Chapter 20: The Heart
1/92
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
93 Terms
3 major components of the cardiovasular system
heart, blood vessels, and blood
function of heart
pumps blood
blood vessels
transport blood throughout the body
blood
carries oxygen, nutrients, and waste products
amount of blood pumped by the heart per minute
5 liters per minute
total volume of blood in the body
5-6 liters
two main circulatory circuits of the cardiovascular system
pulmonary circulation and systemic circulation
pulmonary circulation function
right heart pumps deoxygenated blood to lungs for gas exchange
systemic circulation function
left heart pumps oxygenated blood to the rest of the body
why is the pulmonary circuit a low-pressure system?
it only pumps blood to the lungs, a short distance, so less force is needed
why is the systemic circuit a high-pressure system?
it pumps blood to the whole body, a long distance, so it needs more pressure
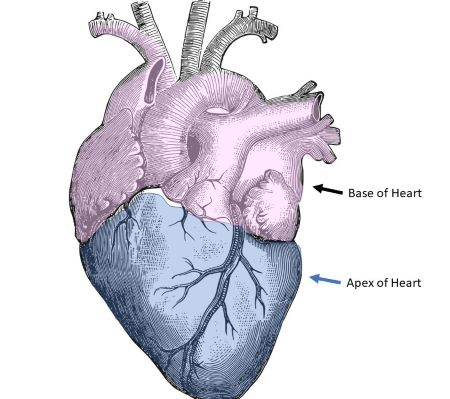
shape of the heart
cone-shaped
size of the heart
about the size of a fist
location of the heart
located in the mediastinum between the lungs, 2/3 to the left of midline, with apex pointing left and resting on diaphragm
where is the apex located and what forms it
pointed inferior (bottom) tip formed by the left ventricle
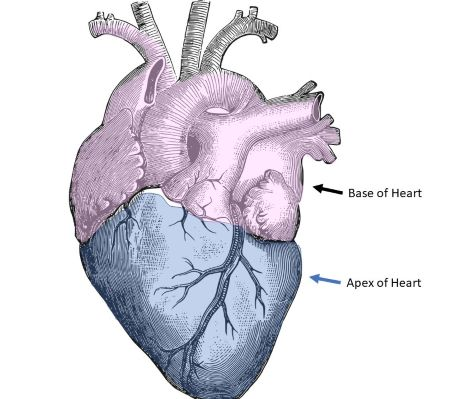
where is the base located and what forms it
broad posterior (top) surface formed by the atria
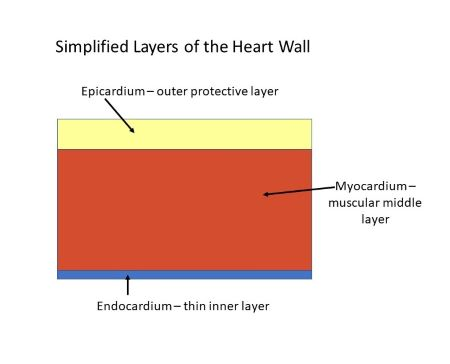
3 layers of the heart wall
epicardium (visceral pericardium), myocardium, endocardium
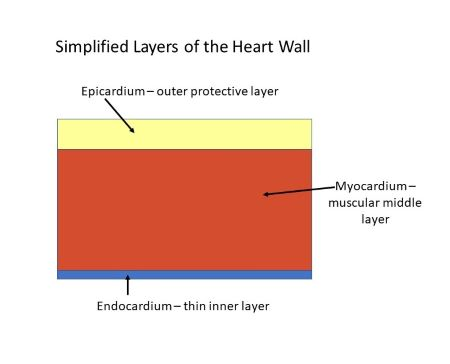
epicardium (visceral pericardium) function
outer protective layer, reduces friction
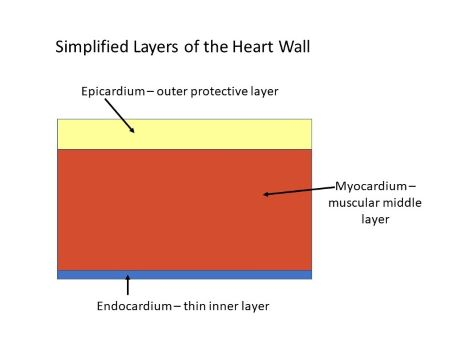
myocardium function
middle muscular layer responsible for contraction
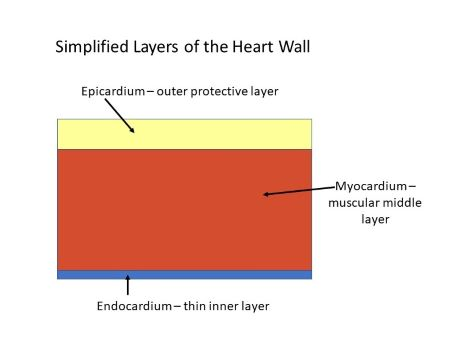
endocardium function
inner layer lining chamber and valves; smooth surface for blood flow
2 layers of pericardium
fibrous pericardium, serous pericardium
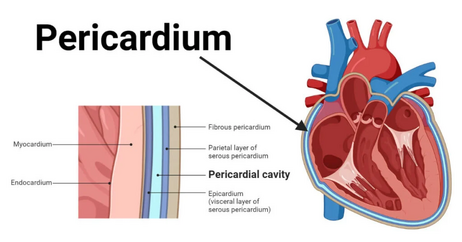
fibrous pericardium function
tough outer layer anchoring the heart, prevents overstretching
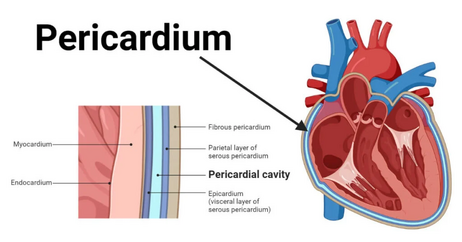
serous pericardium
double-layered membrane (parietal and visceral) with pericardial fluid to reduce friction
what happens if pericardial fluid decreases excessively?
friction between heart and pericardium
what happens if pericardial fluid increases excessively?
compression of the heart, reduced filling, reduced cardiac output
4 chambers of the heart
right atrium, right ventricle, left atrium, and left ventricle
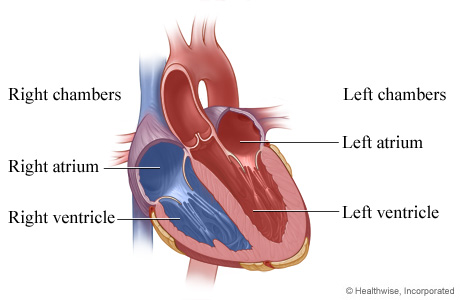
function of right atrium
receives systems venous blood
function of right ventricle
pumps blood to lungs
functions of left atrium
receives oxygenated blood from lungs
function of left ventricle
pumps oxygenated blood to body
what are auricles?
small pouch-like extensions of atria (plural of atrium)
what do auricles do?
they increase the volume capacity of atria (plural of atrium)
which ventricle has the thickest wall and why?
the left ventricle- it must pump blood throughout the entire systemic circuit at high pressure
what is the interventricular septum?
a muscular partition separating the right and left ventricles, crucial for preventing mixing of oxygenated and deoxygenated blood

what is a sulcus (plural sulci)
a groove on the external surface of the heart that marks the division between its chambers and provides a pathway for major coronary arteries and veins
3 sulci of the heart
coronary sulcus, anterior interventricular sulcus, and posterior interventricular sulcus
what does the coronary sulcus mark?
separates atria and ventricles
what does the anterior interventricular sulcus mark?
separates ventricles anteriorly
what does the posterior interventricular sulcus mark?
continuation of the anterior sulcus on posterior surface
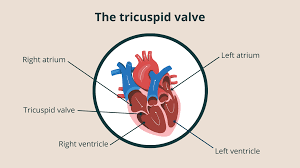
what are the atrioventricular valves?
tricuspid valve & bicuspid (mitral) valve
where is the tricuspid valve?
between the RA (right atrium) and RV (right ventricle)
where is the bicuspid (mitral) valve?
between the LA (left atrium) and LV (left ventricle)
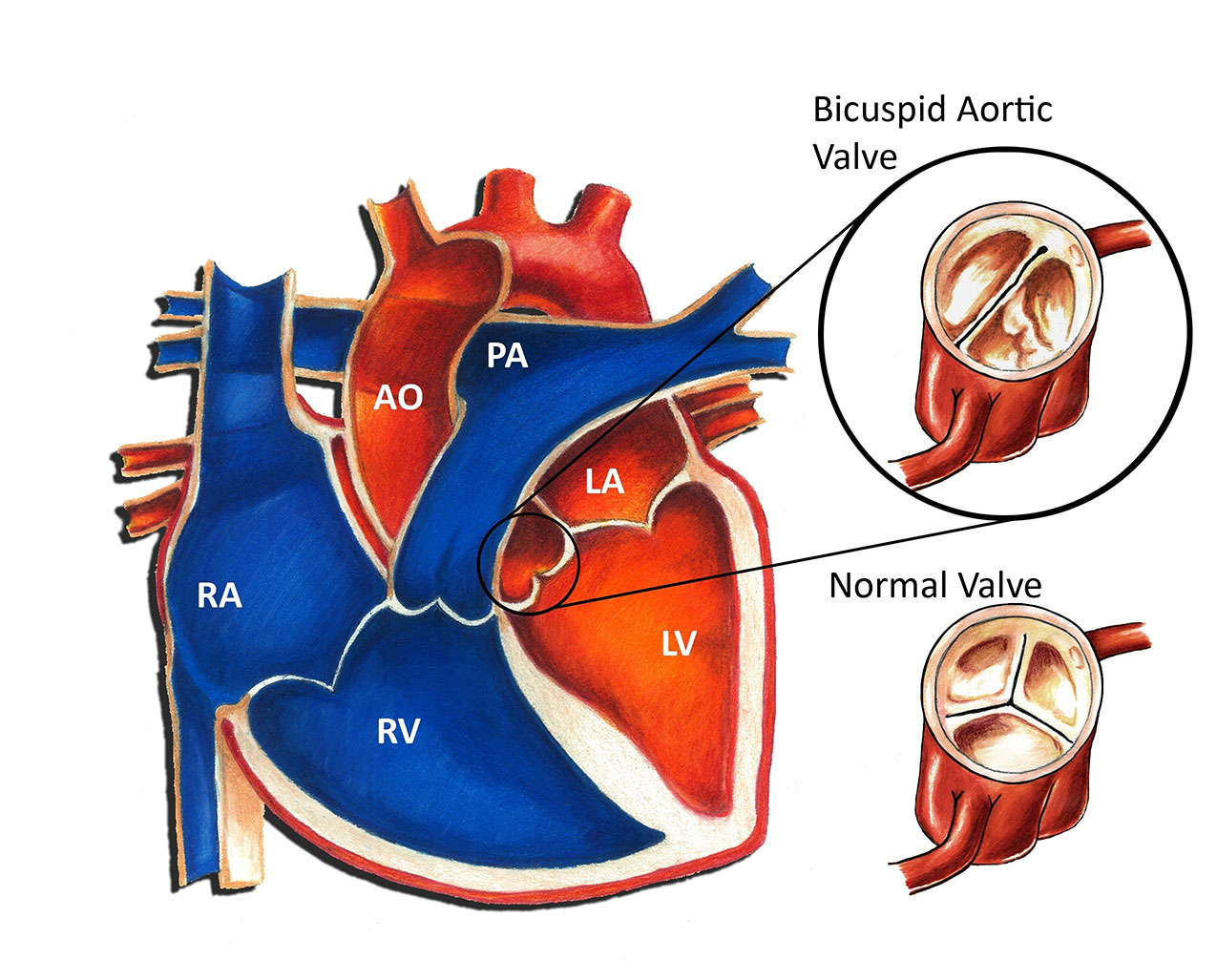
what are the semilunar valves?
pulmonary valve & aortic valve
where is the pulmonary valve?
between right ventricle and pulmonary trunk
where is the aortic valve?
between left ventricle and pulmonary trunk
what structures prevent aortic valves from prolapsing during contraction?
chordae tendineae attached to papillary muscles
stenosis
narrowing of valve opening
insufficiency
valve fails to close fully, causing regurgitation
flow of blood through the right side of the heart
SVC/IVC/coronary sinus, RA, tricuspid valve, RV, pulmonary valve, pulmonary trunk lungs
flow of blood through the left side of the heart
Pulmonary veins, LA, mitral valve, LV, aortic valve, aorta, systemic circulation
purpose of coronary circulation
to supply oxygen and nutrients to the myocardium, which is too thick to receive oxygen directly from blood in the chambers
what happens during coronary artery blockage?
Decreased oxygen supply, ischemia, angina pectoris, possible myocardial infarction if prolonged
intercalated discs
junctions between cardiac cells
junctions that hold cells together
desmosomes: hold cells together gap junctions: allow action potential spread between cells
autorhythmic cells
cells that spontaneously depolarize to generate action potentials, forming the conduction system
conduction pathway in order
SA node, AV node, AV bundle, bundle branches, Purkinje fibers.
why does the AV node slow down conduction?
to allow atrial contraction to finish before ventricular contraction begins
sympathetic nervous system
increases heart rate and contractility
parasympathetic nervous system
decreases heart rate
3 phase of cardiac muscle action potential
depolarization, plateau, repolarization
depolarization
Na⁺ influx
plateau
Ca²⁺ influx maintains depolarization
repolarization
K⁺ efflux
refractory period
time during which another AP cannot be generated
why is the refractory period important?
prevents tetanus in cardiac muscle, ensuring rhythmic contractions
ECG component
P wave, QRS complex, T wave
P wave
atrial depolarization
QRS complex
ventricular depolarization (and hidden atrial repolarization)
T wave
ventricular repolarization
P-Q interval
atrial to ventricular conduction
Q-T interval
entire ventricular depolarization-repolarization
what are the phases of the cardiac cycle
atrial systole, ventricular systole, atrial diastole, ventricular diastole
how does atrial systole contribute to ventricular filling?
adds ~25 mL of blood to the ventricles; ensures full preload before ventricular contraction
EDV
End-Diastolic Volume- volume in ventricles at end of filling, ~130
ESV
End-Systolic Volume- volume remaining after contraction, ~60 mL
stroke volume
EDV-ESV. Normal ~70 mL/beat
isovolumetric contraction
both valves closed; ventricles contract; pressure builds to open semilunar valves
what happens to the relaxation period as HR increases?
it shortens, decreasing coronary perfusion time
what causes the first heart sound (“lubb”)?
closure of the AV valves at the start of ventricular systole
what causes the second heart sound (“dupp”)?
closure of semilunar valves at the start of ventricular diastole
what is a heart murmur and what can cause it?
abnormal heart sound caused by valve stenosis or insufficiency
positive inotropic agents
increase contractility (e.g., sympathetic stimulation, epinephrine, calcium)
negative inotropic agents
decrease contractility (e.g., acidosis, high K⁺, calcium channel blockers)
cardiac reserve
the difference between resting and maximal stroke volume
3 major factors affecting stroke volume
preload, contractility, and afterload
what factors influence heart rate through autonomic control
baroreceptors, chemoreceptors, limbic system, proprioceptors, sympathetic/parasympathetic stimulation
how do hormones affect heart rate?
epinephrine, norepinephrine, and thyroid hormones increase HR; hyperthyroidism can cause tachycardia
tachycardia
heart rate is greater than 100 bpm
bradycardia
heart rate is less than 60 bpm
myocardinal ischemia
reduced blood flow → hypoxia → reversible
infarction
complete blockage → tissue death → irreversible
left heart failure
fluid backs up into lungs → pulmonary edema
right heart failure
fluid backs up into systemic veins → peripheral edema