ADE - Antibody-dependent Enhancement and Immunopathology/Immunotherapy
1/15
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
16 Terms
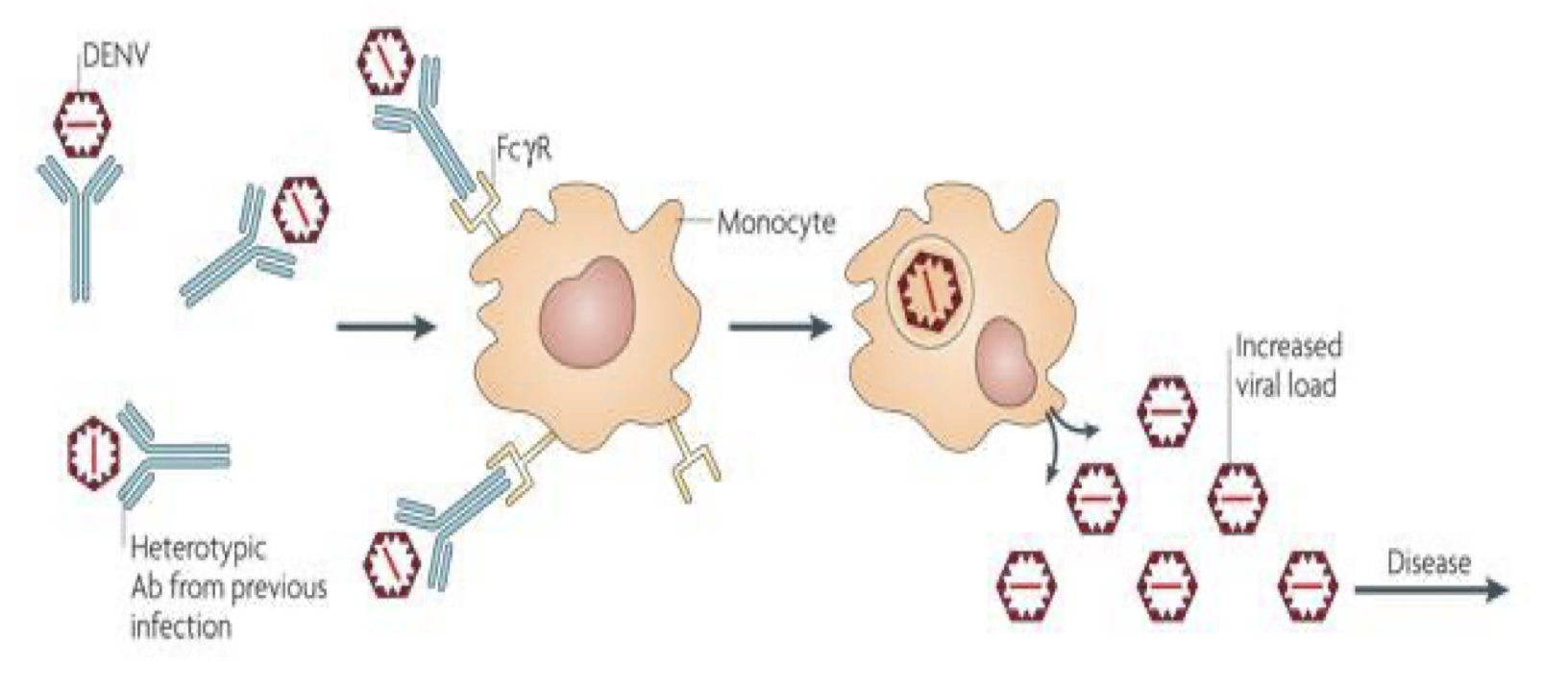
What is Antibody-dependent enhancement?
Certain pathogens induce strong immune responses but have
evolved strategies to escape killing
◼ Persistence of infection results from ability to survive
◼ Infection with a second serotype (different than the original) or a
different virus can worsen the course of the disease because of the
antibodies raised against the first serotype
◼ Bottom line strategy: “Antibodies as a Trojan horse” to generate a strong secondary infection (Fc receptors on the phagocytic cells interact with the Fc part of the antibodies)
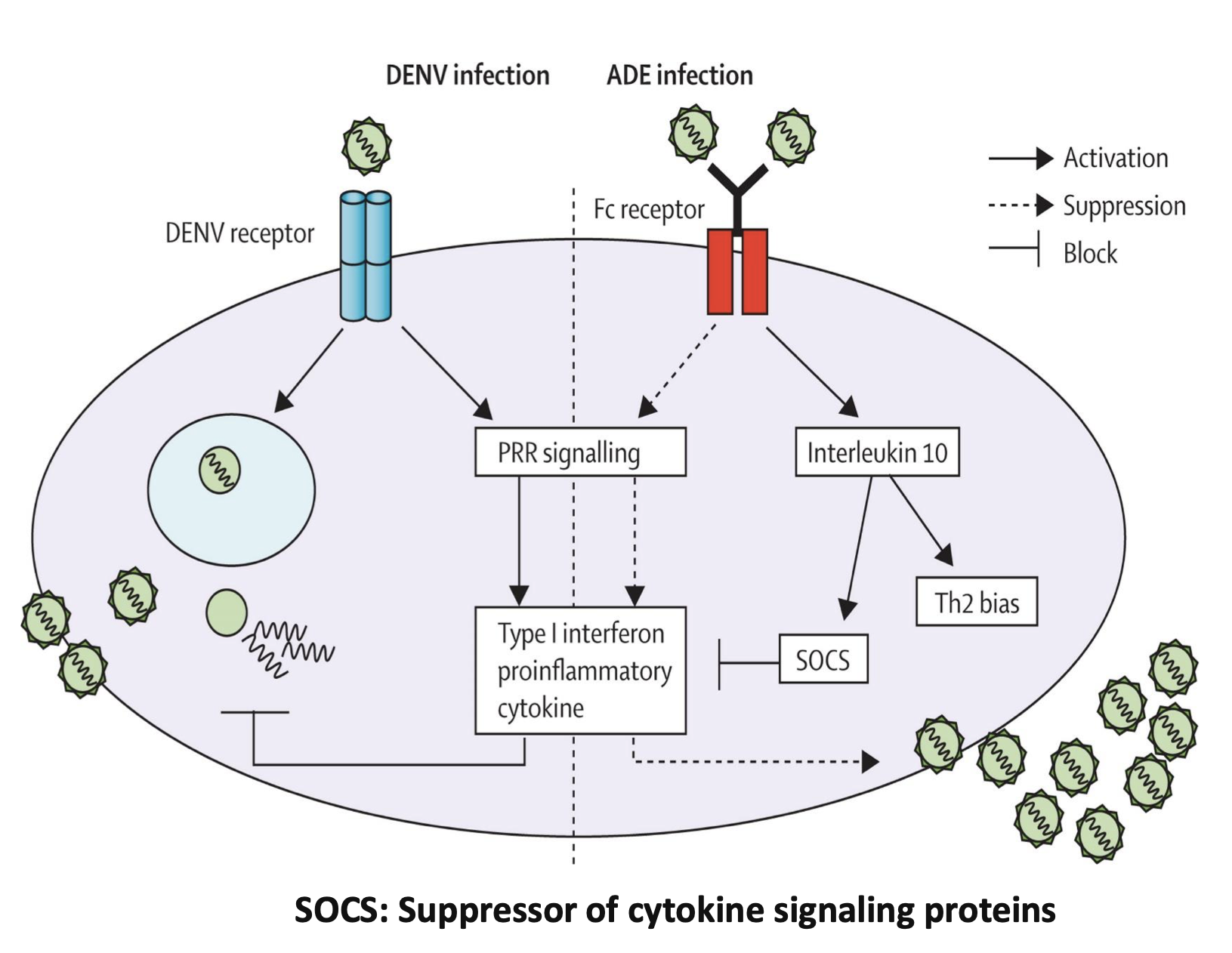
Explain infection with DENV and ADE.
DENV receptor activates PRR signalling which produces type 1 interferon proinflammatory cytokine which inhibits viral replication
For ADE infection
Fc receptor suppresses PRR signalling and inhibits type 1 interferon proinflammatory cytokine (with IL-10 +SOCS) and activates Th2 bias.
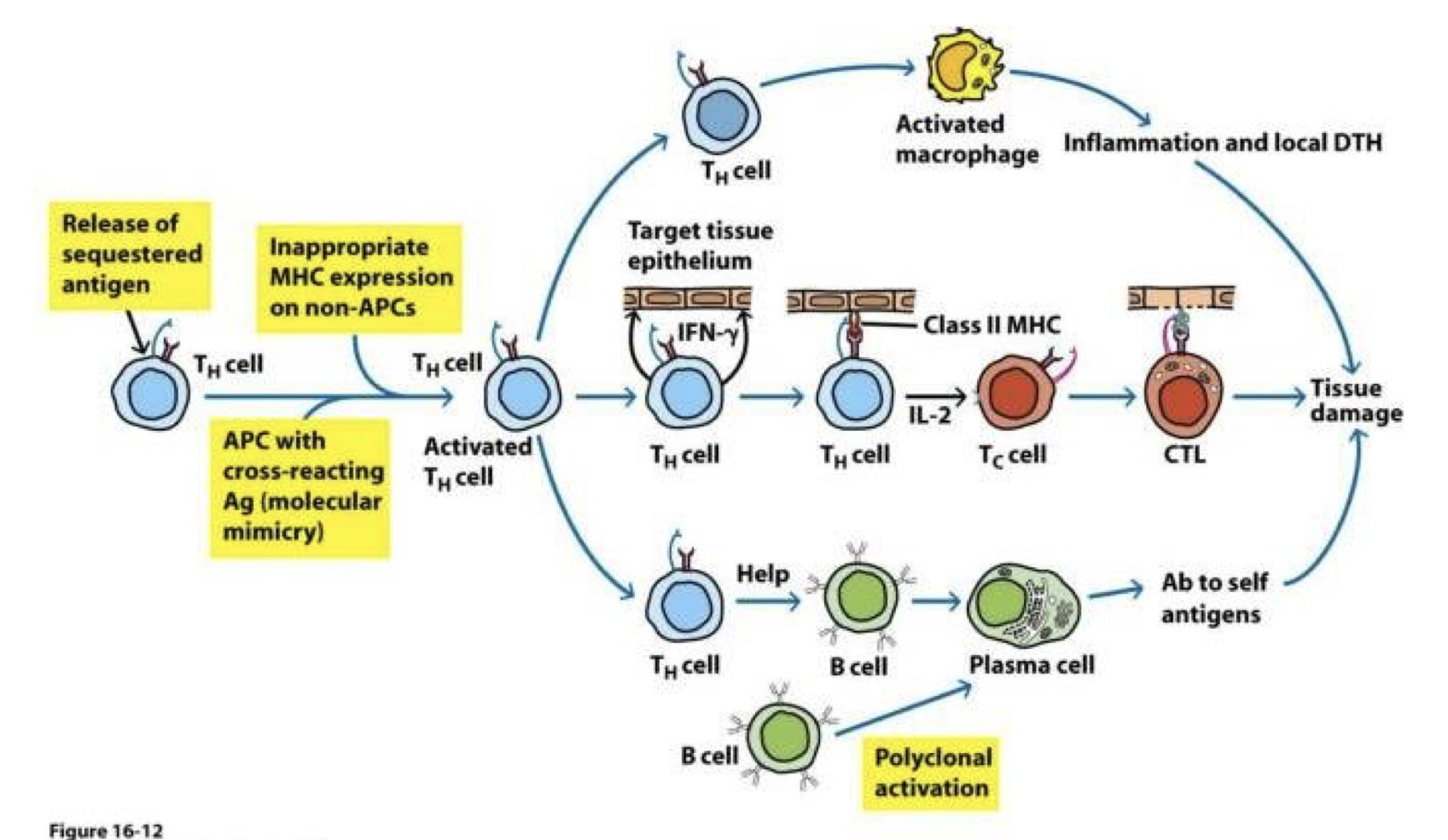
What is autoimmunity? Use a diagram to support your answer.
An inappropriate immune response
against a self antigen
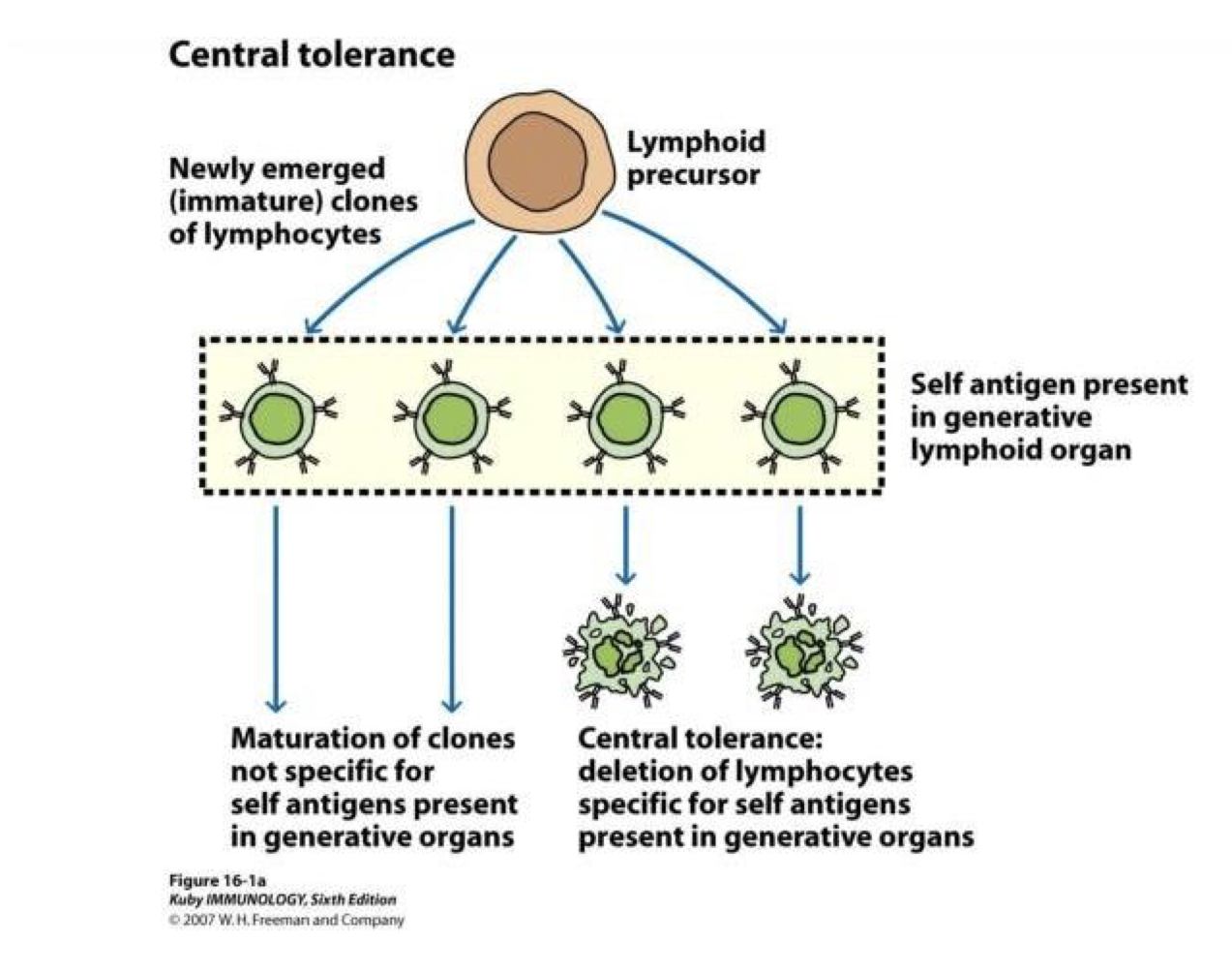
What is tolerance? Use a diagram to support your answer.
mechanisms that exist to
protect an individual from potentially
self-reactive lymphocytes
Explain how the foetus is an allograft?
Foetus is an allograft that is not rejected
Allograft - a tissue graft from a donor of the
same species as the recipient but not
genetically identical
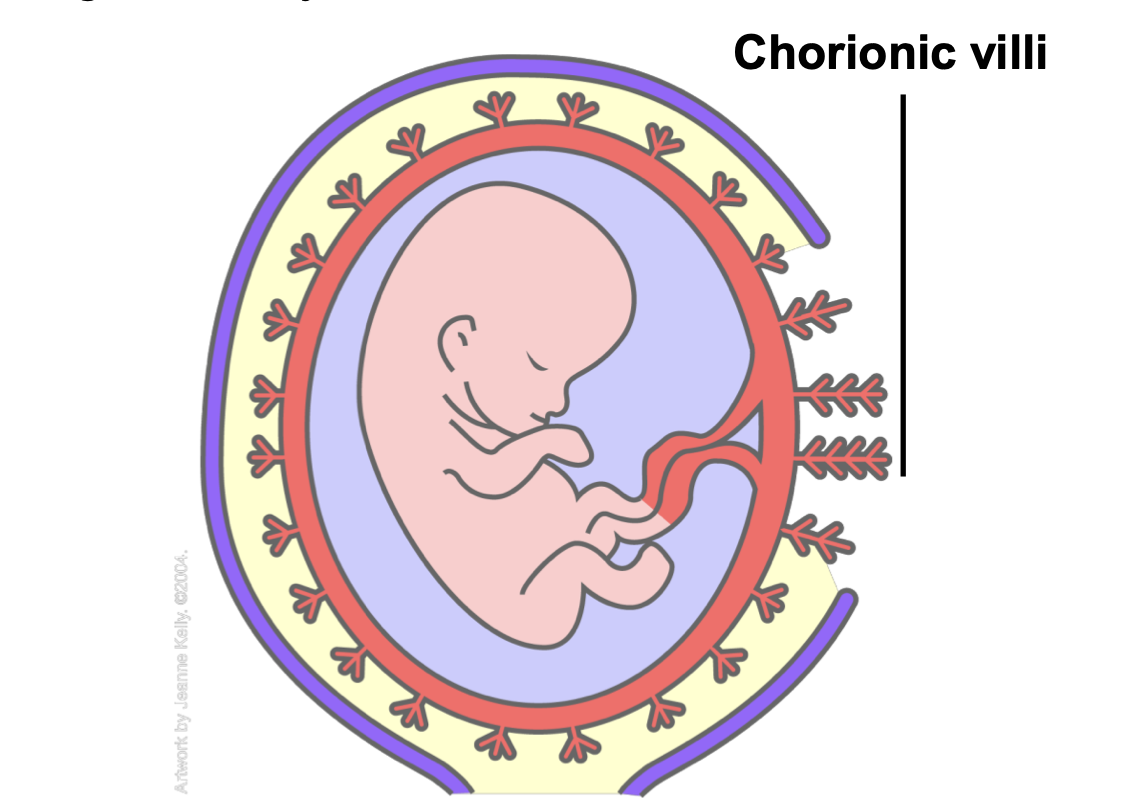
What is foetal tolerance?
Fetal tolerance refers to the unique immunological phenomenon in which the maternal immune system tolerates the presence of the semi-allogeneic fetus, allowing pregnancy to proceed without rejection. This tolerance is remarkable because the fetus expresses paternal antigens that are foreign to the maternal immune system, which under normal circumstances would trigger an immune response.
In foetal tolerance, describe immune privilege.
◼ Tolerance to the introduction of antigens without
eliciting an inflammatory immune response
◼ Tissue grafts are normally recognized as foreign
antigen by the body and attacked by the immune
system
Where are the immune privileged sites in allografts?
In immune privileged sites - tissue grafts can
survive for extended periods of time without
rejection occurring
◼ Immunologically privileged sites include
⚫ eyes
⚫ placenta and fetus
⚫ testicles
⚫ central nervous system
⚫ anagen hair follicle
What is hypersensitivity?
Hypersensitivity refers to exaggerated or inappropriate immune responses to harmless antigens, leading to tissue damage and clinical disease.
Explain type I hypersensitivity.
Mechanism:
• Caused by the activation of IgE antibodies and their interaction with mast cells and basophils.
• Upon initial exposure, the allergen induces IgE production by B cells. IgE binds to Fcε receptors on mast cells, sensitizing them.
• On subsequent exposure, the allergen cross-links IgE on mast cells, leading to degranulation and release of inflammatory mediators (e.g., histamine, leukotrienes, prostaglandins).
• Onset: Within minutes of allergen exposure.
• Examples:
• Allergic rhinitis (hay fever), asthma, anaphylaxis, food allergies, urticaria (hives).
What is an immunodeficiency?
Primary – a group of disorders
characterized by an inability to produce
a normal immune response (genetic)
Characterized by recurrent infections, high risk of autoimmune diseases, allergy and cancer
◼ Secondary – Abnormal immune
response caused by an external force
(acquired)
E.g. infection, tumour, medications, etc.
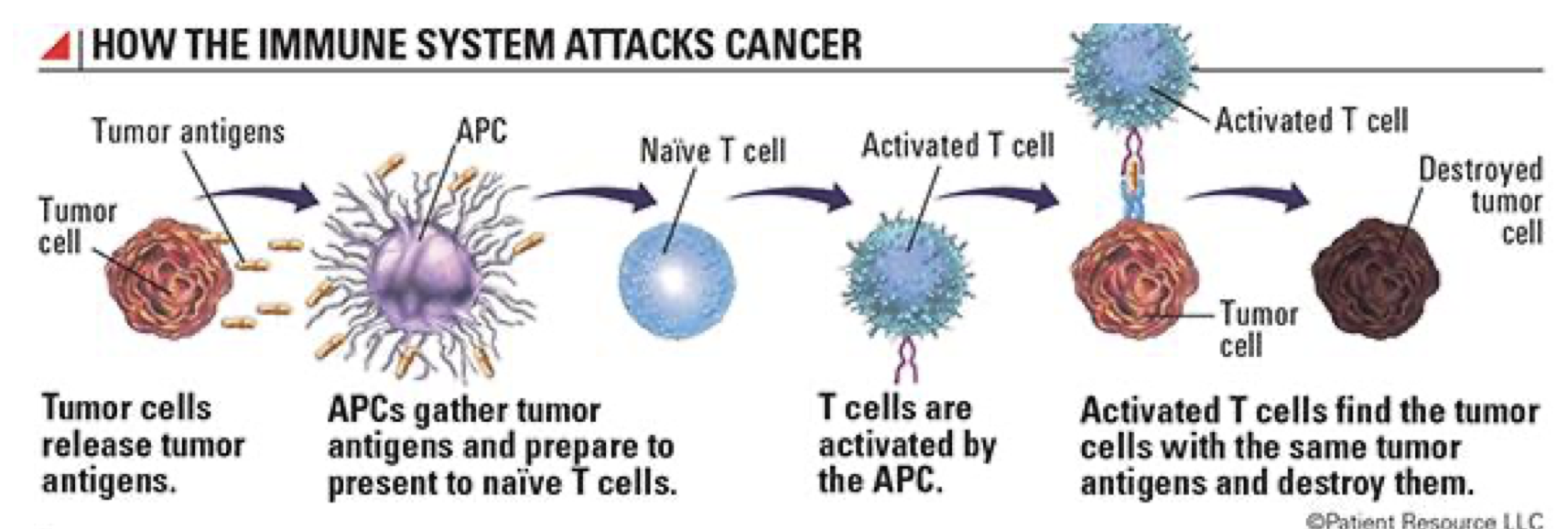
Describe cancer’s role in immunopathology. Use a diagram to support your answer.
Results from a lack of immune surveillance
◼ Cells or secreted molecules can
Induce CTL apoptosis
Suppress CD8+ T cell-mediated immunity
Cause immune exhaustion
Downregulate molecules involved in T cell activation
What is immunetherapy?
Immunotherapy is a medical treatment that harnesses and modifies the immune system to fight diseases, particularly cancer, autoimmune conditions, and allergies. It involves enhancing, suppressing, or manipulating immune responses to achieve therapeutic goals.
What is cancer immunotherapy? Give two examples
Cancer Immunotherapy
• Designed to stimulate the immune system to recognize and destroy cancer cells.
Examples:
• Checkpoint Inhibitors:
• Drugs like nivolumab or pembrolizumab block immune checkpoints (e.g., PD-1/PD-L1 or CTLA-4) that suppress T-cell activity, reactivating the immune system against cancer.
• CAR-T Cell Therapy:
• T cells are engineered to express chimeric antigen receptors (CARs) that specifically target cancer antigens. These cells are reinfused into the patient to attack tumors.
What is a type of immunotherapy for autoimmunity? Give two examples
Autoimmune Disease Immunotherapy
• Suppresses the immune system to prevent it from attacking self-tissues.
Examples:
• Biologic Drugs:
• TNF inhibitors (e.g., infliximab) for rheumatoid arthritis and Crohn’s disease.
• IL-17 inhibitors for psoriasis.
• Immune Cell Depletion:
• Rituximab targets CD20 on B cells in diseases like lupus or multiple sclerosis.
Illustrate hypersensitivity immunotherapy.