septal defects
1/80
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
81 Terms
heart begins as a _____ that bulges and twists to form chambers
primal tube
_____ describes the outflow tract between the embryonic heart between the primitive ventricle and aorta
bulbus cordis
endocardial cushions form the
atrial septum
membranous ventricular septum
mv and tv
exams for suspected chd should include
dynamic 10-20 sec sweeps through the structures evaluated in each view
a sternal scar indicates
open heart surgery that required cardiopulmonary bypass
a lateral scar at the 4th/5th ribs indicates
shunt placement, coarctation repair, pda litigation
situs solitus
normal arrangment
situs inversus
mirror image of normal anatomy
situs ambiguous
arrangement of abdominal organs is varied w absence of spleen or multiple spleens
apex pointing to left
levocardia
apex pointing to the right
dextrocardia
apex pointing to midline
mesocardia
rt atrium is identified by
right artial appendade (auricle) - broad junction and lots of pectinate muscle, small triangular shaped pouch attached to the rt atrium and overlaps the aorta
rt ventricle is more
trabeculated
left atrium is identified by
left atrial appendage - finger shaped pouch, narrow junction of the appendage to the left of the atrial body, less pectinate muscle
left ventricles walls are
smooth and thicker than rt ventricle
categories of adult chd
abnormal intracardiac connections
abnormal chamber/cessel connections
congenital stenotic lesions
congenital regurgitant lesions
most commonly occuring congenital cardiac anomaly (most commonly seen in children)
vsd, but many close spontaneously
most common chd seen in adults
bicuspid av, mvp and asd
small vsds are less than _____ the diameter of the aortic annulus
1/3
small vsds are _____ to flow
restrictive
large vsds are greater than _____ the size of the aortic annulus
1/2
large vsds are _____ to flow
nonrestrictive (rv and lv pressures are relatively equal)
when shunting is present, what is calculated to assess changes in the cardiac output in the rt vs lt heart
Qp/Qs ratio
normal Qp/Qs values should be
approximately 1:1
the stroke volume in the left and right ventricles should be approximately
the same
a Qp/Qs ratio indicating a significant shunt is
2:1 or higher
pulmonary cardiac output (Qp), how is this measured
in psax at mid systole, measure rvot diameter @base of the pulmonary leaflets (inner inner) and calculate csa (0.785 x D²)
in the same location, obtain a pw doppler tracing of the rvot flow and trace for vti
pulmonic sv = csa x vti
pulmonic co = sv x hr
systemic cardiac output (Qs), how is this measured
in plax at mid systole, measured lvot diameter at the base of the aortic leaflets, calculate csa (0.785 x D²)
in apical 5 obtain pw tracing of lvot flow that includes closing click, trace for vti
systemic sv = csa x vti x 100
systemic co = sv x hr
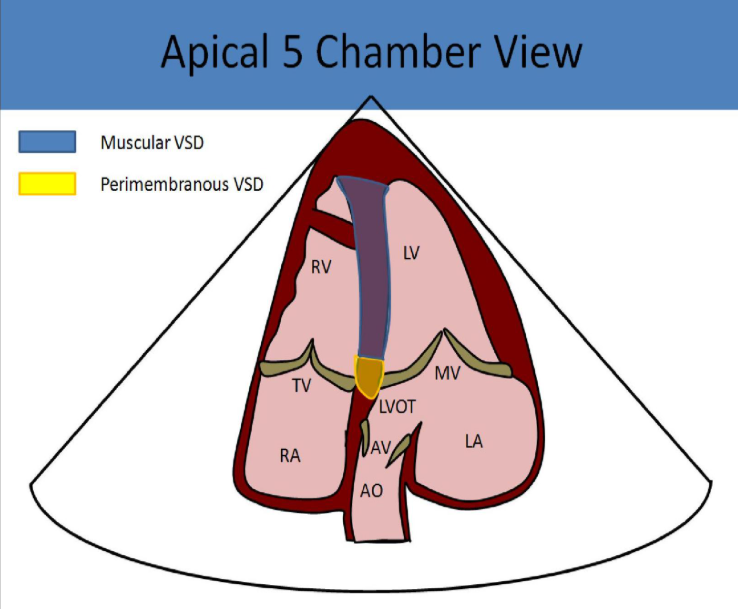
perimembranous vsd
best evaluated in plax
found in lvot near the aortic valve
in psax, seen at 10-12 oclock position
inferior to the rt coronary cusp of the aortic valve and adjacent to the septal leaflet of the tv
what is commonly seen w perimembranous vsd
ai
ventricular septal aneurysm
10% aortic valve prolapse
most common type of vsd
perimembranous vsd
muscular/trabecular vsd
located in the muscular portion of the ivs
best seen in the subcostal view
“T” artifact noted in apical 4 and 5 views
single or multiple causing “swiss cheese” appearance
second most common type of vsd
muscular/trabecular vsd
outlet/supracristal/subpulmonic/doubly committed vsd
located in the rvot near the pulmonic valve
best evaluated in high parasternal short and long axis views
seen at 12-2 oclock position in psax
inferior to the left coronary leaflet of the av and adjacent to the pulmonic valve
what is commonly seen w outlet vsd
rt aortic cusp prolapse (60-70%)
ai is common
inlet vsd
located in the posterior septum, near posterior leaflet of the tv
associated w avsd
best evaluated in the high parasternal short and long axis views
sonographic appearance of vsds
multiple views necessary to evaluate each type
left heart volume overload = dilated left ventricle w hyperkinesis + la dilated
rt ventricle usually normal but can suffer from pressure and volume overload w medium/large defects w pulmonary htn
rt atrium not usually affected
large vsds can lead to _____ syndrome, which is
eisenmenger, rt to left shuntiing
vsd appearance of color/doppler
shunt flow normally left to rt
subcostal and parasternal most useful in diagnosis
cw used to assess gradient
the higher the gradient, the _____ the defect
smaller
a Qp/Qs over _____ requires surgical intervention
1.5:1
what can be deployed via catheter to close a vsd
occlusive device
what is required for vsds that cannot be occluded w a device
open heart surgery
what is used in open heart surgery to cover a vsd
patch, stitches, piece of pericardium
post op evaluation of vsd
evaluate for residual shunt flow around the patch or device
assess changes to lv size/function and la size
evaluate systolic pulmonary artery pressure to evaluate pa pressure to assess success
how is rvsp calculatde w vsd
calculate pressure gradient across vsd w bernoulli
systolic bp - vsd gradient = rvsp
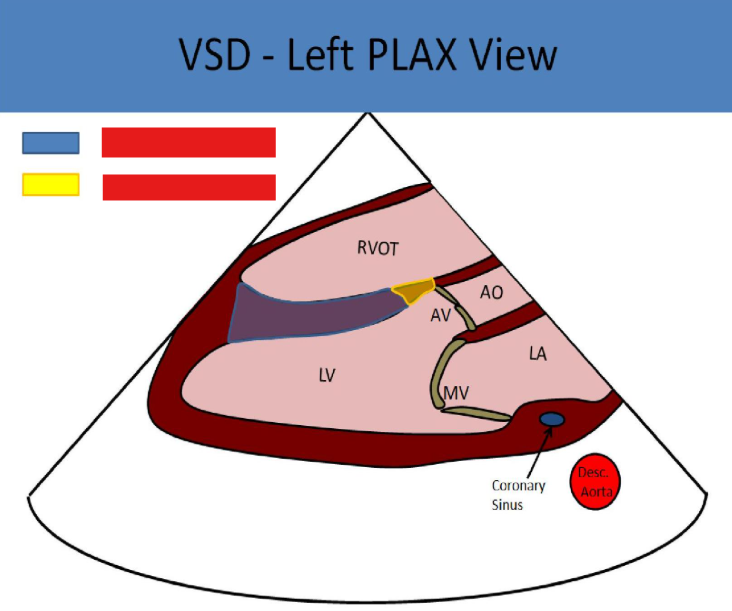
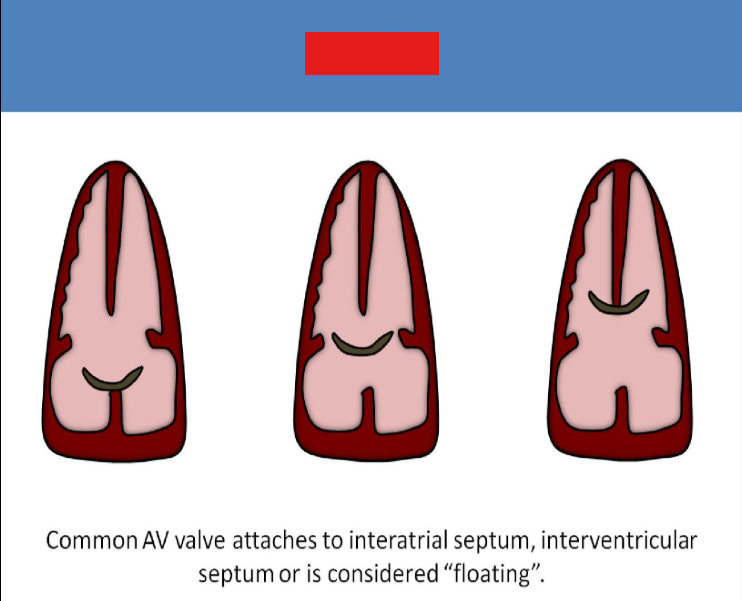
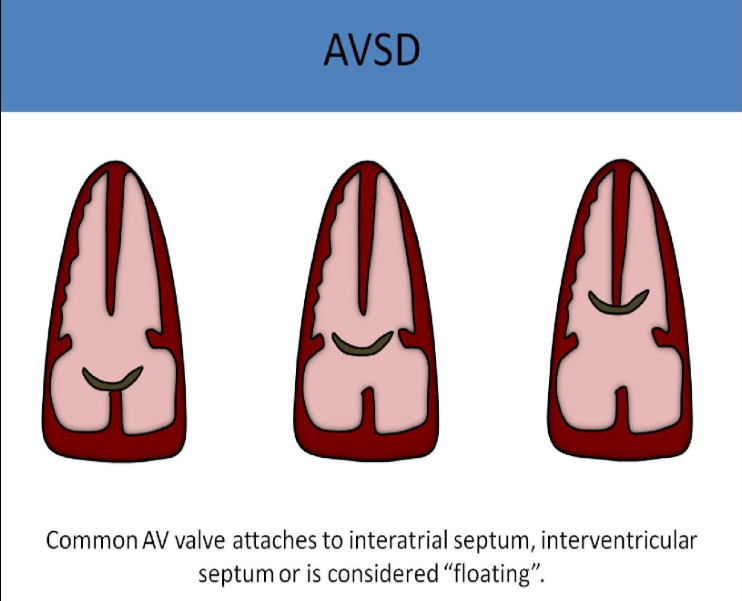
what vsds are pictured
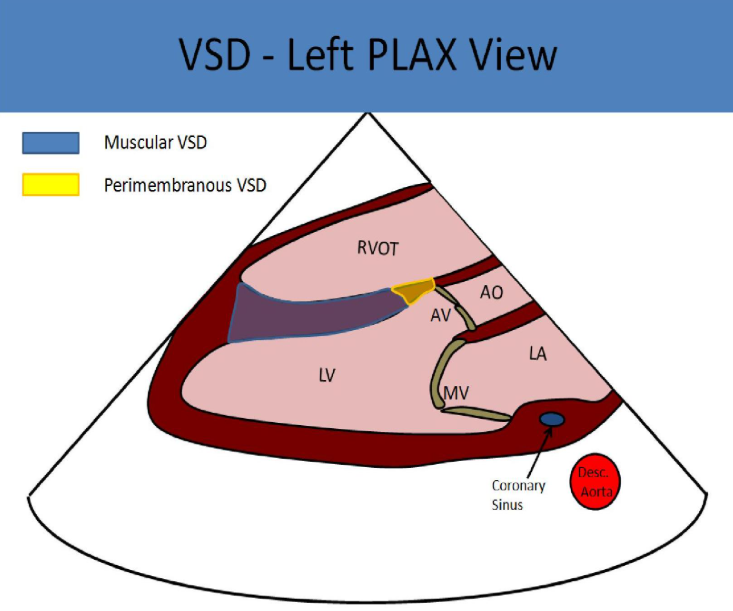
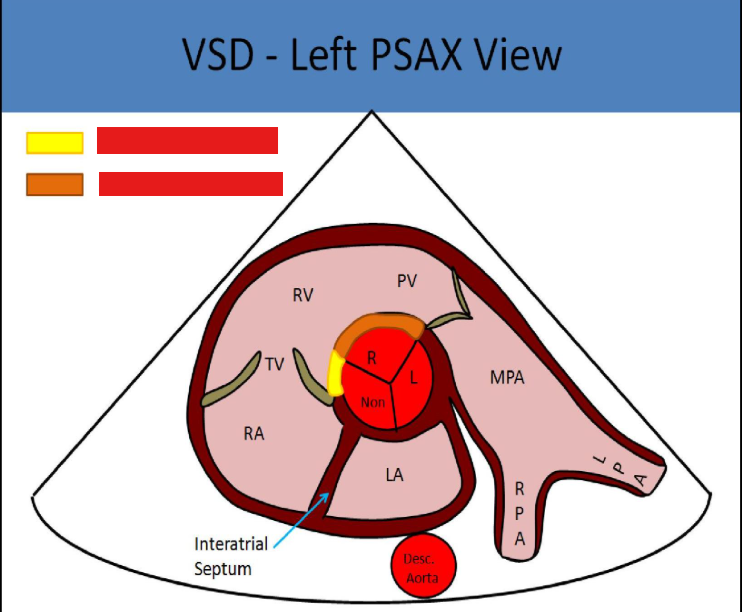
what vsds are pictured
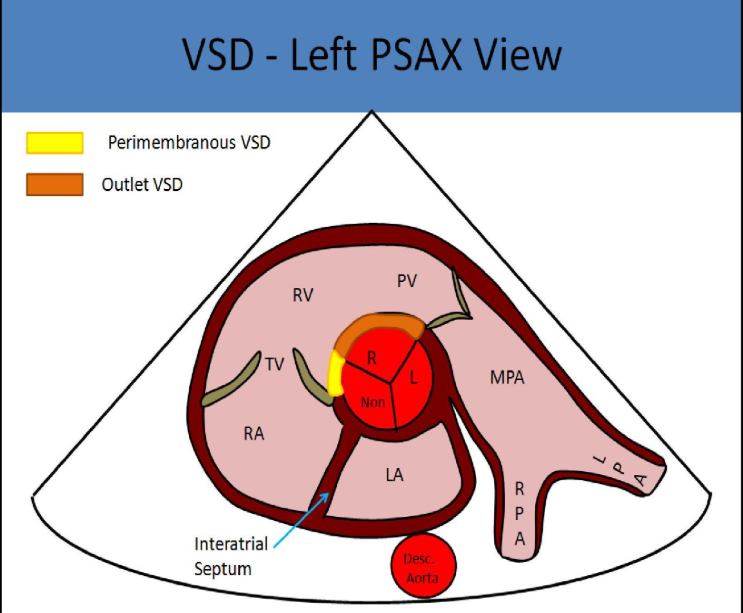
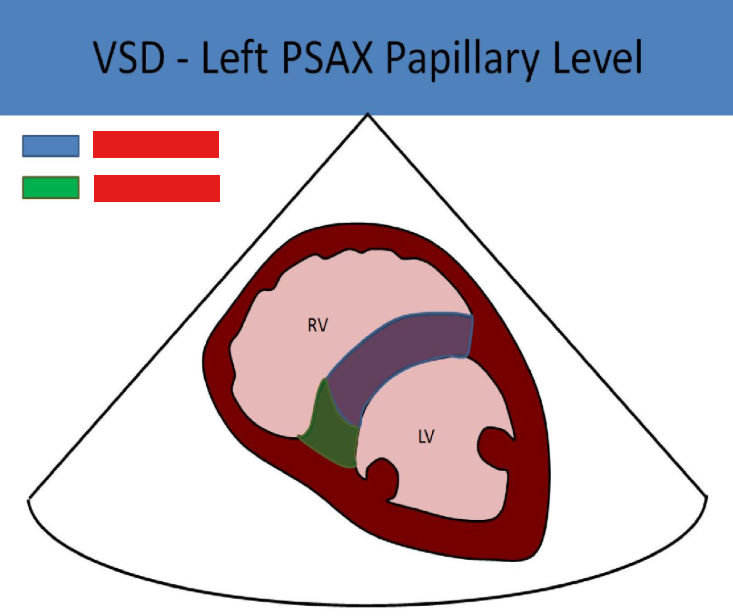
what vsds are pictured
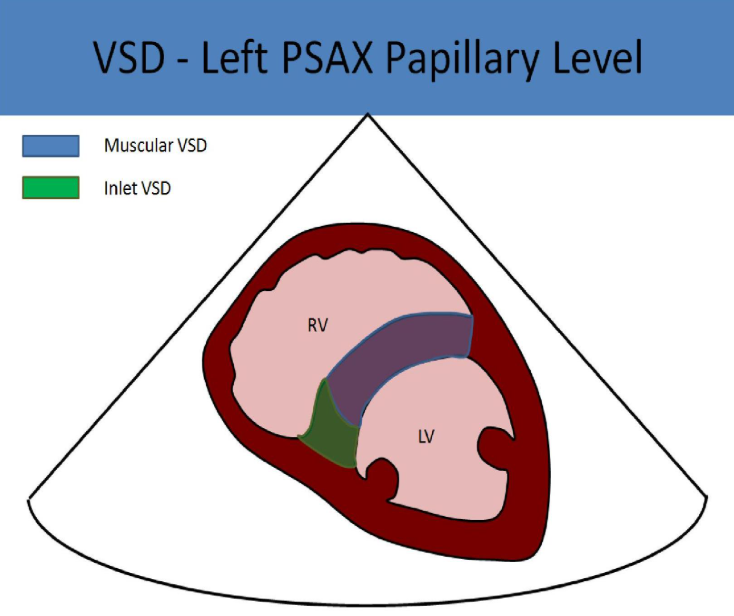
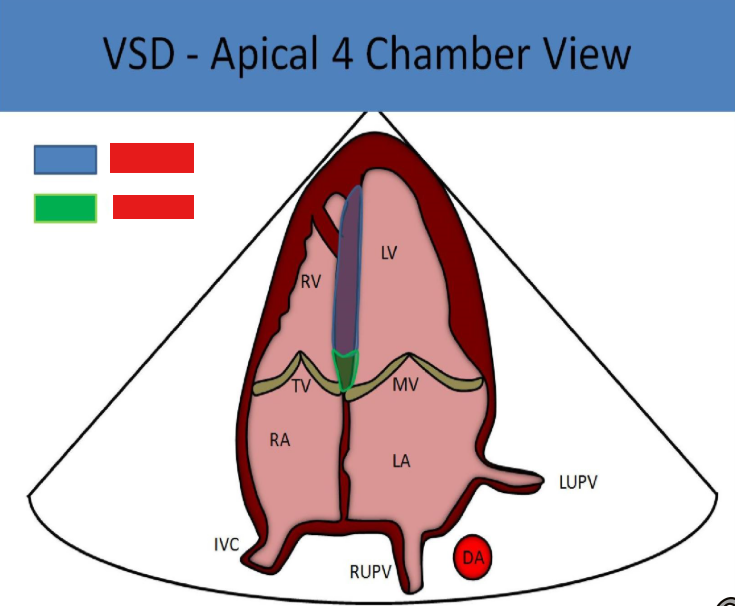
what vsds are pictured
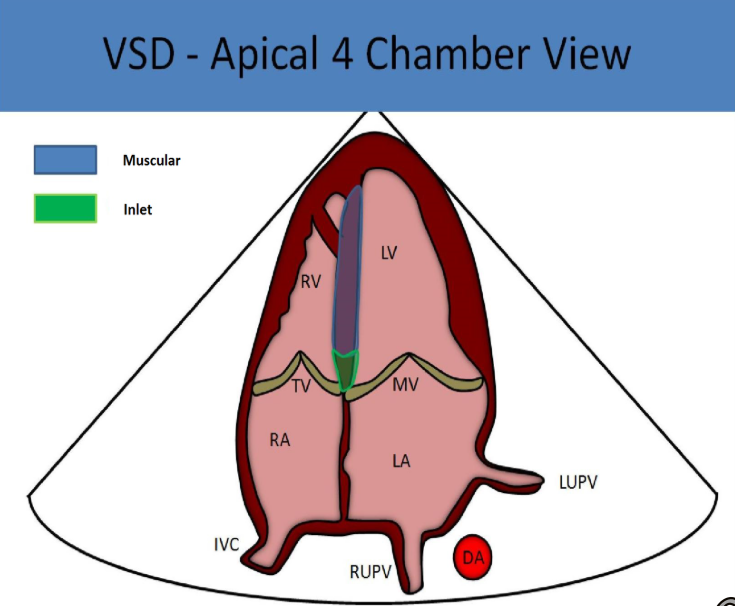
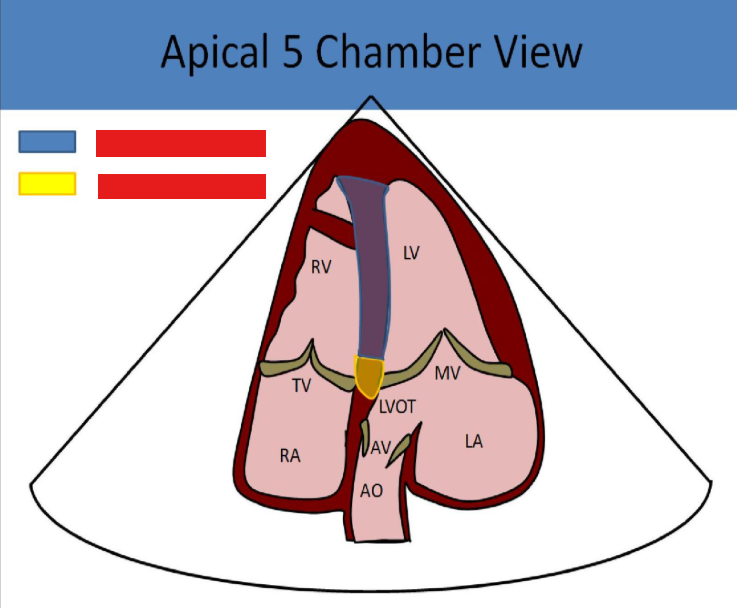
what vsds are pictured
patent foramen ovale
failure of the foramen ovale to close
25% patent in adults
what causes the foramen ovale to close in normal pts as babies
when a baby is born, the pressures drop in the rt heart, and the higher pressure in the left atrium holds the flap of tissue closed over the opening, causing it to fuse and close
how can a pfo be diagnosed
microbubbles injected into the venous system, if they appear in the left atrium within 3 cycles an asd is present
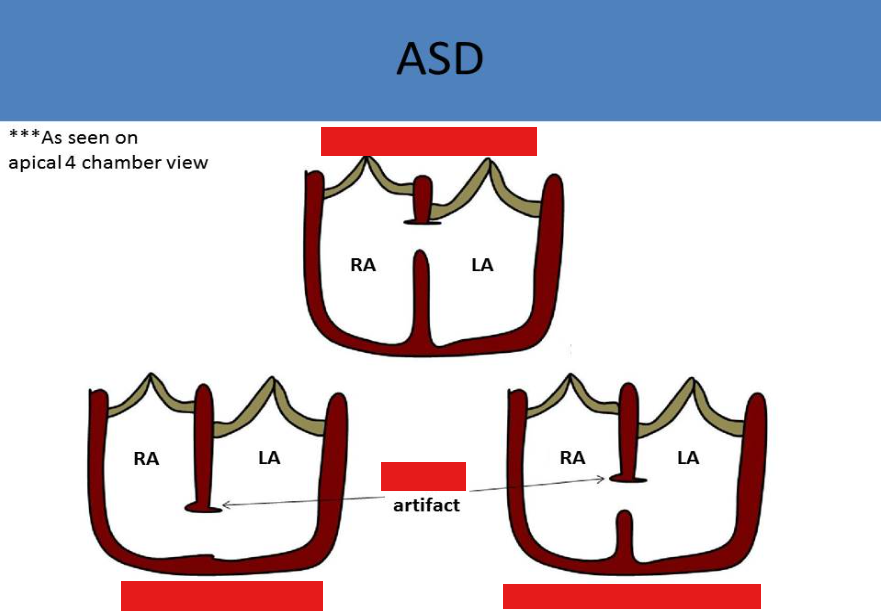
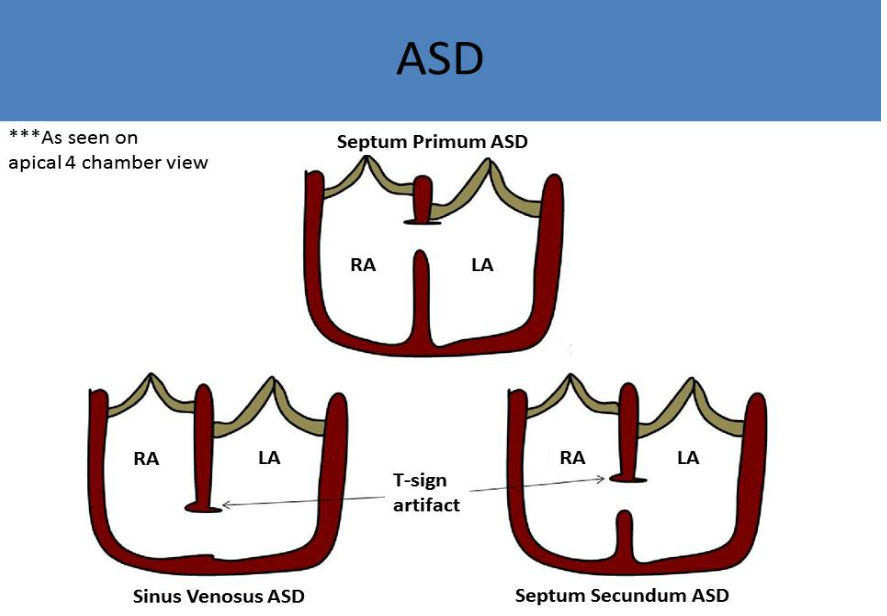
atrial septal defect (asd)
can be associated w interatrial septal aneurysms
defect in the septum primum layer (can be acquired due to differences in interatrial pressure)
associated w systemic thromboembolism
most common asd
septum secundum
septum secundum asd
mid septal area, associated w mvp
second most common asd
septum primum
septum primum asd
close to mv/tv, associated w cleft mitral valve
sinus venosus asd
near svc entrance, associated w partial anomalous pulmonary venous return
coronary sinus defects
inferior portion of the septum, associated w persistent lsvc
common atrium
absence of septum, associated w ellis van creveld syndrome
signs and symptoms of asd
murmur = systolic w a fixed split s2
usually asymptomatic until mid to late adulthood
dyspnea on exertion
orthopnea
jugular vein distension
peripheral edema
what views are optimal for color and doppler eval of the atrial septum
subcostal
normal asd shunt flow
left to right w small amount of flow reversal at early systole
if the pressures in both atria are normal w asd, what will the average peak velocity across the defect be
about 1 m/s = approximately a 5 mmHg peak pressure gradient vc the normal difference in pressure between the right and left atrium is 5 mmHg
how will large asds appearance sonographically
will demonstrate low velocity uni or bidirectional flow, indicating increased rt atrial pressures equivalent to left atrial pressures, causing rt heart dilation from volume overload
how does rt heart dilation from volume overload appear on us (from ivs)
ivs flattening in diastole w increased rt heart pressures and a d shaped left ventricle
treatment of asd (secundum)
percutaneous transcatheter device closure
percutaneous transcatheter device closure
a device called an amplatzer can be used to close a secundum asd
implanted using a balloon cath
tee or intracardiac us is used to guide the procedure
what is necessary for treatment of septum primum and sinus venosus defects and why
surgical intervention, as percutaneous transcatheter device closure is not possible w those defects due to adjacent anatomy/how the device works
how will an amplatzer device look on us
echogenic disk on either side of the septum. no flow should be detected across the septum
endocardial cushion defect
atrioventricular septal defect (avsd) or av canal defect
incomplete development of the endocardial cushions
symptoms of endocardial cushion defect
holosystolic murmur
dyspnea
cyanosis
fatigue
what is endocardial cushion defect associated with
down syndrome
partial endocardial cushion defect
septum primum asd
cleft mitral valve
complete endocardial cushion defect
septum primum asd
inlet vsd
common atrioventricular valve w 5 leaflets
sonographic appearance of avsd
apical views demonstrate the av valves, primum asd and inlet vsd
common av valve appears as a single linear structure between the ventricles and atria (lack of normal offset of tv toward apex)
subcostal views are best for color/doppler eval
leads to rt ht volume overload, dilated rt ventricle w paradoxical ventricular septal motion