Introduction to Antimicrobials
1/32
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
33 Terms
antimicrobials
-drugs that destroy microbes, prevent their multiplication or growth, or prevent their pathogenic action
-differ in physical, chemical, pharmacological properties
-differ in antibacterial spectrum of activity
-differ in their mechanism of action
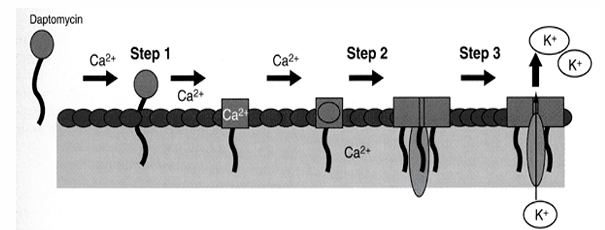
antibiotic classes (by mechanism of action)
-inhibit cell wall synthesis
-inhibit protein synthesis
-alter nucleic acid metabolism
-inhibit folate metabolism
-other mechanisms
antibiotic classes- inhibit cell wall synthesis
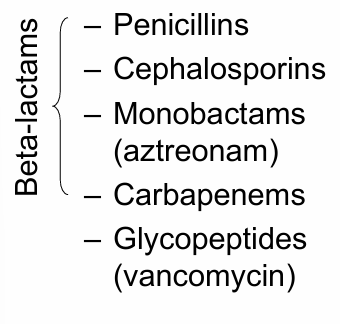
antibiotic classes- inhibit protein synthesis
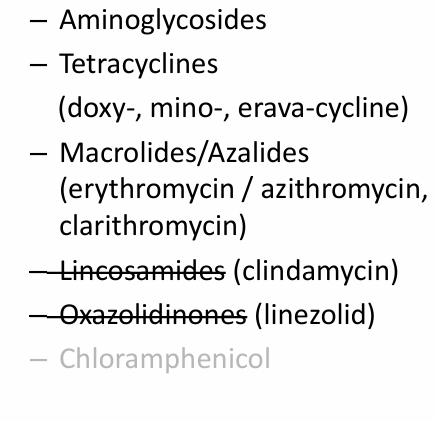
antibiotic classes- alter nucleic acid metabolism
-Rifamycins
-Fidaxomicin
-Quinolones
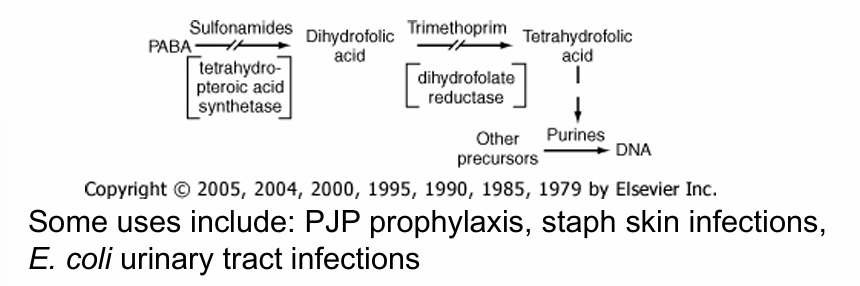
antibiotic classes- inhibit folate metabolism
-trimethoprim
-sulfonamides
antibiotic classes- miscellaneous
-metronidazole
-lipopeptides (daptomycin)
-polymyxins
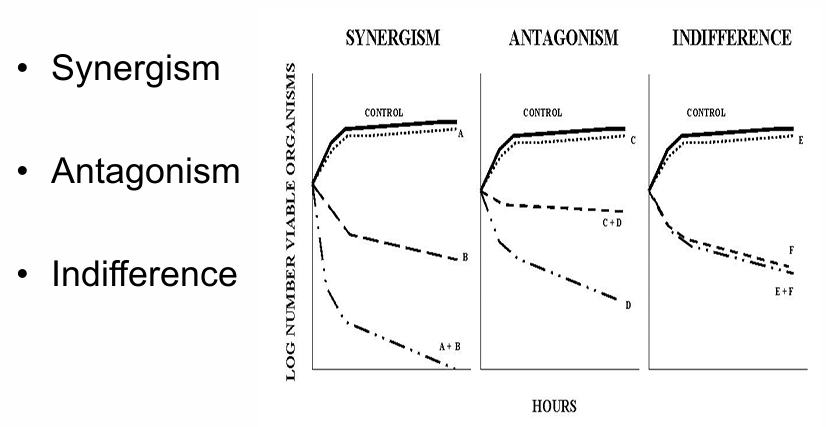
antibiotic targets
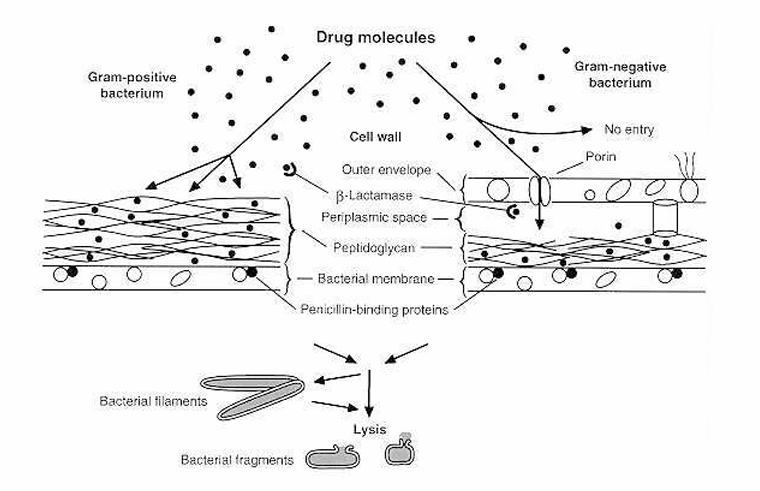
beta-lactams
-all contain the beta-lactam ring with 3 carbon atoms and one nitrogen atom
-inhibit synthesis of the peptidoglycan layer of the cell wall by blocking the action of transpeptidases (penicillin binding proteins)
-includes: penicillins, cephalosporins, monobactams, and carbapenems
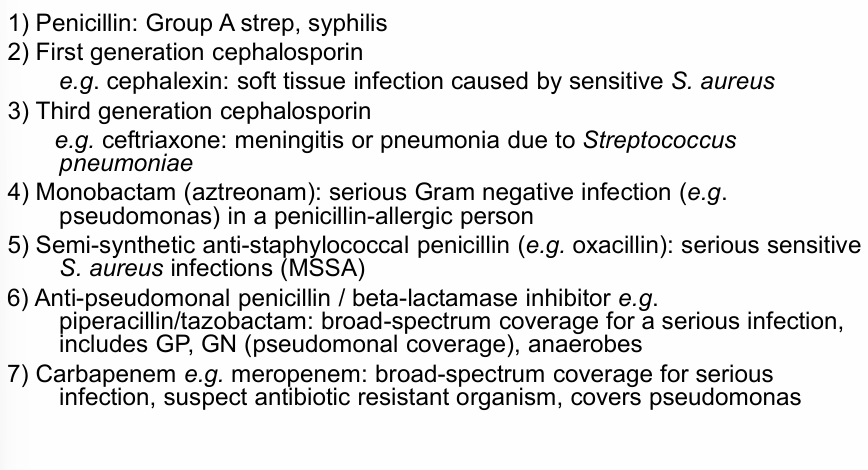
examples of uses of beta-lactam antibiotics
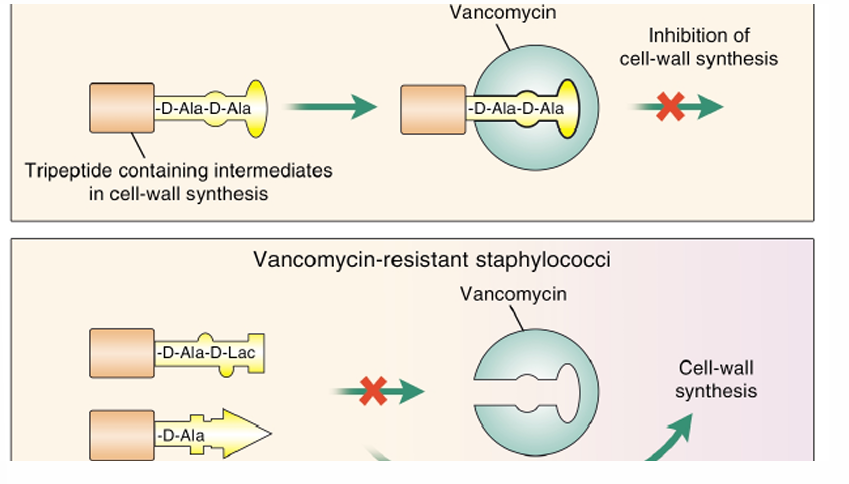
vancomycin (glycopeptide)
-inhibits cell wall synthesis by interfering with peptidoglycan synthesis
-binds to the D-Ala-D-Ala terminals of N-acetylmuramic acid (NAM)- N-acetylglucosamine (NAG)-peptide subunits
-prevents cross-linking of the peptidoglycan chains
-with a rare exception, only active against gram positive bacteria
-used for serious infections caused by methicillin-resistant Staphylococci
vancomycin and vancomycin-resistant staphylococci
protein synthesis inhibitors
-inhibit translation of bacterial proteins in various ways
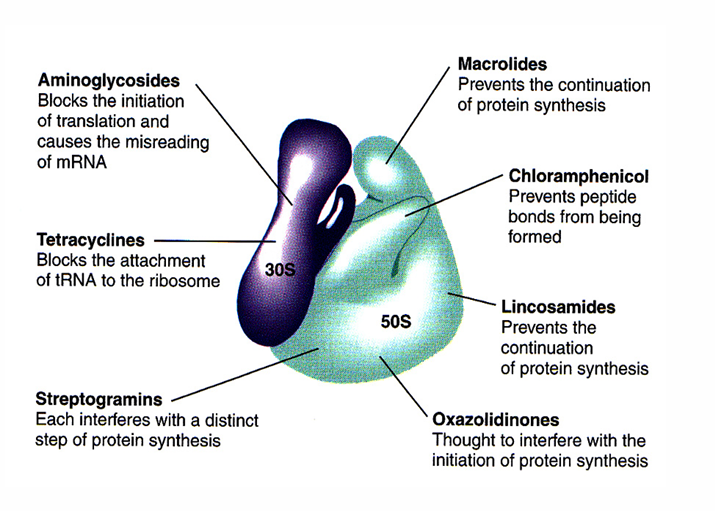
examples of uses of protein synthesis inhibitors
rifamycins (rifampin, rifabutin)
-mechanism of action: blocks mRNA synthesis (prevents transcription of bacterial DNA) by binding to the bacterial DNA-dependent RNA polymerase
-used in combination with other antimicrobials
Fidaxomicin
-another option for C. difficile diarrhea: very expensive, usually reserved for immunocompromised host or recurrence, vancomycin and metronidazole are alternatives
-inhibits transcription, binds to DNA template-RNA polymerase complex and prevents the initial separation of DNA strands oral- the subunit it binds to is different in different bacterial species
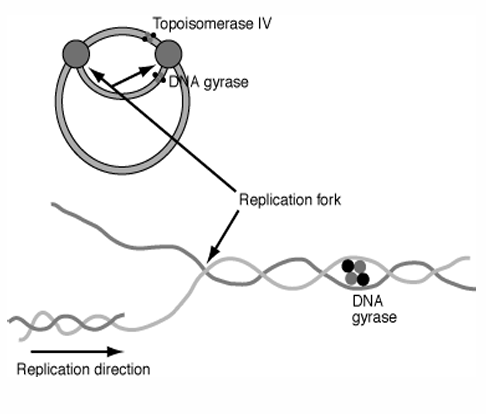
quinolones
-inhibit DNA synthesis
-inhibit the topoisomerases responsible for supercoiling DNA (DNA gyrase) and relaxing the supercoiled DNA (topoisomerase IV)
-examples: ciprofloxacin, levofloxacin, moxifloxacin
inhibitors of folate metabolism
-examples: trimethoprim, sulfonamides
-often given in combination (example: trimethoprim-sulfamethoxazole)
metronidazole
-diffuses into the cell and is reduced
-metronidazole free radicals interfere with organism DNA causing breakage, destabilization, and cell death
-active in anaerobes (e.g. Bacteroides, C. diff) and select parasites such as Entamoeba and Giardia
metronidazole- mechanism of action of anaerobes
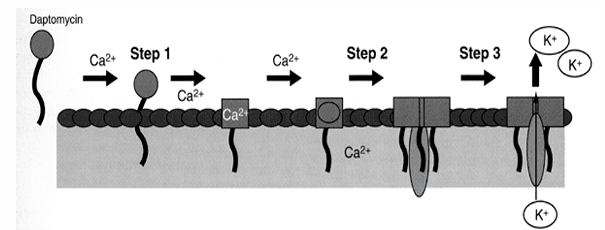
daptomycin (lipopeptide)
-binds to the cell membrane of gram-positive organisms in a calcium-dependent process and disrupts the bacterial cell membrane potential causing ion leakage, interference with numerous cell processes, and cell death
polymyxins
-bind to LPS in the outer membrane of Gram negative bacteria
-then destroy bacterial membranes with a surface detergent-like mechanism by interacting with membrane phospholipids and increasing cellular permeability
-only active against Gram negative bacteria (do not have access to the bacterial cell membrane in Gram positives and polymyxin resistant Gram negatives)
-work like detergents for serious, resistant Gram negative infections
major modes of antimicrobial drugs
antibiotic spectrum
-broad spectrum: covers many potential pathogens (example: a carbapenem which has Gram positive, Gram negative, and anaerobic coverage)
-an antibiotic with a narrower spectrum has a more targeted spectrum of activity (example: clindamycin which only has Gram positive and anaerobic coverage- no Gram negative coverage)
how are antibiotics used?
-empiric therapy: often “broad spectrum”
-(definitive) therapy: if possible, initial empiric therapy should be changed to an antibiotic with a narrower spectrum of activity
-prophylactic or preventative therapy
culture and sensitivities
-identify the pathogen
-determine the sensitivity of the organism to various antibiotics (is it “sensitive”, “intermediate”, or “resistant”?)
-sensitivity determined by the interpretation of the minimum inhibitory concentration (MIC) which is the lowest concentration of antibiotic that prevents visible bacterial growth after 24 hours of incubation in the appropriate culture media
the MIC
-organism and drug specific
-”susceptible” implies that the concentration of antibiotic that can be achieved at the site of infection is >/= MIC
-numerous ways to determine the MIC: Kirby-Bauer disk diffusion, Broth dilution, E-test
mechanisms of resistance
when choosing and dosing an antibiotic, consider
-pharmacodynamics and pharmacokinetics
pharmacodynamic considerations when choosing and dosing an antibiotic
-what the drug does to the body/bacteria
-desirable effects: cidal v static, concentration v time-dependent killing, post antibiotic effect
-undesirable effects: toxicity, allergy, antibiotic-associated diarrhea or C. difficile colitis
pharmacokinetic considerations when choosing and dosing an antibiotic
-what the body does to the drug
-absorption (consider food/drug interactions)
-distribution (does it get where it needs to go in the right concentration?)
-metabolism (will it be metabolized properly, are there drug-drug interactions?)
-excretion: renal v nonrenal, half-life
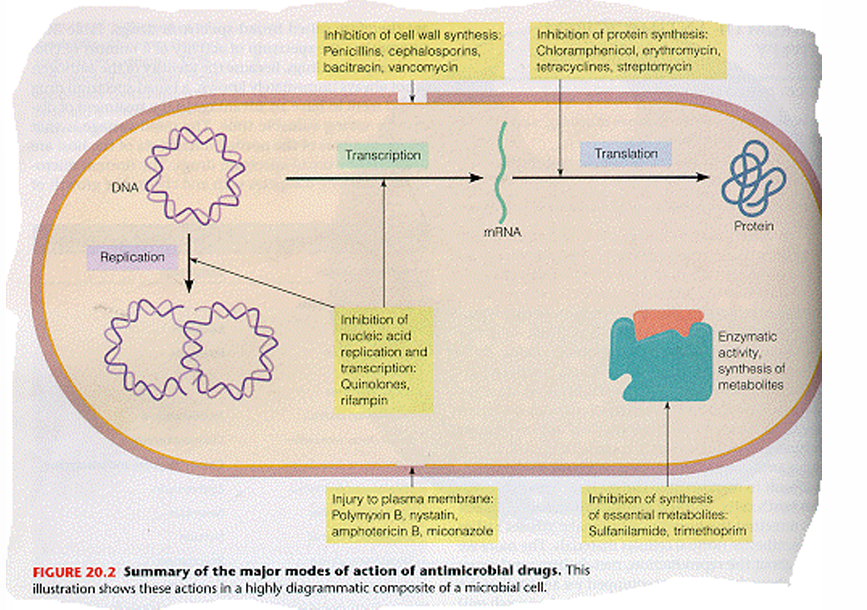
using antibiotics in combination
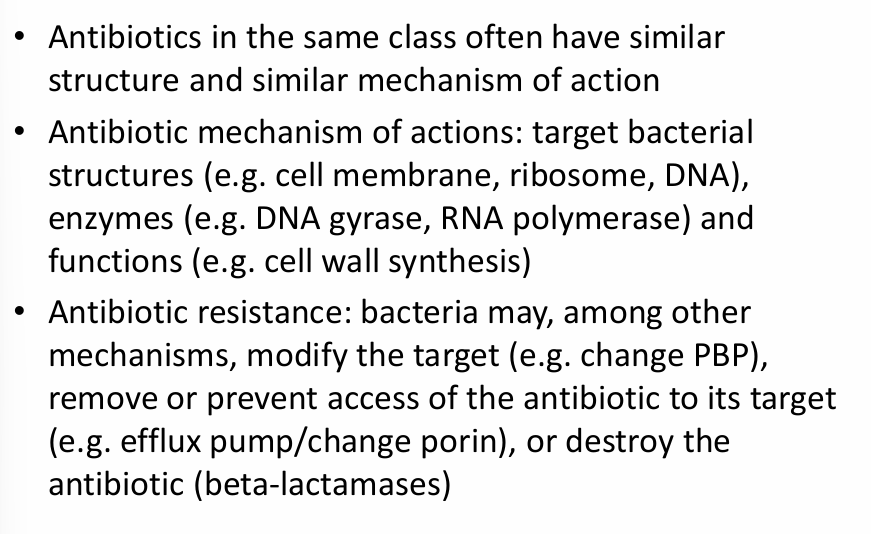
take home points