sseps
1/62
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
63 Terms
SSEPs
electrical activity in response to touch; give info on proprioception and vibration sensations
What do SSEPs monitor?
- individual extremities for positioning effects
-dorsal column of spinal cord
- Brainstem and cerebral cortex
SSEPpathway
- ascending/afferent
- peripheral stimulation; cortical recording
- UN or MN and PTN or peroneal N or popliteal fossa
Where are the synapses of the DCML Pathway?
1. nucleus cuneatus/gracillis in MEDULLA OBLONGATA
2. Thalamus
3. Primary somatosensory cortex
Where does decussation/crossover happen?
- Medial lemniscus pathway in thalamus
- Pyramids in thalamus
Where does decussation/crossover happen?
- Medial lemniscus pathway in medulla oblongata
- Pyramids in the medulla-spinal cord junction in medulla oblongata
Fasiculus Cuneatus
upper extremities
Enters at T6 and up
Lateral distr. in dorsal column
Fasciculus Gracilis
lower extremities
Medial distr. in dorsal column
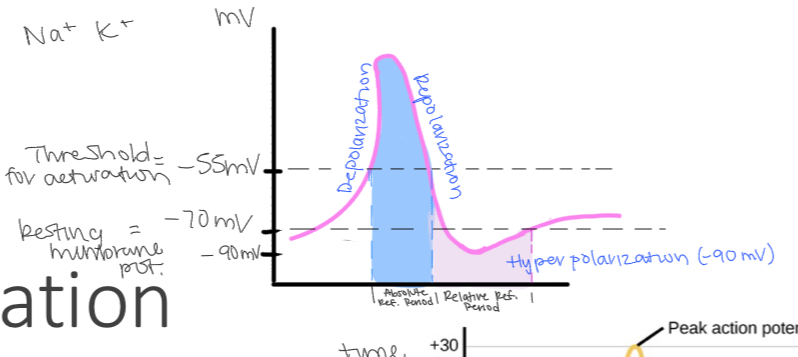
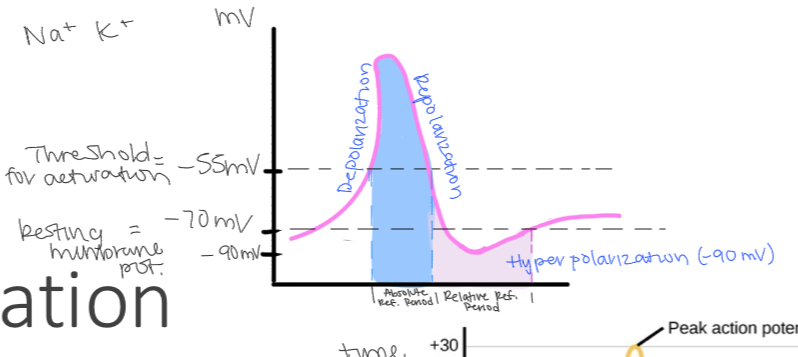
What is a neurons resting potential?
-70 my
What substance does neuron contain more and less of?
More potassium inside, more sodium outside
Relative Refractory Period
Period after absolute refractory period where AP reaches hyperpolarization and begins to return back to its resting potential
doesn’t include period where its back to resting potential
SSEP Stimulation electrodes called..
Anode (+) - where hyperpolarization occurs
Cathode (-) - where depolarization occurs
Cathodal Stimulation
Anions flow from cathode into tissue and back to anode
Absolute Refractory Period
Period from start of AP to return to below threshold
Comes before refractory period
Starts AP therefore NO other AP can be started during this period
How should you place electrodes for cathodal stimulation
Anode > cathode > recording electrode
cathode is proximal
Anode is distal
“The black (-) cat goes up the tree”
Anodal Blocking
Anode is more proximal than cathode, causing the blockage of ascending sensory signals from traveling up
SSEP stimulation units
Milliamperes (mA)
What distance should anode and cathode be? What happens if they’re too far or too close?
2-3 cm
Too close = small amplitudes bc current penetration very deep
Too far = increased in resistance therefore increase in stimulus artifact
Ohm’s Law
voltage (v) = current (i) x resistance (R)
Voltage = electrical force needed to drive electrical current
Resistance = opposition to current flow
Increased distance = increased resistance to current
Current remains constant - constant current stimulation
Factors that increase resistance
increased distance between anode and cathode
Flaky/oily skin (skin quality)
Contact impedance (electrode contact)
Factors that increase voltage
increased resistance
Increased current
Polarity Types
Normal - cathode is stimulating electrode and is proximal
For SSEPS
Reverse - anode and cathode switched at stimulating unit
Now anode stimulates
For TOF
Biphasic - switches anode and cathode over and over
Neutralizes voltage at cost of lower amplitude
Decreases stim artifact
Stimulating Ulnar N
Anode (+): 2-3 cm above wrist
cathode (-): medial to palmaris longus; 2-3 cm above anode
Alt site: medial epicondyle of humerus
Stimulating Medial N
Cathode: 2-3 cm proximal to anode, between palmaris longus and flexor carpi radials (FCR)
Anode: 2-3 cm from wrist
Alt site: cubical fossa (inside elbow)
Posterior tibial nerve (PTN) (L4-S3)
Plantar flexion - abductor Hallicus muscle
Cathode: between medial malleollus and Achilles tendon
Anode: 2-3 cm distal to cathode
Peroneal N (L4-S2)
plantar eversion - peroneus longus and peroneus Brevis
Cathode - below fibulae head
Anode - 3 cm distal to cathode
Saphenous N is alt stim site for above the knee amputees
Changes in SSEPs
Stimulate below surgery
Record above stimulation site, around surgical site, and above surgical site
Monitor upper and lower SSEPs on ALL cases
Cervical case: upper and lower SSEPs run through cervical region
Thoracic/Lumbar case: lower SSEPs run through surgery pathways; upper SSEPs give you info on positional issues of arms and shoulders
Global changes: changes in all SSEPs (upper and lower) indicate high level of anesthesia or significant decrease in BP
Near field
Generator is close to recording electrodes
Cortical responses: recording electrodes (CPz, CP3, CP4) placed over/near generator (somatosensory cortex)
Peripheral responses: Erbs point (upper SSEP) and pop fossa (lower SSEP) placed over/near generators (brachial plexus-erbs and sciatic nerve-pop fossa)
Far field
Generator far from recording electrodes
recording electrodes (FPz) places far from generator (Brainstem - caudal medial lemniscus and thalamus)
Stationary Potential
not seen Intraoperatively @ MPH
From gray matter
Amplitude changes, latency constant
Propagating potential
from white matter
Latency changes, amplitude constant
Where do peripheral responses come from? What waveform latency do they produce?
Erbs and Popliteal fossa are peripheral responses
Their stimulating points are brachial plexus ad tibial/sciatic N
They produce N9 latency waveforms
They are near-field and propagated
Where do subcortical responses come from? What waveform do they produce?
caudal medial lemniscus (CML) and Brainstem-thalamic junction are subcortical responses
They receive responses from erbs and politeal fossa
CML and Brainstem-thalamic junction produce P14-N18 latency waveform
They are Fairfield
Waveform Characteristics
Morphology: shape of wave
Peaks - negative polarity (N)
Trough - positive polarity (P)
Latency: time
Milliseconds (ms)
Waveform number is expected latency AFTER stimulation
Amplitude: height
Microvolts (uV)
Waveform for UPPER stimulation
Peripheral: N9
Cervical: N13
Subcortical: P14-N18
Cortical: N20
Analogous peaks
Share same generator
Waveform for LOWER stimulation
Peripheral: N9
Lumbar: N22
Subcortical: P31-N34
Cortical: P37
Latency is higher because the lower limbs are more distal to the SScortex than the upper limbs
Peripheral responses upper electrode position
erbs point: @ clavicular notch (2cm above middle of clavicle)
2 electrodes:
Red/+/anode on left erb
Black/-/cathode on right erb
Alt sites:
Sub-clavicular
Axillary crease
Posterior trap muscle
Peripheral responses lower electrode position
popliteal fossa: behind knee
2 electrodes:
Cathode 5cm above knee crease
Anode 2cm above knee crease
Inactive cephalic electrodes in subcortical responses
Anything that is NOT a cephalic site
Active cephalic electrodes in subcortical responses
Anything in cephalic region
Where do cortical responses come from? What waveform do they produce?
Primary somatosensory cortex (based on stimulated limb) are cortical responses
They receive responses fromcaudal medial lemniscus (CML) and Brainstem-thalamic junction
Primary somatosensory cortex produces N20 latency waveform
They are nearfield and stationary
Cortical Electrode Locations
upper extremity SSEPs - CP3 or CP4
Since more lateral
Lower extremity SSEPs -CPz
Since more mediaL
Inactive cephalic electrodes
FPz
Non-cephalic electrodes
Not on scalp
Called references
Ex. Mastoid
Channel logic rules
somatosensory cortical potentials - active electrode must be active cephalic electrode
Isolated subcortical potential - active electrode must be inactive cephalic electrode
Channels must be created w intentional of isolating a single desired potential in each respective channel
Common mode rejection
Same signals received by two electrode cancel out
Cortical SSEP blood supply
MCA
ACA
Subcortical SSEP blood supply
Vertebrobasilar artery
SSEP peripheral blood supply
Erbs - subclavian artery
Politeal fossa - popliteal artery
Paradoxical Lateralization
When CPz doesn’t give a good response but ipssilateral side to stimulated side give better response
High frequency filters (HFF)
Diminish signals above set frequency
low pass filters - allow lower freq to pass; cuts out high freq
Low freq filters (LFF)
Diminish signals low set frequency
High pass filters - allow higher freq to pass; cuts out low freq
Band pass
Only range of freq allowed to pass
combined low and high pass filters
Phase lag
Increased latency
Decreased high frequency filters over time
Phase lead
Decreased latency
Increased low frequency filters over time
Notch filter
Aims at cutting out narrow band of freq
Con: ringing effect that filters out surrounding Hz of targeted Hz
Ex. 60Hz notch filter
58-62 Hz is filtered dur to proximity to 60 Hz
Used fr sRMG and EEG
Recording parameters
analysis time
Upper 5-10 ms
Lower 10-15 ms
Trials
Upper 100-200+
Lowers 200+
LFF
10-30Hz
HFF
Cortical 250-500 Hz
Subcortical 500-1500Hz
Peripheral 1500 Hz
Stimulation parameters
intensity: how high you stim
Upper 20-50 mA
Lowers 35-100 mA
Pulse width/ duration how long each pulse
Upper and lower 200-500 us (0.2-0.5 ms)
Repetition rate: how often
Upper and lower 1-5 Hz (cycles/second)
Not whole integer
Baseline range changes (waveform repeatability)
1% latency
15% amplitude
Alert criteria
50% amplitude
10% latency
Ideal SSEP anesthetics 1MAC
Des 6%
Sevo 2%
ISO 1%
Ideal ssep map >60 mmhg