CO2026 fungal and protozoa
1/126
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
127 Terms
___________ is a widespread protozoan diarrheal disease and most common chronic diarrhea in travelers
Giardiasis
What is parasitism? What do they do to the host?
parasites benefit while the host is harmed; deprive host of nourishment and suppress immune system
Parasitic pathogenesis is usually an exogenous source, not found in normal flora. How do they mainly infect the body?
ingestion or direct penetration
T or F: Adhesion of parasites is usually not as tissue specific
true
Most protozoans replicate intra- or extra-cellularly in the human host. Do worms only produce intra-cellularly or extra-cellulary?
extra-celluarly
Severity of parasitic pathogenesis depends on what 2 things?
1. infectious disease dose (how much did you ingest)
2. the pathogen itself (where is it living?)
Parasites are usually not very virulent. They can be subacute or chronic but some can have ________ infections.
asymptomatic
____________ a single-celled microscopic animal of the kingdom of Protista.
Protozoan
Sexual reproduction occurs in parasites via what?
definitive host (not all undergo sexual reproduction)
What does the intermediate host do?
support ones or more developmental cycles
What is it called when an intermediate host does not allow transmission to a definite host? What does this prevent?
dead-end host - prevents parasite from completing development (ex. Lyme disease)
Protozoans usually reproduce via what?
binary fission
What is the organism class, Apicomplexans/Sporozoa, morphology like? How do they reproduce? What is a good example?
unicellular;, frequently intracellular, multiple forms including trophozoites, sporozoites, cysts (oocysts), gametes; schizogony and sporogony (asexual and sexual reproduction), NO organelle of locomotion; Plasmodium
Which organism class of protozoans is unicellular, involved in binary fission OR conjugation, and uses cilia? List a good example.
Ciliates; B.coli
Which organism class is unicellular, possibly intracellular, reproduces via binary fission, and uses flagella? List a good example.
Flagellates; Leishmania donovanii
Ameba is a unicellular protozoan. It has ___ and ____. It reproduces via binary fission. It uses ______ for locomotion. A good example is Naegleria fowleri (brain-eating ameba)
cyst and trophozoites; pseudopods
Which class is Plasmodium in?
apicomplexan so complex life cycle
How is Plasmodium spread? What is its definitive host? What disease does it cause and what is its epidemiology?
during blood meal; definitive host: mosquitos; most tropics with high burden in Sub-Saharan Africa; causes malaria
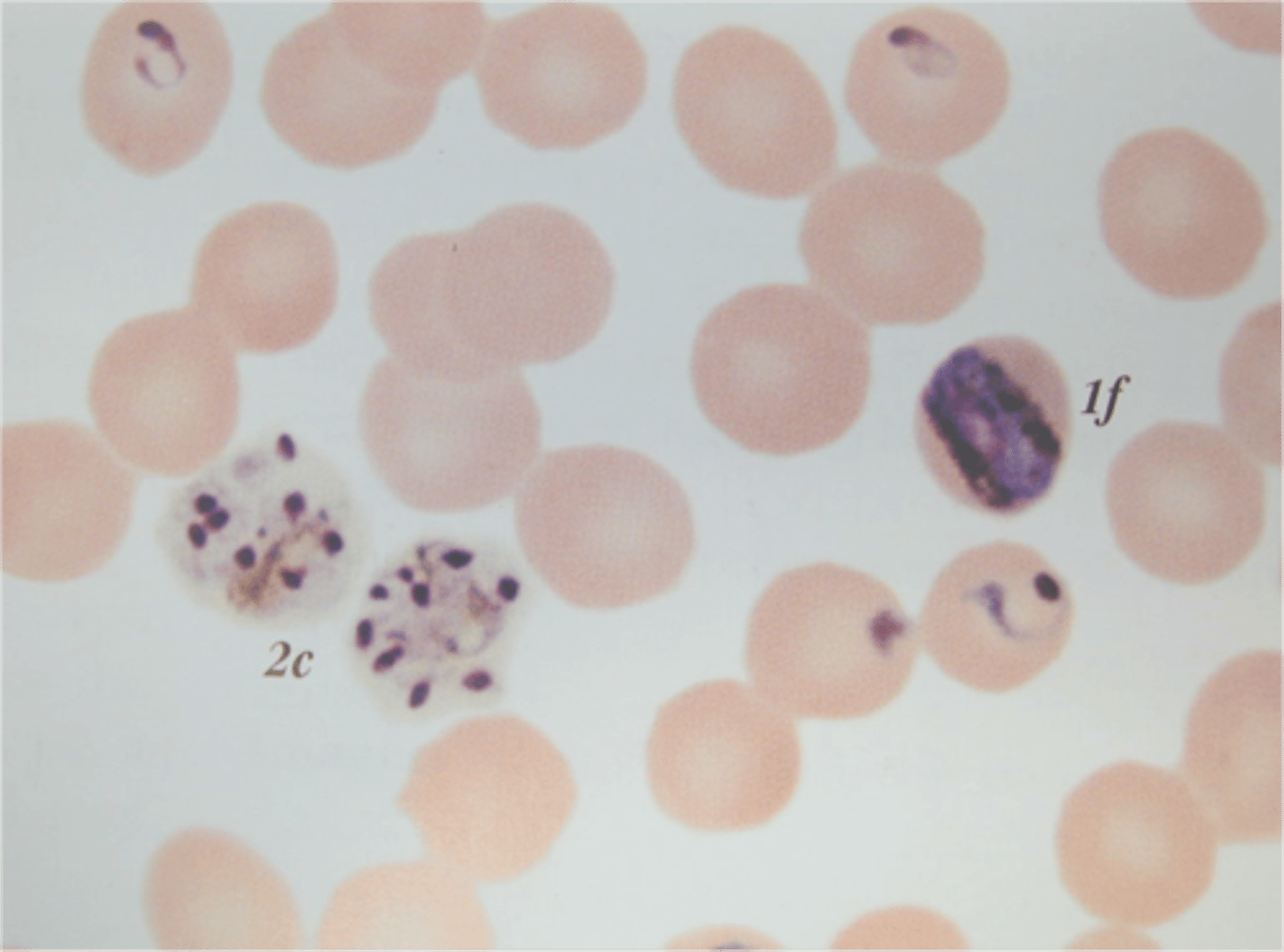
The Plasmodium life cycle begins with _____ biting which ejects _______ into the liver.
mosquito; sporozoites
In the Plasmodium life cycle, the sporozoites turn into what in the liver? What do they affect once they leave the liver?
meterozoites get released and infect RBCs
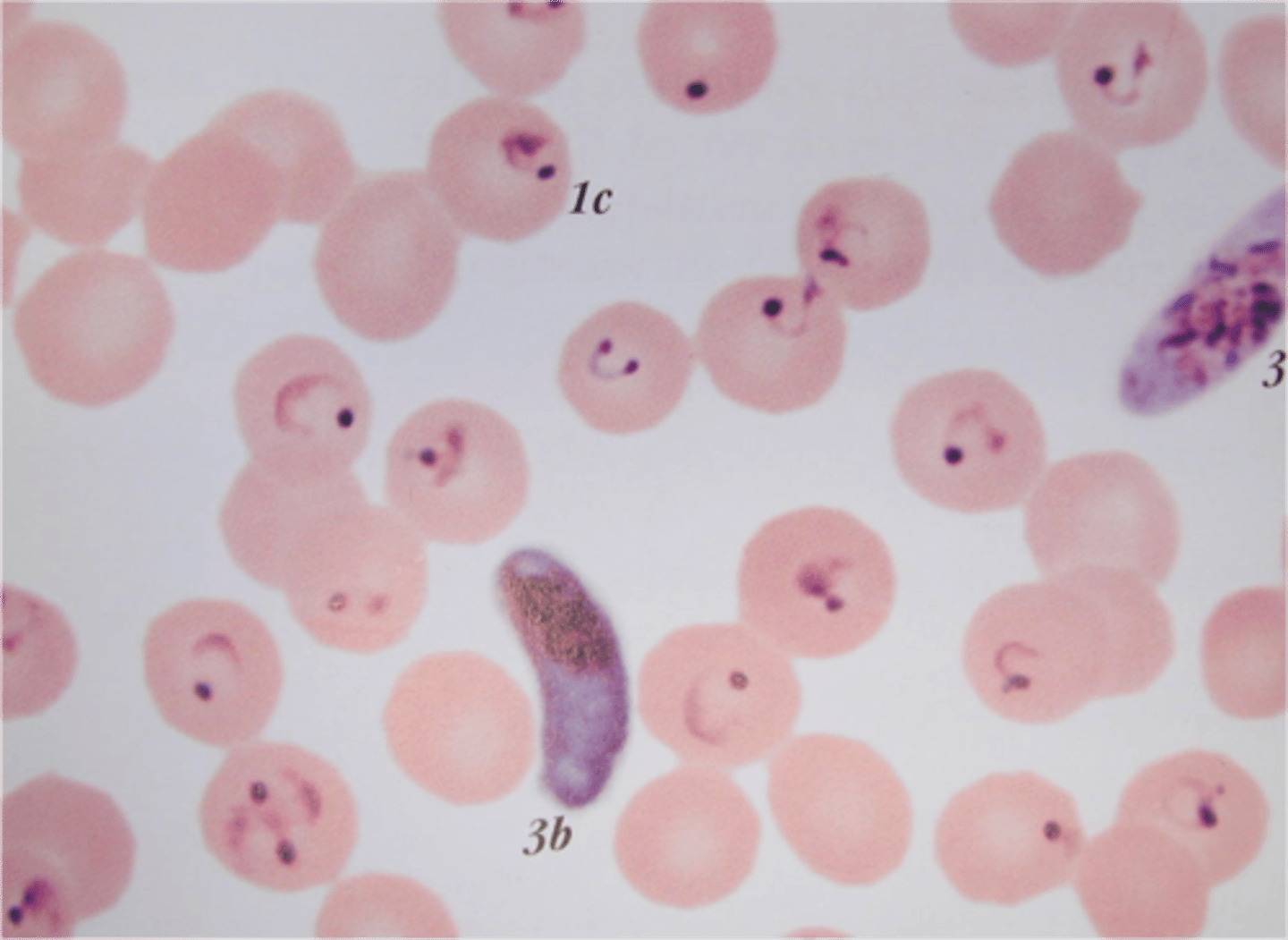
In the Plasmodium life cycle, meterozoites infect RBCs and develop a ring formation making them ________.
trophozoites
In the Plasmodium life cycle, trophozoites can then either become what?
1. develop into male and female gametocytes (adults) where they are ingested by mosquito during feeding OR
2. revert back to meterozoites and reinfect RBCs
Malaria (caused by plasmodium) has a 2 week incubation period. What are some of its symptoms? P. falciparum cam infect more RBCs and lead to what two major medical issues?
cyclic fever, chills, headaches, myalgias, arthralgias; cerebral malaria and kidney failure
Which morphological form of malaria is most likely responsible for a relapse in the infection?
hypnozoite
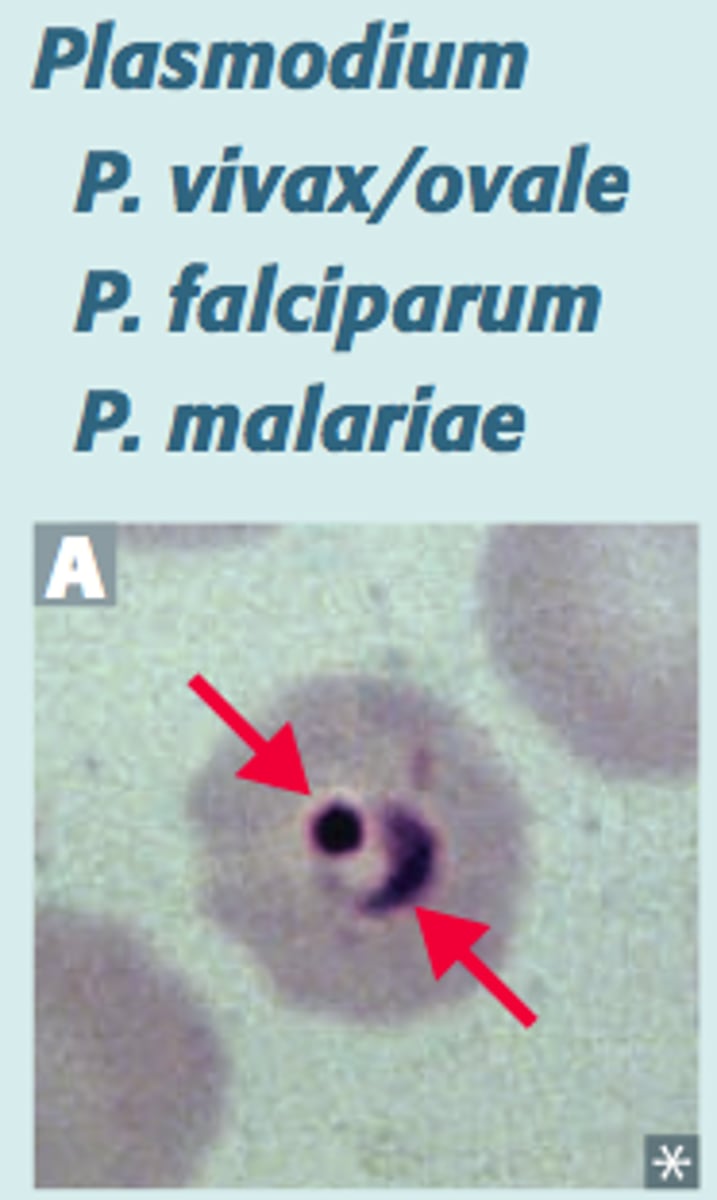
What parasitic infection has flagellated protozoan and gets spread via warm water and fecal contamination?
Giardia lamblia
3 multiple choice options
Giardia lamblia gets transmitted through what? It can be found world wide but you are more act risk when you are doing what activities?
ingestion of cysts; hiking, camping, river streams, swimming
T or F: Giardia lamblia is resistant to stomach acid and attaches to the intestines, resulting in malabsorption.
true
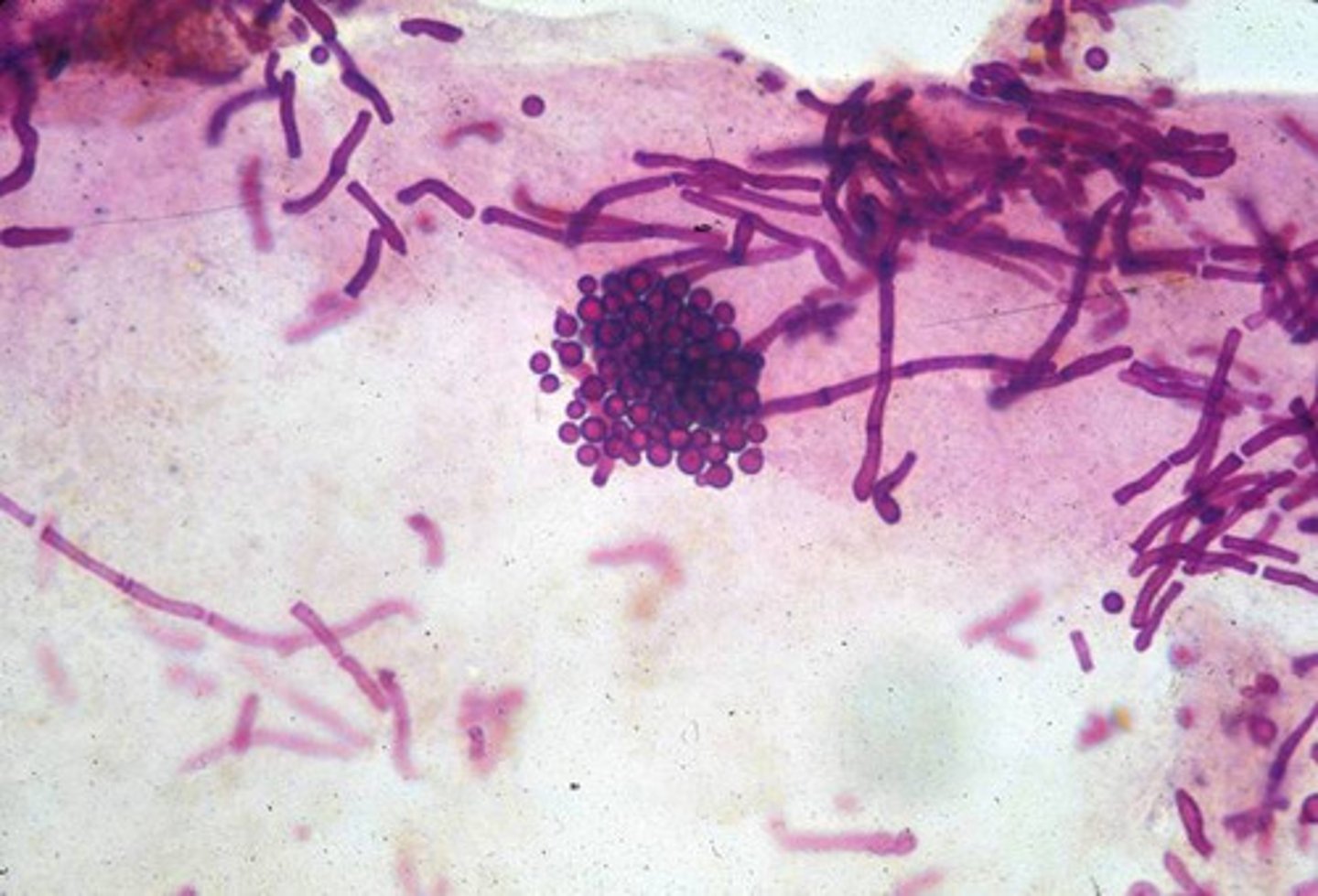
What is Giardia lamblia's infective stage? What about its diagnostic stage?
Infective- human ingests cyst
Diagnostic- trophozoites are passed in stool or look for a cyst
What types of symptoms does some with Giardia lamblia have?
abdominal pain and bleeding, flatulence, large-volume, watery, foul-smelling diarrhea ("greasy")

How do you diagnose Giardia lamblia?
-O&P visualize trophozoites, cysts in stool
-stool antigen test
*picture is trophozoite

What protozoan is located in the urogenital tract and is the ONLY protozoan transmitted sexually? It causes trichomoniasis.
Trichomonas vaginalis
3 multiple choice options
Entamoeba histolytica, Giardia intestinalis, Crptosporidium spp., Cytoisospora belli, Cyclospora cayetanensis, and Microsporidia all are located where and are transmitted via what?
intestinal tract; ingestion of cysts in food or water
T or F: Helminths are uni-cellular eukaryotes.
FALSE; they are multi-cellular eukaryotes
T or F: The helminths, flukes and nematodes, have a digestive tract while tapeworms do not.
true
How do platyhelminths appear?
flattened bodies with muscular suckers and / or hooks for attachment to the host

How to nematodes appear?
long cylindrical bodies and generally lack specialized attachment organs (but hookworms do)

What are the 4 ways helminths are transferred?
1. swallowing infective eggs or larvae (fecal-oral route)
2. Swallowing infective larvae in the tissues of another host (ex. eating raw meat)
3. Active penetration of the skin by larval stages
4. The bite of an infected blood-sucking insect vector
Trematodes aka flukes are mostly hermaphrodites (have both female and male organs). The eggs develop into larvae and must pass through what to be infectious again?
intermediate host
ALL flukes/trematodes have an indirect life cycle involving stages of larval developing in the body of _____. 2 of the species are transmitted by eating infected freshwater _____ and _____.
a snail; freshwater fish or crabs
How are humans infected by flukes/trematodes?
when they encounter water containing infective larvae released from the snails, the larvae penetrating the skin
What is the definitive and intermediate host of the Schistosoma species? How are humans infected?
Definitive host- human
Intermediate host- snail
Humans are infected when cercariae penetrate the skin

Where is the Schistosoma species found?
fresh water with snails
Cerceriae (a Schistosoma species) penetrate the skin in fresh water. They get into the circulation and go to the ______ where they mature into adults. Schistosoma mansoni adults moves to the venules of the __________. Eggs shed back into fresh water and hatch, penetrating the _____ (intermediate host). Cercariae are released to infect.
liver; bowel/rectum; snail
Schistosomiasis is most known for causing what rash?
Swimmer's itch - pruritic popular rash usually on legs and feet (but sometimes asymptomatic)
How do you diagnose Schistosoma? What are some prevention strategies?
eggs in stool/urine, ELISA; water sanitation, mass antiparasitic therapy of a community, control of water snail population

How do Schistosoma evade the immune system?
-surface coated with molecules that mimic self antigen (body does not recognize as foreign
-surface protein that inhibits MAC formation (end of complement cascade)
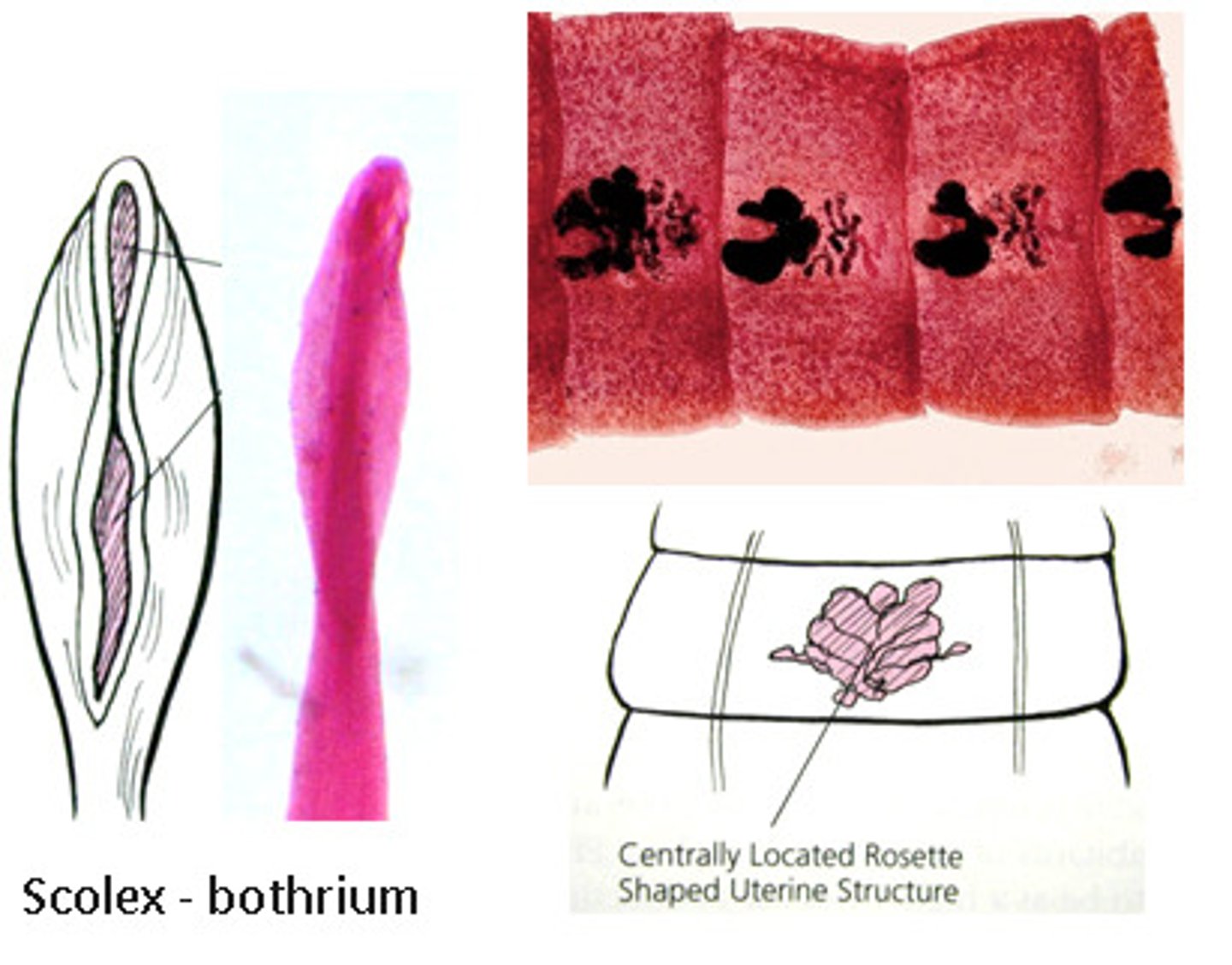
What is a prominent feature of the cestodes (aka tape worms)?
proglottid at each segment with reproductive organs (male and female) within each segment
In cestodes, the gravid proglottid contains what? What do the terminal proglottids do?
gravid - contain fertilized eggs
terminal-released and pass through feces
In cestodes, what must the larvae do in order to be infective again? What do they have that can attach them to the intestinal wall?
larvae must go through 1 intermediate host before it can be infective; uses scolex, suckers to attach to intestinal wall
Diphyllobothrium latum is a form of tapeworm also known as "________ tapeworm." What is the shape and size of the proglottides like?
"fish tapeworm"; proglottids are wide and short
What is the definitive and intermediate host of the Diphyllobothrium latum?
Definitive host: humans (and other animals that each fish
Intermediate host: freshwater fish (crustaceans as well)
-ingest larvae in flesh of raw/undercooked fish
Where are most cases of Diphyllobothrium latum?
Northern hemisphere - Scandavia, norther Russia, Japan, Canada, some north-central states of US
What is the life cycle of Diphyllobothrium latum?
1. human ingests raw or undercooked freshwater fish that contain larvae
2. Larvae develop into adults in small intestine
3. Eggs released by proglottids and enter fresh water to embryonate
What does Diphyllobothriasis cause?
vitamin B12 deficiency (megablastic anemia), mechanical obstruction of intestines, weight loss, malabsorption
-can be mostly asymptomatic
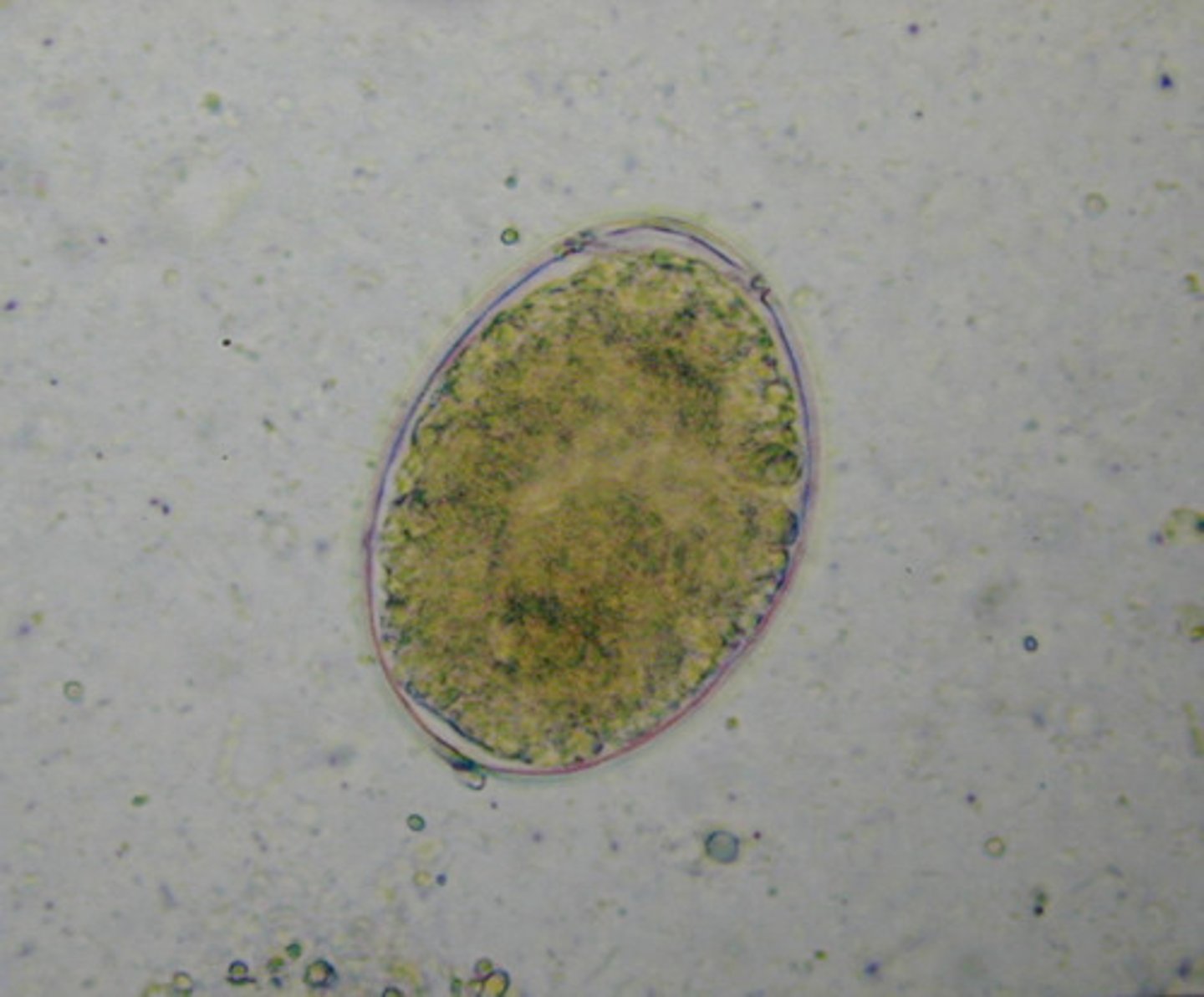
What are some diagnostic test for Diphyllobothrium latum? What are some prevention strategies?
tests: proglottids, eggs in stool (eggs have a clear zone and a cap), low serum vitamin B12
prevention: proper disposal of human feces, cook fish thoroughly
In nematodes (round worm), the sexes are ______. Most species liberate fertilized eggs from the host.
separated
T or F: In nematodes, the development from egg, to larvae, to adult can be direct and occur in the same host. Some are highly human-specific while others are zoonotic
true
Necator is a _______. It has a _______ definitive host. It is transmitted by direct penetration of skin by larvae.
nematode; HUMAN-ONLY DEFINITIVE HOST
In a necator, a form of nematode/hook worm, it is mostly found in what (they require this to hatch)?
warm-moist soil

The life cycle of an intestinal hookworm, like a necator, the eggs are released in human feces and require warm soil to hatch. They develop into larvae where they penetrate human skin and move into what? Where do they develop into adults?
circulation to the lungs where they are coughed up and swallowed; small intestine where they hook onto wall

Adult hookworms attach to intestinal wall and secrete enzymes which are what? How can we prevent hookworm?
anticoagulants (leading to anemia); wear shoes in endemic areas, prevent human feces from contaminating soil

Parasitic infections involve increasing which leukocyte the most?
eosinophils
What is the treatment for Giardia (diarrhea)? What does it do?
metronidazole- causes DNA breaks and inhibits DNA synthesis, leading to death
The Necator is treated using Mebendazole or albendazole. What does it do?
prevents microtubule formation, disrupts cellular transport, starving parasite
List 2 of the most important parasitic and fungal immune evasion strategies.
1. interfere with complement activation
2. Schistosoma has a surface protein that inhibits MAC formation
Ectoparasites are arthropods found either on the ____ or only in the superficial layers.
skin
T or F: Ectoparasites include 6-legged arthropods and arachnids (8-legged arthropods).
true
In a brown recluse spider bite, what common feature may you see?
necrotic ulcer (tissue necrosis due to proteolytic enzymes in venom)

In louse/lice, the nits are egg and found attached where?
hair shaft (very sticky)
Botfly or other flies deposit eggs in a _____. The egg then hatches to produce _____
wound; larvae

Bedbugs cause what?
pruritic (itchy), erythematous wheal

How are mites/scabies spread? What symptoms do they cause?
personal contact / fomites such as clothing (overcrowding/unhygienic conditons); pruritic, red lesions (delayed hypersensitivity reaction to antigenic proteins of eggs or feces)
-affects 700,000,000 worlwide

A black widow spider bite results in what symptoms?
1 hour after bite- pain and numbness spread
-fever, chills, sweats, vomiitng

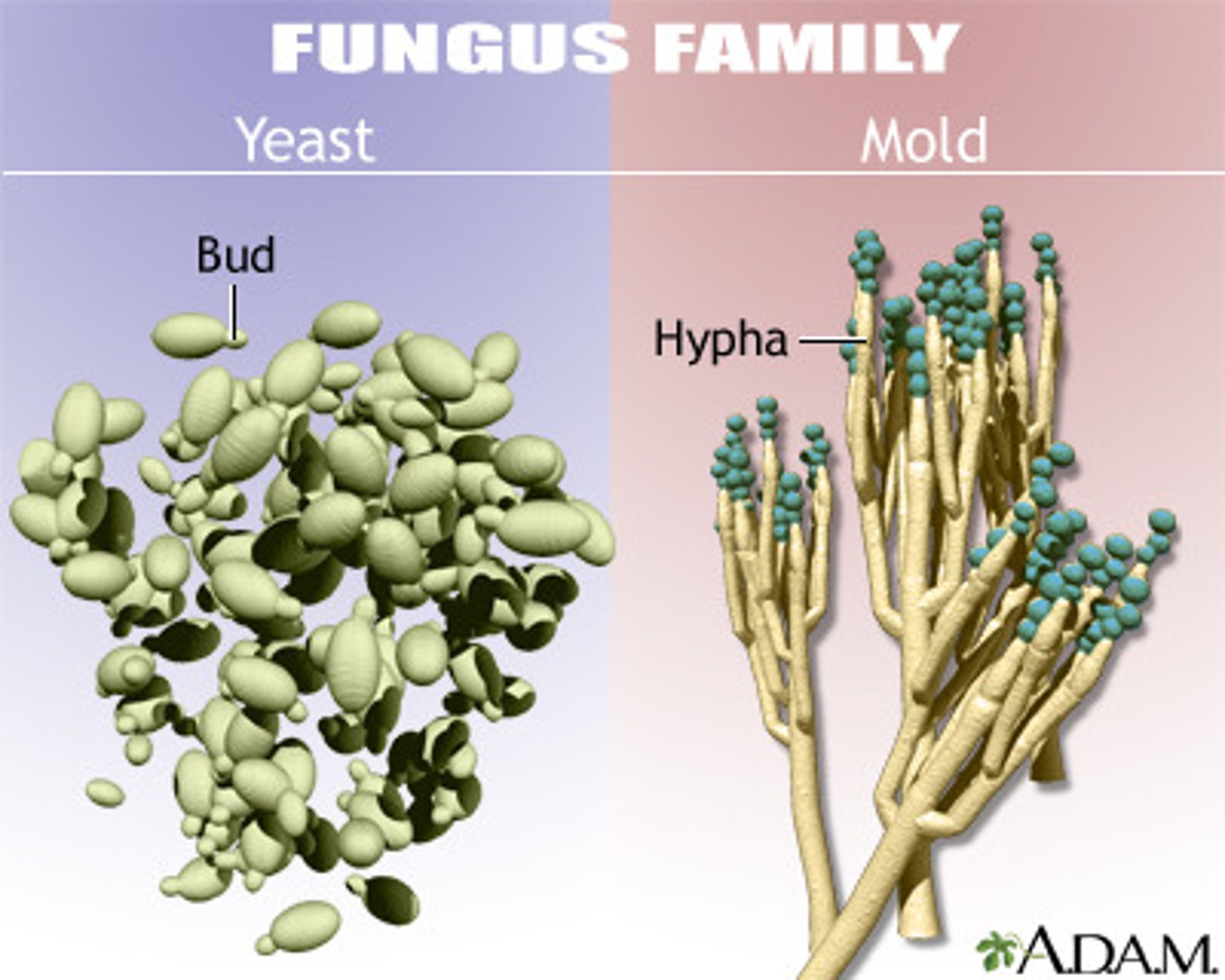
Define mycology
study of fungi (yeast and molds)
Infections caused by mycoses are always due to _________
fungi
3 multiple choice options
What differentiates molds and yeast?
Molds- multicellular mold have hyphae (multicellular filaments), grow fuzzy
Yeast- round, unicellular (single cell), reproduce by budding (asexual- asymmetrical division), grow as colonies
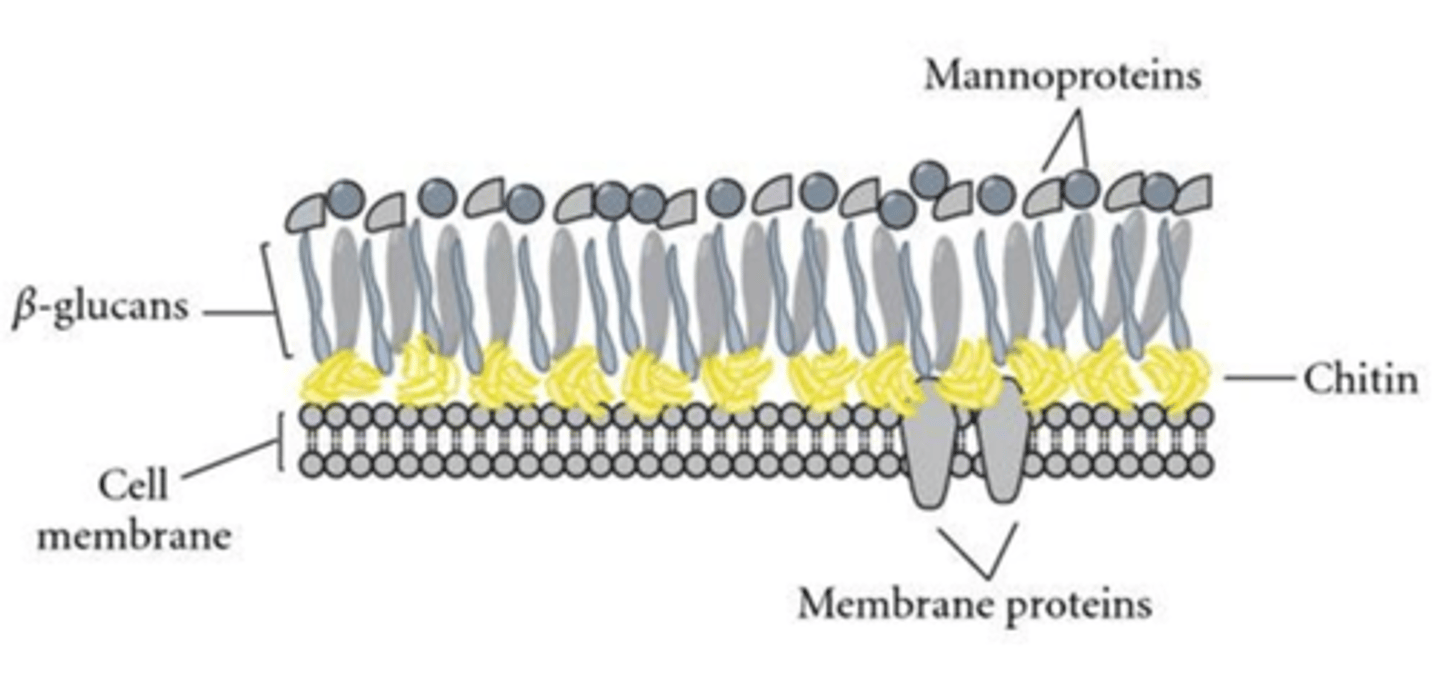
What does the cell membrane of fungi contain?
ergosterol
What does the cell wall of fungi contain?
chitin (over plasma membrane), beta-glucans (leukins), mannoproteins (surface)
Myosis is an infection caused by a _________
fungus
One fungus, a yeast, has a capsule. What is it called?
Cryptococcus neoformans
T or F: Fungi have nucleus and organelles as well as the mitochondria.
true
What do Azoles and Terbinafine do to fungal cells?
interrupt/stop ergosterol synthesis, making the cell membrane weak
What does Flucytosine do to fungal cells?
stops DNA/RNA synthesis
What do Echinocandins do to fungal cells?
stop Beta-glucan synthesis, so cells lose their intergrity
What do Amphotericin B and nystatin do to fungal cells?
form pore
___________ interact with ergosterol, disrupt plasma membrane, causing the fungal cell to burst.
Polyenes
_________ and _______ inhibit ergosterol synthesis in fungi.
Azoles and Allylamines
_______________ inhibit glucan synthesis (in fungal cell wall)
Echinocandins
What similarities do mold and yeast share? (both are fungi)
all are free living in the environment with no obligate intracellular needs
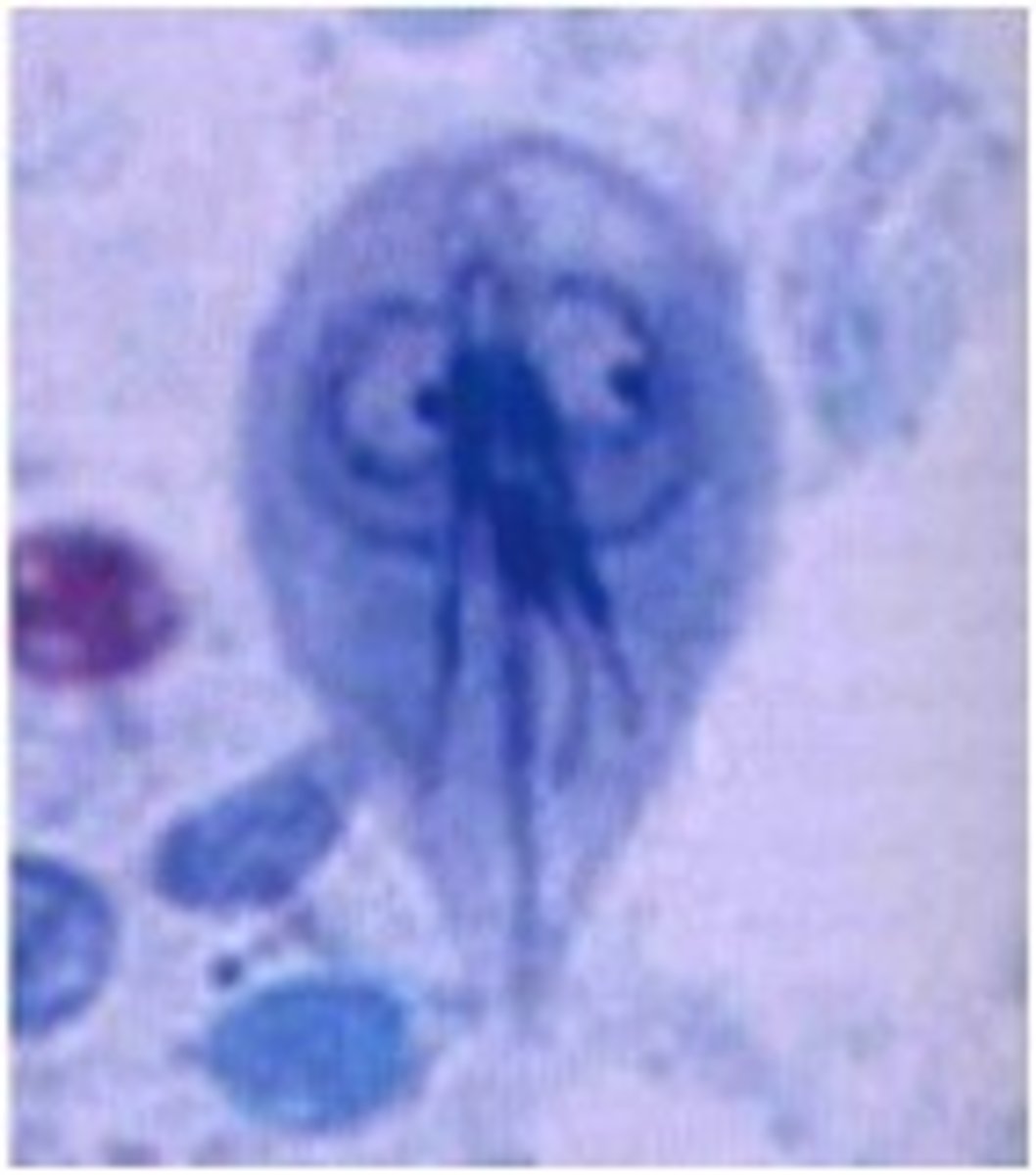
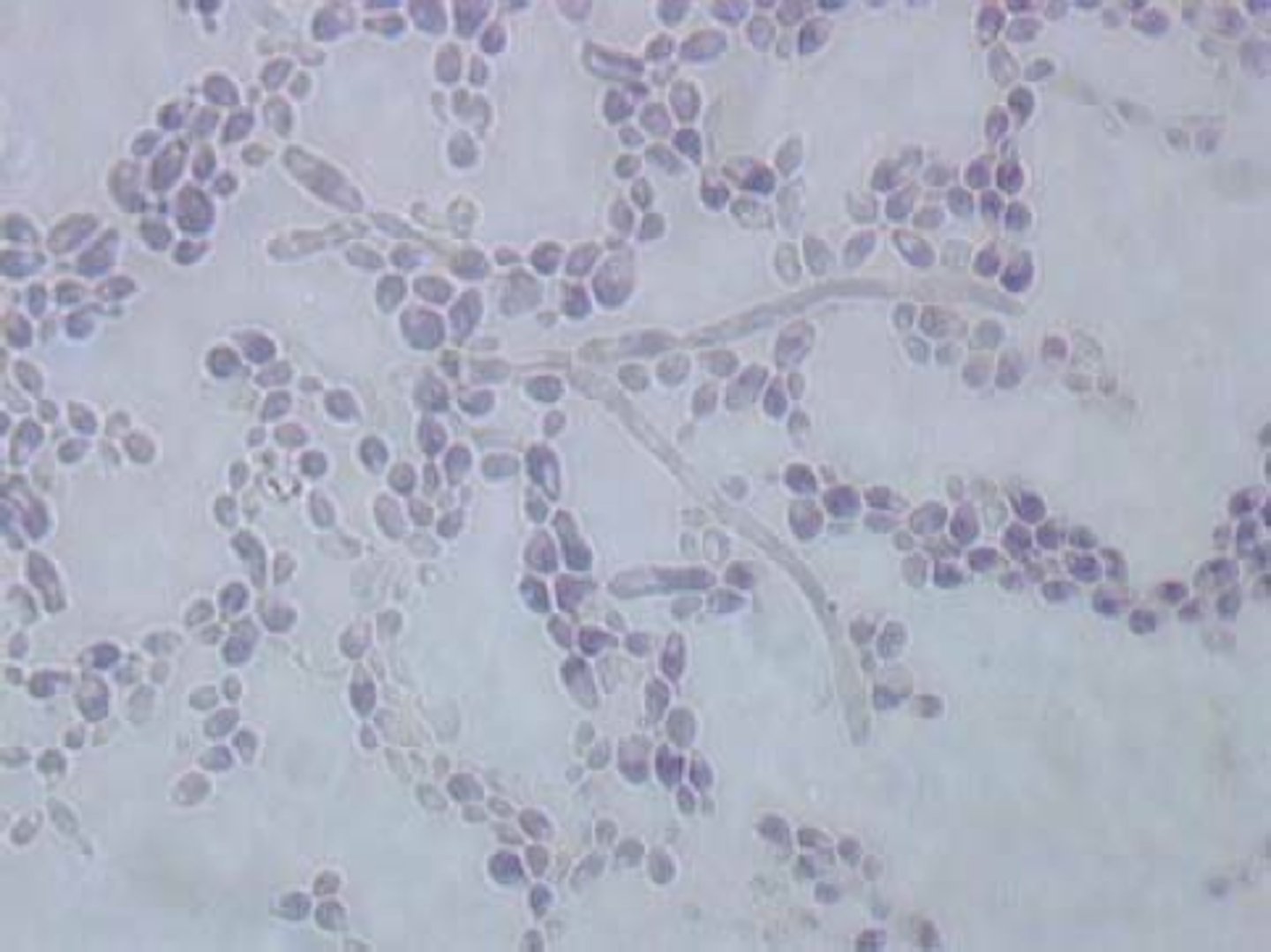
What are the buds in yeast called? What are they called when they will not detach, therefore forming a chain?
buds = blastoconidia
chain = pseudohypha / pseudohyphae
What species is the most common yeast infection?
Candida
How does Candida albicans transmit? It is an opportunistic pathogen
humans- normal flora of colon; colonization of oral cavity, rectum, and vagina
What fungus is the most common cause of invasive fungal infections in immunocompromised?
Candida albicans

What are the risk factors for Candida?
-antibiotic use (loss of protective normal flora)
-immunocompromised- HIV/AIDS, neutropenia (no neutrophils to control)
-poorly controlled diabetes
-pregnancy (esp. 3rd trimester)
-impaired cell-mediated immunity
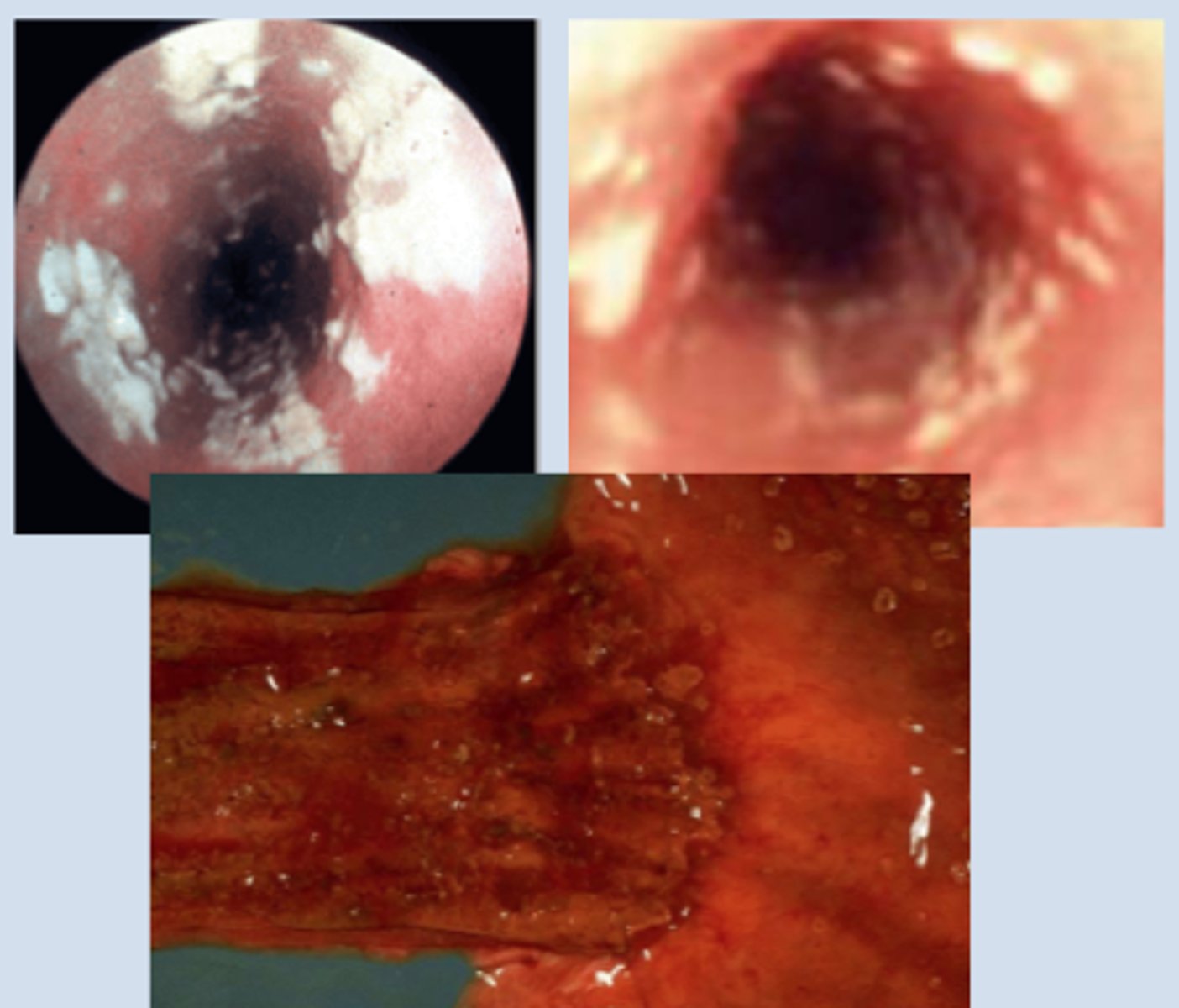
What are some oral candidiasis infections? (hint:2)
1. Thrush- white patches, pseudomembranous that can be wiped off
2. Esophagitis- difficulty/painful swallowing, AIDS-defining infection
How does someone diagnose candida albicans?
Microscopically with KOH prep (destroys human cells, but allows fungal cells to remain)
-look for budding yeasts and pseudohyphae
What are the treatments for candida albicans?
-oral/topical fluconazole: inhibits sterol synthesis
-echinocandin: stops glucan synthesis
How does the yeast, Malassezia transfer?
normal flora of skin --> overgrowth
What is one of the most common superficial (just on skin) mycoses worldwide?
Malassezia furfur
Malassezia fufur is what type of infection? What layer of the skin is it limited to and what does it prefer to be around?
cutaneous infection; stratum corneum; prefer around sebaceous glands (like lipids)