Pulm. Structure and Mechanics
1/88
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
89 Terms
Non-respiratory functions of respiratory systems
water loss and heat elim.
enhances venous return
speech
defends against foreign matter
removes/inactivates various materials in pulm. circulation
nose = organ of smell
Cellular respiration is mainly carried out by what organelle?
e.g. krebs cycle, ETC
intracellular metabolic processes carried out within the mitochondria
use O2 and produce CO2
4 steps of external respiration
1. ventilation into and out of alveoli
2. exchange of air in the alveoli and blood
3. blood transport between lungs and tissues
4. exchange between tissues and blood
What is the conducting zone?
from the nose to the terminal bronchioles and alveoli
responsible for bringing air into the respiratory zone (=alveoli surrounded by pulmonary capillaries)
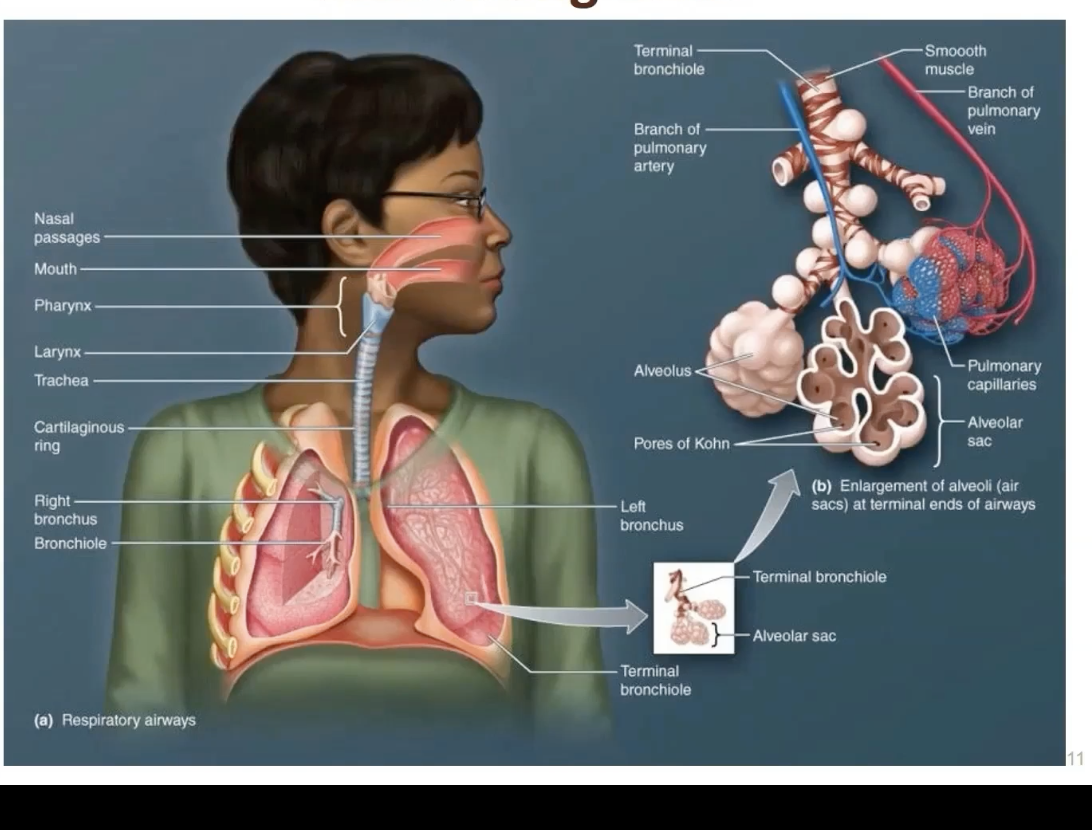
What do epithelial cells in the conducting airway secrete for protection? (within the mucous)
molecules that act as antimicrobials
chemokines, cytokines
As you go from trachea to alveoli, the sectional area increases or decreases?
increases
(velocity slows)
What keeps the conducting zone open?
cartilaginous rings encircling the trachea and bronchi
What are the effects of the autonomic nervous system on the tonic smooth muscle in the terminal bronchioles?
ParaS: contraction (ACh→bronchoconstriction via M3 muscarinic receptors)
Symp: relaxation/dilation (norepi→bronchial-dilation (b2 adrenergic receptors)
small particles that enter the upper airways can initiate what reflex?
initiate the cough reflex (bronchial constriction and coughing)
Small particles that enter the upper airways are moved away from the lungs by…?
either coughing, or the "mucociliary escalator"
What is the musociliary escalator?
ciliated epithelium bathed in a periciliary fluid (submucosal glands) that push material back up, which then gets swallowed
Why may ciliary motility be defective? What can this lead to?
SMOKING
environmental factors
genetic deficiencies
leads to:
chronic sinusistis,
recurrent lung infections and
bronchiectasis (damaged bronchial tubes)
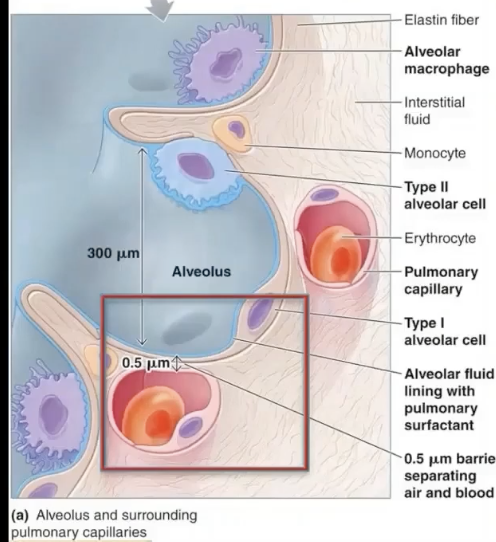
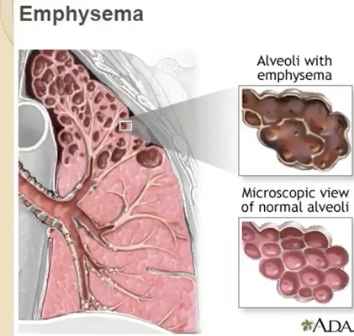
Where is the pulmonary interface? What is it also called?
the small interstitial space between the alveoli and the surrounding pulmonary capillary
aka = air blood barrier
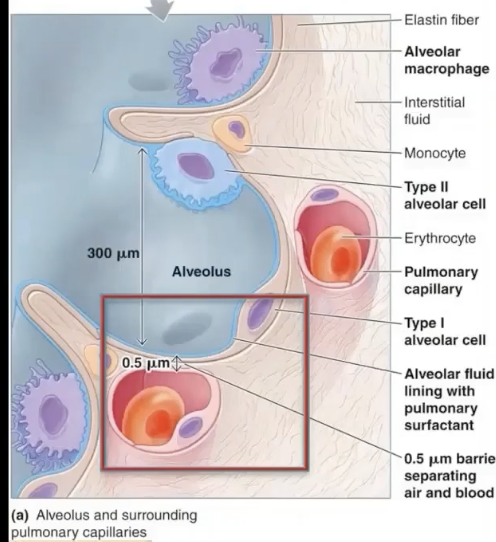
How do the structures of the air-blood barrier connect?
The thin basement membranes of alveolar cells are fused with the endothelial cell of the pulmonary capillary
What are type I alveolar cells?
simple squamous cells where gas exchange occurs
Extremely thin and squamous — optimized for gas diffusion.
Cover about 95% of the alveolar surface area, even though they make up only ~40% of the total alveolar cells (type II cells are more numerous but smaller).
Connected to each other by tight junctions to prevent fluid leakage into the alveolar space.
Function
Form the respiratory surface of the alveoli — the blood–air barrier — along with the capillary endothelial cells and their shared basement membrane.
Their thinness allows for efficient diffusion of oxygen and carbon dioxide between alveolar air and blood.
Role and Function of type II alveolar cells
1. Secretion of Pulmonary Surfactant
Surfactant reduces alveolar surface tension, preventing alveoli from collapsing during exhalation (atelectasis).
Helps maintain alveolar stability so small alveoli don’t collapse into larger ones.
(Surfactant production begins late in fetal development — that’s why premature infants can develop respiratory distress syndrome (RDS) due to surfactant deficiency)
2. Secretion of antimicrobial proteins and cytokines
They also secrete antimicrobial proteins and cytokines, contributing to the innate immune defense of the lung.
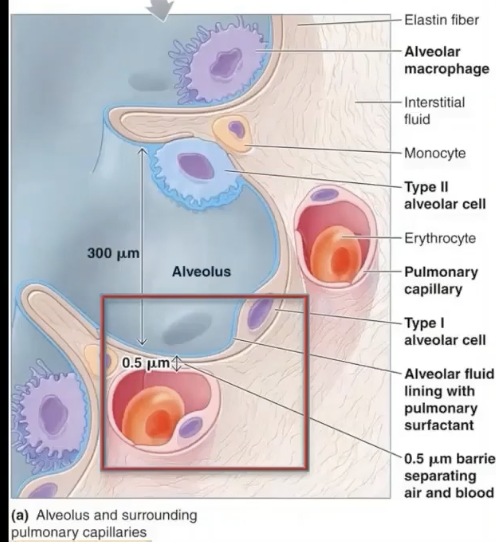
What cells help to guard/protect alveoli from infections, toxic, or allergic particles within the alveoli?
alveolar macrophages
External respiration steps
air is moved in and out of lungs so exchange can occur btwn atmosphere and alveoli (done by ventilation)
o2 and co2 are exchanged by diffusion for transport by the blood
blood transports the gasses
gas exchange between cells and blood
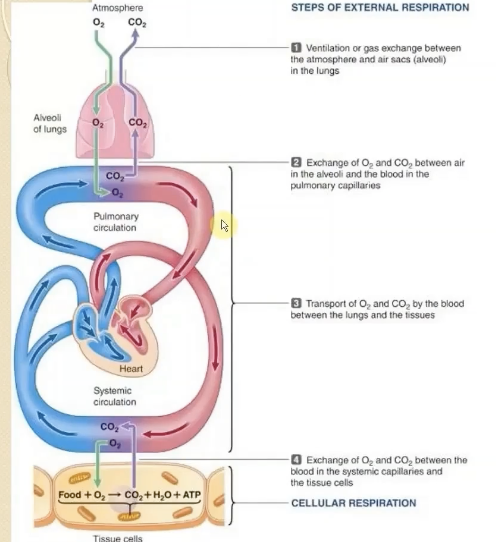
In external respiration the respiratory system is only involved with
1. ventilation
2. exchange of O2 and CO2 between the lungs and the blood
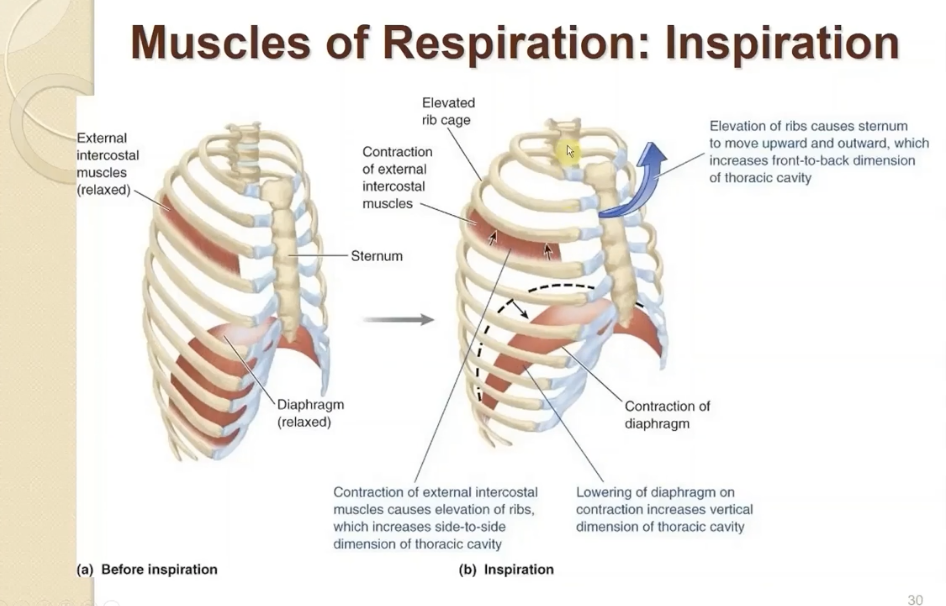
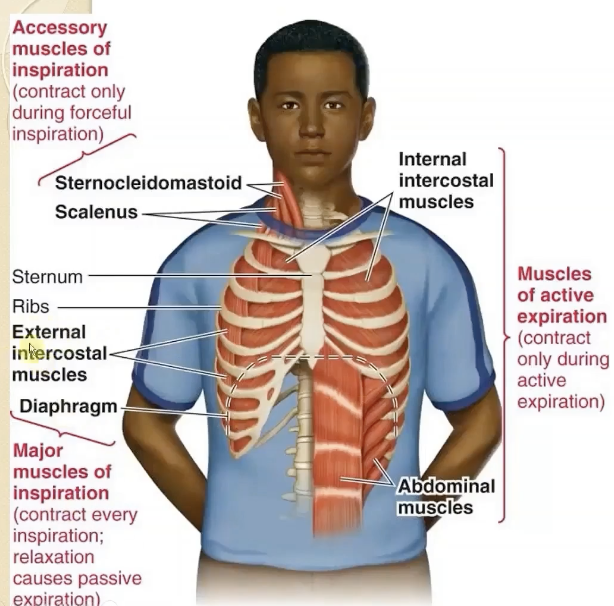
Major muscles of inspiration
diaphragm
external intercostals
During quiet breathing, what muscles are responsible for expiration?
relaxation of active inspiratory muscles:
diaphragm
external intercostals
decrease in lung volume raises the inner pressure, pushing air out.
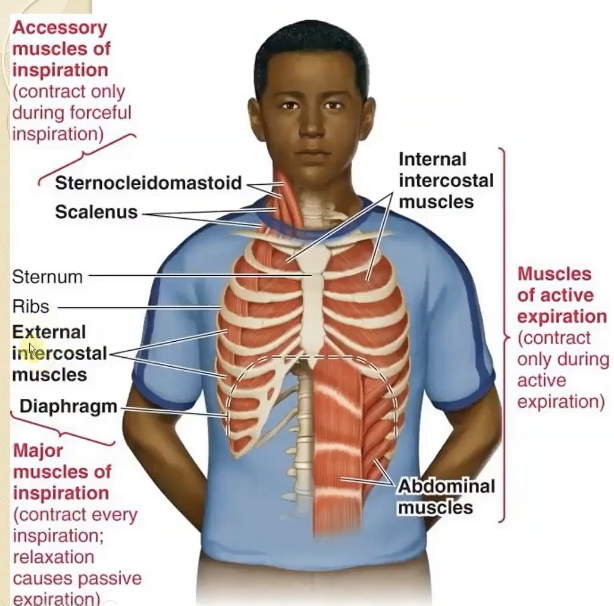
What are the muscles of active expiration?
contract only during active expiration
abdominals
internal intercostal muscles (contract and depress rib cage)
how does contraction of muscles of inspiration bring air into the lungs?
contraction increases thoracic volume → decreases intrapulmonary pressure
(stretch of lungs, inside lungs pressure decreases, bringing air into the lungs)
Boyle's Law in respiration
Boyle’s Law explains that ventilation is driven by pressure changes caused by volume changes in the thoracic cavity.
P1V1=P2V2
Boyle's Law in the respiratory system
To bring air into the lungs:
intra-alveolar pressure < atmospheric pressure
For expiration:
intra-alveolar pressure > atmospheric pressure
Boyle’s Law explains that ventilation is driven by pressure changes caused by volume changes in the thoracic cavity.
What is the thin fluid-filled space between the two pulmonary pleurae membranes?
the Pleural cavity (pleural sac)
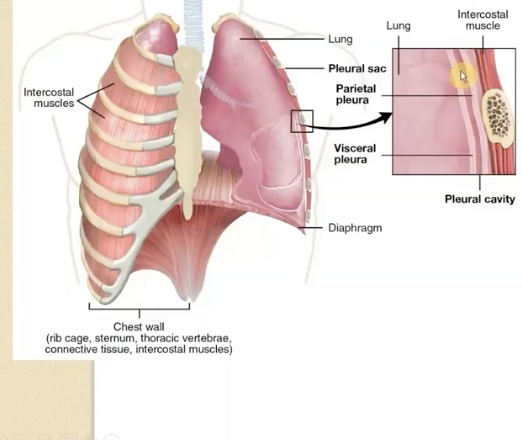
visceral pleura
covers the lungs
parietal pleura
covers the inner surface of the thoracic cavity
Pleurisy
inflammation of the pleura accompanied by painful breathing due to friction of inflamed tissue
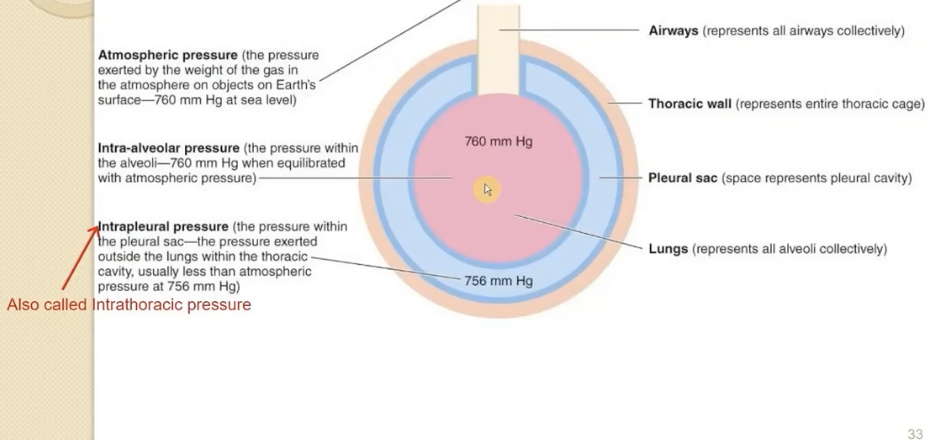
atmospheric pressure
pressure exerted by the weight of the gas in the atm on objects on earth’s surface
760 mmHg (29.92 inHg)
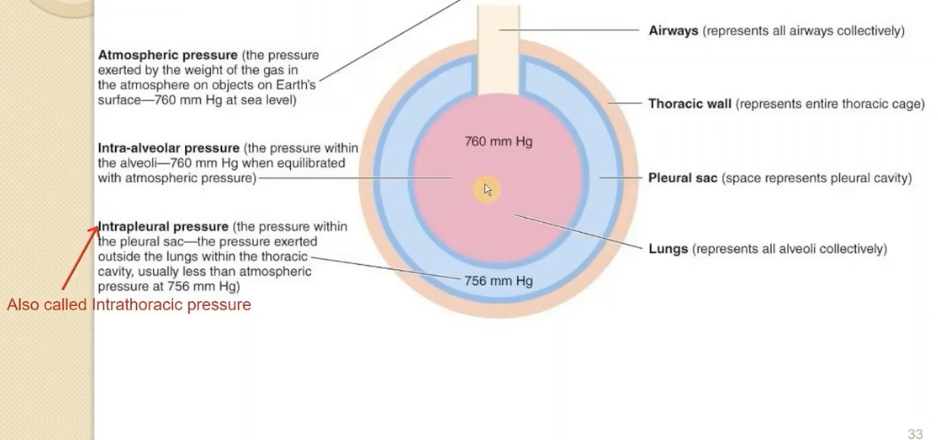
intra-alveolar pressure
pressure within the alveoli
760 mmHg (29.92 inHg)
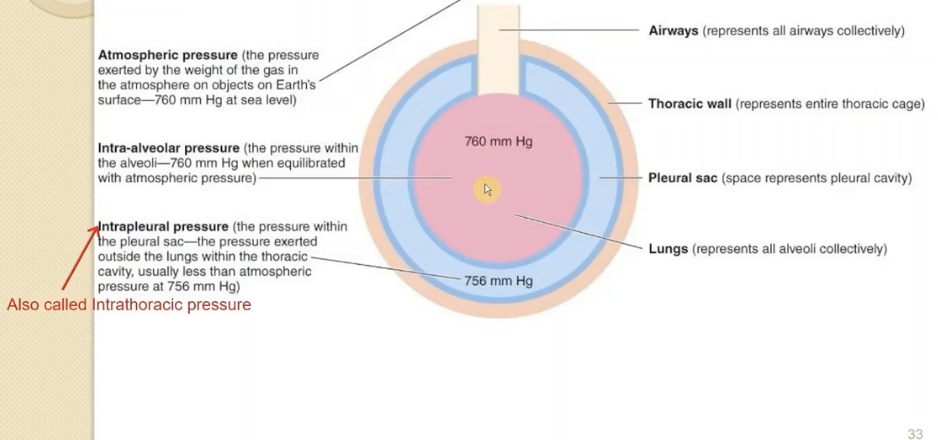
intrapleural (intrathoracic) pressure
pressure within the pleural sac (pressure exerted outside the lungs, but within the thoracic cavity)
pulls lungs against inside thoracic cage.
will always be slightly less than the atm or intra-alveoili pressure
756 mmHg
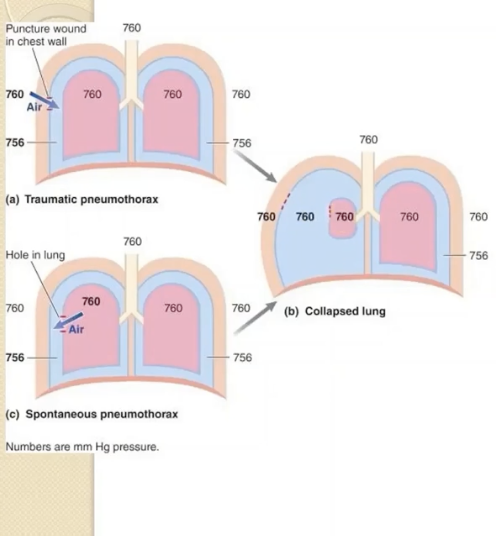
Why does a pneumothorax cause a lung to collapse?
the intrapleural and intra-alveolar pressure are now equal with atmospheric pressure
no longer any pressure holding the lung to the thoracic cage (pleural cavity no longer has that negative pressure)
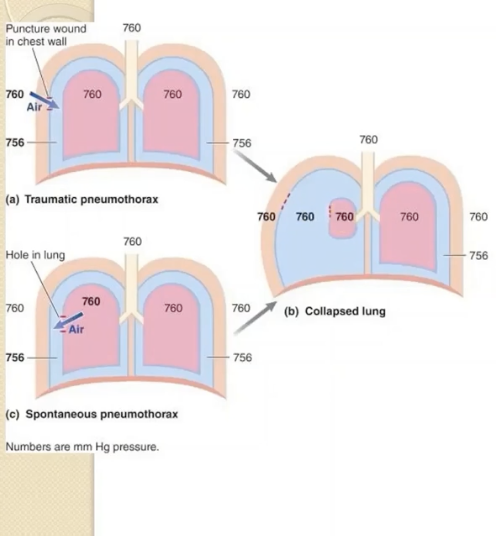
What happens to the thoracic wall when you get a pneumothorax?
it springs outward
less serious than the collapsed lung
Spirometry measures
diagnostic tool to evaluate lung diseases:
the volume of air entering or leaving the lungs
Maximal and minimal lung volumes of healthy YA
Maximum:
5.7 L in males
4.2 L in females
Minimum:
1.2 L
During normal breathing: varies between 2.7L and 2.2 L
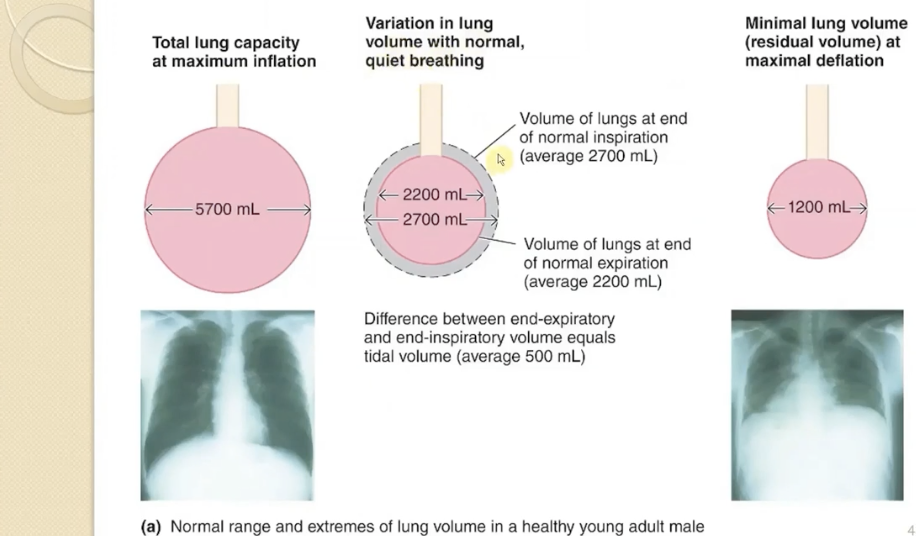
Residual volume of the lungs
Minimum volume the lungs can hold
1.2 L
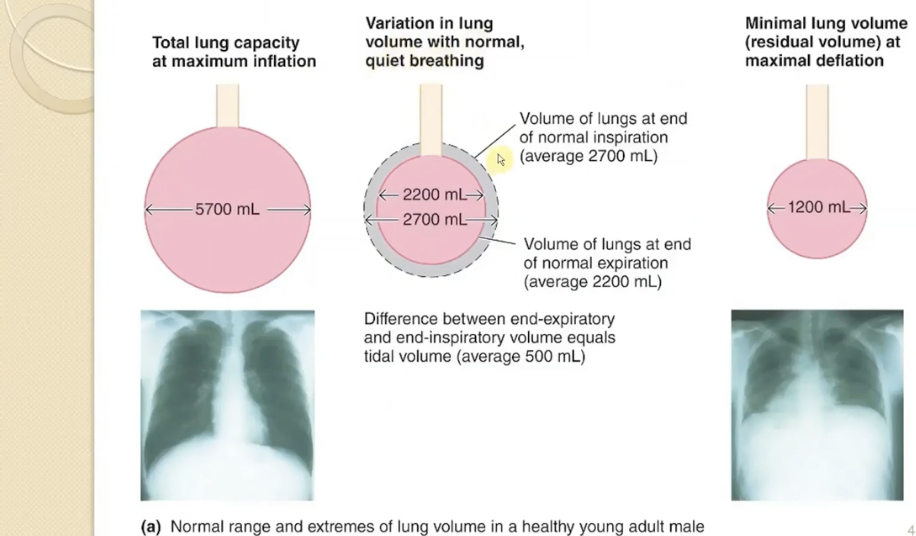
Functional residual capacity of lungs
(air left in lung at the end of normal quiet expiration)
2200mL (2.2L)
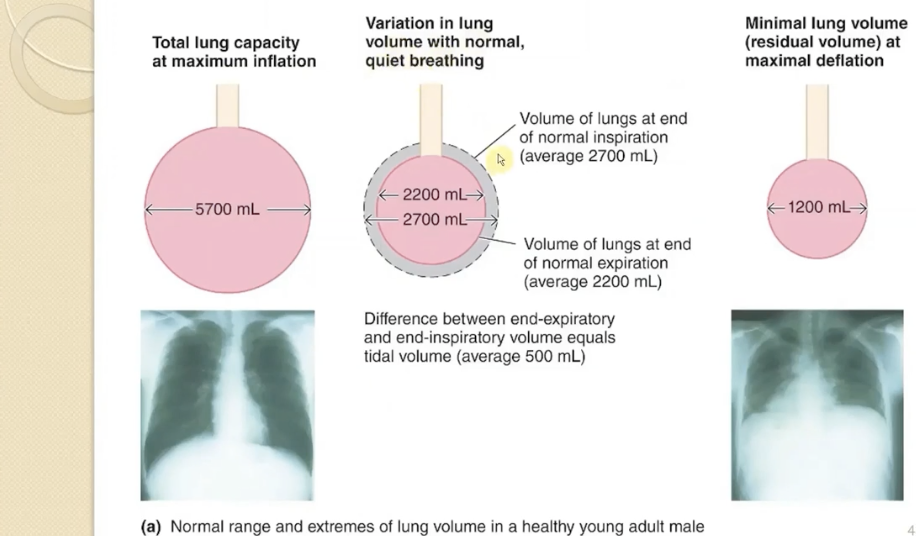
in normal breathing how much air is inspired and expired? What is the volume called?
500mL
(tidal volume)
during max expiration lung volume can decrease to
1200mL (residual volume)
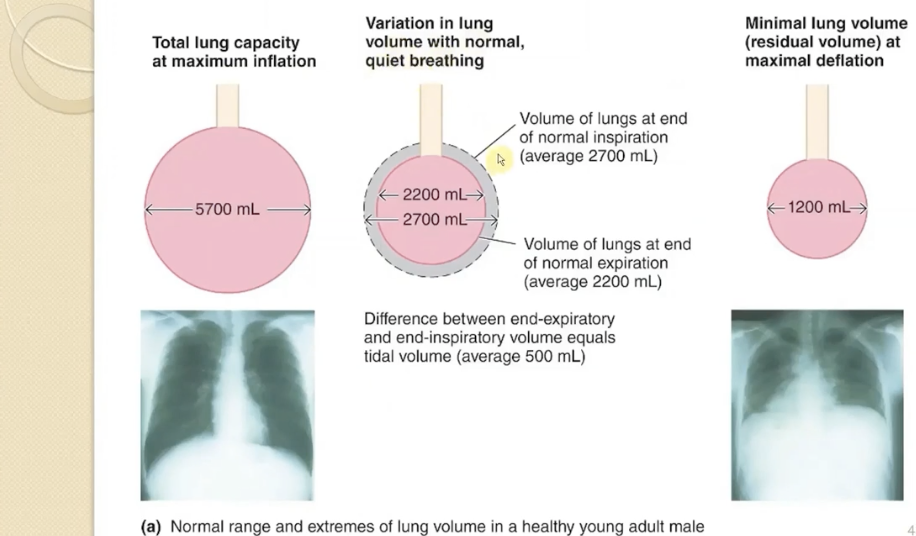
why can the lungs never fully deflate?
the small airways collapse, which traps air into the airways (residual volume is 1.2L)
Tidal Volume (TV)
volume of air entering or leaving the lungs under normal resting conditions (~500mL)
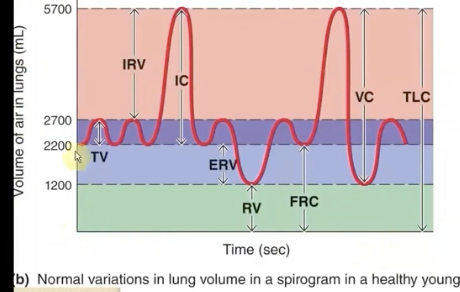
Inspiratory Reserve Volume (IRV)
volume of additional air that can be forcibly inhaled after a normal inhalation (~3000mL)
max contraction of ext intercostal and diaphragm
can bring in 3 extra L
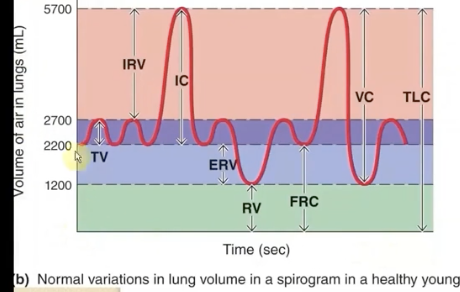
Expiratory Reserve Volume (ERV)
the volume of additional air that can be forcibly exhaled after a normal exhalation (~1000mL)
can push out extra 1L with max contraction of expiratory muscles
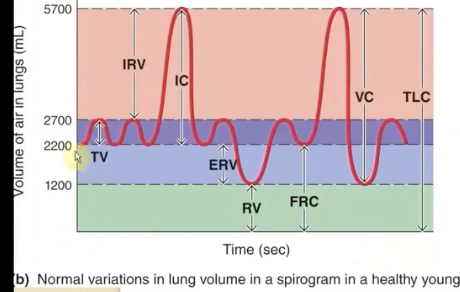
Residual Volume (RV)
volume of air remaining after max force expiration (can’t be expelled)
usually about 1L
Inspiratory Capacity (IC)
after you normally exhale, it’s the max amount that you can inhale
(TV+IRV= 3.5L)
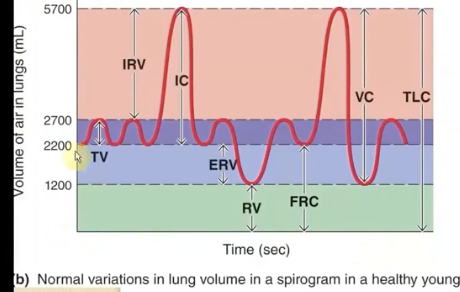
Functional Residual Capacity (FRC)
volume of air remaining in the lungs after a normal passive (tidal volume) expiration
(ERV+RV= 2200mL)
forcibly exhale then → air you breathed out plus the air you cannot get rid of
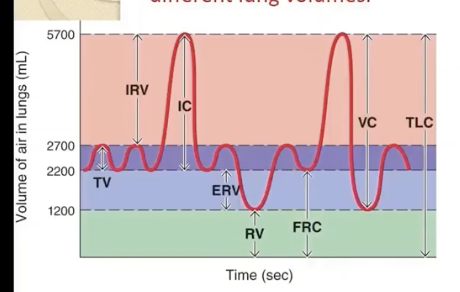
Vital Capacity (VC)
Maximum volume of air that can be exhaled after a maximum inhalation
(IRV+TV+ERV = 4500mL)
breathe all the way in (IRV) and then exhale everything you can (ERV)
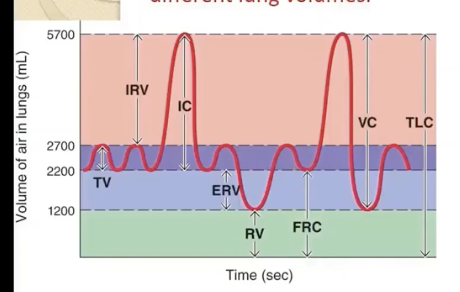
Total Lung Capacity (TLC)
maximum amount of air that the lungs can hold
(VC+RV= 5700mL)
everything you can possibly exhale + the reserve amount that’s always in there
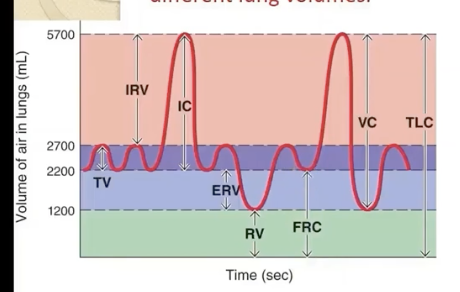
pulmonary ventilation =
tidal volume x respiratory rate
PV at rest = 500mL/breath x 12 breaths/min = 6L/min
Anatomic dead space volume (VD)
inspired air that does not reach the alveoli conducting airways (~150mL)
alveolar ventilation =
atm air that actually reaches the alveoli. more important than pulmonary ventilation.
(tidal volume - dead space) x respiratory rate
Why is shallow, rapid breathing not effective?
You really only end up inhaling air to fill the dead space (conducting space), so no air is actually reaching your alveoli. your AV is zero, but PV would be higher.
lung compliance
distensibility/stretchibility of the lungs
(∆V/∆Ptp)
ease of which lungs can be expanded under pressure. should be very compliant to make inspiration easy. not too compliant, airway would collapse during active expiration → trapped air
lung elasticity
the tendency of the elastin fibers to return to their original position away from the chest wall after being stretched
depends on the amount of elastin fibers in the l ungs and the alveolar surface tension. mostly due to the thin layer of fluid coating alveoli cells.
If lungs were too elastic, that would make inspiration more easy/difficult?
more difficult, it would require more work to expand the lungs
An object with high compliance and low elasticity would be ___ to stretch?
easy
An object with low compliance and high elasticity would be ___ to stretch?
hard to stretch
Pulmonary fibrosis: what is she? what causes her? how does she work?
commonly seen in coal miners with black lung disease
DECREASES LUNG COMPLIANCE (tendency to stretch)
INCREASES LUNG ELASTICITY
→ smaller lung volume → less air enters → lungs can not expand as well
increases the amount of work to bring air in
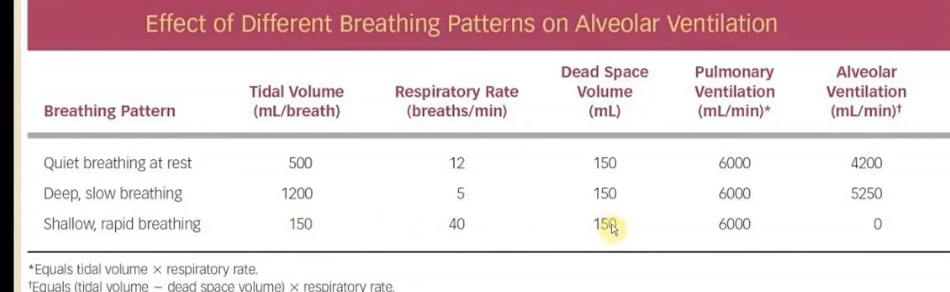
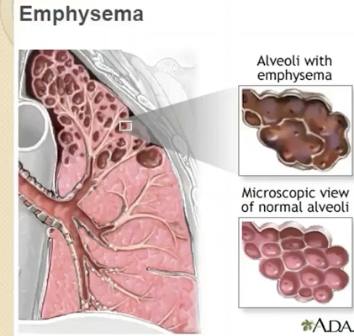
chronic obstructive pulmonary disease (COPD)
a group of lung diseases characterized by increased airway resistance from narrowing of lower airways
→ chronic bronchitis and emphysema
COPD bronchitis
inflammatory response:
airways narrowed due to prolonged thickening from long term exposure to irritants
edematous thickening of airway linings, overproduction of thick mucous, mucous escalator is immobilized
why are pulmonary bacterial infections so common in COPD bronchitis?
accumulated mucus is excellent medium for bacterial growth
COPD Emphysema: etiology? what is she?
characterized by collapse of the smaller airways and breakdown of alveolar walls
increase in TLC, FRV, and RV.
gas exchange is then compromised bc the functional area for gas exchange is reduced and air is trapped during expiration
commonly caused by: excessive release of trypsin enzyme from alveolar macrophages as a defense mechanisms in response to chronic exposure to inhaled smoke or irritants
elastic recoil is decreased.
COPD ephysema pts have difficulty with what? why?
decrease in elastic recoil, increased air resistance (excess mucus) → difficulty with expiration.
the lungs are more compliant and less elastic. when they breathe out, the airways collapse and trap alveolar air.
Forced Expiratory Volume in 1 sec (FEV1)
volume of air that can be expired during the first second of expiration in a force vital capacity
FEV/FVC
take deep breathe in, then push as hard and fast as u can out
indicates maximum airflow rate possible from the lungs
Normal FEV1/FVC ratio
80% (of air can be expired from the lungs in one second)
FEV1/FVC ratio in emphysema
< 80%
FVC is lower than normal
is obstructive disease
(increase in compliance. can not expel air well bc the airway is collapsing)
FEV1/FVC ratio in fibrosis
>80%
FVC is lower. the lung is restricted from filling to normal capacity.
is restrictive disease
(lung is too stiff, it is hard to inspire, a lot of elasticity)
Asthma: what is she? what’s going on there?
Transiemt, not chronic
inflammation and histamine-induced edema → excessive secretion of thick mucus → airway is plugged/obstructed
Airway smooth muscle hyperresponsiveness: trigger (allergens, irritants) → spasm of smooth airway → increased airway resistance → LARGE constriction of smaller airways
how much of the body's total energy is used for quiet breathing?
~3%
the work of breathing may be increase in what four situations?
1. increased airway resistance (COPD)
2. decreased compliance (fibrosis)
3. decreased elastic recoil (empphysema)
4. increased need for ventilation (exercise)
alveolar surface tension
thin film of surfactant normally lining each alveolus.
forces btwn wooder molecules resists any force that tries to increase its surface area (surface tension) so it will oppose expansion of alveolus.
this is the driving force behind the lungs’ elastic recoil, along with elastin fibers
what is lung surfactant
secreted by type II pneumocytes
these molecules coat the internal surface of alveoli, reducing surface tension of alveolar fluid.
how does surfactant reduce the work of respiratory muscles?
increase compliance (makes it easier to inflate the lungs) and stabilize alveolar size during ventilation
Why are infants born prematurely at an increased risk of developing respiratory distress syndrome (RDS)?
They lack sufficient surfactant because type II alveolar pneumocytes have not matured
this makes breathing much harder
How can you support infants experiencing RDS?
mechanical ventilators and exogenous surfactants to support the infants until type II cells mature
Dalton's Law of Partial Pressures
total pressure exerted by mixture of gases is equal to sum of partial pressures of the individual gasses
PO2 in atmosphere
160 mmHg
partial pressure of atmospheric air
760mmHg
partial pressure of carbon dioxide in atmosphere
0.2mmHg
What happens to the partial pressures of gasses as you inspire?
within the dead space, you are humidifying inhaled air with wooder vapor.
this wooder vapor is a gas wiht a partial pressure of its own, which will influence the partial pressures of everything you inhale.
the partial pressure of the gasses you inhale will decrease to make room for the partial pressure of wooder vapor in the dead space as it enters the lungs.
Why does the oxygen partial pressure decrease drastically within the alveoli (especially compared to atmospheric oxygen partial pressure)?
alveoli is being perfused with blood thats returning with a WAY lower partial pressure of oxygen.
additionally, the partial pressure of this incoming blood is much higher than what is out in the dead space (essentially zero)
gas exchange!
How is it that the partial pressure of oxygen and carbon dioxide stay at a constant 100 and 40 in the alveoli during inspiration and expiration?
the constant perfusion of blood going on around the alveoli (reduced o2, increased co2) will quickly equilibriate with the inhaled gasses
o2 is constantly being diffused into arterial blood.
Capillary Reserve Time: what is she? allows for?
takes 1/3 of the length of a cpaillary for the blood to equilibrate for partial pressure of o2 and co2
even when flow rate is high, there is still plenty of time fro gas exchange to occur when it is flowing very quickly
accommodates
gases diffuse from alveoli to the blood
sufficient gas exchange when cardiac output increases → less time that blood spends in capillary, but there is plenty of reserve → even at high cardiac output, you’ll still reach equilibirum very quickly
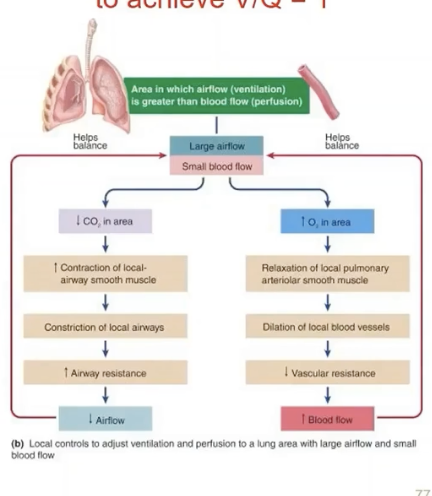
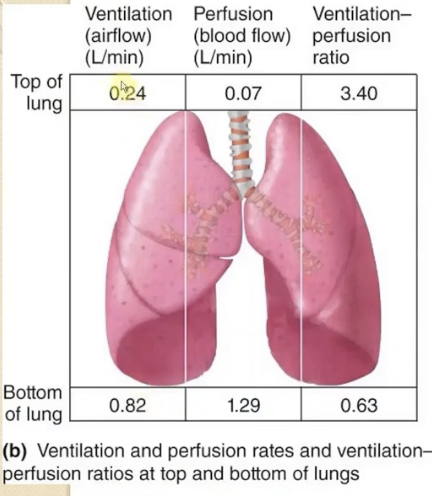
ventilation to perfusion ratio
should be equal to one
ventilate alveoli needs ot match the blood flow
not always perfect, not all alveoli are equally ventilated or equally perfused by blood. especially when standing upright
ventilation-perfusion ratio when standing
ventilation and perfusion is increased in the bottom of the lung. perfusion increases more. this is due to gravity.
top of lung: more ventilation than perfusion (V/P > 1)
bottom of lung: more perfusion than ventilation (V/P < 1)
Bronchiolar smooth muscle: what is she sensitive to changes in? how does she change to help with V/P when standing or in a suboptimal position?
the radius of arterioles and bronchioles supplying alveoli can be changed.
bronchiolar smooth muscle: sensitive to CO2 changes
increased CO2 levels = dilation
decreased CO2 = constriction
increases ventilation to a poorly ventilated area
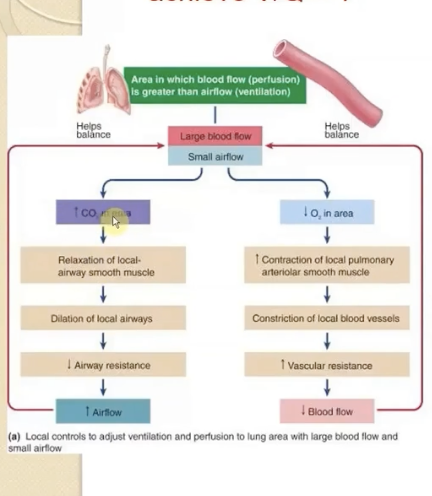
Pulmonary arteriolar smooth muscle: what is she sensitive to changes in? how does she change to help with V/P when standing or in a suboptimal position?
pulmonary arterioles: sensitive to O2 changes (opposite direction of systemic arteriolar smooth muscle)
increased O2 levels = dilation (higher blood flow)
decreased O2 levels = constriction (lower blood flow)
increases blood flow to well-ventilated alveoli