Neurology Physiotherapy Wk7-11
1/31
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
32 Terms
Difference between Walking & Gait
Walking: means of locomotion involving the use of two legs, where one foot is always in contact with the ground, and each leg alternately provides support with propulsion (the action)
Gait: a person’s manner of locomotion (the pattern)
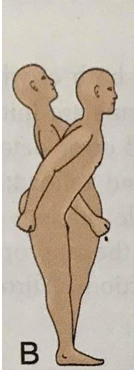
What are some common neurological Presentations of Gait?
Ataxic gait (lurching from side to side)
Parkinsonian gait (shuffling)
Spastic gait (hemiplegic, diplegic) (affected leg swoops)
Myopathic gait (waddling)
Neuropathic gait (high-stepping to compensate foot drop)
3 Essential Components of Walking
Propulsion → generation of power to propel body in intended direction
Postural control → maintain dynamic stability though movement
Adaptation → modulation of pattern to achieve goals
What is Postural Control? and the 2 aims?
Control of posture and movement in attaining balance
Motor output that occurs following integration of sensory, perceptual, cognitive and motor processes
Aims:
Postural equilibrium/stability: maintain upright position and COM
Postural orientation: gravity, vertical, internal references, environment
Sensorimotor Control of Balance
Sensory Input (vestibular, visual, proprioceptive)
Integration of Input (coordination of posture, movement and balance)
Motor output (VOR, motor impulses)
Balance
3 Essential Components of Sensation
Somatosensory System (proprioception)
Vision (perception of verticality)
Vestibular system (head position relative to gravity)
Sensory feedforward for anticipatory postural adjustments
Components of Sensory Integration and Weighting of Perception
Brain receives visual, vestibular and somatosensory input to guide motor control
Signals are effectively integrated and weighted (upweighted-downweighed)
Minimal cognitive processing by the cortex for postural control
Movement Plan Selection and Coordination
Optimal motor plans developed with:
Knowledge of individual, task and environment
Motor plan generated in cerebral cortex → refined in BG → transmitted to peripheral motor system → motor plan acted upon
BG and cerebellum use sensory feedback to detect errors
Execution of Balance Motor Responses
Motor response by which balance recovering determines whether the displacement is COM causes a fall
Appropriate motor responses require
Muscle strength, power, endurance, ROM
Fine grading of agonists, antagonists, synergists and appropriate co-contraction
High level of reciprocal innervation
Attention, cognition, judgement and memory
3 Reflexes of Balance in Motor
VOR → stabilization of the gaze when the head moves
VSR → controls body when head moves
Righting reactions → head righting, trunk righting and limb movement
What are APRs?
APR → Automatic Postural Responses
Operate to keep center of gravity of base of support
Occur in response to unexpected stimulus
If a balance disturbance is predicted, the body responds in advance by developing a “postural set” to counteract the coming forces
Failure to produce appropriately calibrated APAs → risk of sudden balance loss
4 stereotypical APRs
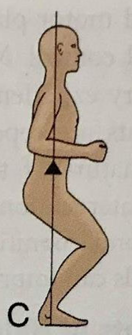
APR: Ankle Strategy
Anteroposterior perturbations
Ankle movement to restore COM
Forward loss of balance: gastrocs → hammys → paraspinals
Backward loss of balance: tib ant → quads → abdominals
Head movement occurs in-phase with hips
APR: Hip strategy
Anteroposterior and medial-lateral perturbations
Rapid hip flexion and extension to maintain
Forward loss of balance: abdominals → quads → tib ant
Backward loss of balance: paraspinals → hammys → gastrocs
Head movements occur out of phase with hips
APR: Suspension Strategy
Lowering of COG toward BOS
lower extremity flexion
easier to control COG
APR: Stepping and Reaching Strategies
Large forces displace COM beyond stability limits
Step/reach enlarges BOS
Perturbations are rapid and large amplitude
Motor Components of Balance: Volitional Postural Movements
Consciously controlled movements
Range from simple weight shifts to complex balance skills
disturbances COG disturbances to reach a goal
Strongly modified by experience and instruction
3 Key Steps in Functional Assessment of Balance
Observe the Task
Identify movement components (postural alignment, quality, patterns)
Identify impairments interfering with movement
Physical Examination of Balance: Examine & Establish
Examine:
variety of conditions, static/dynamic sitting, static/dynamic standing, running, skipping, bouncing, jumping etc
Establish:
level of independence and support, endurance, alignment/symmetry, balance reactions, anxiety levels
Common Impairments in Neurological Patients Associated with Reduced Balance
Motor Dysfunction
Musculoskeletal: Muscle strength, trunk instability, ROM, altered muscle tone
Biomechanics: Stability limits, balance response, altered movement strategies
Sensory Dysfunction:
Altered sensation: proprioception, vestibular system damage, dizziness, visual deficits, somatosensation
Altered Sensory Integration: difficulty dividing attention between tasks, delayed response, altered stability limits
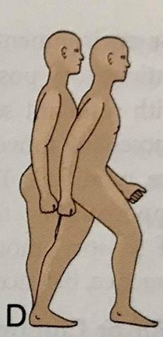
Gait Problems in Neurological Patients - Heel Strike to Midstance
Impaired Trunk control (upper trunk over lower trunk)
Lack of proper initiation pattern (lateral weight shift, forward trunk flexion)
Insufficient ankle joint DF (muscle tightness, oedema, impaired muscle activation)
Inappropriate foot contact
Gait Problems in Neurological Patients - Single & Double Limb Support
Insufficient trunk control to maintain alignment over one leg (loss up upper trunk control, asymmetries during unilateral stance)
Altered LL control (hip instability, loss of knee control, altered timing of LL muscles)
Loss of ability to transfer weight through foot (inability to maintain leg on floor behind body)
Gait Problems in Neurological Patients - Early & Late Swing
Atypical leg muscle firing patterns (lack of initiation, can’t control trunk and LL sequencing)
Inability of body to continue to move forward as leg swings
Aberrant foot movement
Functional Ambulation Assessment Considerations
Clinical reasoning
Consider use of walking aid
Create a safe situation
Incorporate various environmental contexts and tasks
Challenge their behavior
Activity Measures (Balance, Mobility/Gait)
Balance
Sitting Balance test
Clinical Test of Sensory Interaction and Balance
Functional reach test / lateral reach test
Four square step test
Gait/Mobility
6-min walk test
Timed up and go test
Considerations for Re-training Balance and Gait
Impairments may be temporary and re-trained (neural adaptation)
Consider principles of motor learning
Follow a progression
Target patient’s deficits/impairments
Manage fear of falling and falls risk
Critical Factors to Optimize Motor Learning for Restoration of Function
Establish concrete goals
Modify tasks to achieve success
Provide instructions as well as demonstrations
Practice routines using same cues
Monitor performance
Give feedback
Benefits of Balance Training
Encourages LL strength and endurance
Optimize soft tissue extensibility and joint flexibility
Maximize skill through progressive challenges
Improve ADLs
Gait training often focusses on ___-___degrees hip _____ in _____ stance plantarflexion at end of stance for ____ __ flexion at the hip for pull off.
Gait training often focusses on 10-15hip extension in late stance plantarflexion at end of stance for push off flexion at the hip for pull off.
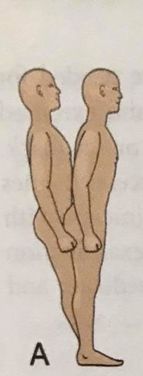
Parkinson Gait Characteristics
Shuffling steps
Bradykinesia
Difficulty turning
Reduced arm swing
Muscle weakness
4 Components of Re-education in Balance
Restoration
Adaptation
Maintenace
Prevention
3 Types of Gait Training to maximize speed, skill and endurance
Overground walking → regular floor surface (whole task)
Speed-dependence & BW supported Treadmill → speed and duration gradually increased
Robot-assisted gait → walking with electromechanically controlled footplates that controls the legs.
Examples of Gait Training Interventions
Improve gait velocity
Improve swing motion and step length
Address contributing impairments
Improve gait symmetry
Minimize impact of compensations
Improve push-off