Calcium Discussion
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
42 Terms
PTH is synthesized in what cells of the parathyroid gland and in response to what 3 things
1) synthesized in chief cells of PT gland
2) in respond to low Ca2+, low 1,25-(OH)2 vit D, or high PO4
Ca2+ binds to what receptors on the PT chief cells, resulting in a signal that ____________ PTH secretion
binds to the CaSR (calcium sensing receptor), resulting in a decrease of PTH secretion
PTH indirectly stimulates activity of which cell within the bone matrix to do what
osteoclasts to release Ca2+ in the blood
PTH reduces ___________ reabsorption from the PCT of the kidney
(PO4)3- (phosphate)
PTH activates what enzyme to convert VitD to its active form in the kidney, thus aiding what in the gut
1-alpha-hydroxylase; aids Ca2+ absorption in the gut
use this case for the following questions
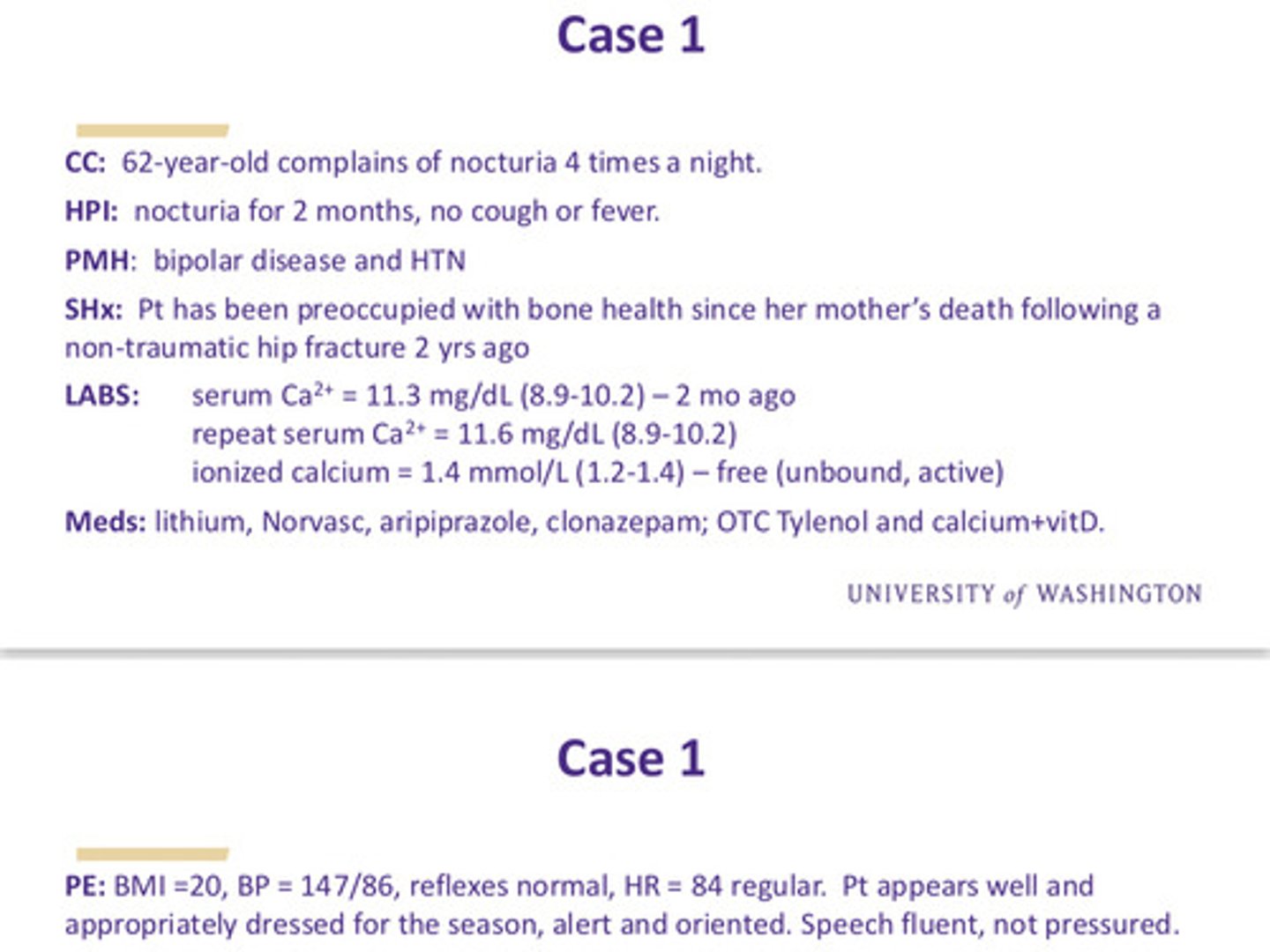
case 1: what is the next lab test needed to help generate a DDx for the cause of her hypercalcemia
serum PTH: the initial evaluation of a pt with hypercalcemia is to determine whether this is a PTH-mediated phenomenon
case 1: repeat calcium is 11.5 mg/dl (normal is 8.9-10.2) and serum PTH is 123 pg/ml (normal is 10-55). what is the dx for her hypercalcemia?
we see high calcium and high PTH so this is a problem with the parathyroid gland itself —> primary hyperparathyroidism
primary hyperparathyroidism is the ______ __________ cause of outpatient hypercalcemia; why do we rule out secondary hyperparathyroidism for the case 1 pt
most common! in the setting of hypercalcemia, serum PTH should be LOW; normal or elevated serum PTH suggests primary
what is the differential diagnosis for elevated PTH (independent of calcium)
1) primary hyperparathyroidism (non-suppressed PTH)
2) secondary hyperparathyroidism
case 1: how do we determine what the causes of these diseases states are?
first must determine where the problem lies - is it at the PT gland or with Ca2+ handling
what are some DDx of elevated Ca2+ in background of normal/high PTH (primary hyperparathyroidism) (6)
1) parathyroid gland adenoma (benign, most common cause)
2) parathyroid gland malignancy (1-2% of all hyperPTH cases)
3) familial hypocalciuric hypercalcemia (CaSR mutation)
4) medication induced hypercalcemia (thiazide diuretics, lithium)
5) irradiation to the head and neck (rare)
6) MEN syndromes (rare)
what are some DDx of decreased Ca2+ in background of normal/high PTH (secondary hyperparathyroidism) (3)
1) chronic renal dz (most common, Ca2+ is dumped in urine)
2) vitD deficiency
3) malabsorption syndromes like chronic pancreatitis, bariatric surgery, small bowel dz (ie cannot take up ingested Ca2+)
case 1: what if pt's repeat calcium is now 11.5 mg/dl (8.9-10.2) with a serum PTH of 9 pg/mL (10-55)? what would be the Dx for her hypercalcemia now? (4)
DDx of elevated Ca2+ in background of low PTH: non-PTH mediated hypercalcemia
1) hypervitaminosis D or ingested calcium toxicity (milk-alkali syndrome from too many calcium containing antacids)
2) tuberculosis (peripheral 1-alpha-hydroxylase activation)
3) multiple myeloma or other cancer (bone metastases and production of PTHrP)
4) sarcoidosis (peripheral 1-alpha-hydroxylase activation)
in the face of hypercalcemia, if PTH levels are normal/high, what is the likely cause?
primary hyperparathyroidism:
1) parathyroid adenoma/hyperplasia
2) meds: thiazides, lithium
3) inactivating CaSR mutation
4) MEN syndromes
5) parathyroid malignancy
in the face of hypercalcemia, if PTH levels are low, what is the likely cause?
non-PTH mediated hyperparathyroidism:
1) hyperVitD or Ca intake
2) small cell lung CA
3) TB
4) MM or other cancer
5) sarcoidosis
if we had to generally define 3 causes of non-PTH mediated hypercalcemia, what would they be
1) increased bone resorption
2) impaired renal excretion
3) increased gut absorption
case 1: what additional lab tests are needed to confirm a Dx of non-PTH mediated hypercalcemia (aim is to identify possible sources of Ca2+ excess)
among the many additional lab tests, the most important ones are urinary calcium tests and urinary pH tests

case 1: how do you interpret the additional lab tests
according to urinary calcium and urinary pH, the gut is absorbing the excessive calcium supplements being ingested. this creates hypercalcemia which leads to polyuria and alkalosis (calcium salts are alkalotic)
use this case for the following questions
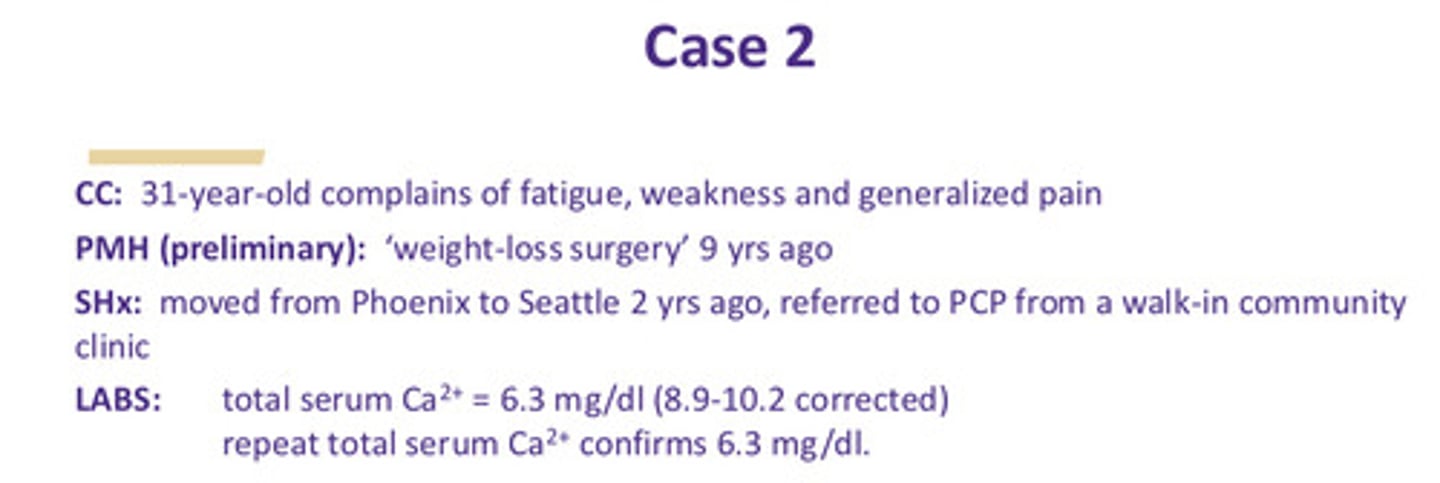
case 2: what is the best test to order next for further evaluation?
serum albumin! (total serum calcium measures both albumin-bound and unbound free calcium; since most calcium is bound, one must correct the serum Ca2+ if serum albumin is low)
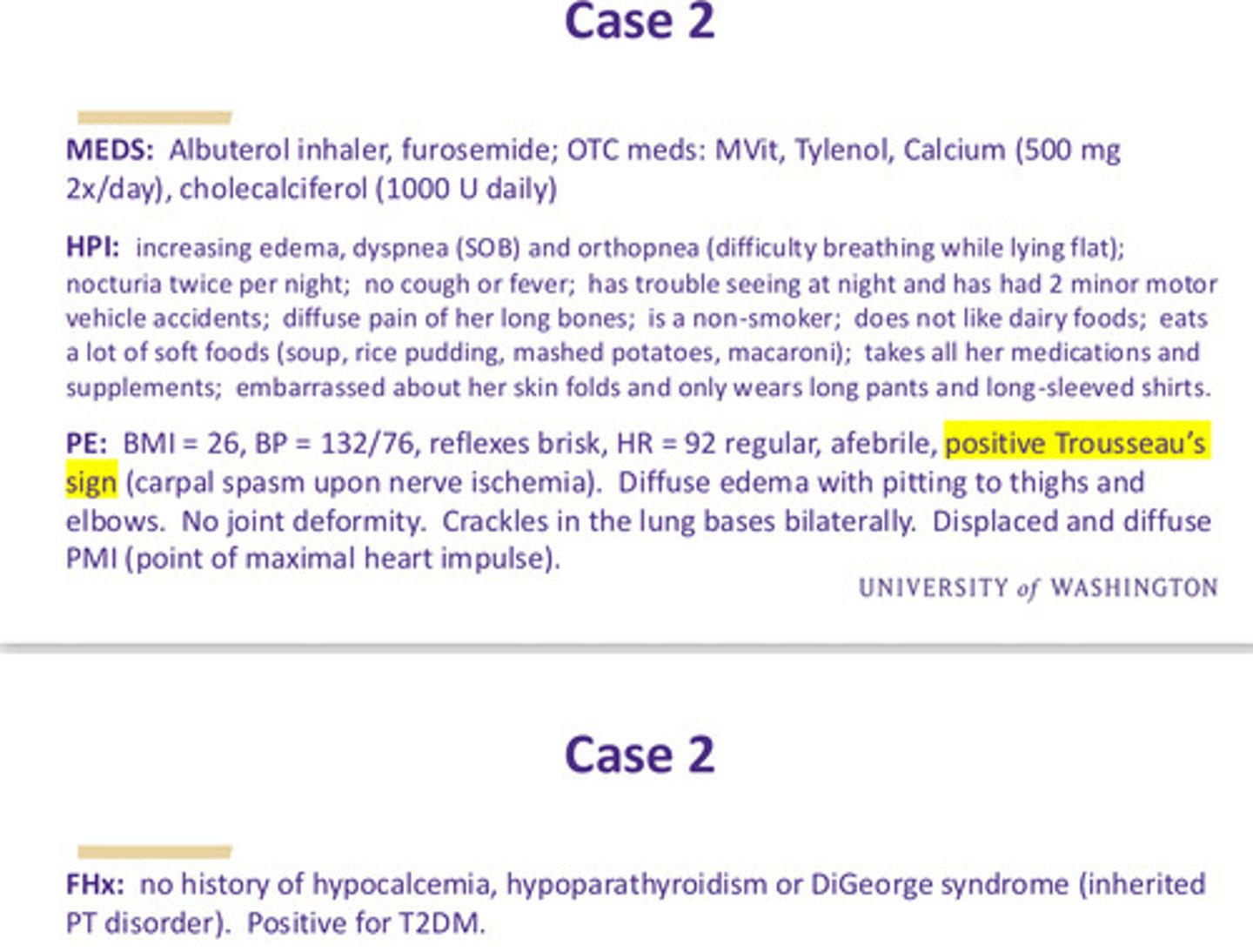
case 2: results of serum albumin test + past medical hx
even after correcting serum Ca2+, it is still low
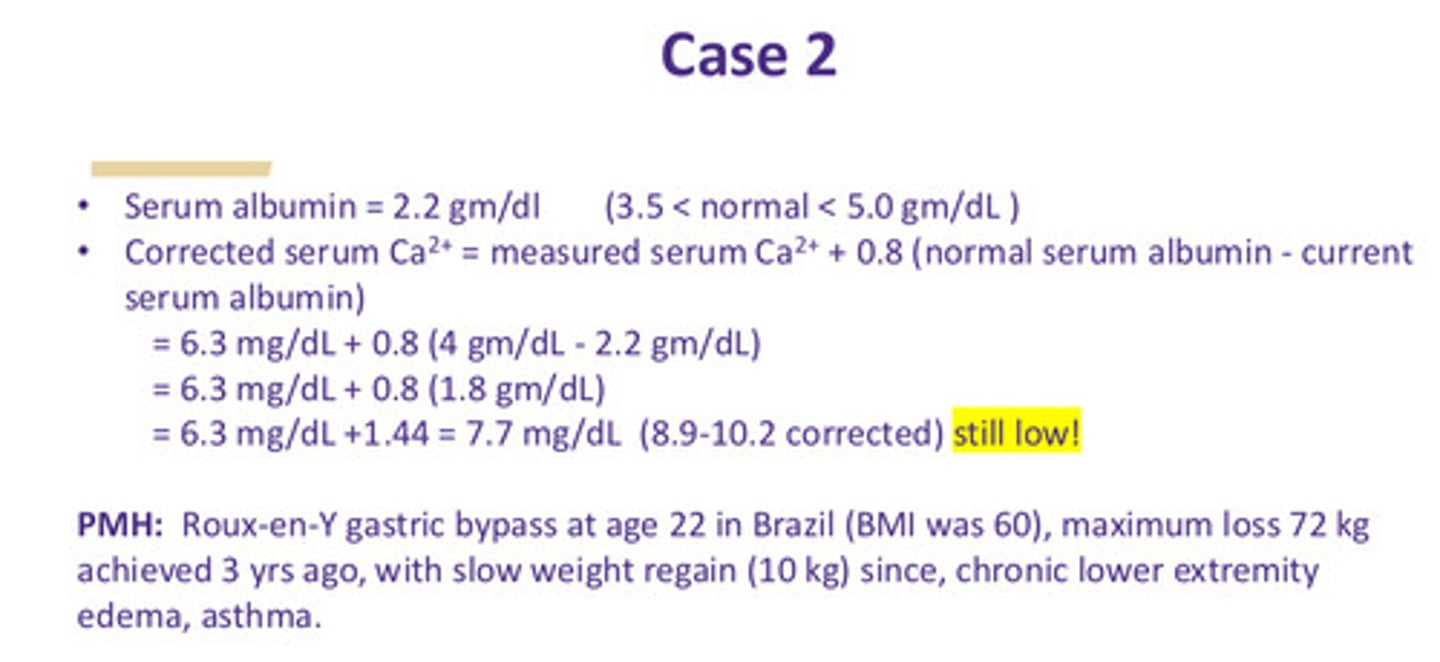
case 2: more meds, HPI, PE, FHx
note that in PE we see a positive trousseau's sign (carpal spasm upon nerve ischemia)
case 2: based on the pt's hx, what can we put in a general DDx for her hypocalcemia (7)
1) hypoparathyroidism (autoimmune)
2) severe vitD deficiency
3) malabsorption
4) renal calcium loss (kidney failure)
5) severe magnesium deficiency (can cause hypoPTH)
6) calcium sequestration from necrotic pancreatitis
7) anabolic bone dz from skeletal metastates
in the face of hypocalcemia, if we see low PTH levels, what can we assume is the cause?
primary hypoparathyroidism:
1) congenital (ex DiGeorge)
2) post surgical (neck)
3) autoimmune
4) infiltrative dz
in the face of hypocalcemia, if we see high PTH levels, what can we assume is the cause?
secondary hyperparathyroidism:
1) decreased bone remodeling
2) renal disease (Ca loss)
3) vit D/Ca deficiency
4) malabsorption
5) meds: glucocorticoids
case 2: what additional lab tests would help clarify the Dx?
the most important additional tests would be vit D levels, PTH levels, and micronutrient panel: in this pt, Vit D and micronutrient levels are all low but PTH levels are high
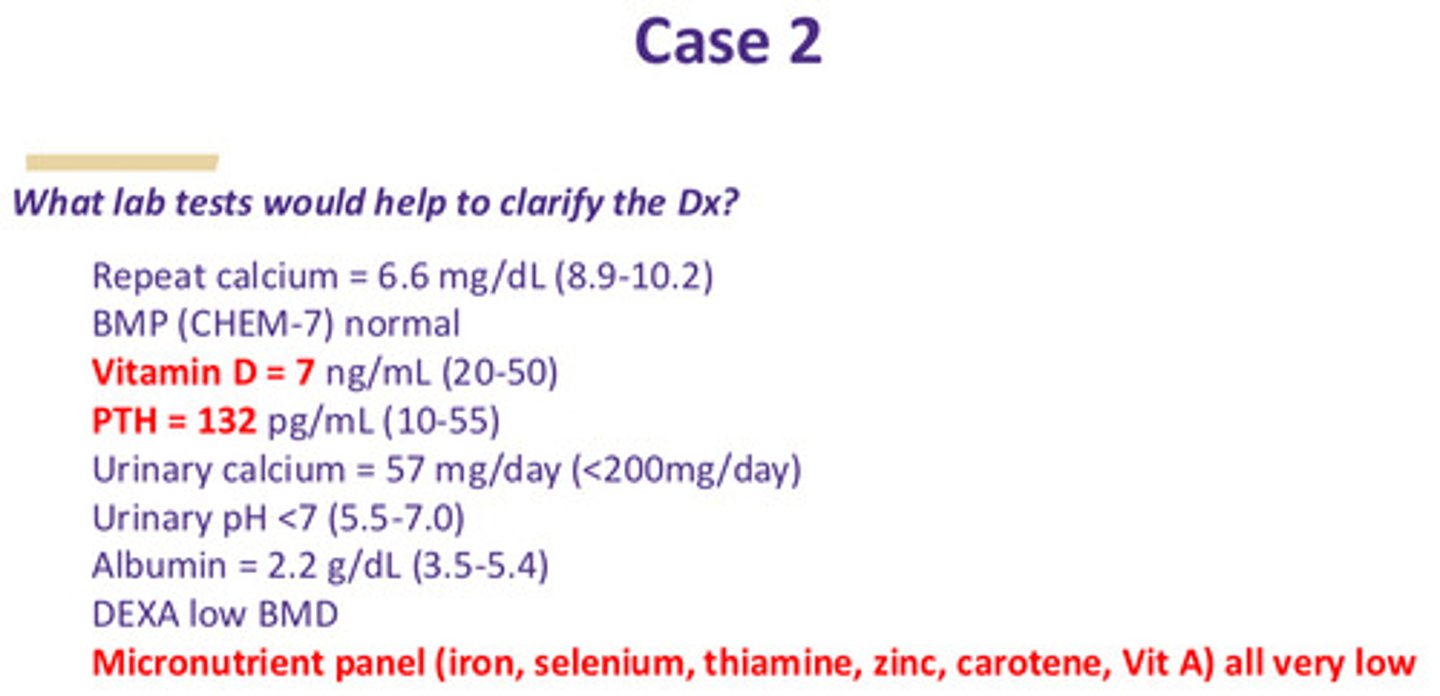
case 2: what is the most likely diagnosis for this pt if we have hypocalcemia but hyperparathyroidism
secondary hyperparathyroidism due to hypocalcemia from severe vit D deficiency and malabsorption related to prior bariatric surgery (labs are c/w this diagnosis), plus her poor dietary habits
case 2: if a different pt presented with a confirmed and corrected serum Ca2+ of 6.2 (8.9-10.2) and a serum PTH of 5 (10-55), what would the DDx be?
hypocalcemia and low PTH would be representative of primary hypoparathyroidism, which is most often iatrogenic due to inadvertent injury or resection following neck surgery (thyroid or parathyroid)
case 2: what is the recommended tx for the original case pt
Ca2+ and activated vit D supplementation + PTH replacement
what are the risks of hypocalcemia
calcium is imperative for certain muscular function; therefore risks include:
1) life threatening muscle spasms (including laryngeal)
2) seizures
3) arrhythmias
4) cardiac arrest
5) non life threatening: paresthesia, petechiae
use this case for the following questions
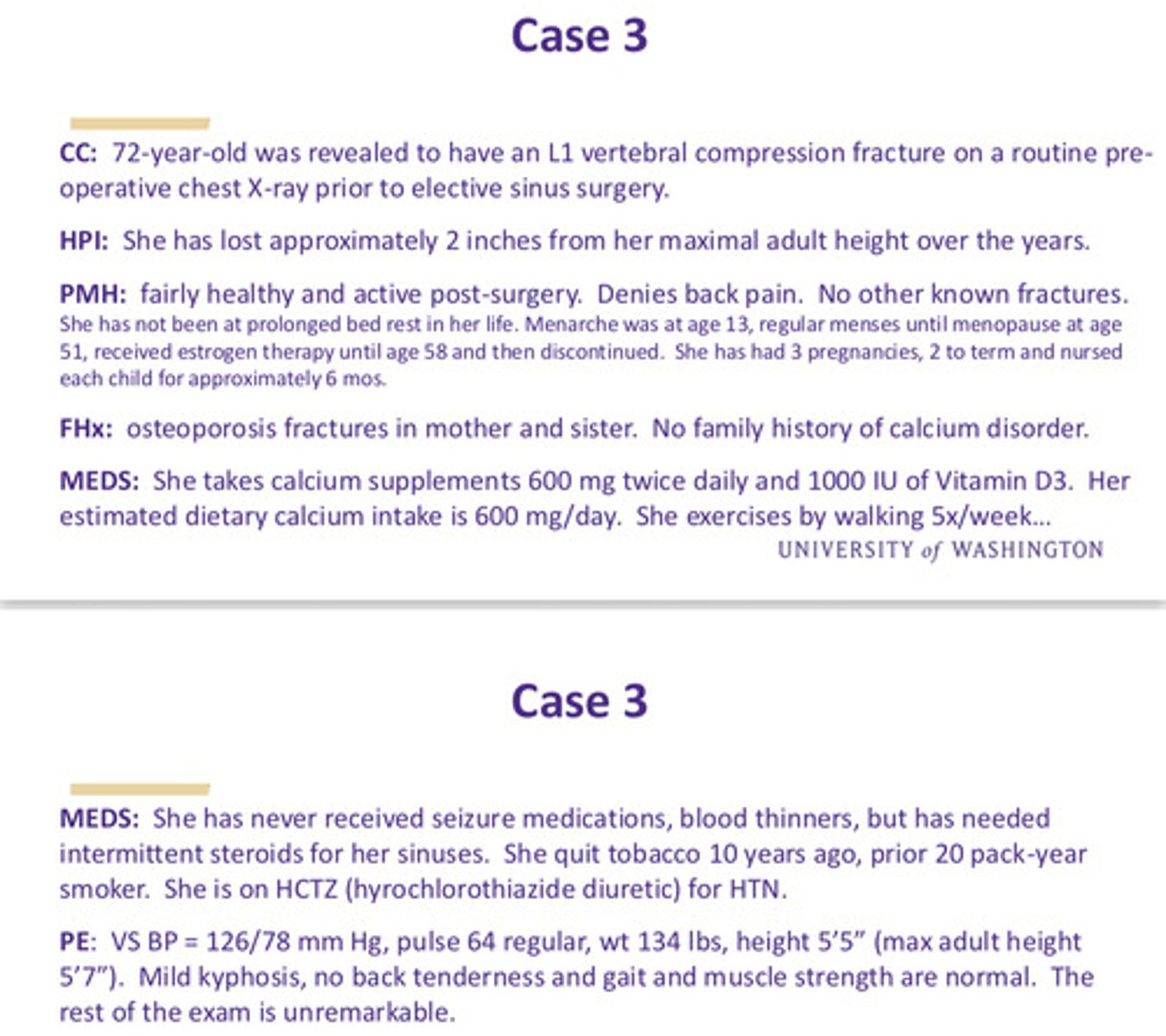
case 3: list some possible reasons why this pt might have skeletal fragility
1) age
2) post menopausal status
3) glucocorticoid exposure
4) tobacco history
5) strong family history
case 3: which labs or radiologic studies would help in evaluating this pt's skeletal fragility?
1) renal and liver assessment, serum calcium, 25-OH-Vit D, TSH, 24-hour urine Ca2+ —> indirect assessment of calcium absorption and also direct assessment of renal calcium handling
2) bone biomarkers: alkaline phosphatase or osteocalcin (bone formation marker) or serum or urine N-telopeptides (bone resorption markers)
3) xray of spine and a bone mineral density assessment by DEXA (T-score, Z-score BMD)
4) vertebral compression (incident) fractures are the most common osteoporotic fracture and 2/3 of them are asymptomatic so spine films should be a part of the eval of any pt suspected of having osteoporosis
case 3: new labs
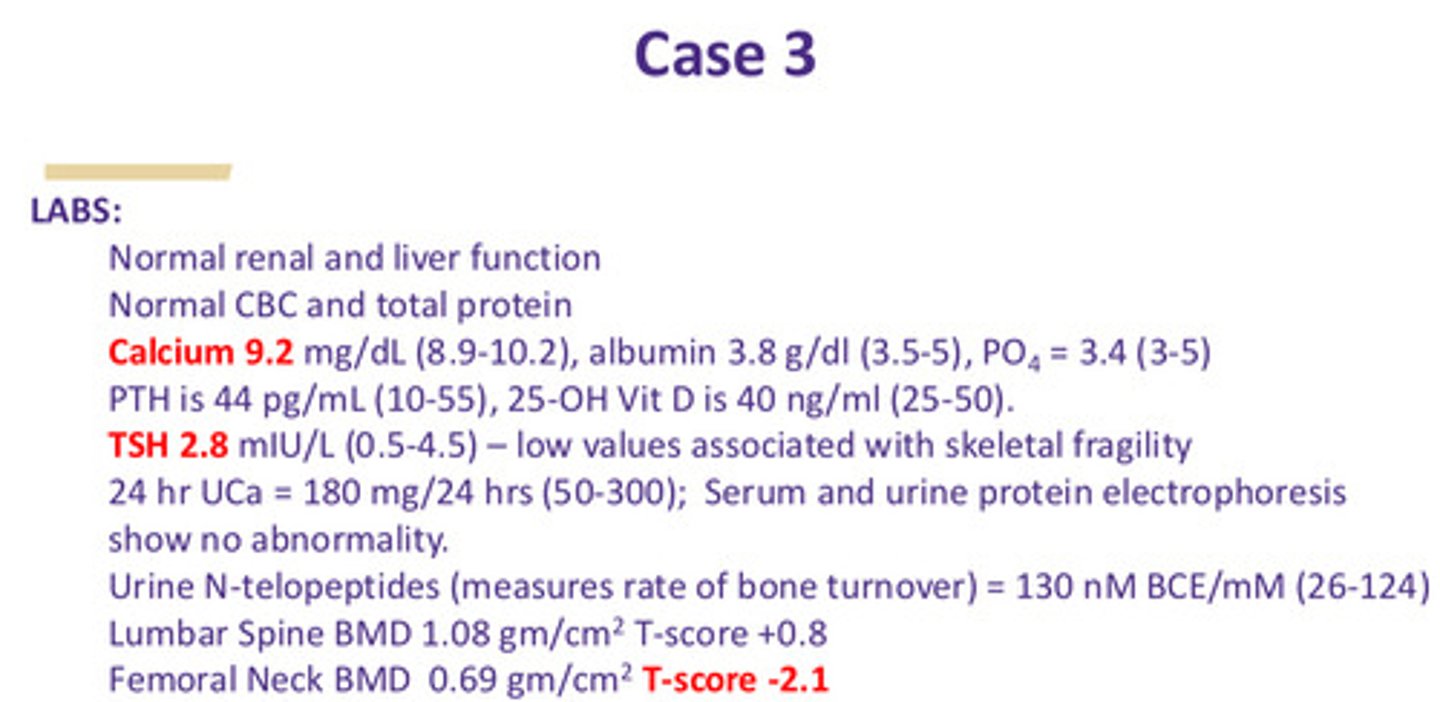
case 3: what is the best tx for this pt
this case represents a "perfect" candidate for bisphosphonate tx: a post-menopausal female w an incident fracture
what is MOA of bisphosphonates
suppress osteoclast activity, thus slowing bone loss
what are adverse effects of bisphosphonates
1) GI (reflux, esophagitis, ulcers)
2) osteonecrosis of the jaw, only after IV bisphosphonates (co-morbidities: CA tx, GCs, DM, periodontal dz, smoking)
3) atrial fibrillation
4) atypical femur fractures
what is RANKL's role in bone remodeling
RANKL is found on osteoblast surface; it is a ligand to osteoclast membrane receptor RANKL controlling osteoclast proliferation
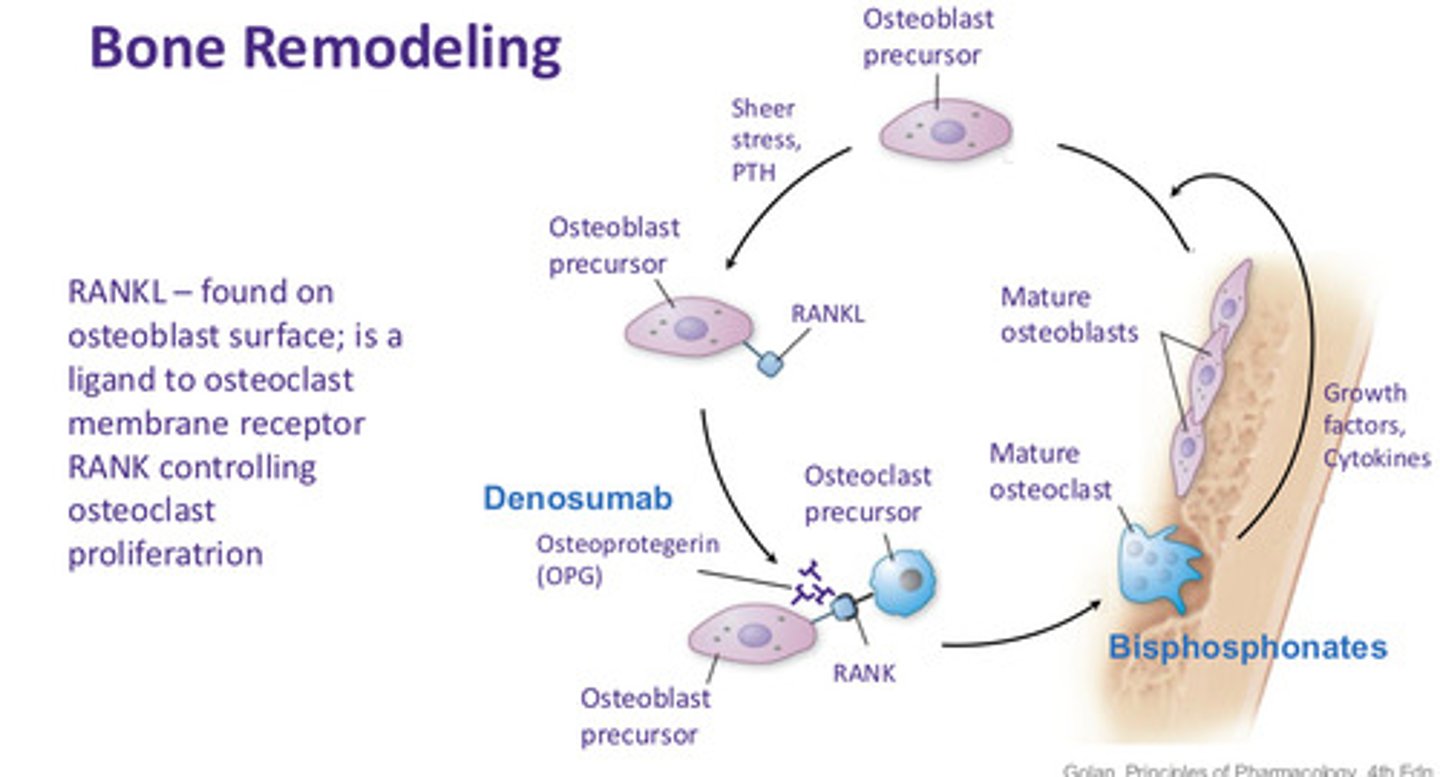
describe the pharmacology of bone remodeling: bisphosphonates (4)
1) most widely used anti resorptive drugs
2) incorporated into the bones (become part of the bone matrix) and taken up by osteoclasts, leading to osteoclast apoptosis
3) bones become stronger but less elastic (more brittle)
4) only IV (q12 mo) BPs are implicated in ONJ: zoledronic acid (aredia)
describe the pharmacology of bone remodeling: RANKL inhibitors (4)
1) inhibit osteoclast formation, activity, and survival
2) not deposited in bone, not cleared by kidney (can be used in CKD)
3) no MRONJ risk if drug is discontinued prior to dental work, but osteoporosis risk returns
4) SC injections q6 mo: denosumab (prolia)
what are the 6 effects of glucocorticoid exposure on calcium metabolism
1) causes osteoblast apoptosis
2) decreases calcium gut absorption
3) causes central hypogonadism
4) causes GH suppression
5) reduces vit D conversion to active metabolite
6) promotes calciuresis