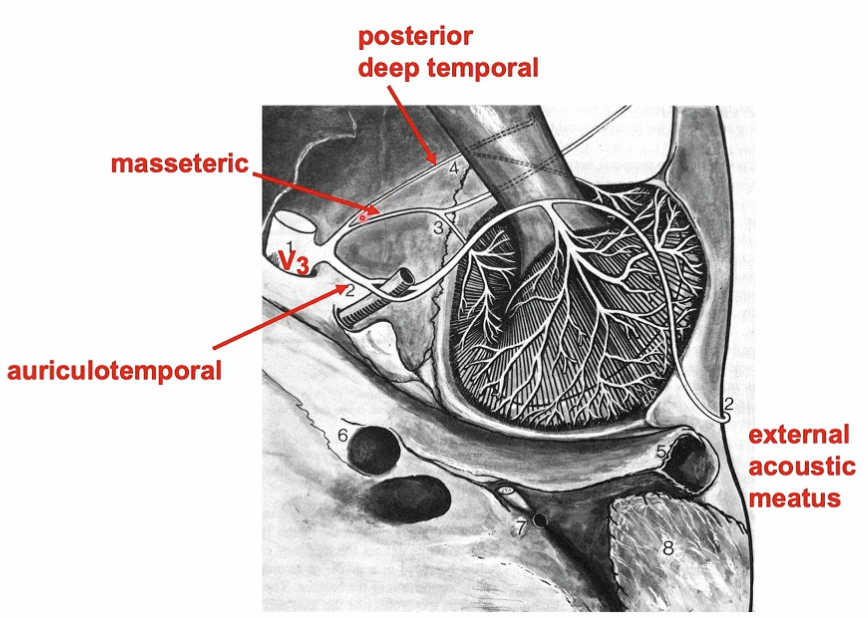
What muscles do the masseteric and posterior deep temporal nerves innervate?
Masseteric nerve → Masseter muscle
Posterior deep temporal nerve → Temporalis muscle
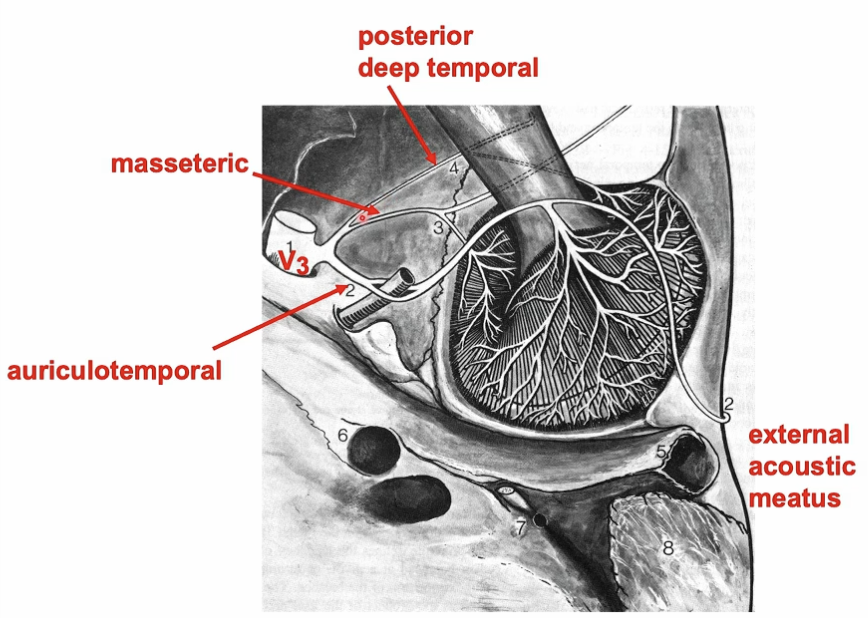
Besides motor function, what other role do the masseteric and posterior deep temporal nerves have?
They carry sensory fibers that supply the anterior part of the TMJ capsule
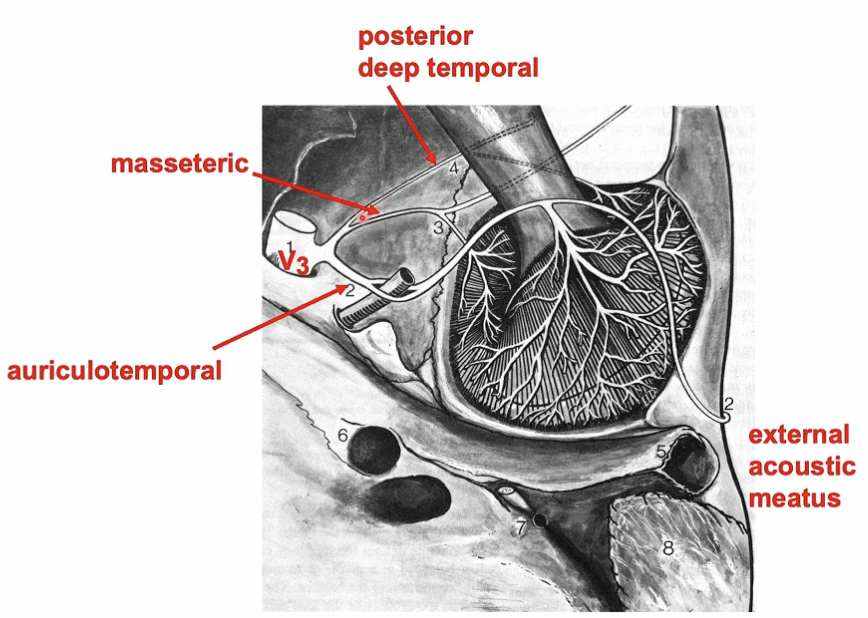
Which part of the TMJ capsule receives sensory innervation from the masseteric and posterior deep temporal nerves?
The anterior part of the capsule
What types of nerve endings are found in the TMJ?
The same types as in other joints: free nerve endings and corpuscular (specialized) nerve endings
What type of nerve endings make up about 80% of all nerve endings in the TMJ?
Free nerve endings (nociceptors)
What stimulates the free nerve endings in the TMJ?
Injury and inflammation
Where are free nerve endings located in the TMJ?
They are widely distributed throughout the joint capsule, retrodiscal tissue, synovial membrane, and on the periphery of the disc where it is adjacent to the capsule
Does the center of the articular disc or the articular surfaces of the TMJ have nerves or blood vessels?
No, both are not innervated and avascular
TMJ pain comes from surrounding soft tissues instead
What does Ruffini’s corpuscle do?
Dynamic proprioception that detects mostly static position, and velocity
What does Pacini’s corpuscle do?
Dynamic mechanoreception that detects accelerations and decelerations when in motion, and send that information back to the brain
What is the Golgi tendon organ?
A stretch reception found in the TMJ ligament
What type of cells are found in the TMJ disc?
Fibrochondrocytes
What is the composition of fibrochondocytes?
They can be fibroblasts or cartilage cells, depending on the circumstances, not both at the same time
What type of tissue is the TMJ disc made of?
Fibrocartilage
What type of cells are fibrochondroblasts, and how do they change with age?
They are similar to fibroblasts but may become more like chondrocytes in older individuals
What type of collagen is found in the TMJ disc, and what does it do?
The disc has Type I collagen, which provides tensile strength
What are glycosaminoglycans (GAGs) in the TMJ disc and what role do they play?
(Mainly chondroitin sulfate and dermatan sulfate) are bound with water and give the disc strength under compression
Is the TMJ disc vascularized and innervated?
The disc is avascular and lacks innervation, but the periphery where the disc meets the capsule is rich in blood and nerve supply
What does the extracellular matrix of the TMJ disc consist of?
fibrous connective tissue (mostly Type I collagen, some elastin) and glycosaminoglycans (GAGs) bound to a protein core to form proteoglycans
What happens to the type of collagen expressed in the TMJ disc with age?
In younger individuals, the disc expresses Type I collagen (fibroblast phenotype). In older individuals, Type II collagen (chondrocyte phenotype) may be expressed, indicating more cartilage-like cells
Superior view of disc
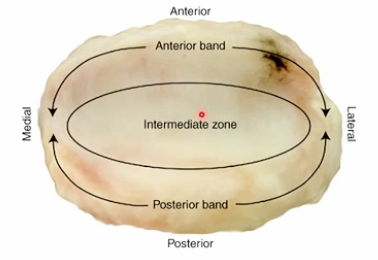
In the TMJ disc, what direction do the collagen fibers in the anterior and posterior bands run?
Mediolateral
In the intermediate band of the TMJ disc, what direction do the collagen fibers run?
Anteroposterior
What is the shape of the TMJ disc from a superior view?
Oval-shaped
How is the TMJ disc attached to the condyle?
The disc is attached to the poles of the condyle by the collateral ligaments
What is the structure of the collagen fibers in the anterior and posterior bands of the TMJ disc?
Mediolateral direction, forming an annulus
What is the size of the intermediate zone
Thinner
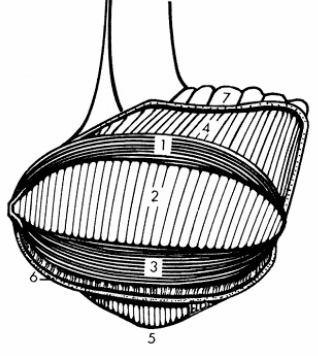
What is 1 and 3?
Anterior and posterior bands - collagen fibers run mediolaterally
What is 2 and 4?
Intermediate band - collagen fibers run anteroposteriorly
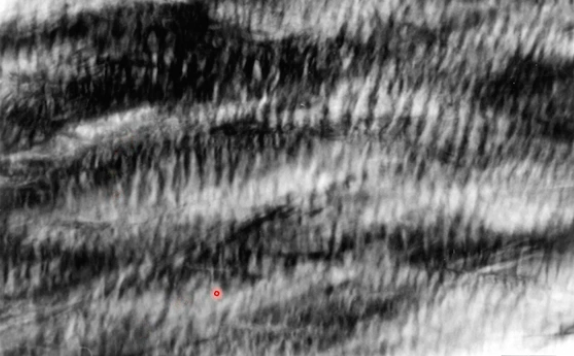
What is this
Intermediate zone - bunched up collagen fibers like an elastic waistband
In which direction is the TMJ disc stiffer and stronger, based on tensile testing?
In the anteroposterior (AP) direction compared to the mediolateral (ML) direction
Why is the TMJ disc stiffer and stronger in the AP direction?
because the collagen fibers are aligned to resist tension in that direction
this is also the direction of disc translation and stretching
What does the tensile testing of the TMJ disc show about the relationship between loading rate and mechanical properties?
The strength and stiffness of the TMJ disc vary with loading rate, indicating that the disc has viscoelastic properties
What is the primary role of synovial fluid in the TMJ?
Lubricate the joint, decrease friction, and nourish the articular tissues
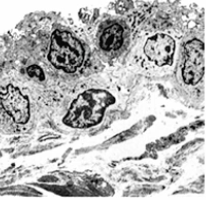
What is this a picture of?
Synovial membrane
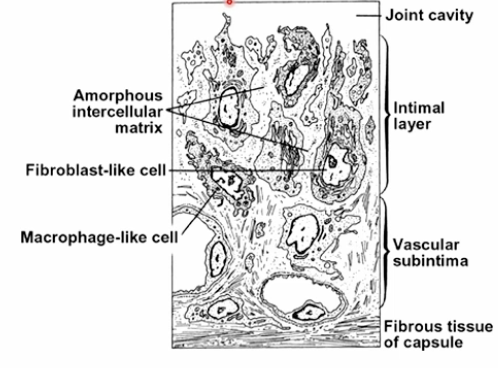
Labeled synovial membrane histological image
What drives the movement of synovial fluid in the TMJ during function?
The forces that occur during function
Where is the synovial membrane located in the TMJ?
The joint capsule
What is the structure of the cellular layer of the synovial membrane?
The cellular layer faces the joint cavity and sits on a vascular layer
What type of cells are found in the cellular layer of the synovial membrane, and what are their functions?
Fibroblast-like cells make hyaluronan, and macrophage-like cells remove debris
How do the cells in the synovial membrane interact with the loose connective tissue matrix?
The cells in the synovial membrane have no junctional complexes and are floating in the loose connective tissue matrix
What is the function of the subintima layer of the synovial membrane?
It has vessels that allow plasma (a major component of synovial fluid) to leak out of the capillaries and between cells to contribute to fluid
What components make up synovial fluid in the TMJ?
Dialysate of plasma, hyaluronan, and sugars, which lubricate and nourish joint tissues
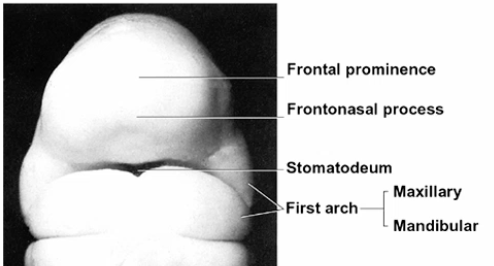
What are the basic components of the first branchial arch?
Mesoderm
Neural crest cells
Nerve
Artery
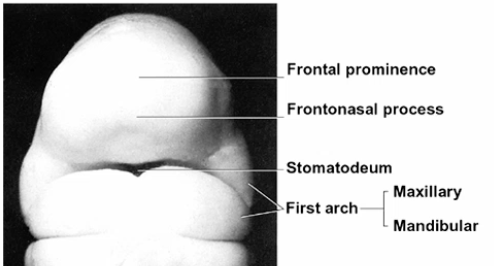
What does the first branchial arch do?
Maxillary and mandibular processes give rise to the jaws
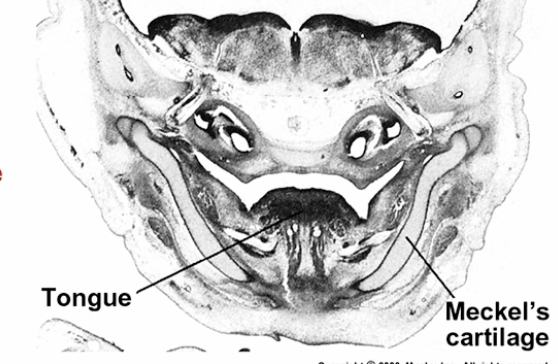
What does Meckel’s cartilage do?
Provides a template for the development of the mandible
What happens to meckel’s cartilage?
It resorbs and goes on to become parts of the middle ear
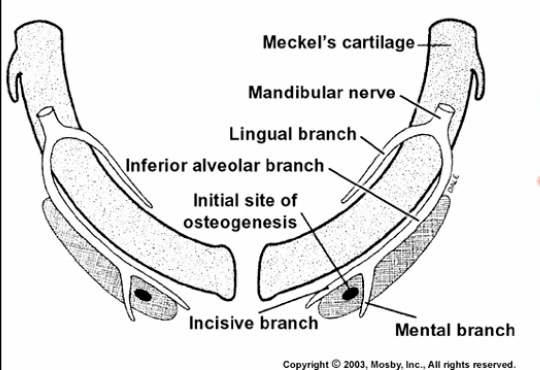
Most of the mandible is formed by
Intramembranous ossification
How many distinct mesenchymal condensations form around Meckel’s cartilage during fetal development?
At least seven developmentally and functionally distinct condensations of mesenchyme around Meckel’s cartilage
What type of ossification occurs in the mesenchymal condensations around Meckel’s cartilage to form the mandible?
intramembranous ossification
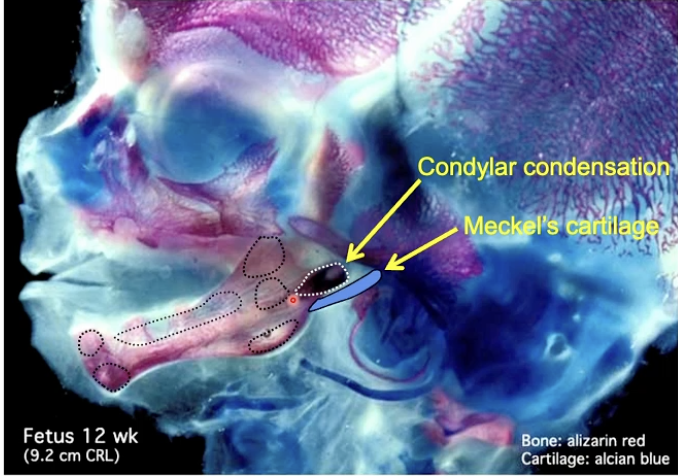
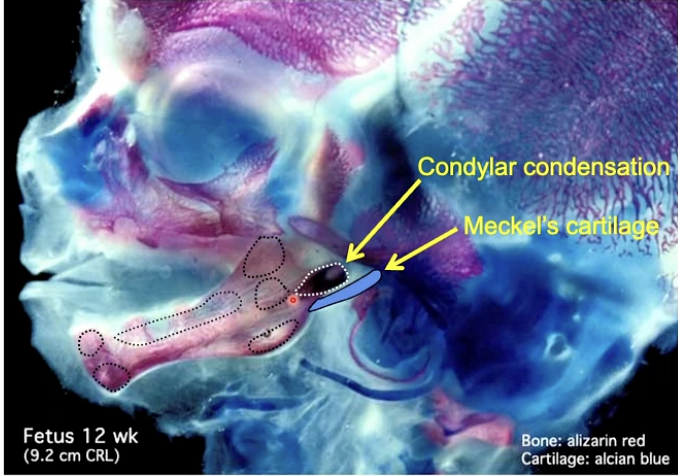
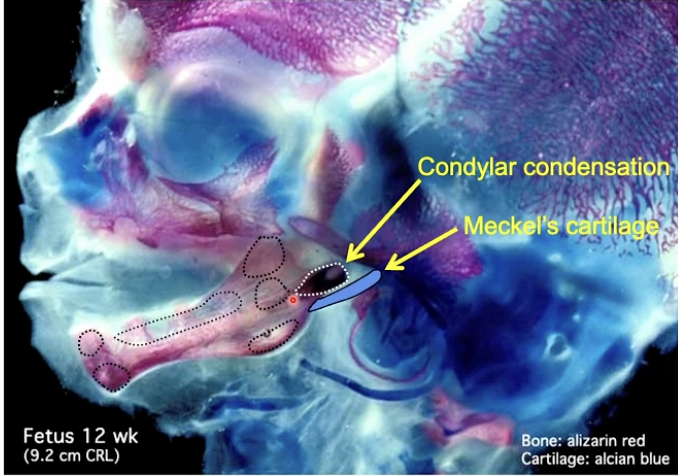
Where does the condylar condensation form in relation to the mandible during fetal development?
at the superior-posterior ramus of the mandible
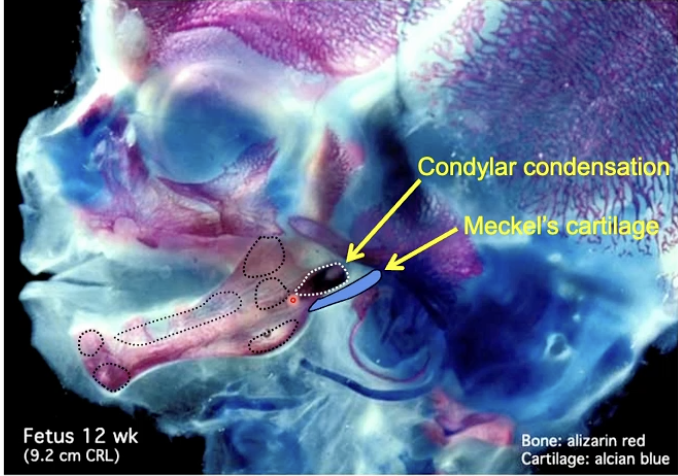
Where is Meckel’s cartilage located during fetal development?
medial to the mandible
What is the role of the temporal condensation during fetal development?
The temporal condensation forms in the optic capsule of the cranial base
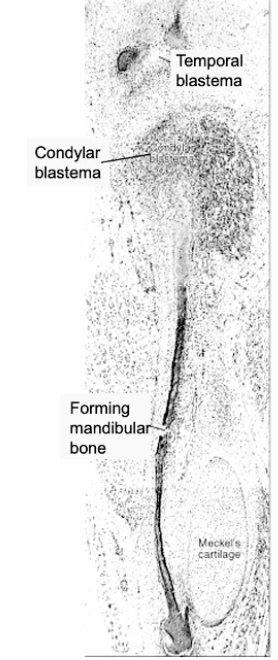
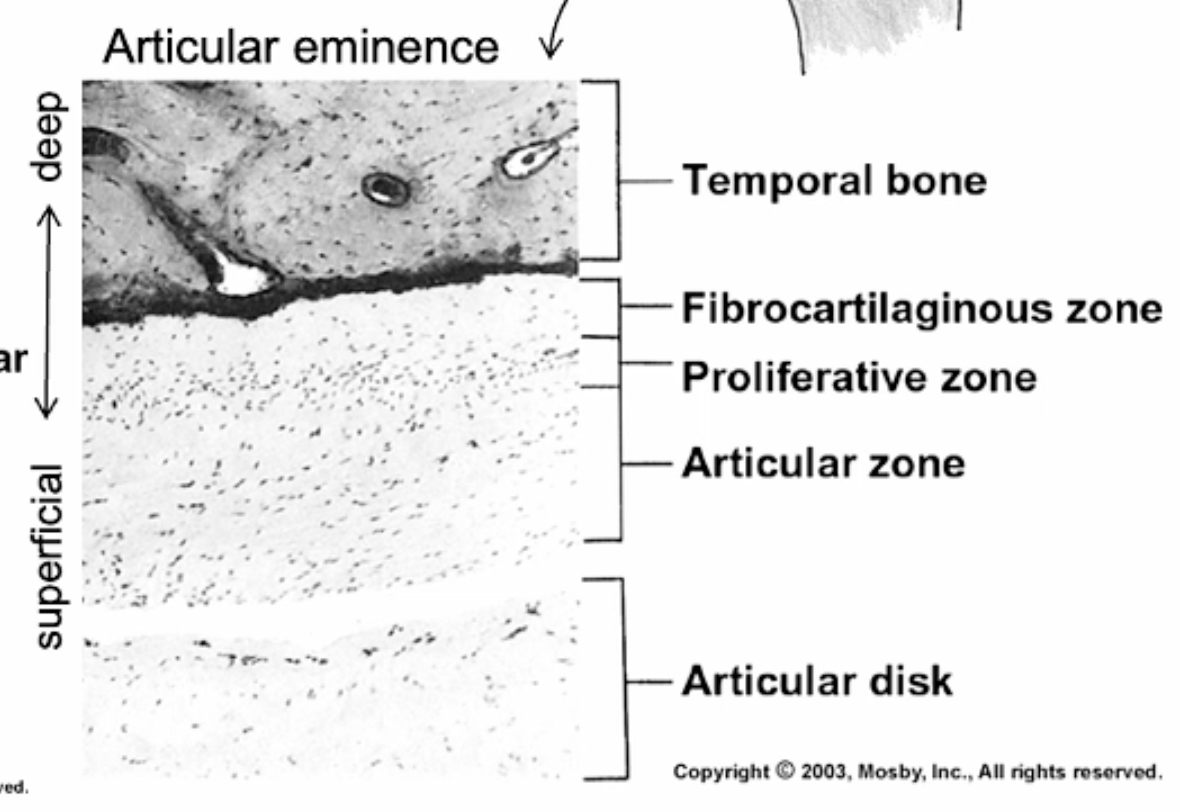
What is this
A histological image of the condensation (blastima) stage
What is the mesenchymal stage of TMJ development, and when does it occur?
The condensation (blastima) stage occurs during weeks 7-8. During this stage, mesenchymal cells are loosely arranged in a “mesenchyme soup”
What happens during the condensation stage of TMJ development?
mesenchymal cells become organized into a discreet clump at the site of the future condyle
What occurs during the cavitation stage of TMJ development, and when does it occur?
Weeks 9-11
cartilage formation begins in the central region
mesenchymal cells differentiate into chondroblasts that produce the cartilage matrix
What happens during the cavitation stage with regard to joint cavity formation?
spaces coalesce, starting inferiorly adjacent to the condyle and then superiorly near the squamous part of the temporal bone, forming the joint cavities
What occurs during the maturation stage of TMJ development, and when does it occur?
Weeks 12-17
The joint capsule and disc develop attachments
Meckel’s cartilage becomes smaller
Endochondral ossification of the condyle begins