38. Diseases of the stifle joint- patella luxation and fractures. Screening program and therapy. Radiological examination and assessment of the DJD in stifle joint.
1/58
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
59 Terms
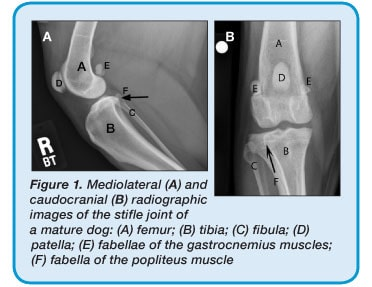
Femorotibial
Femoropatellar
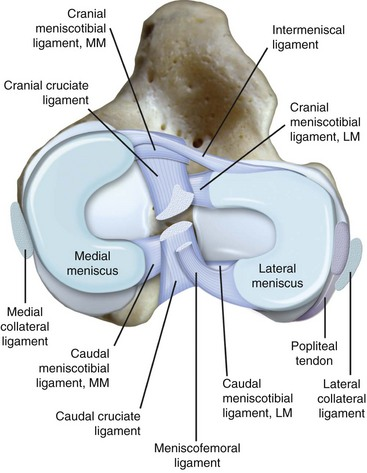
What are the components of the femorotibial joint?
Menisci
Meniscal ligaments
Femorotibial ligaments
Fabellae
Menisci lateralis et medialis. Cartilage structures between the femoral condyles and tibia
lig. meniscotibiale craniale/caudale
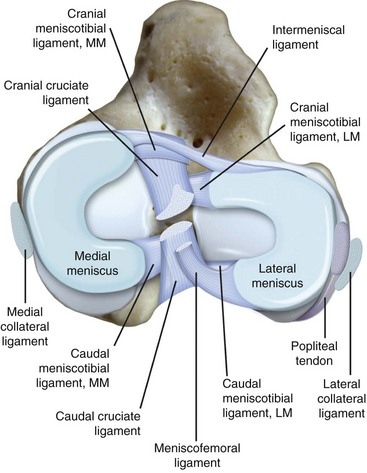
Which ligament attaches the meniscus to the femur, and which meniscus?
Lateral meniscus. lig. meniscofemorale
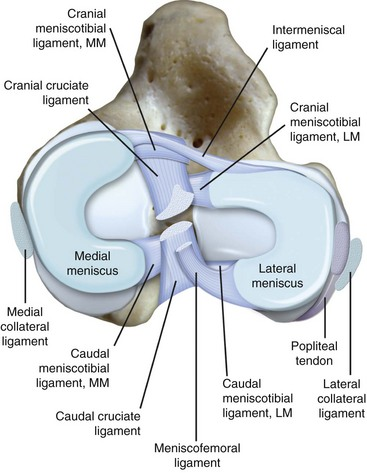
Which ligament attaches the anterior parts of the menisci?
lig. transversum genus
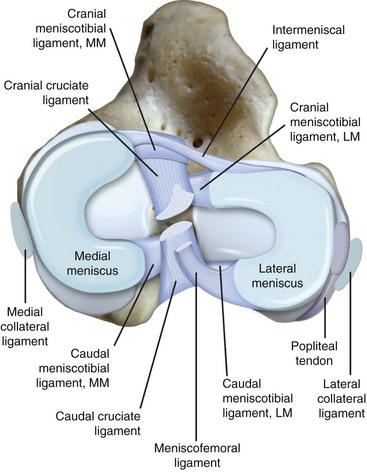
Which ligaments are part of the femorotibial joint?
ligs. collaterale laterale/mediale
ligs. cruciatum craniale/caudale
lig. popliteum obliquum
What are the components of the femoropatellar joint?
Patella
Ligaments
retinaculum patellae laterale/mediale (fibrous tissue on lateral/medial aspects of the patella; extension of m. vastus lateralis)
ligs. femoropatellare laterale/mediale
lig. patellae (apex patellae → tuberositas tibiae)
Quadriceps (m. vastus lateralis/medialis/intermedius + rectus femoris)
m. popliteus
More than 25% is fat (more radiolucent, but makes arthroscopy difficult)
Secondary intention healing → increased risk of degenerative joint disease
Bone remodels itself to become stronger with increased loading, weaker with decreased loading
(→ production of osteophytes → thickening of cortical bone & change of shape (ankyloses of bone))
What are examples of diseases of the stifle?
Patella luxation
Patellar fracture
DJD
Where is the physiological location of the patella?
Trochlear groove
Which species is more susceptible to patellar luxation?
Dogs
What are the aetiologies of patellar luxation?
Shallow trochlear groove
Varus deformity of femur
Valgus deformity of tibia
"Misplaced" quadriceps pull
Condyle damage
Femur bending
Damaged medial ridge → medial patellar luxation → inward tibial tuberosity rotation → weakened lateral tissues, contracted medial tissues
What are the clinical signs of patellar luxation?
Depend on severity: from asymptomatic to non-weight bearing lameness
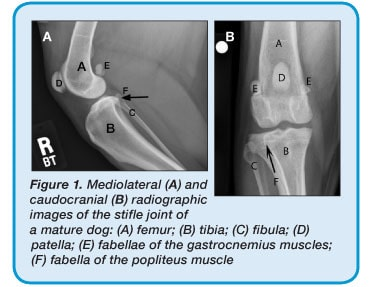
Grade 0: Physiological → no symptoms/normal - can move patellar but moves back to physiological position
Grade 1: Asymptomatic - patella in physiological position but skips spontaneously
Grade 2: Weight bearing lameness, skipping gait when walking - patellar permanently on side but can move back
Grade 3 + 4: Intense non-weight bearing lameness - patellar permanently on side and can’t move patellar back
How is patellar luxation diagnosed?
Physical exam (standing and lateral patient). X-ray/CT only used to assess the degree of changes
How is a physical exam for patella luxation performed?
Palpation of patella: find tuberositas + Patella ligament + Patella
W/ thumb & finger only slight movement to sides are normal. Palpate both in standing & lateral position: Palpate patella while moving leg in full range of motion. It is important to check the following structures for alignment & joint movement: Quadriceps femoris muscle, patella, patellar tendon, tibial tuberosity!!
0: normal
1: Located in groove, but can be luxated. Immediately returns to groove after displacement. Asymptomatic. No surgery needed. <15° tibial rotation
2: Luxate w/ flexion, returns w/ extension / Luxates when walking. Mildly bow-legged.
Intermittent non-weight bearing. Requires surgery. 15-30° tibial rotation
3: Permanently located medially, but able to push back to groove- will return immediately. Moderate bow-legged, flexed stifles. Frequently non-weight bearing. Requires surgery. 30-60° tibial rotation
4: Permanently luxated/medially, not possible to push back to groove. Severe bow-legged and flexed stifles. Requires surgery. 90° tibial rotation
Grade 1 w/ CS: conservative (NSAIDs & chondroprotectives). No treatment needed if no CS
Grade 2 depends on which side it leans to. If significant CS → surgery. If intermittent and non-progressive → conservative and re-evaluate
Grade 3 & 4 surgical correction
What are examples of surgical treatments for patella luxation?
Combination therapy:
Trochleoplasty: wedge or block resection to deepen the patellar groove
Trochlear wedge resection
Trochlear block resection
Tibial tuberosity transposition: Resect tuberosity & move it until patella lies in patellar groove & patellar tendon is aligned perfectly & straight
Medial release: release medial tissue to relieve tension
Lateral tightening: tighten lateral soft tissues (capsule and retinaculum)
Tibial anti-rotation: non-absorbable suture material used to suture around fabella & through tibial tuberosity to get centred patella
Trochlear chondroplasty: up to 6 months
What is trochleoplasty?
Deepening the trochlear groove
What are the methods of trochleoplasty?
Trochlear wedge resection
Trochlear block resection
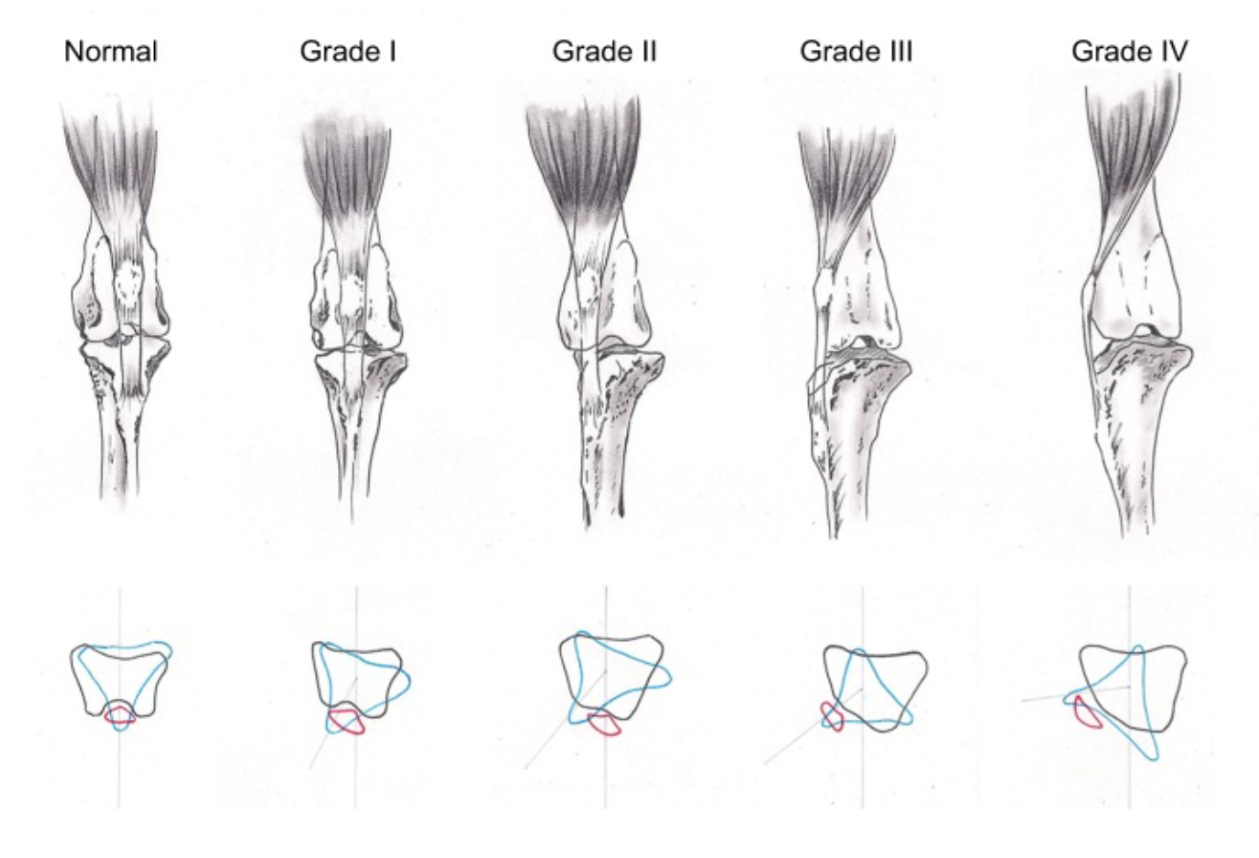
Direct or indirect trauma. Usually a complication of tibial plateau-levelling osteotomy (TPLO) surgeries
Non-weight bearing lameness, pain and swelling of cranial surface, possible void in quadriceps mechanism. Usually no crepitus.
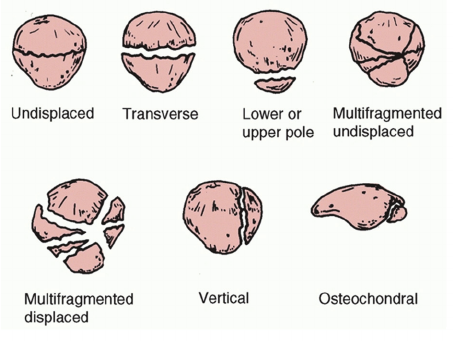
Radiographs (craniocaudal/caudocranial & mediolateral)
When is conservative treatment for patellar fractures indicated?
Cats with minimal displacement of fractured segments
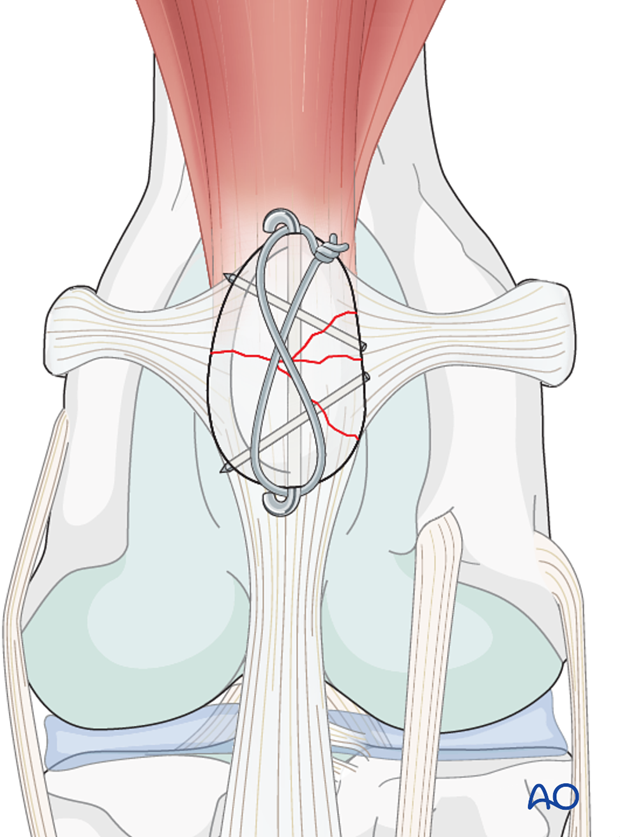
What are the surgical treatment options for patellar fractures?
Undisplaced fissure fracture: Wire through quadriceps tendon and patellar ligament. Wires tightened.
Transverse fracture: Kirschner wire and tension band wire, second wire in larger dogs.
Multi-fragmentary fracture: Kirschner wire and tension band wire
What are the grading systems for DJD?
Usually 0-3 or 1-4
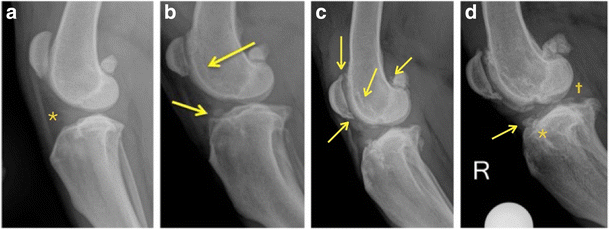
Initial: reduced density of the infrapatellar fat pad (asterisk);
Early: osteophytosis in the femoral ridge (left arrow) in the femur and tibia ligament insertion with osteophytosis in the femoral ridge (right arrow)
Osteophytes become apparent in the patella insertions, in the mid-zone portion of the femoral condyle’s trochlear ridge and in the femoral sesamoids (arrows);
Advanced: osteophytosis (arrow), enthesophytosis (asterisk), and calcification of the ligaments and meniscus (cross)
What often occurs prior to DJD?
Patella luxation or ruptured CCL
What are common signs of DJD in the stifle?
Osteophyte formation on patellar apex (& later patellar base is affected)
Fat pad sign – fat pushed out of joint capsule due to joint effusion
Periarticular osteophyte formation
Femoral subchondral sclerosis
Displacement of the fat pad due to joint effusion
Where do periarticular osteophytes form?
On femoral condyles, fabellae, proximal tibia, tibial plateau