Lecture 12- Electrocardiography: Manifestations of disease
0.0(0)
Card Sorting
1/108
There's no tags or description
Looks like no tags are added yet.
Study Analytics
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
109 Terms
1
New cards
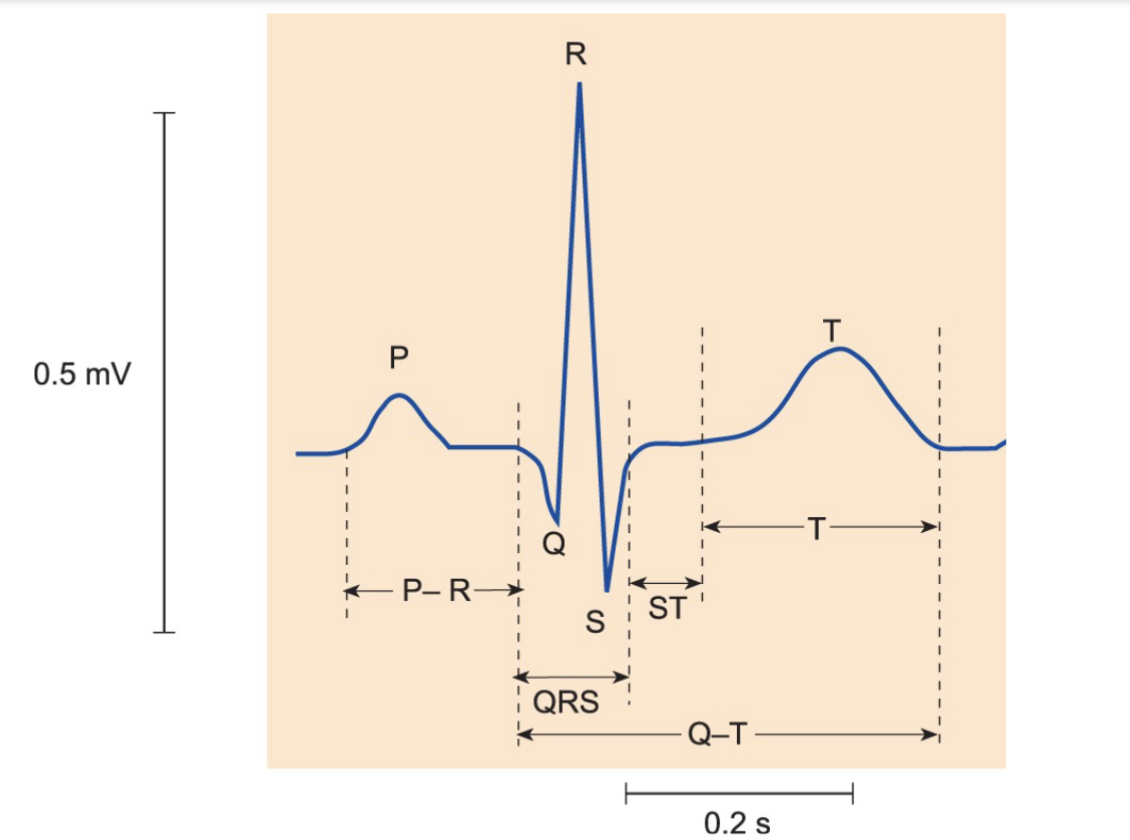
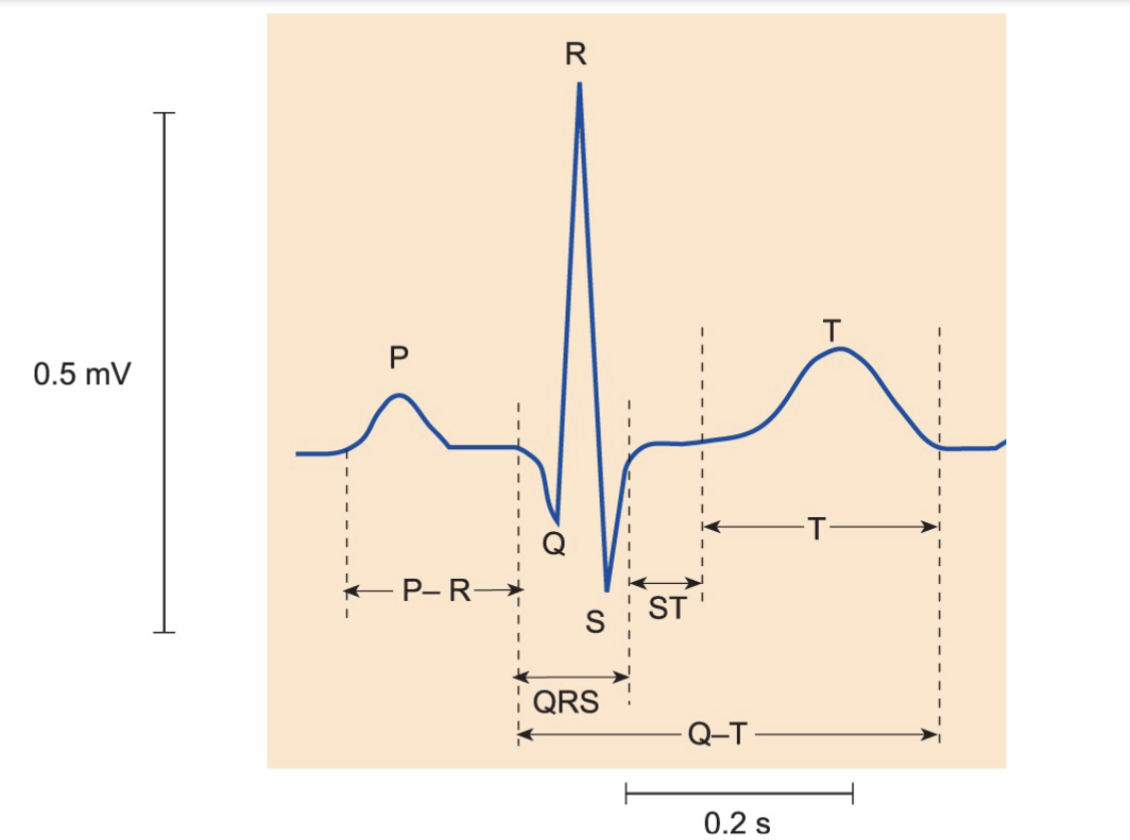
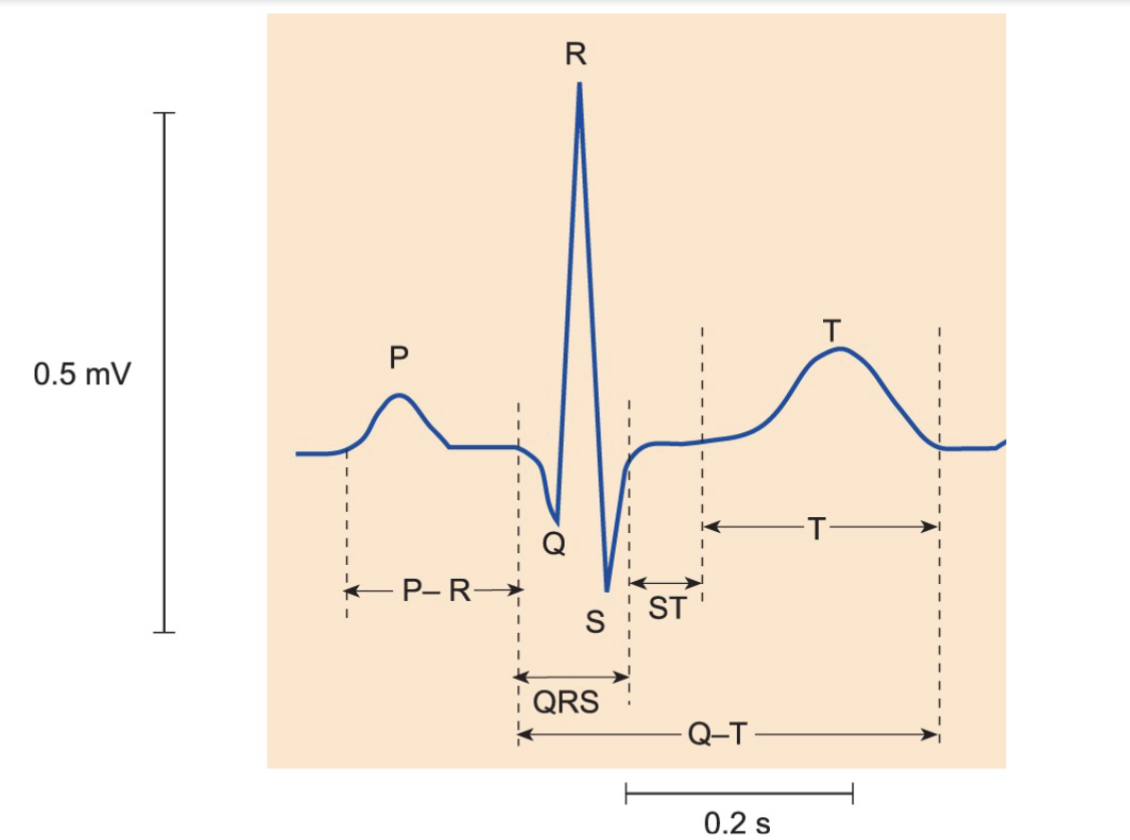
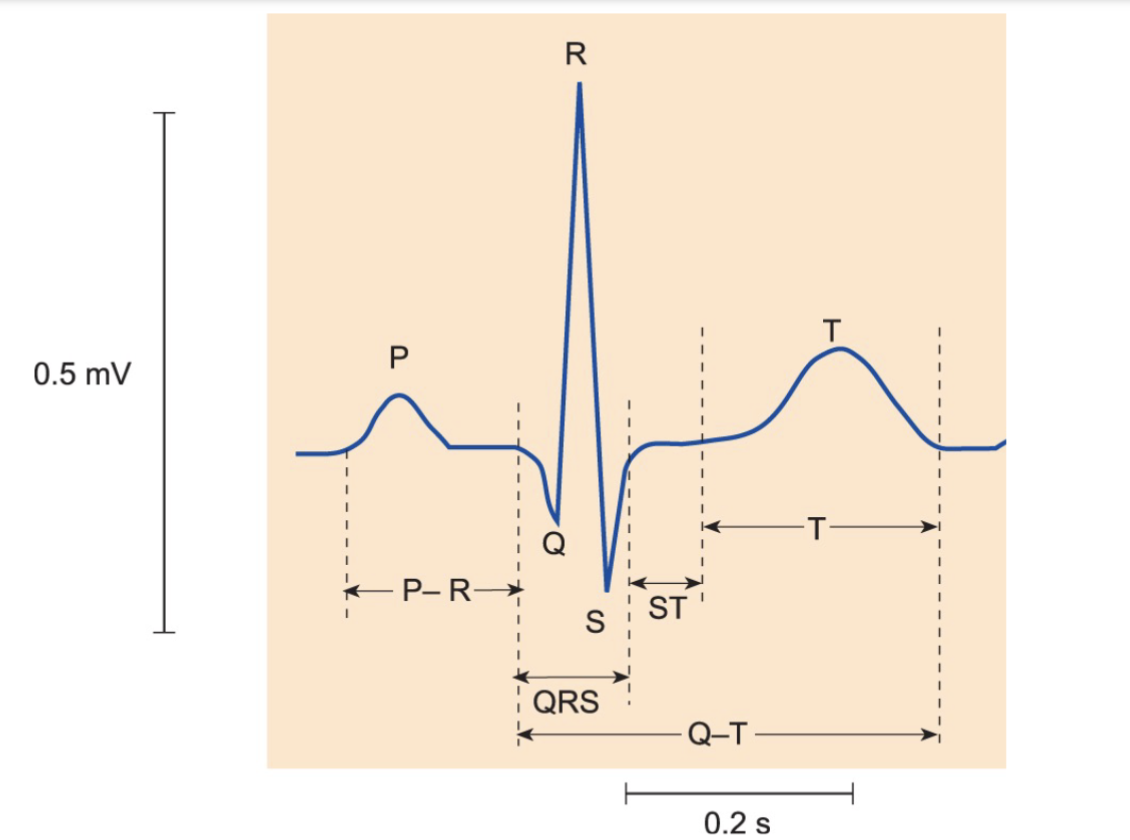
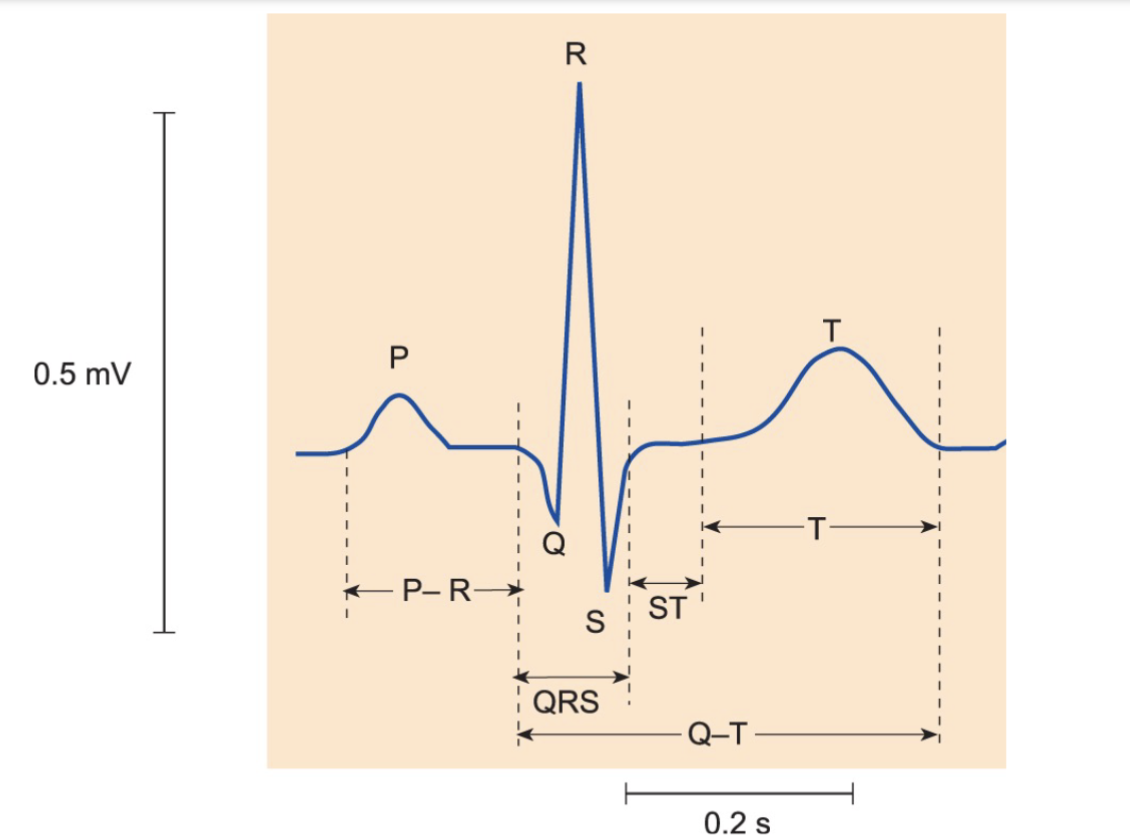
What are the four standard questions in clinical electrocardiography?
What is the heart rate?
What is the rhythm of the heart ?
What are the intervals between the electrical events in the heart ?
What is the electrical axis of the heart?
What is the rhythm of the heart ?
What are the intervals between the electrical events in the heart ?
What is the electrical axis of the heart?
2
New cards
What is normal sinus rhythm in clinical electrocardiography?
A regular heart rate within normal limits, with each P wave followed by a QRS complex & a relatively constant interval.
3
New cards
What is a regular heart rate in normal sinus rhythm?
Consistent time interval between each heartbeat.
4
New cards
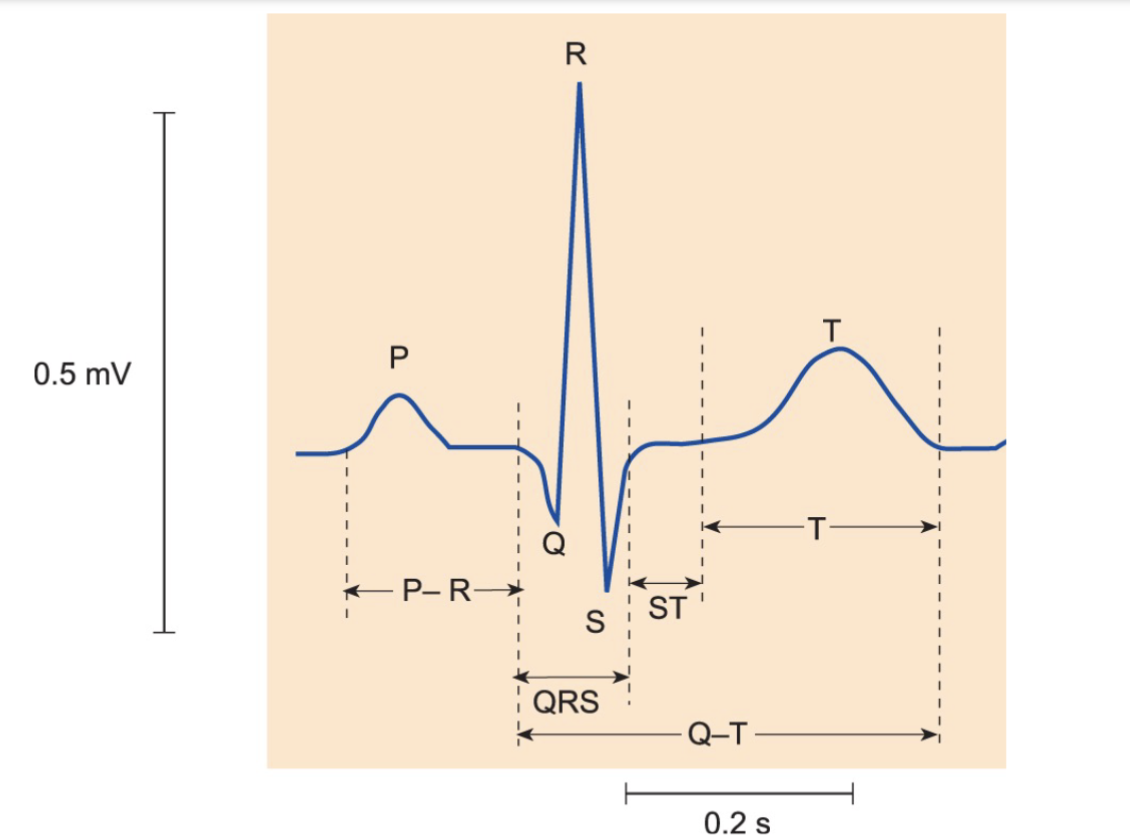
What is a P wave in normal sinus rhythm?
P wave is an electrical signal that represents the depolarization of the atria.
5
New cards
What is a QRS complex in normal sinus rhythm?
QRS complex is an electrical signal that represents the depolarization of the ventricles.
6
New cards
What is a relatively constant interval in normal sinus rhythm?
Consistent time intervals between each P wave & its corresponding QRS complex.
7
New cards
What is an arrhythmia in clinical electrocardiography?
Abnormal heart rhythm.
8
New cards
What is abnormal sinus rhythm in clinical electrocardiography?
Any deviation from the normal sinus rhythm, including irregular heart rate, absent P waves, & other abnormal features.
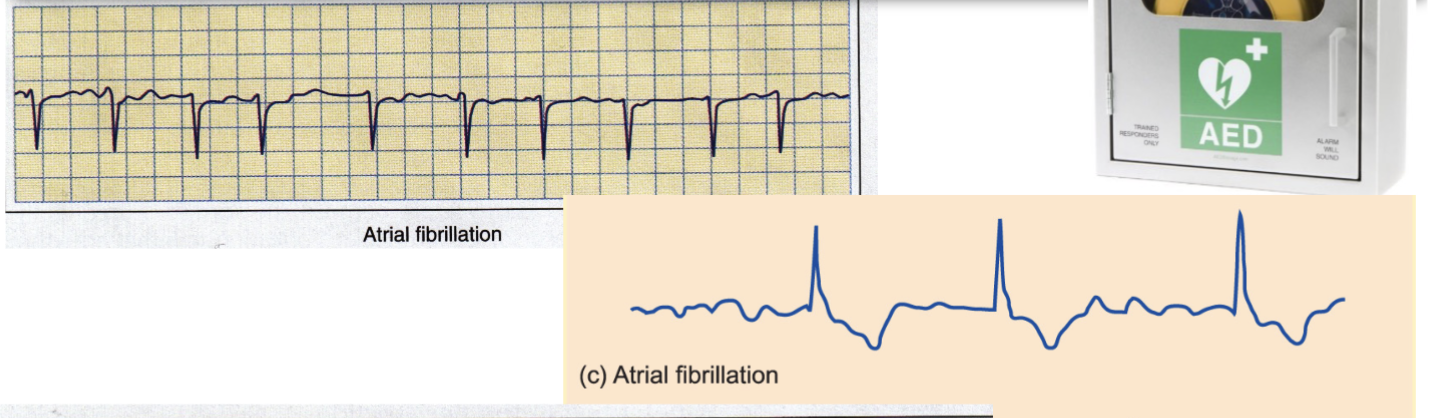
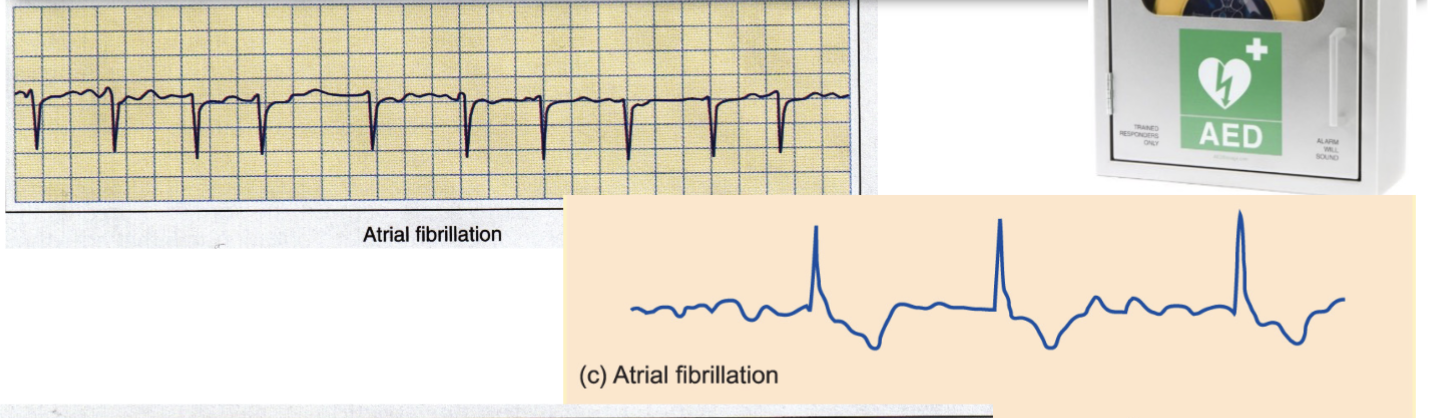
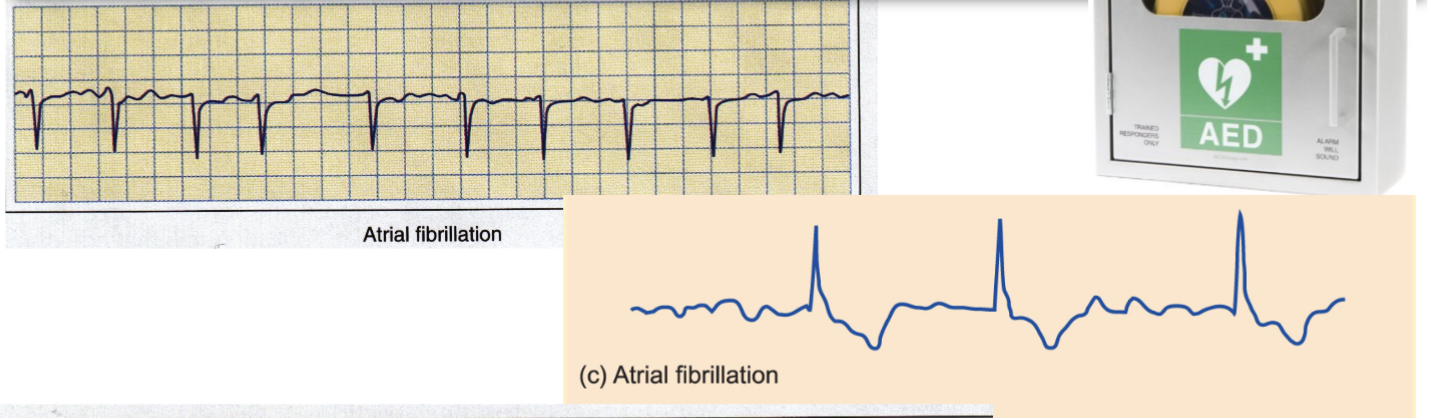
9
New cards
Are all arrhythmias of concern in clinical electrocardiography?
No, not all arrhythmias are of concern .
Some, such as respiratory sinus arrhythmia, are normal variations in heart rate that do not require treatment.
Some, such as respiratory sinus arrhythmia, are normal variations in heart rate that do not require treatment.
10
New cards
What is respiratory sinus arrhythmia?
Normal variation in heart rate that occurs during breathing, characterized by an ↑↑↑ in heart rate during inhalation & a ↓↓↓ during exhalation.
11
New cards
How is arrhythmia diagnosed & treated in clinical electrocardiography?
Analysis of ECG tracings, & treatment depends on the type & severity of the arrhythmia. Treatment options may include medication, electrical cardioversion, or implantable devices such as pacemakers or defibrillators.
12
New cards
What are some common types of arrhythmias in clinical electrocardiography?
Atrial fibrillation, ventricular tachycardia, & supraventricular tachycardia, among others.
13
New cards
What are the potential consequences of untreated arrhythmias in clinical electrocardiography?
Stroke, heart failure, & sudden cardiac death.
14
New cards
What is heart block in clinical electrocardiography?
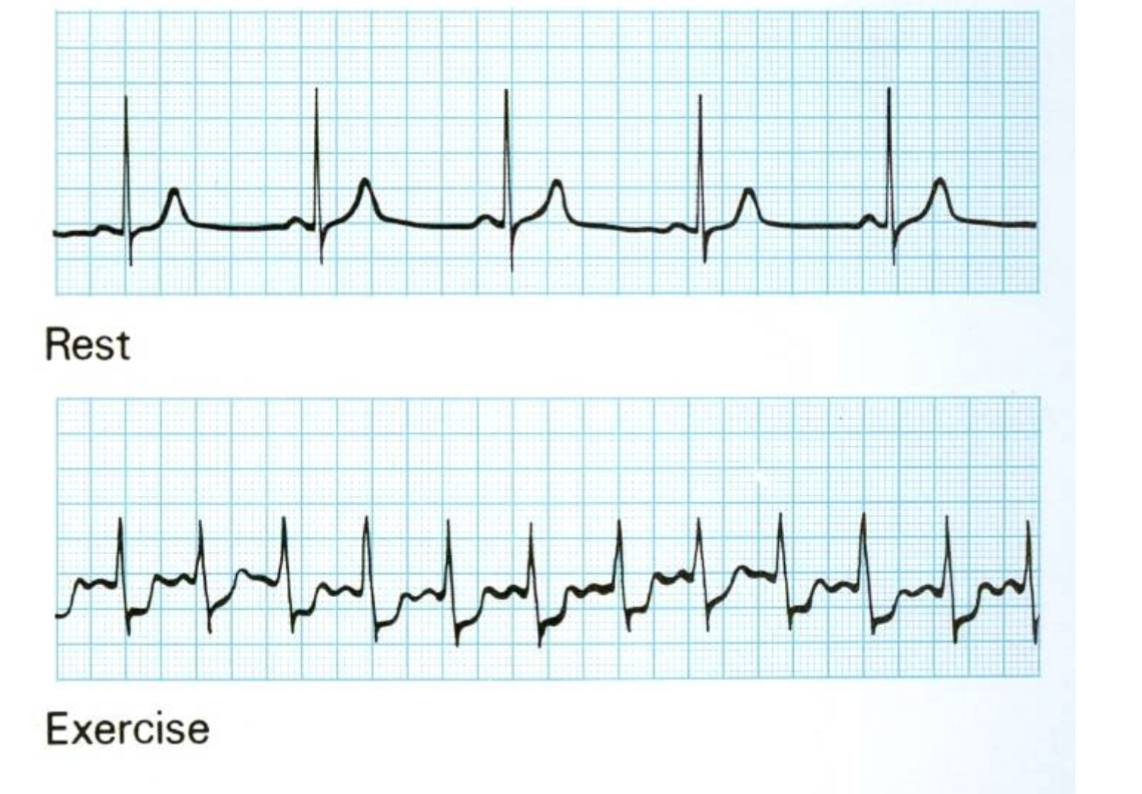
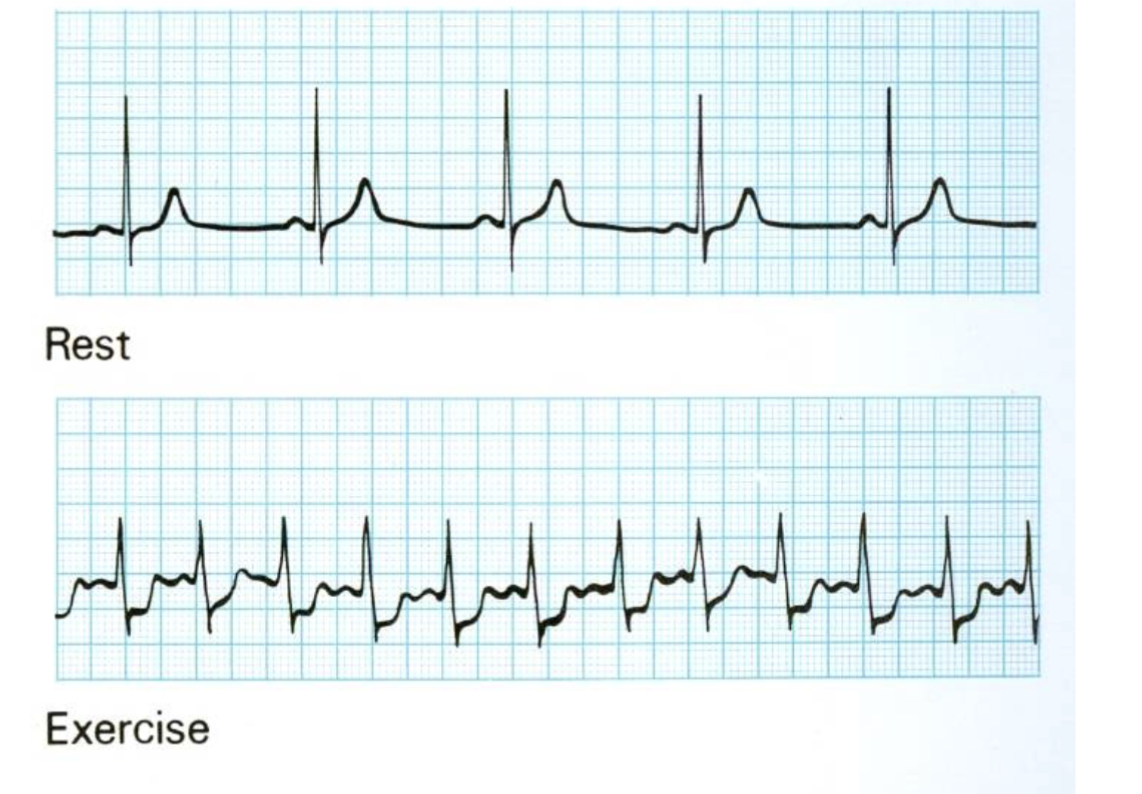
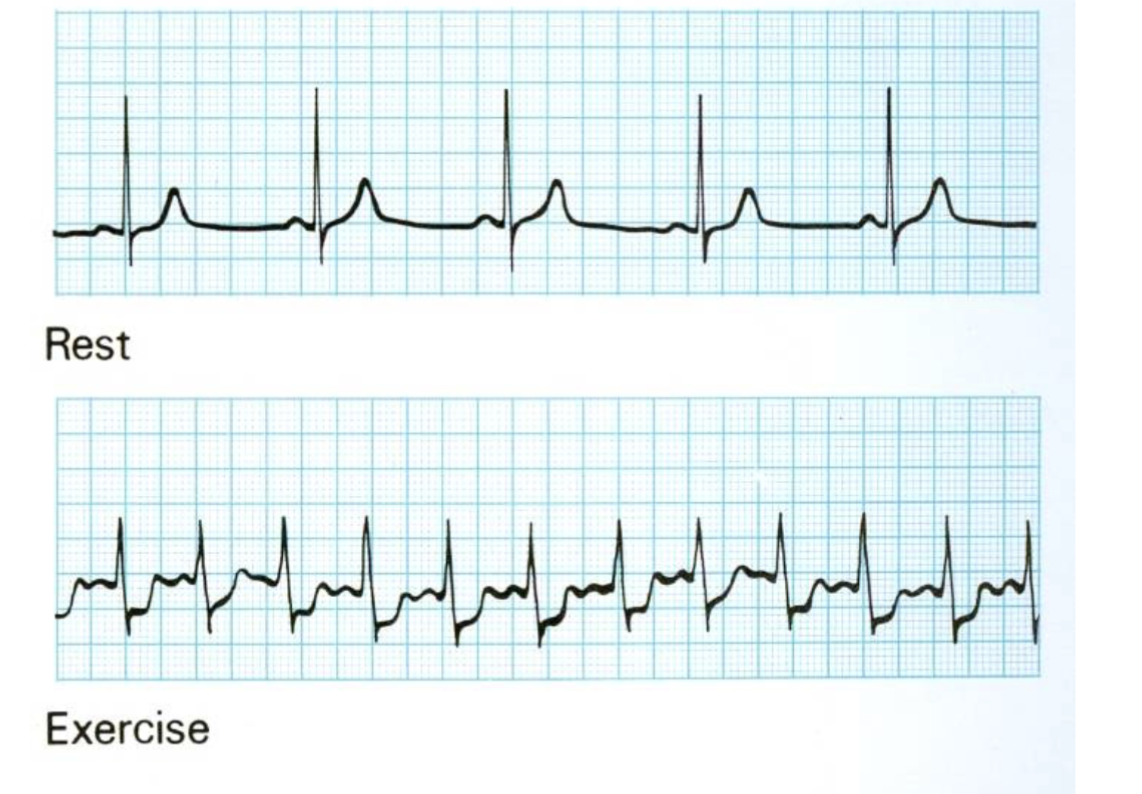
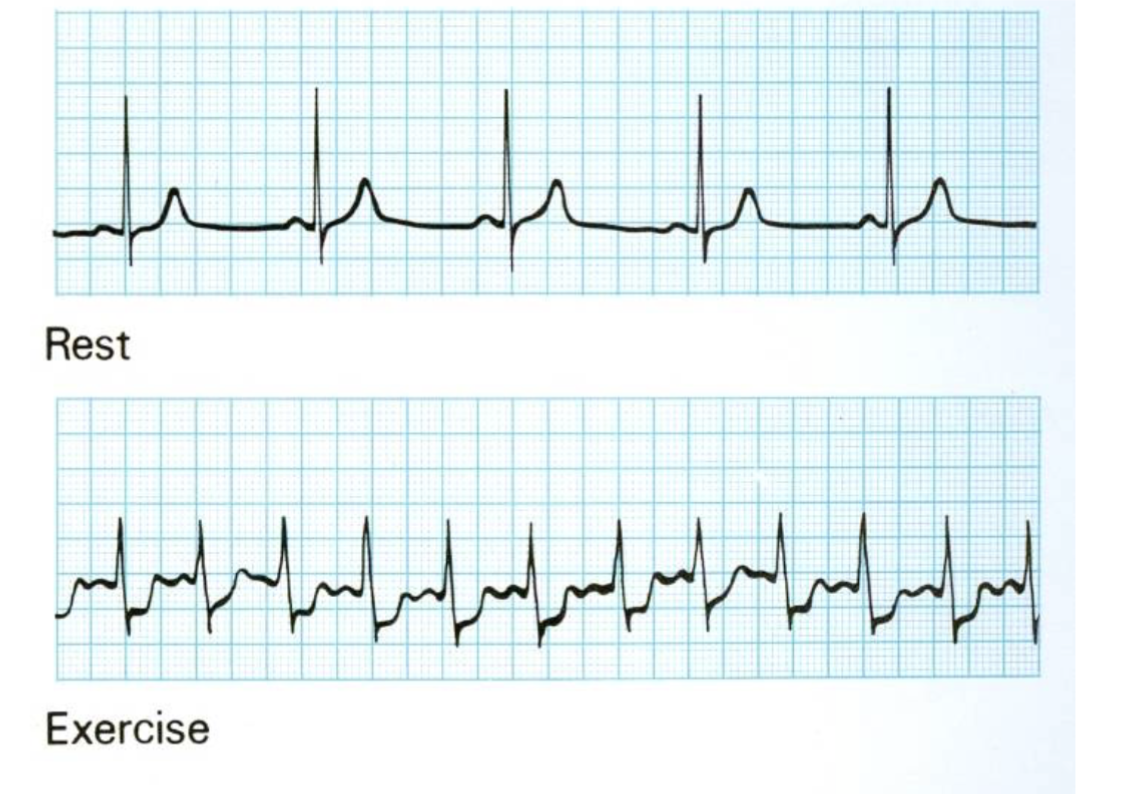
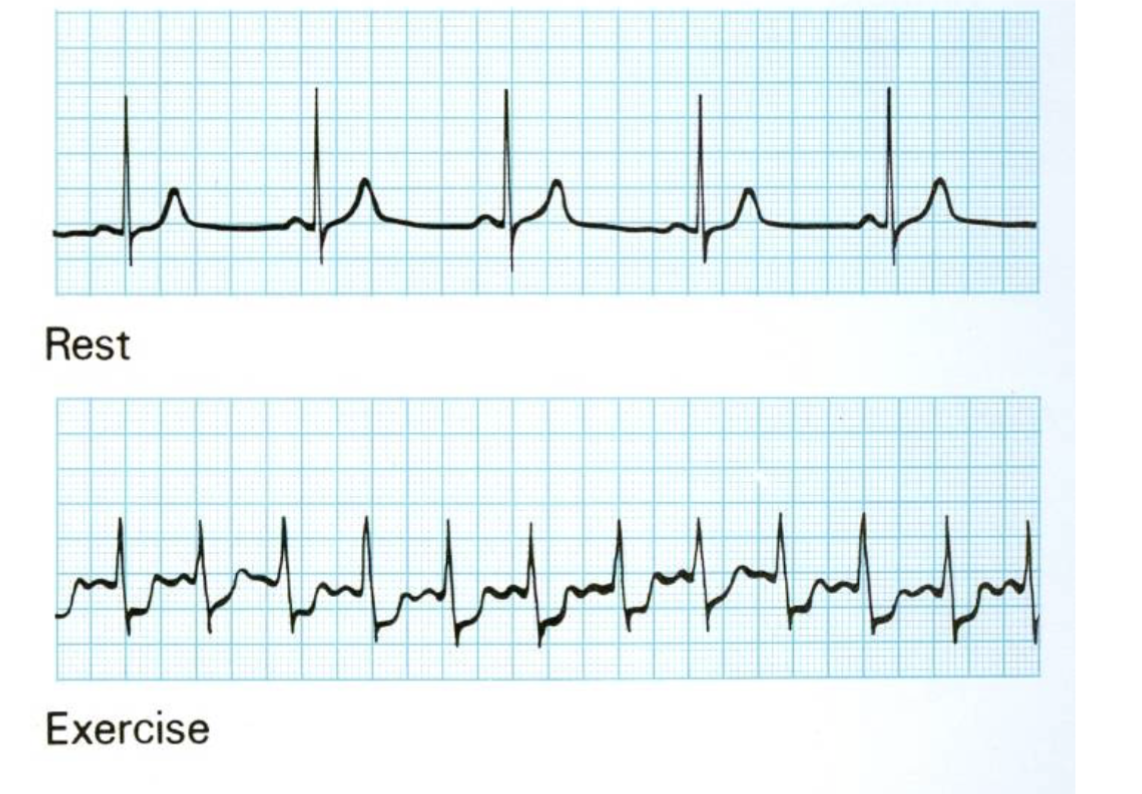
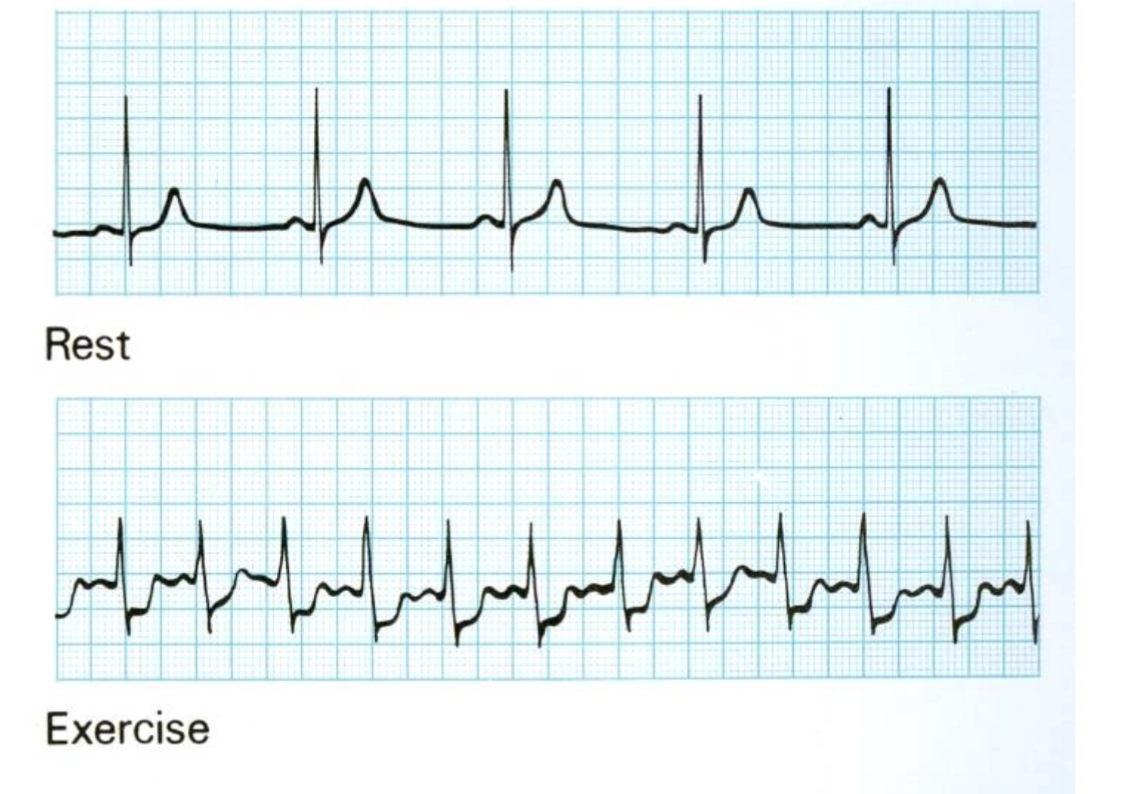
An interruption in the electrical signals that control the heartbeat, resulting in a slower or irregular heart rate.
15
New cards
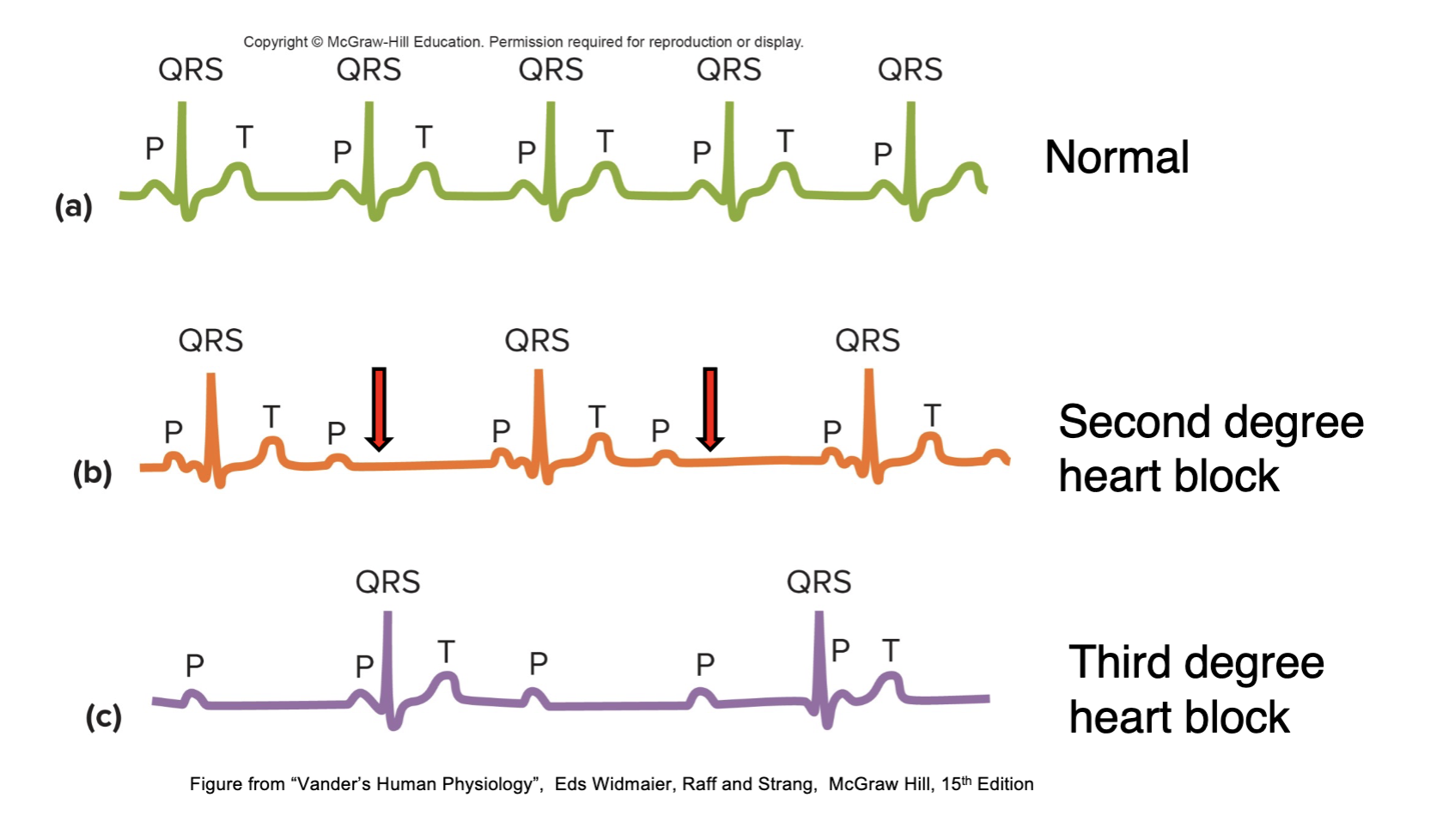
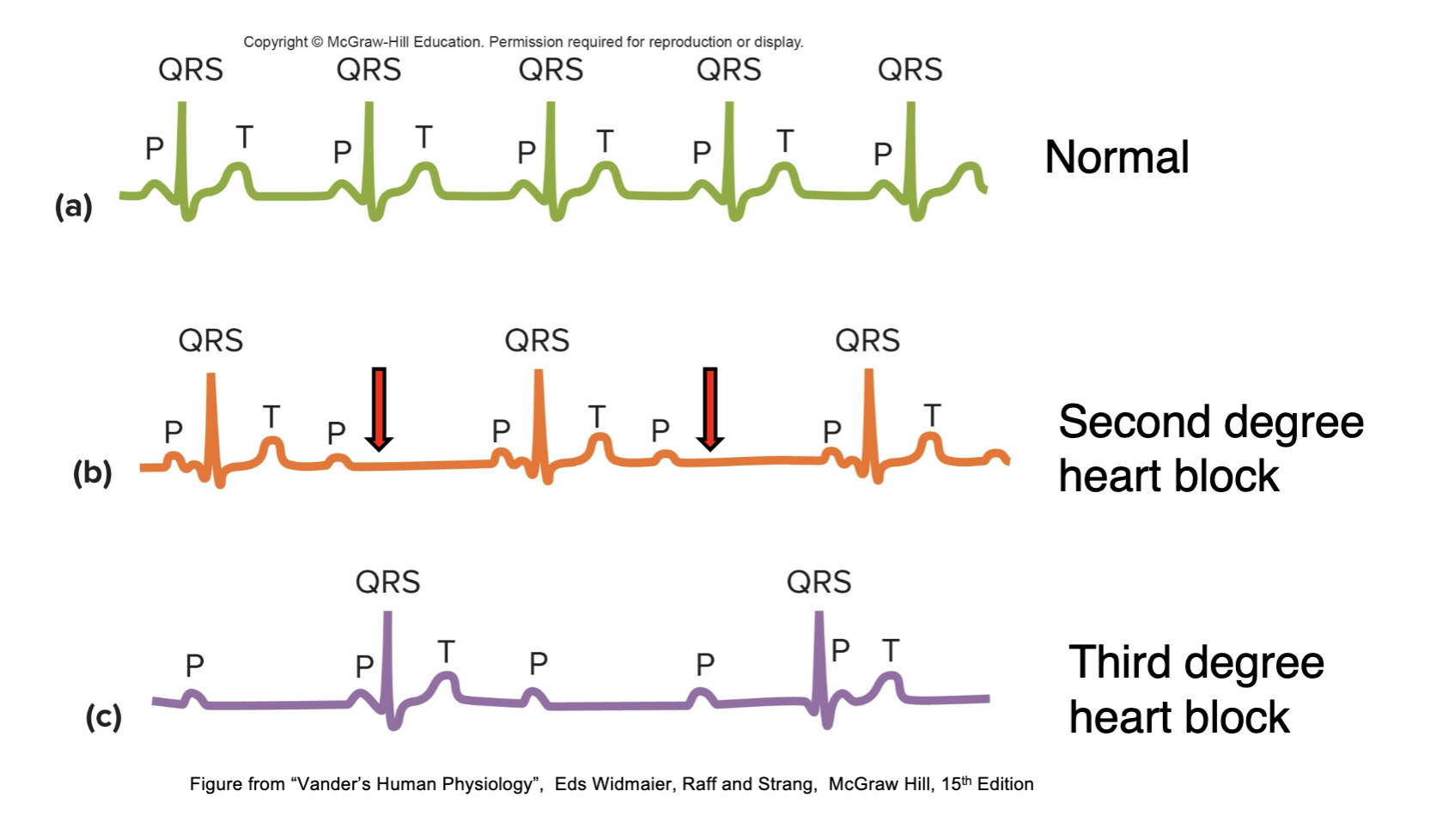
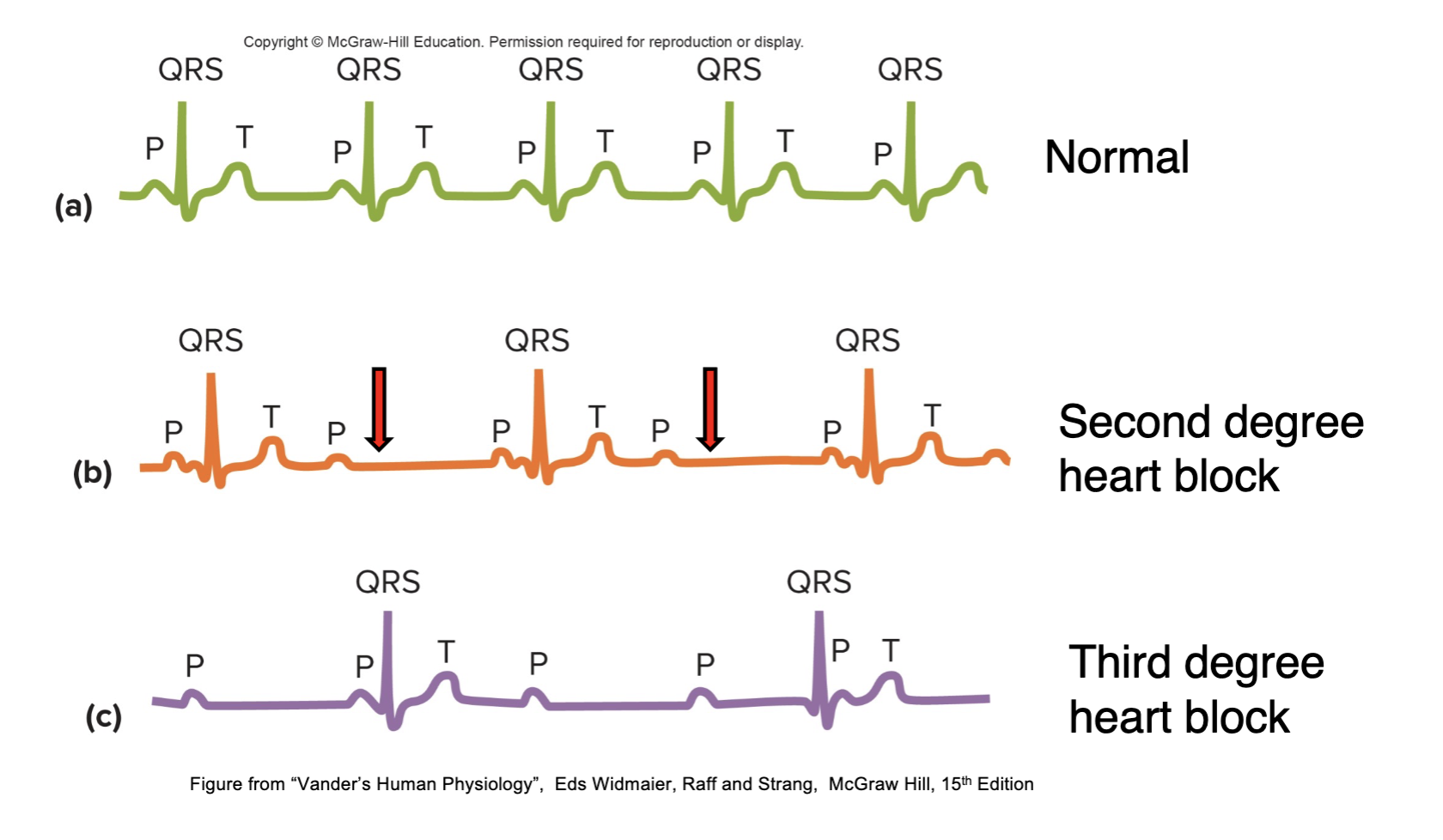
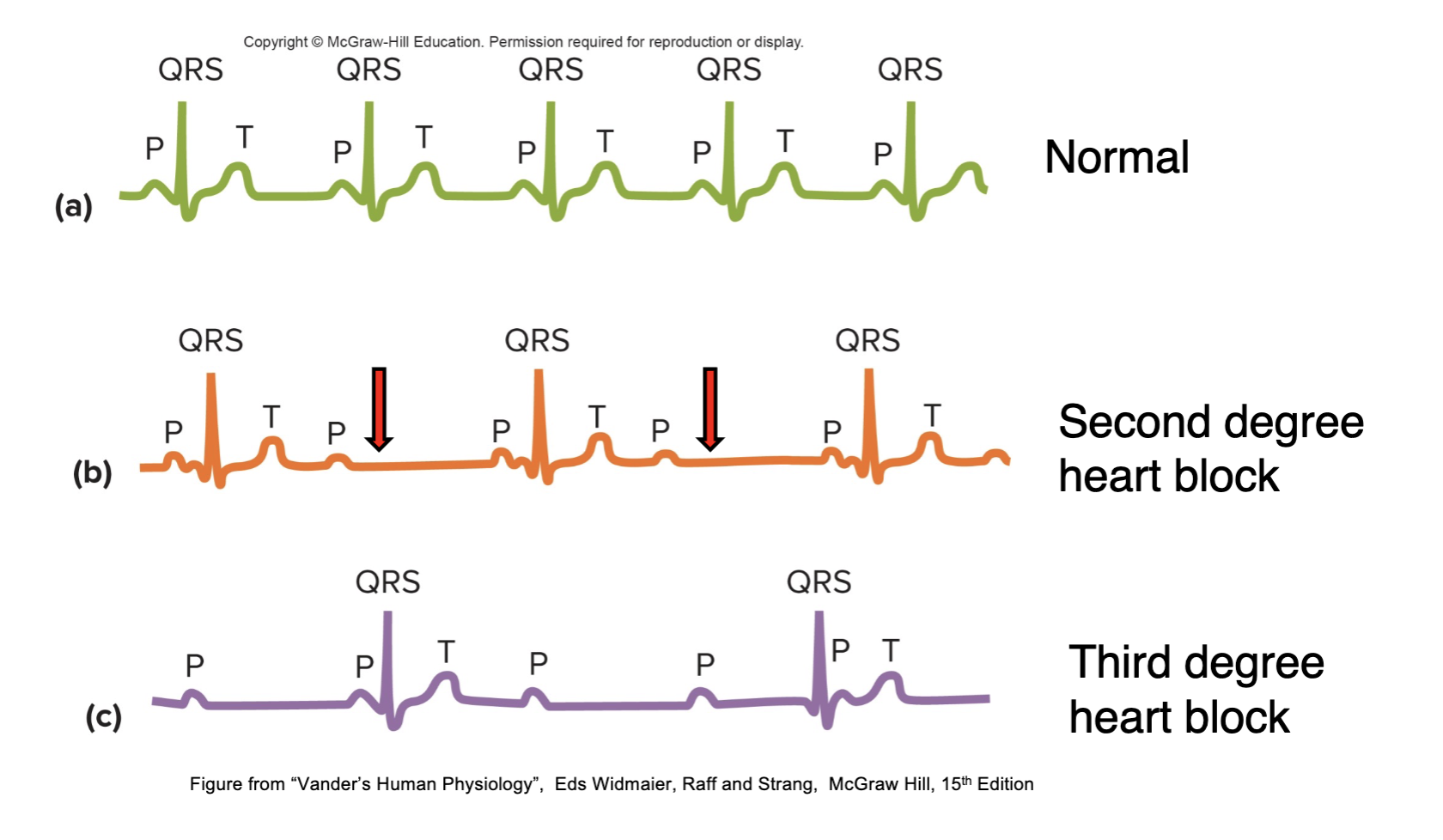
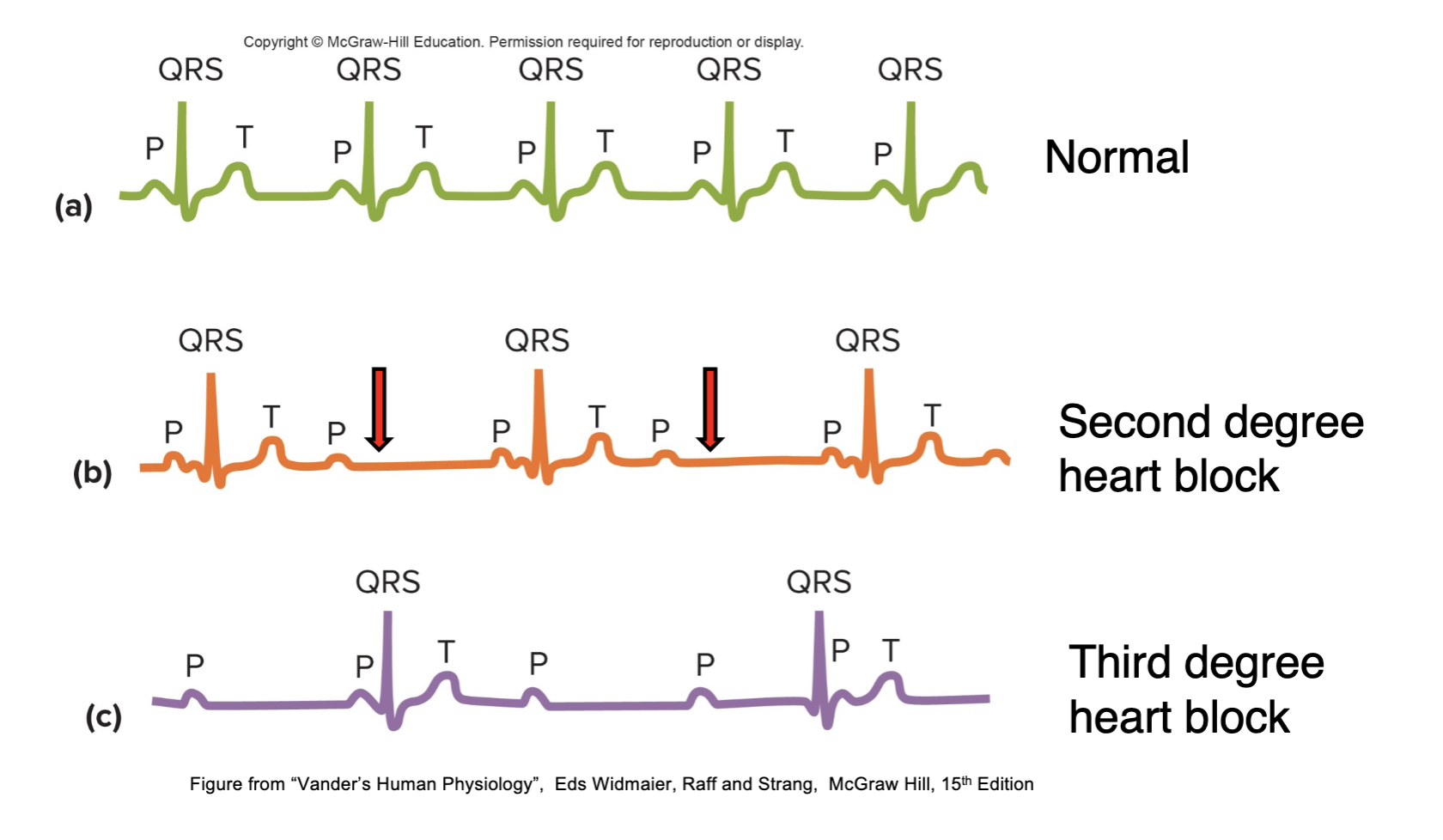
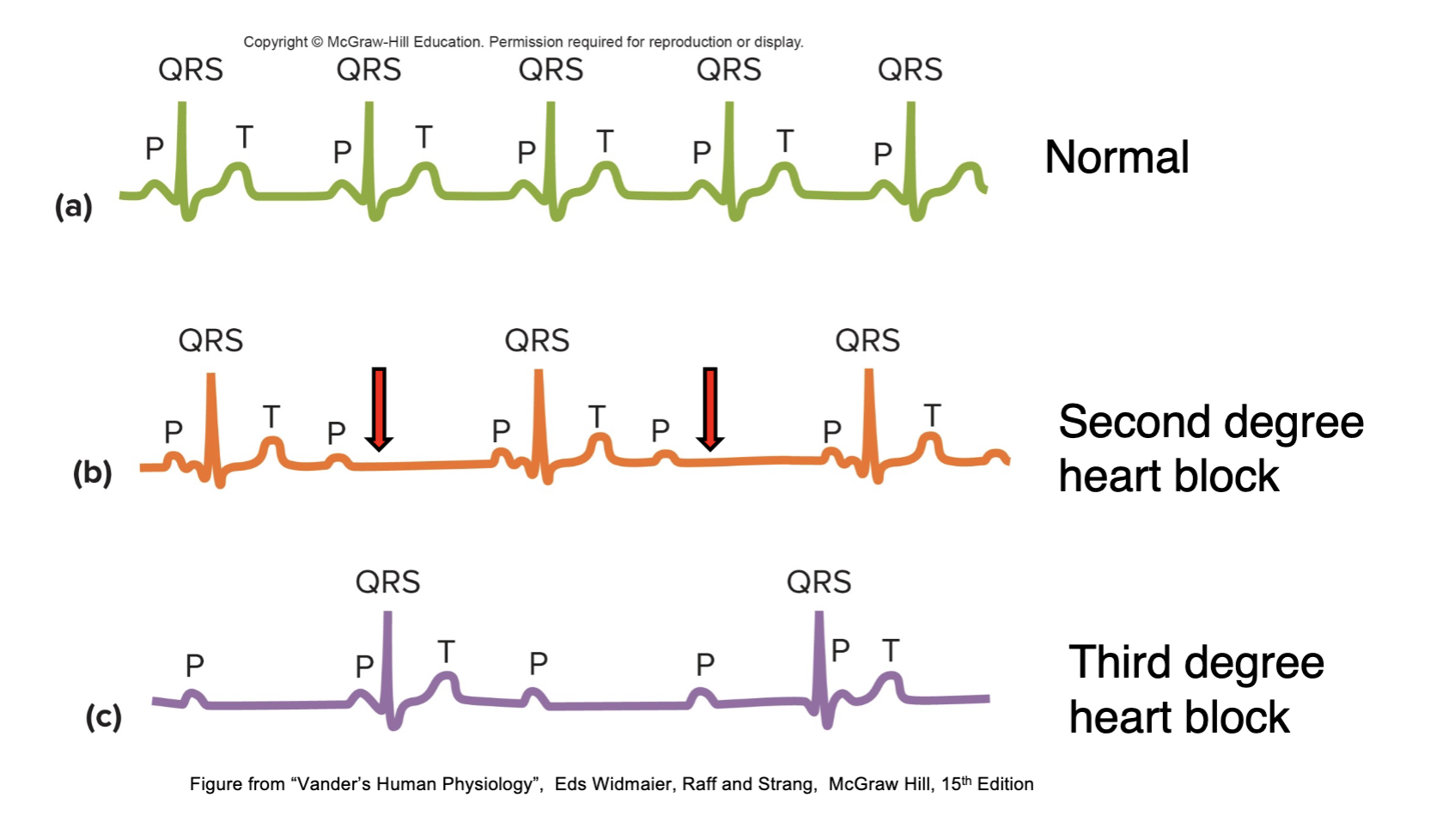
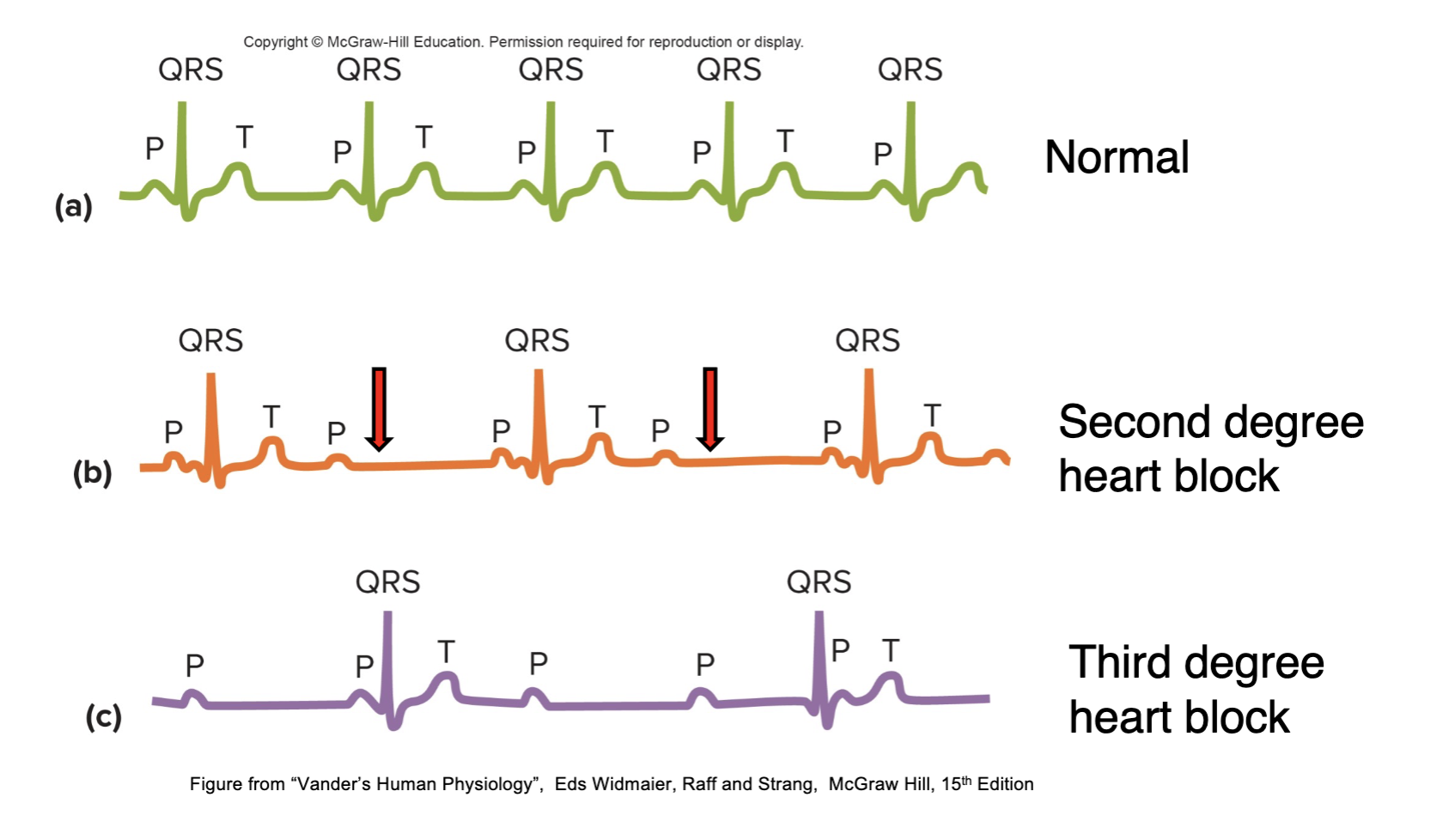
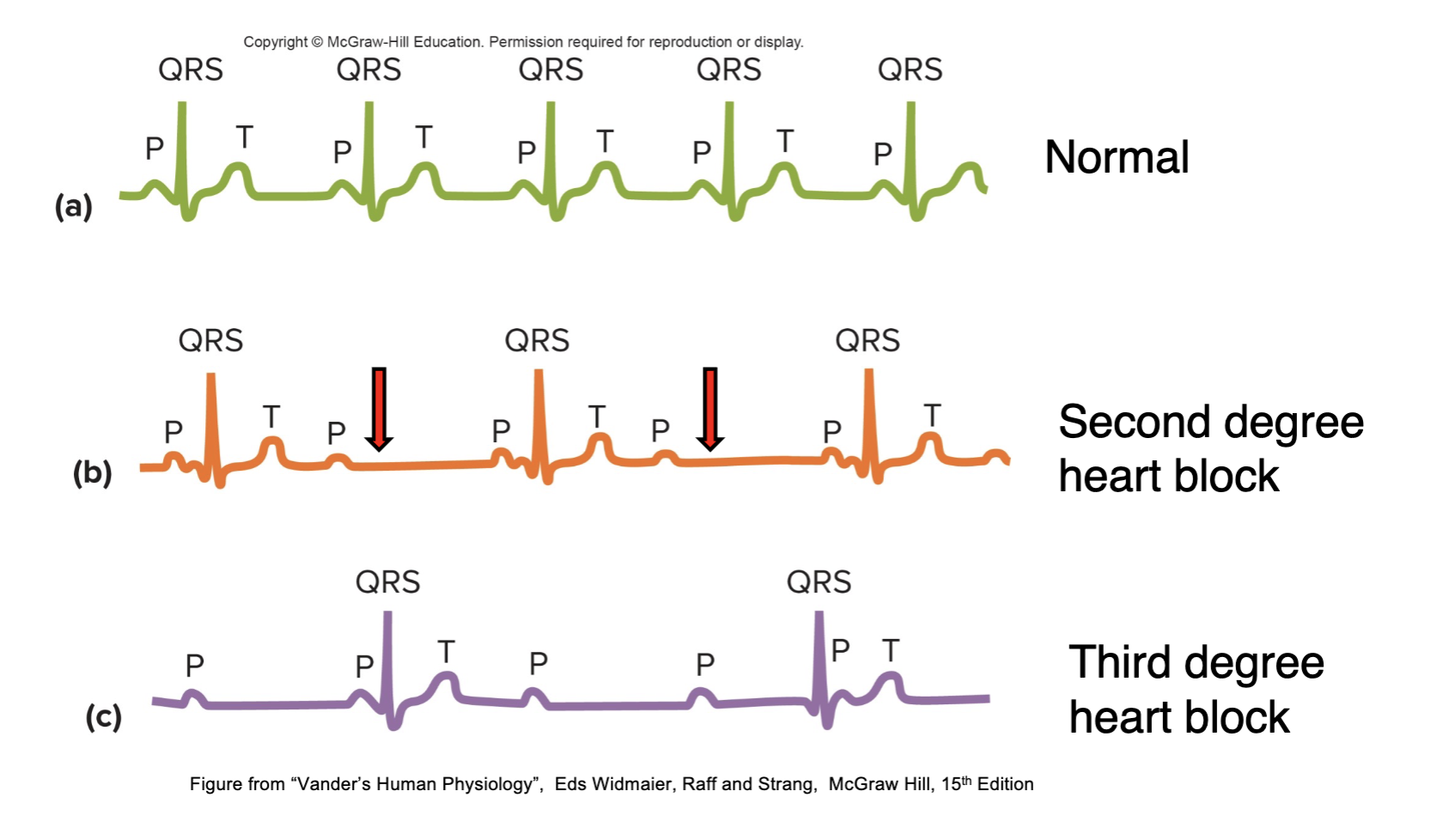
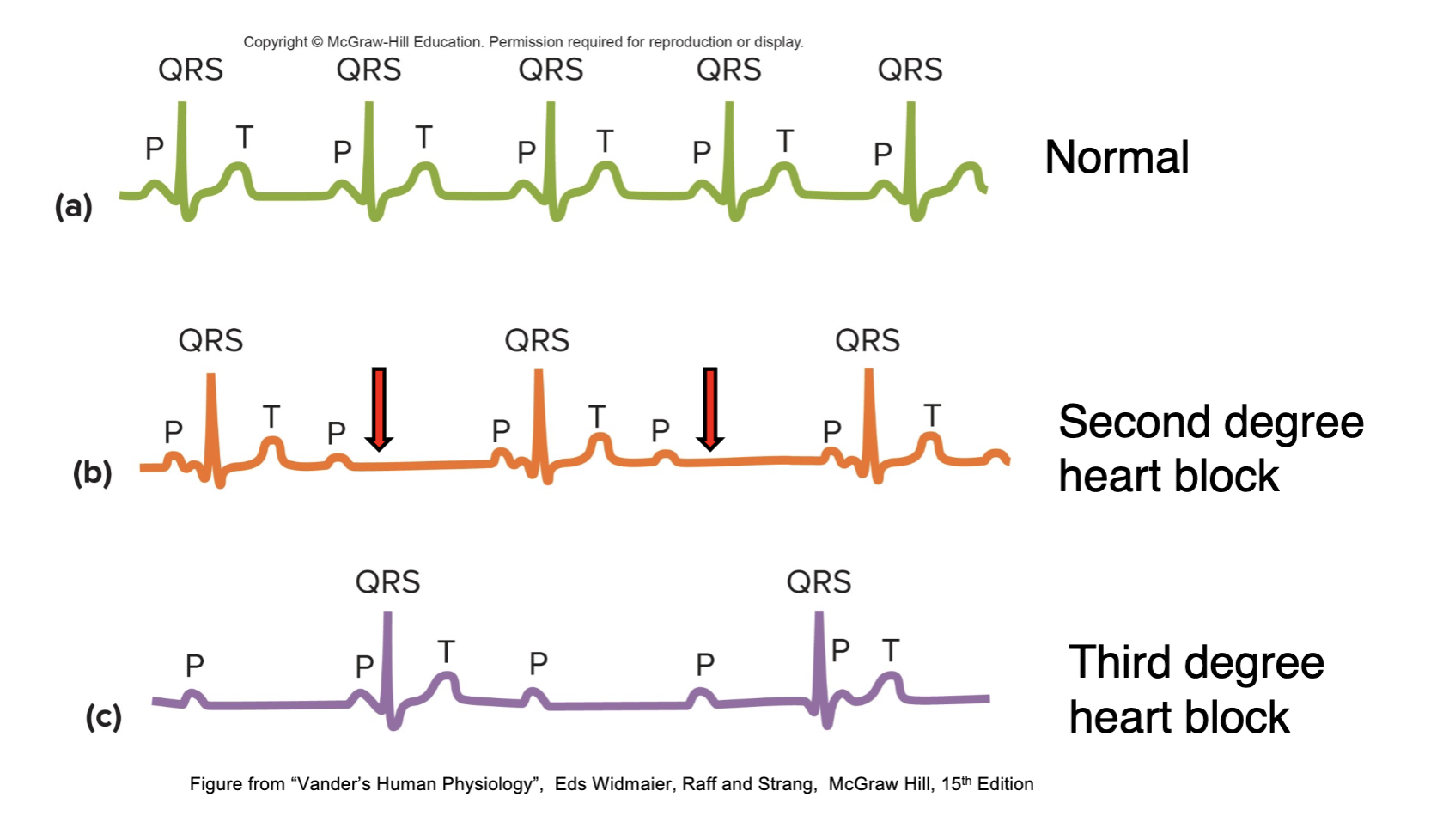
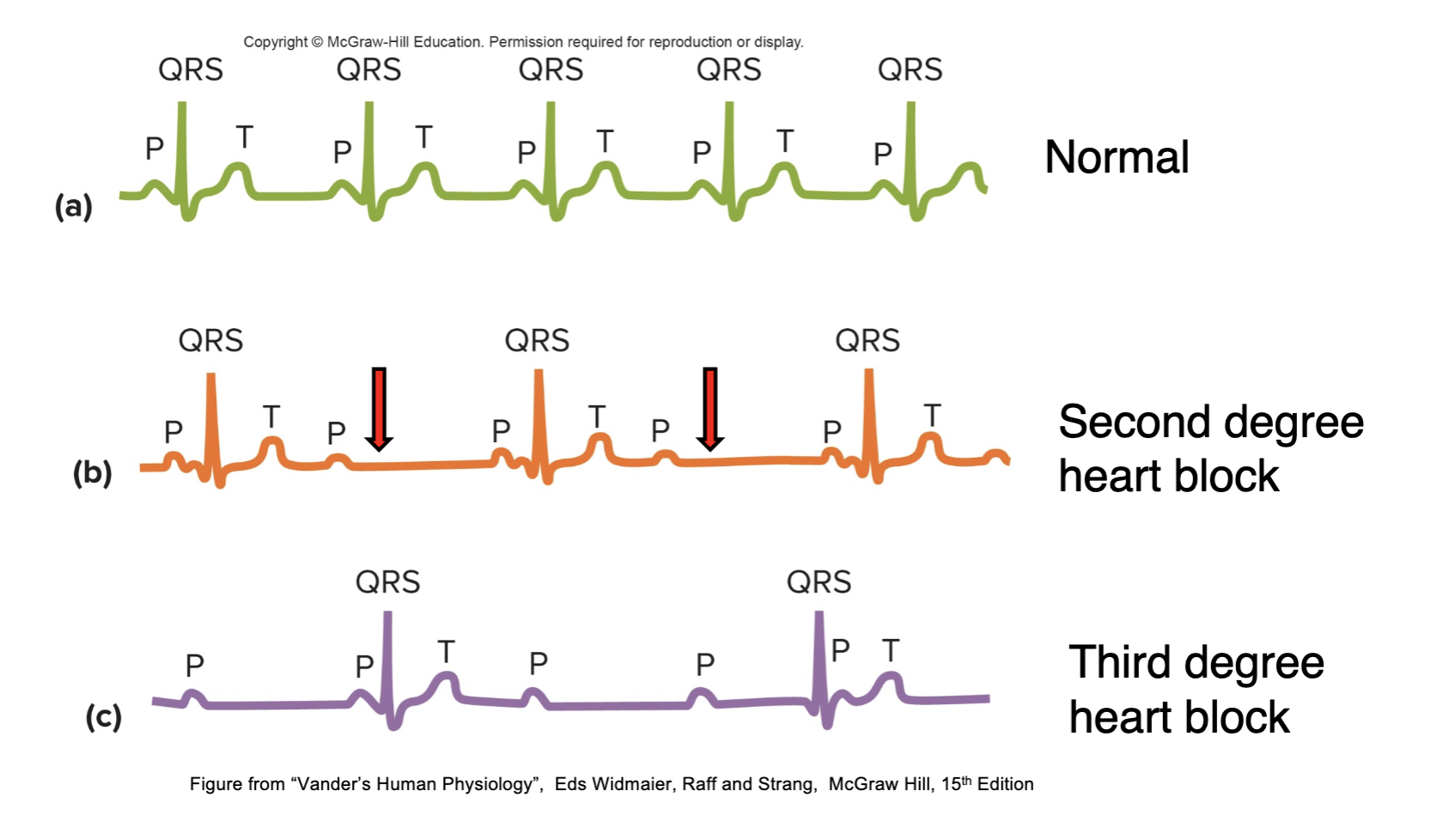
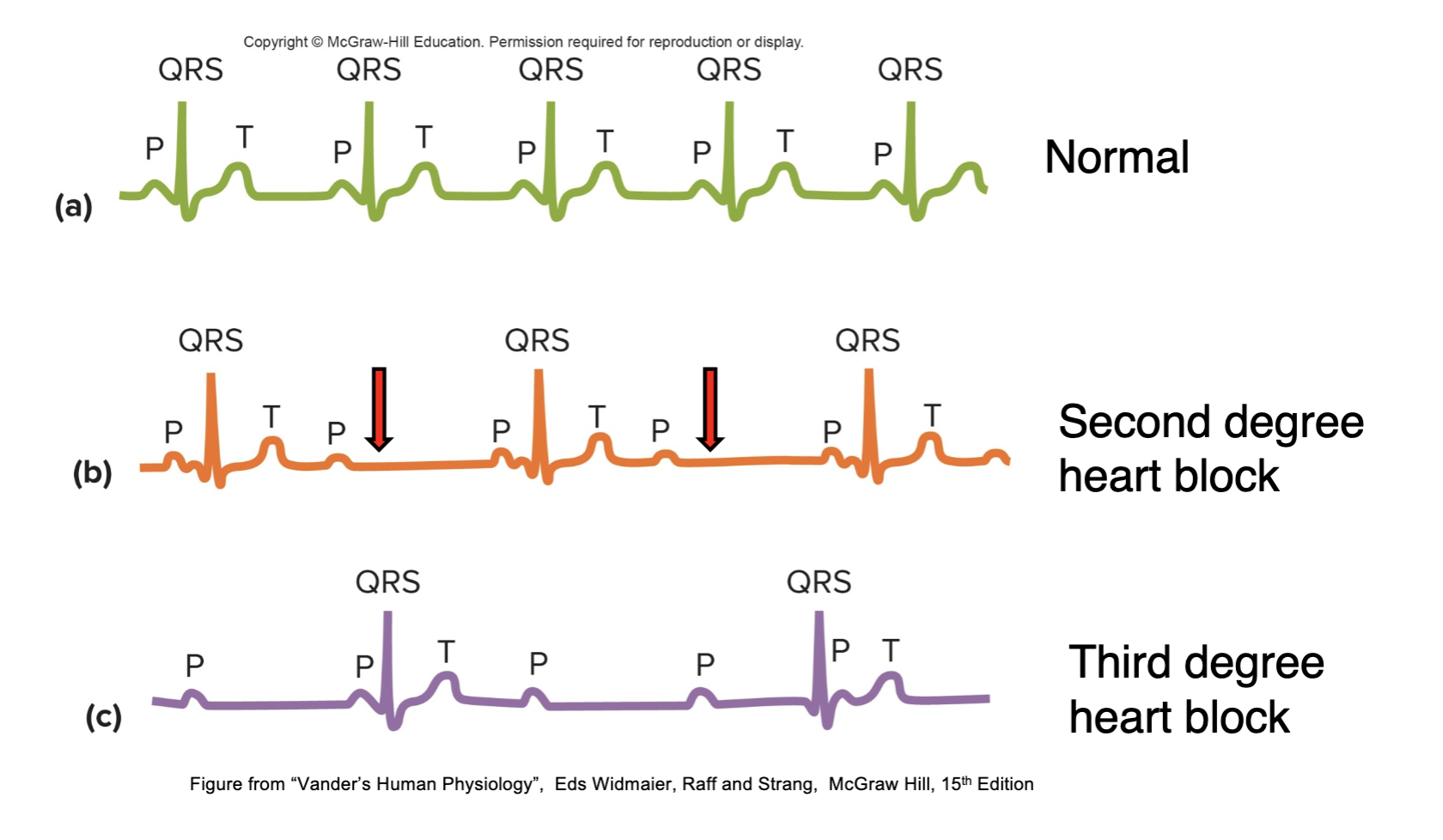
What are the three types of heart block?
First degree, second degree, & third degree.
16
New cards
What is a normal heart block in clinical electrocardiography?
A regular heartbeat with a consistent time interval between each heartbeat.
17
New cards
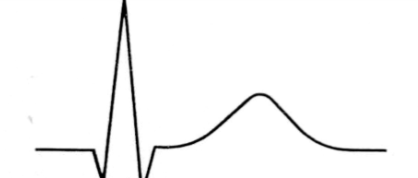
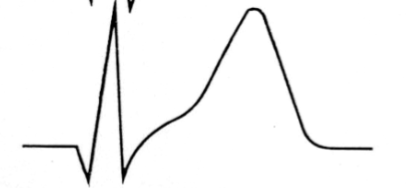
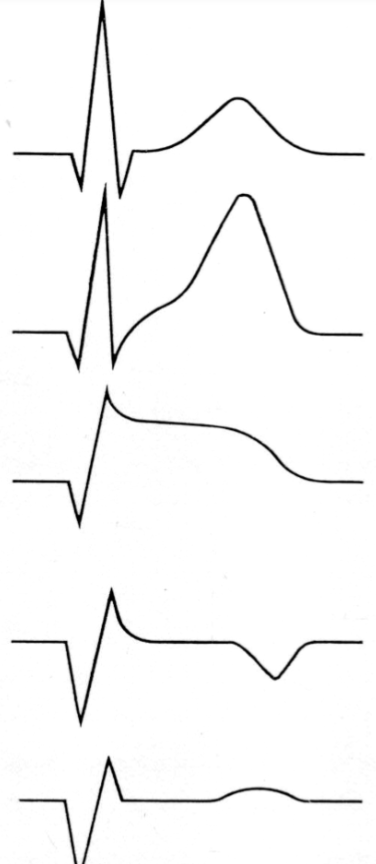
What is second degree heart block in clinical electrocardiography?
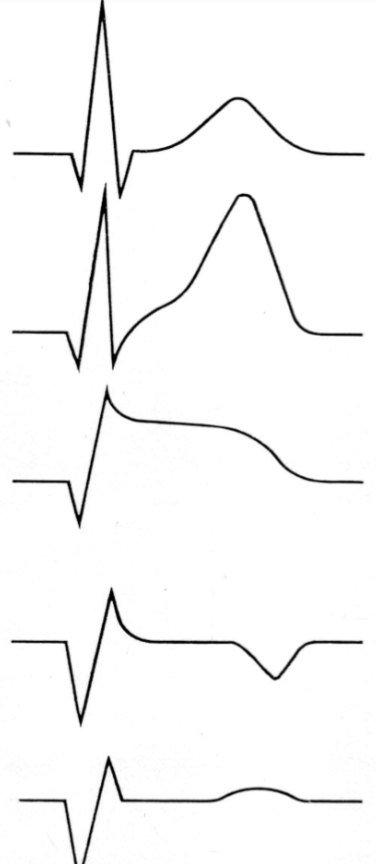
An interruption in the electrical signals that control the heartbeat, resulting in a slower or irregular heart rate with occasional dropped beats.
18
New cards
What is third degree heart block in clinical electrocardiography?
Complete heart block, where the atria & ventricles beat independently of each other, resulting in a slow & irregular heartbeat.
19
New cards
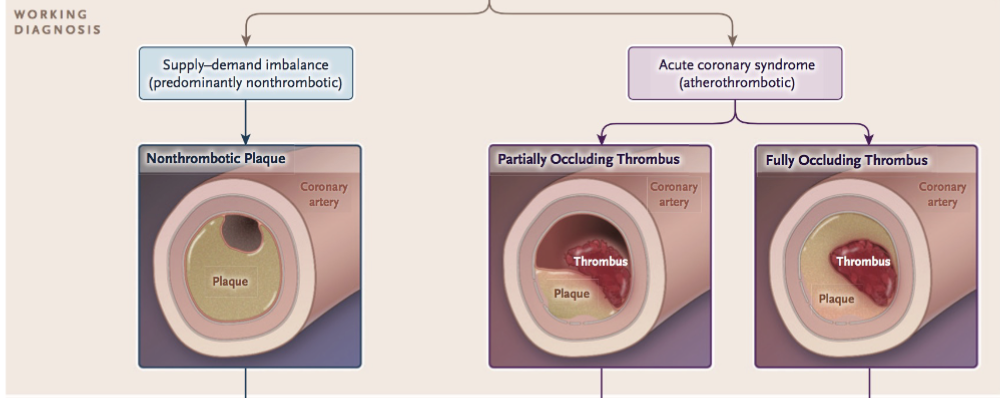
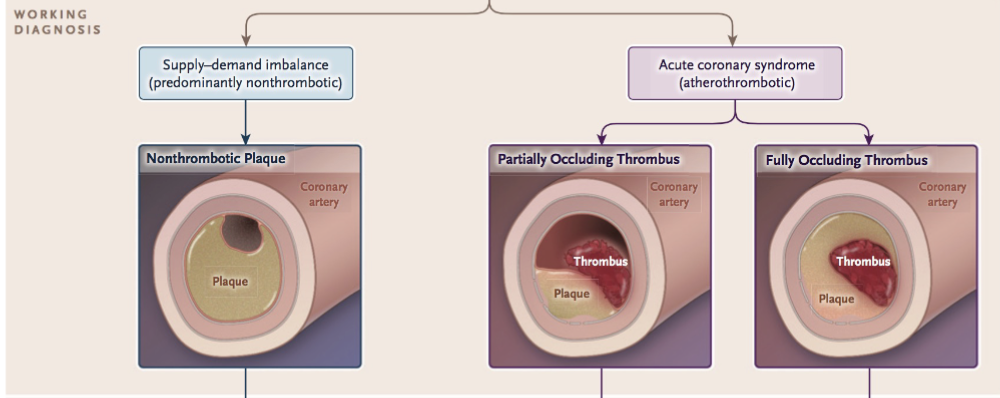
What are some common symptoms of heart block in clinical electrocardiography?
Fatigue, dizziness, shortness of breath, & chest pain.
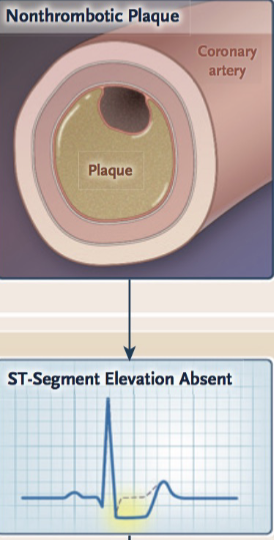
20
New cards
What are the potential consequences of untreated heart block in clinical electrocardiography?
Heart failure, stroke, & sudden cardiac death.
21
New cards
How is first degree heart block characterised?
By a prolonged PR interval on the ECG, but every heartbeat is conducted to the ventricles.
22
New cards
How is second degree heart block characterised?
Type I \= Progressive lengthening of the PR interval until a beat is dropped, after which the cycle repeats.
Type II\= PR interval remains constant, but beats dropped intermittently with no pattern.
Type II\= PR interval remains constant, but beats dropped intermittently with no pattern.
23
New cards
What is third degree heart block?
Regular P-P interval (atrial depolarization), but a variable R-R interval (ventricular depolarization), with no apparent relationship between the two. Atrial rate faster than ventricular rate
24
New cards
How is heart block treated?
First degree heart block usually does not require treatment, while second degree & third degree blocks may require electrical pacing or implantable devices such as pacemakers.
25
New cards
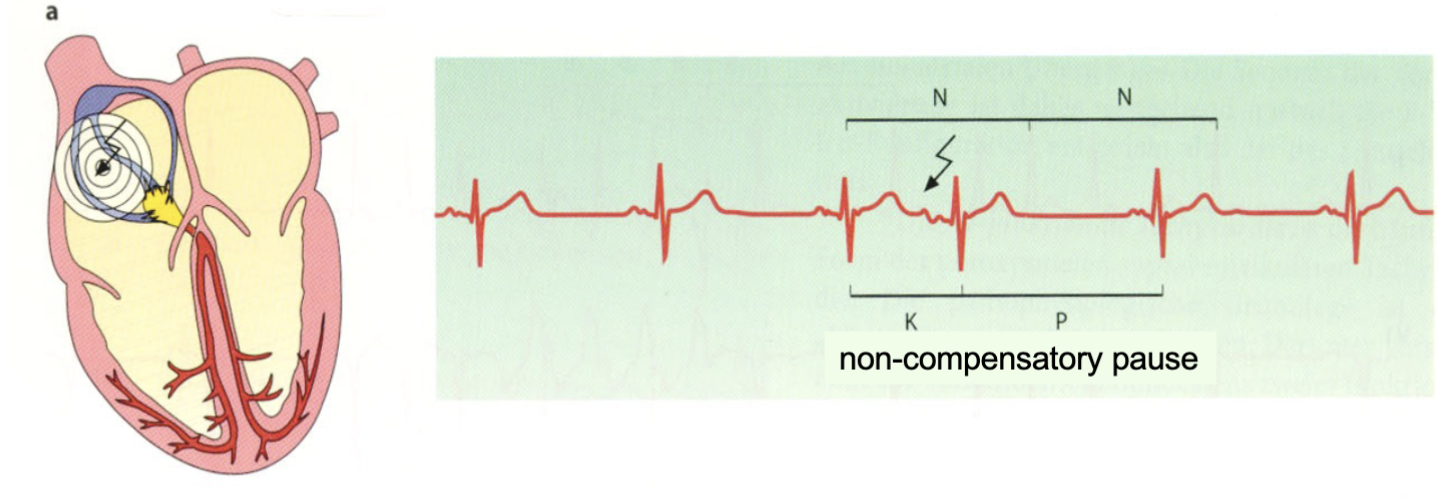
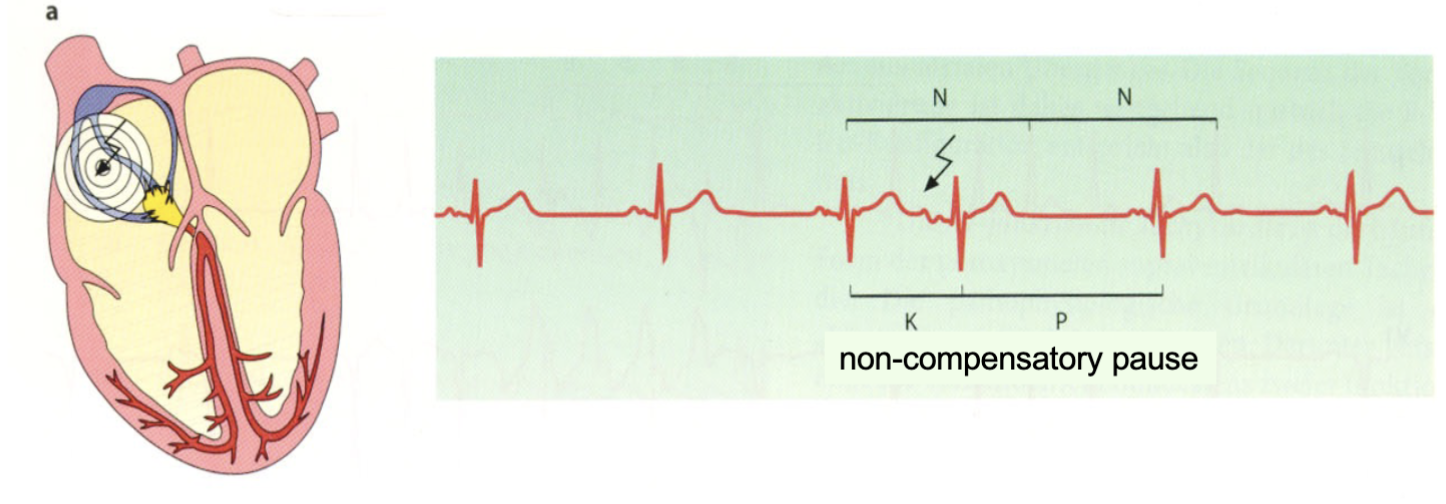
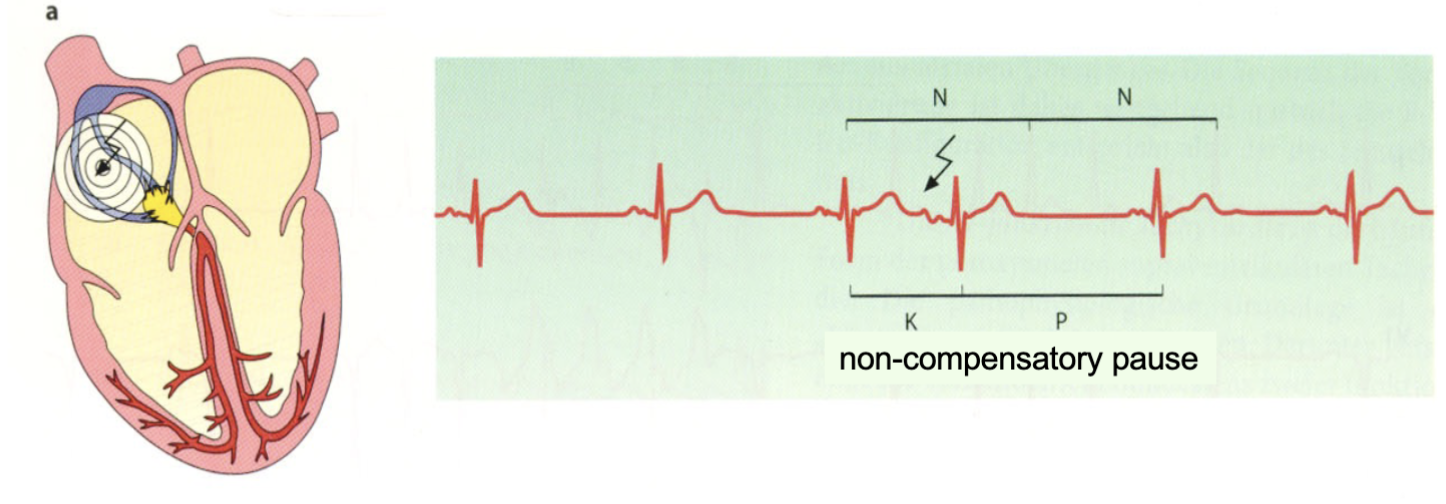
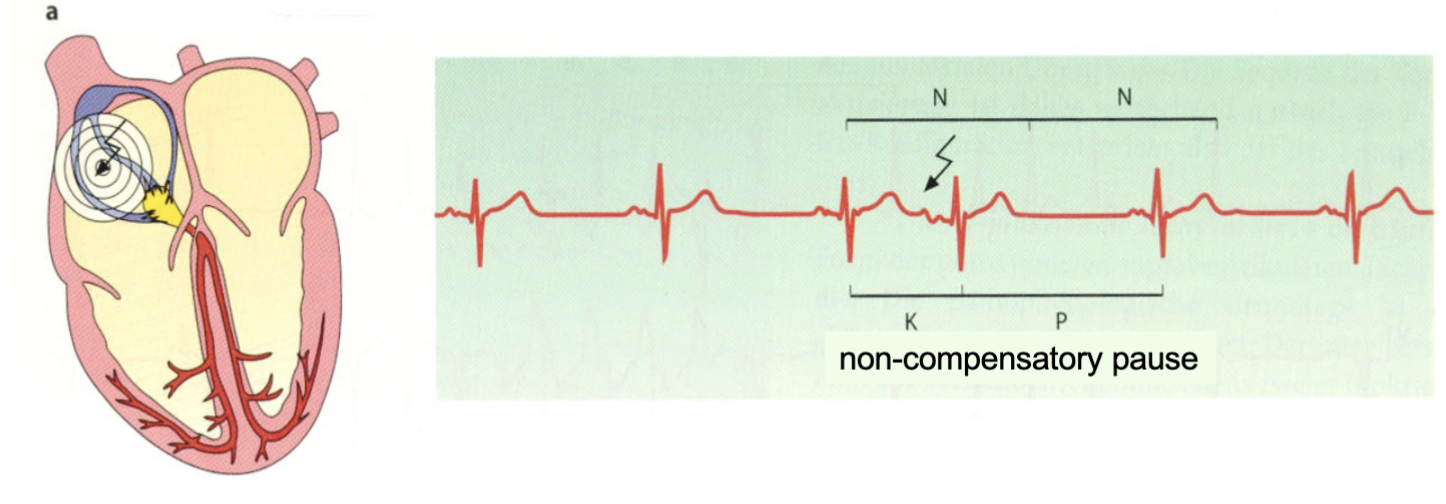
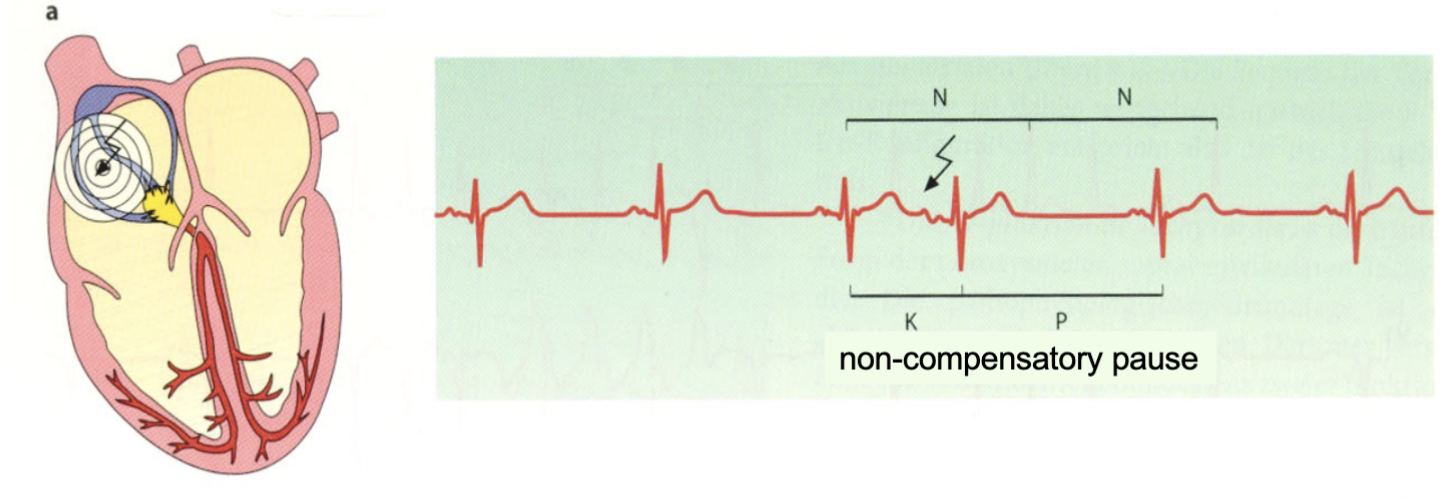
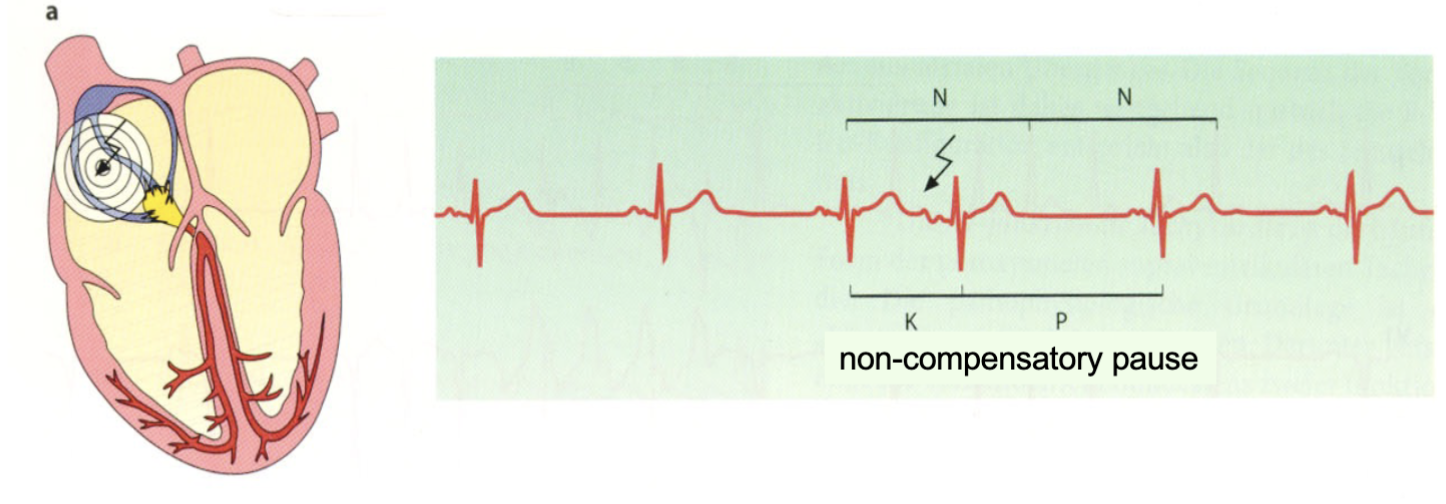
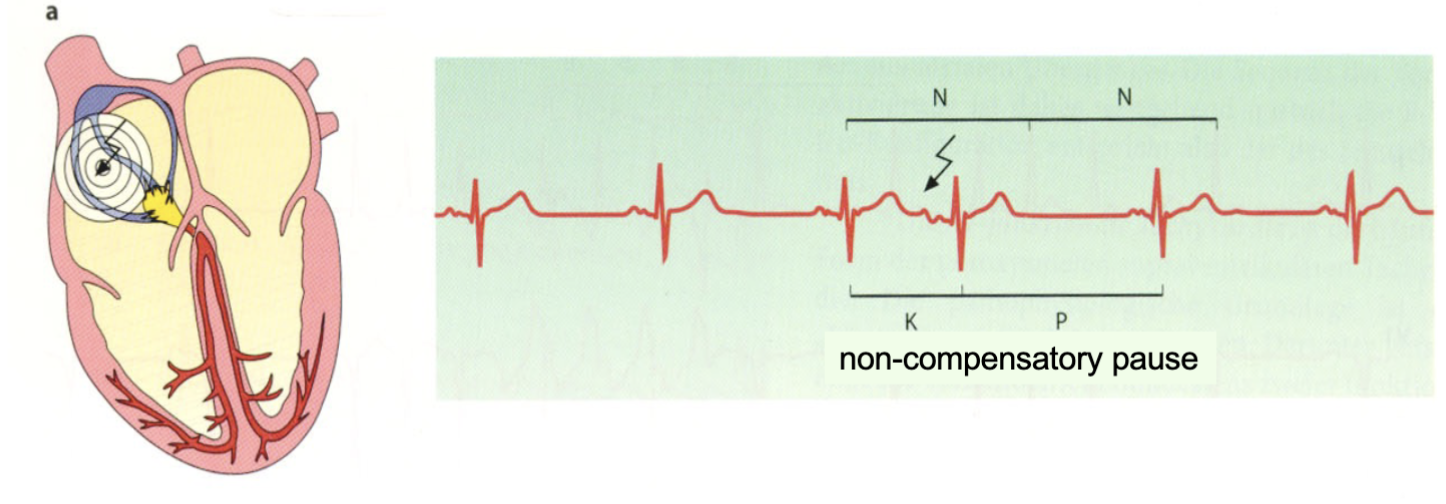
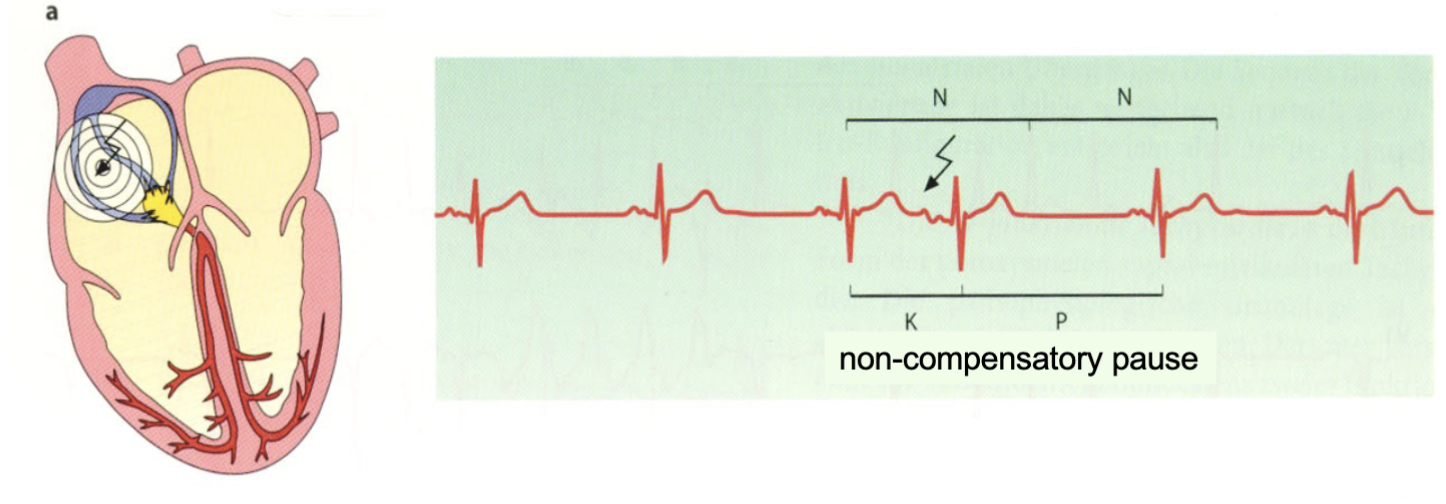
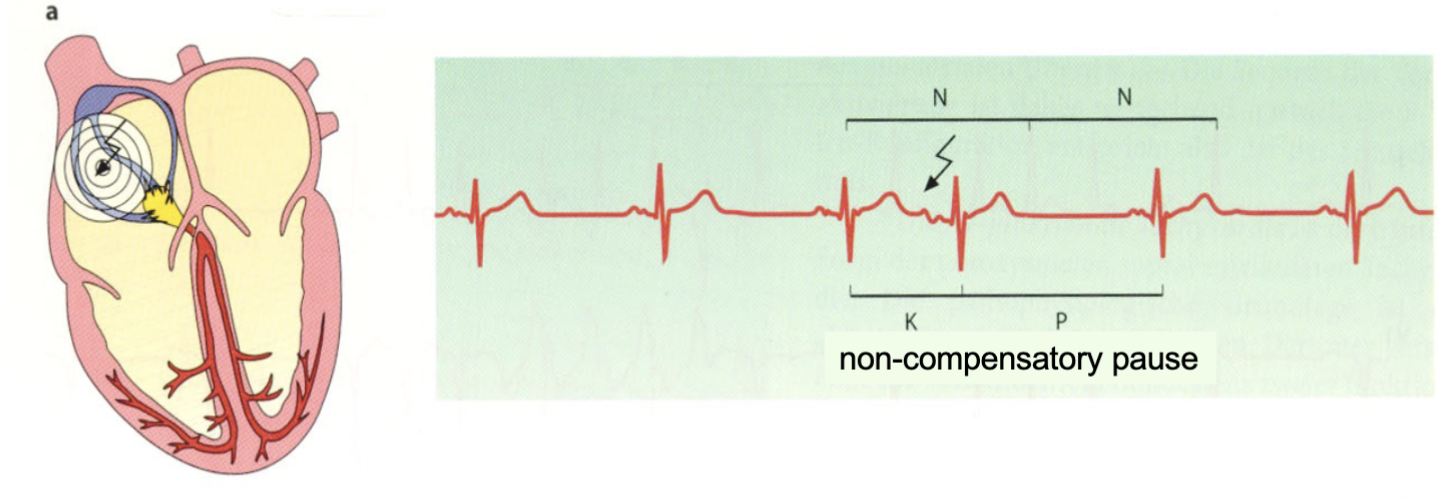
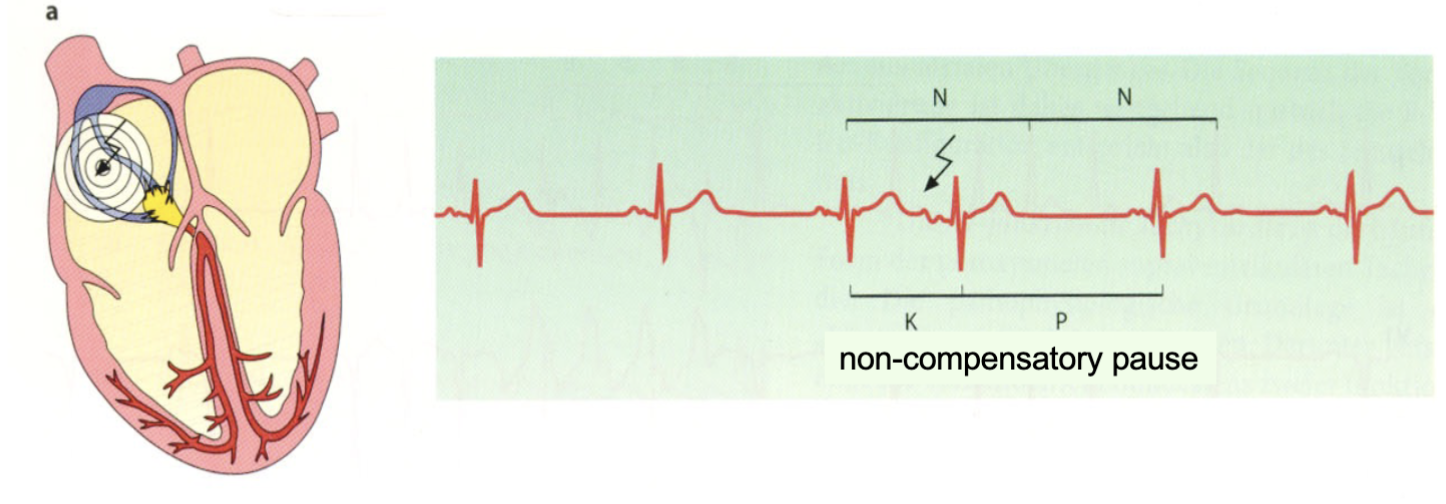
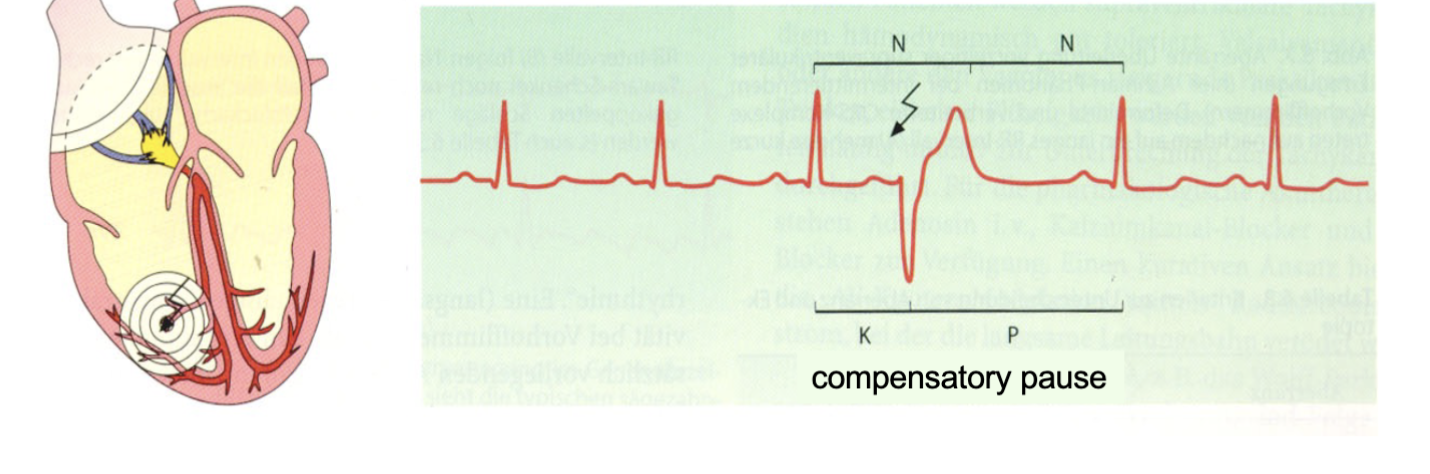
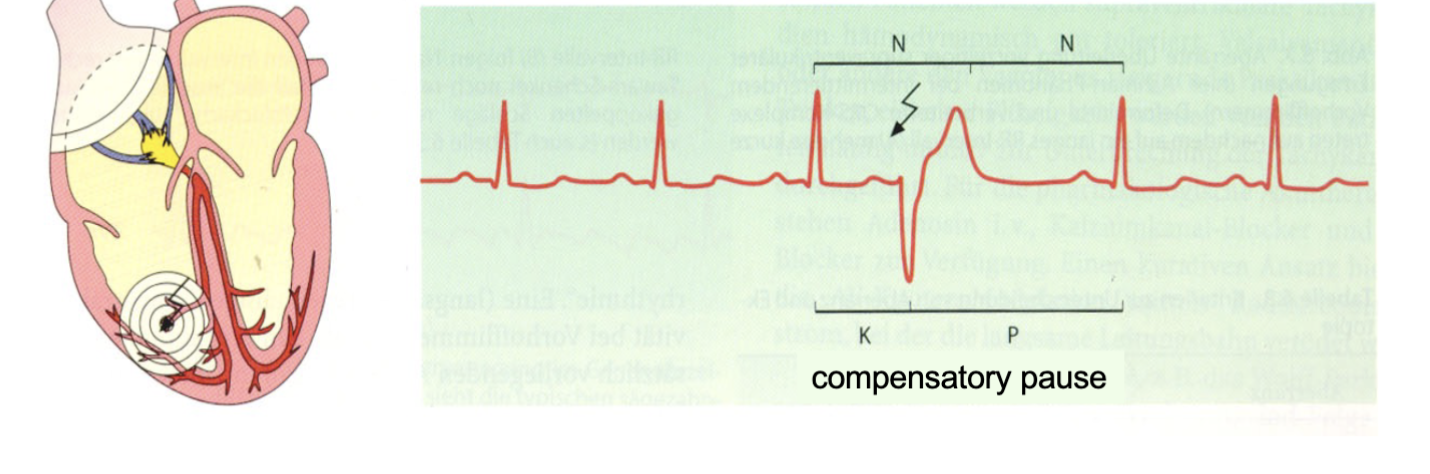
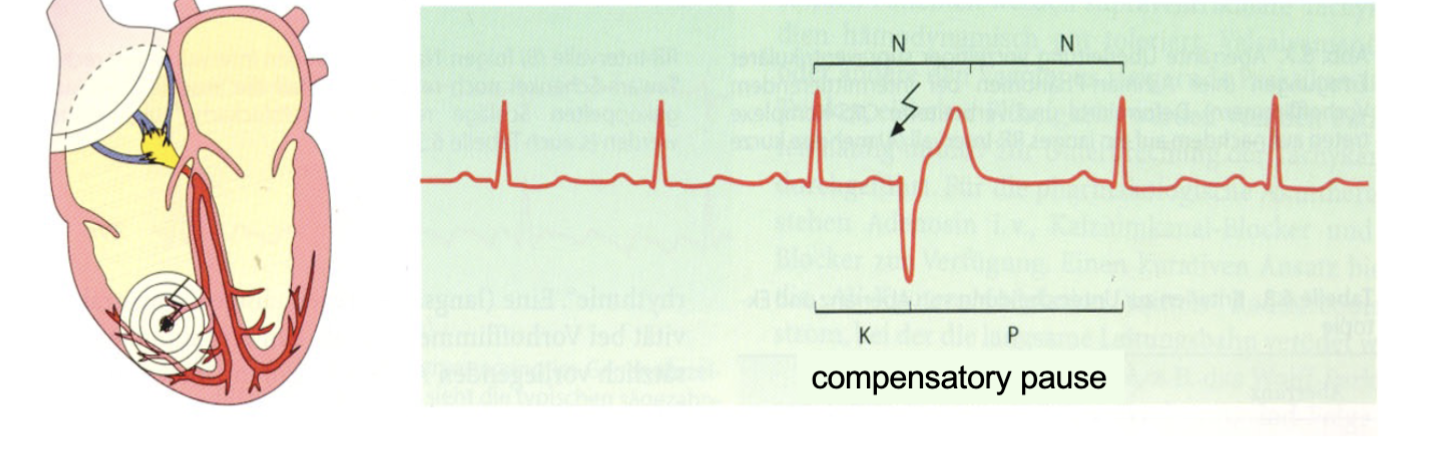
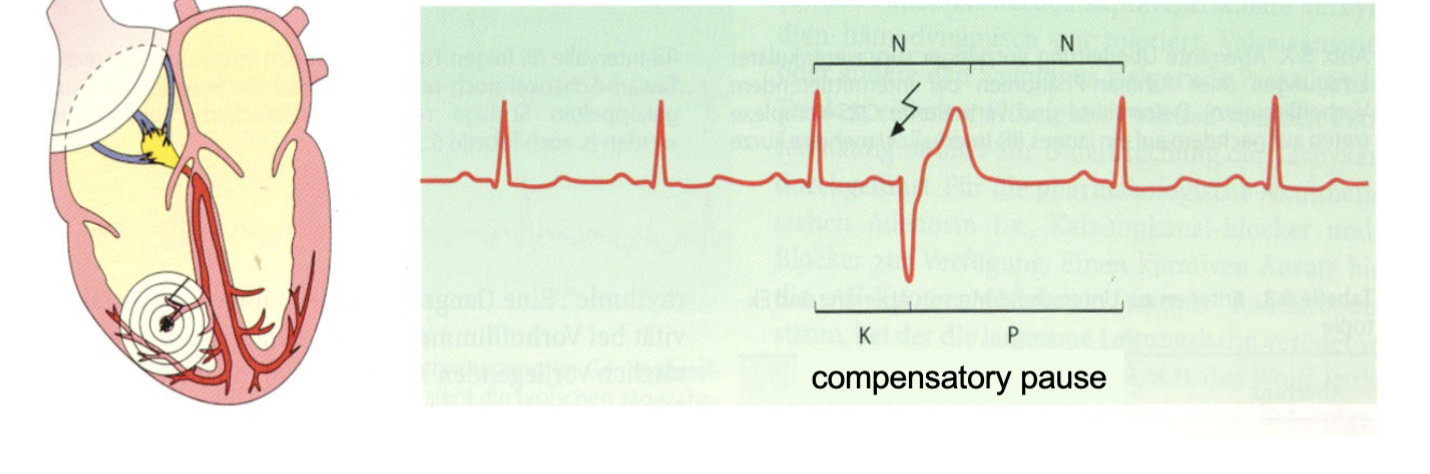
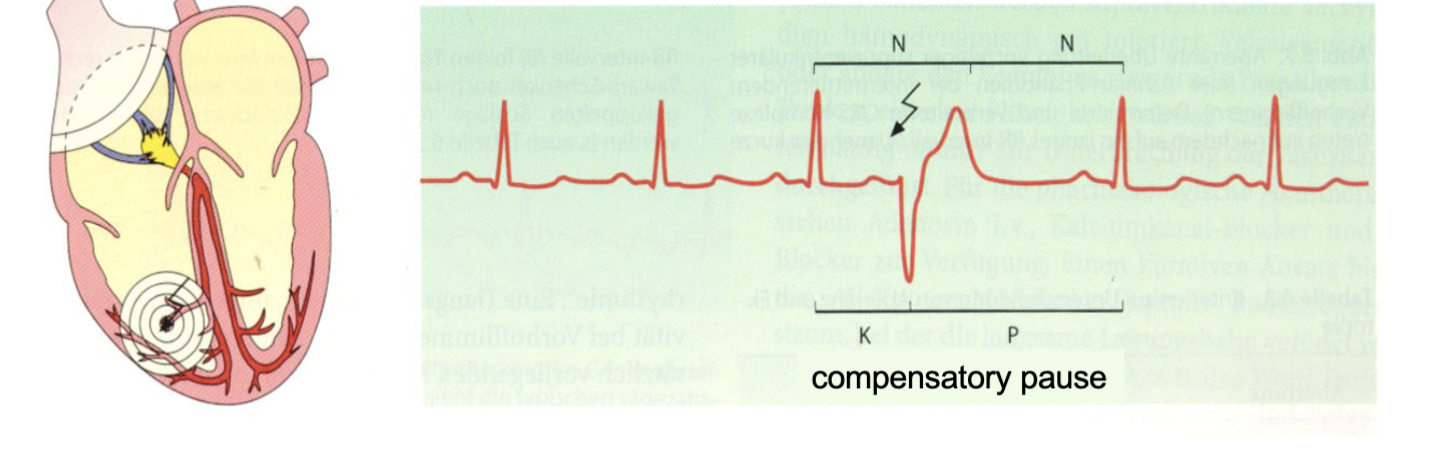
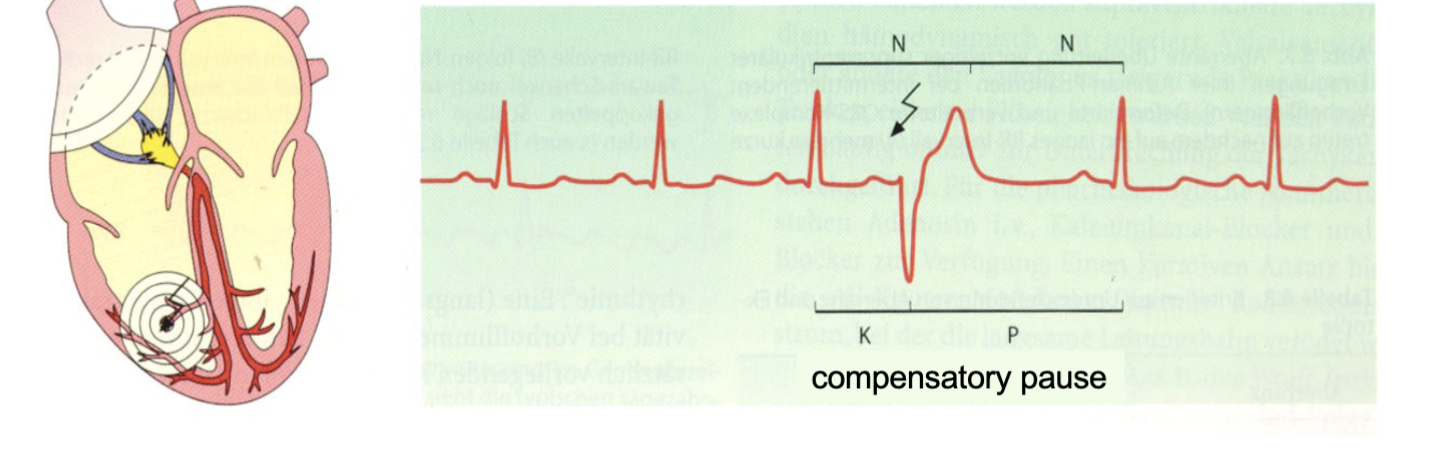
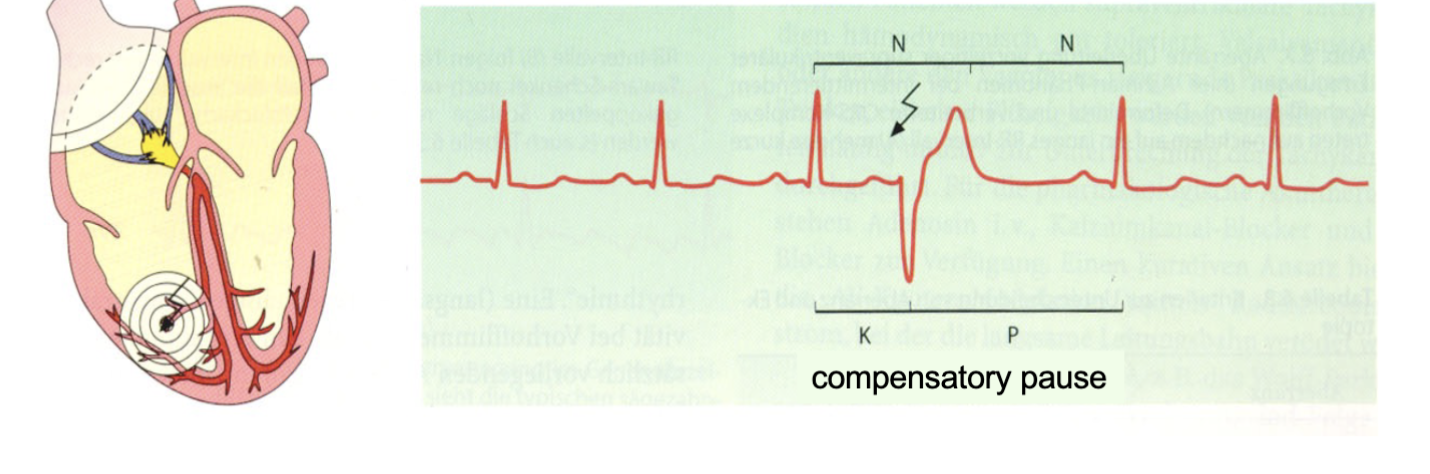
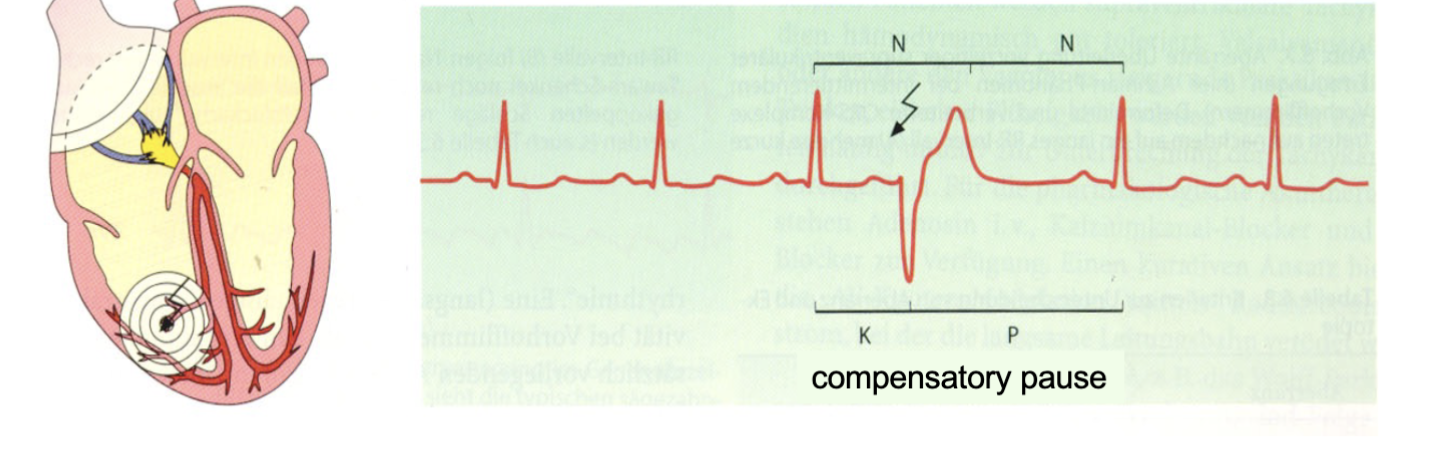
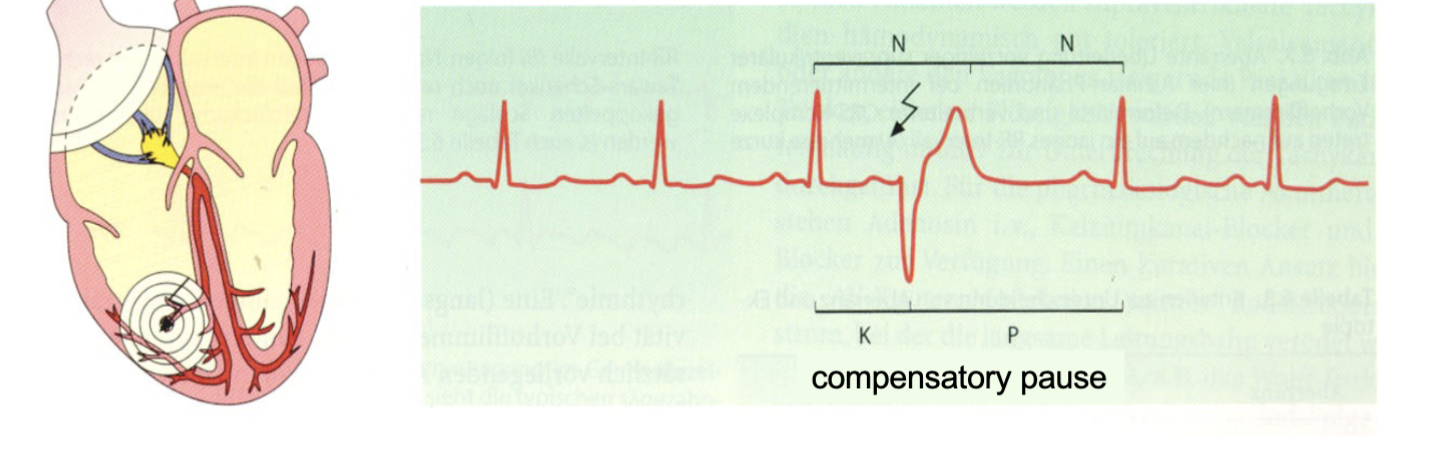
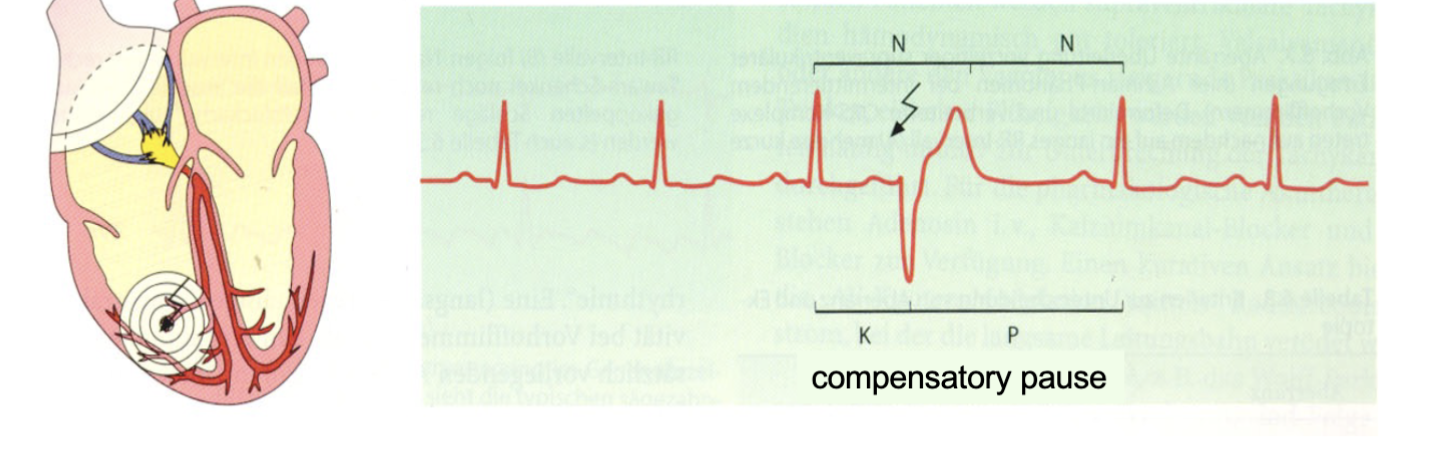
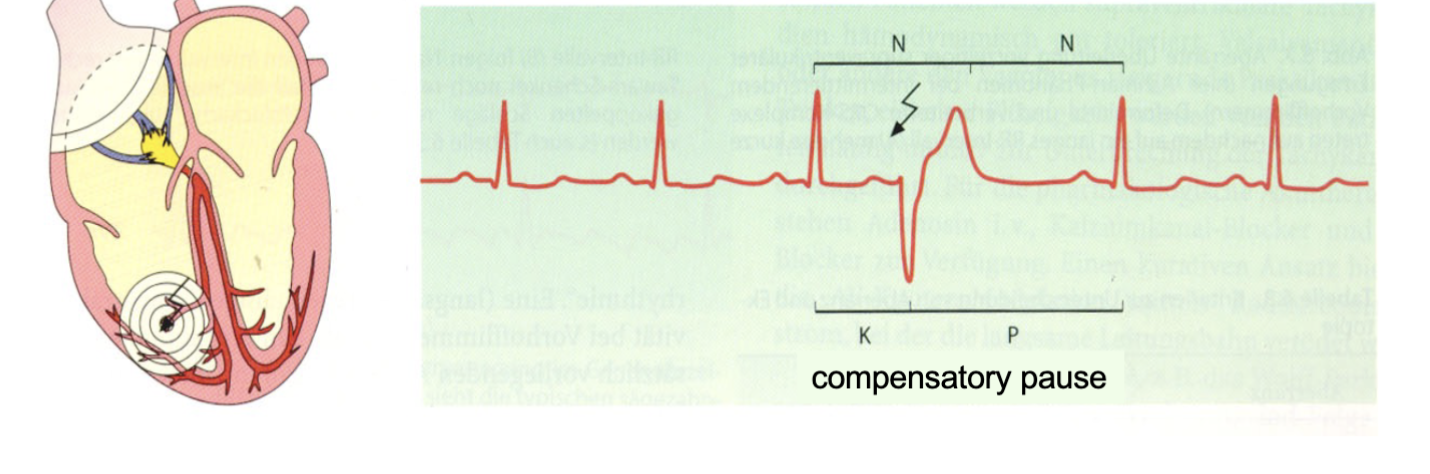
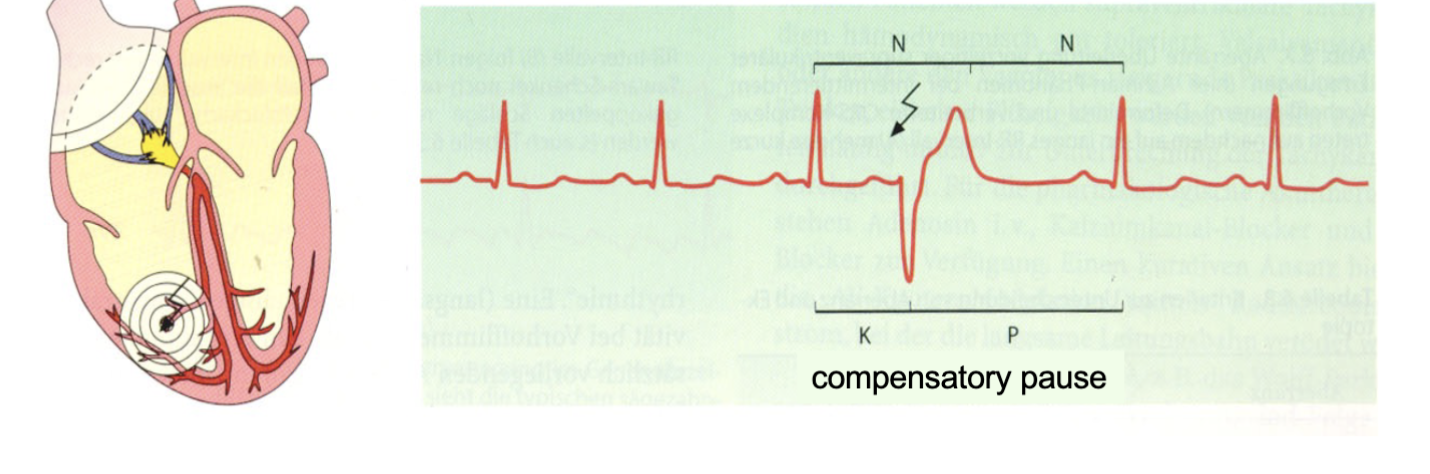
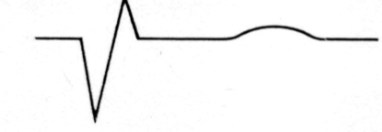
What are atrial premature complexes (APCs)?
Type of arrhythmia originating from ectopic focus in atria, causing premature depolarization of atria before next expected normal beat.
26
New cards
How are APCs identified on an ECG?
A P wave that is earlier than expected & usually different in shape compared to normal
P wave may also be inverted or hidden within the preceding T wave.
Following the APC, there may be a compensatory pause before the next normal beat.
P wave may also be inverted or hidden within the preceding T wave.
Following the APC, there may be a compensatory pause before the next normal beat.
27
New cards
Are APCs generally considered to be benign?
Yes, APCs especially if they occur infrequently & do not cause symptoms.
28
New cards
What are some potential causes of APCs?
Hpertension, coronary artery disease, valvular heart disease, & atrial fibrillation.
In some cases, lifestyle factors such as excessive caffeine or alcohol intake, smoking, & stress may also contribute to the development of APCs.
In some cases, lifestyle factors such as excessive caffeine or alcohol intake, smoking, & stress may also contribute to the development of APCs.
29
New cards
What is the treatment for APCs?
Adressing the underlying cause &/or using medications such as beta-blockers or calcium channel blockers to reduce the frequency of the APCs.
However, if the APCs occur frequently or are associated with symptoms such as palpitations or chest pain, further evaluation needed
However, if the APCs occur frequently or are associated with symptoms such as palpitations or chest pain, further evaluation needed
30
New cards
Does ventricular conduction typically change with APCs?
Typically not affected by APCs, as the premature depolarization occurs in the atria & the electrical signal still travels through the normal pathway to reach the ventricles.
31
New cards
What is a compensatory pause in the context of APCs?
Pause in the heart rhythm that occurs after an APC.
It is called compensatory because the heart takes a pause to "compensate" for the premature atrial contraction before resuming the regular rhythm.
It is called compensatory because the heart takes a pause to "compensate" for the premature atrial contraction before resuming the regular rhythm.
32
New cards
How is a compensatory pause measured on an ECG?
End of the APC to the beginning of the next normal beat. It is usually equal to two regular R-R intervals.
33
New cards
Are compensatory pauses always present with APCs?
No, not all APCs are followed by compensatory pauses. The presence or absence of a compensatory pause depends on the timing of the APC in relation to the underlying rhythm.
34
New cards
Why are compensatory pauses important to consider in APCs?
Help distinguish APCs from other types of arrhythmias.
Presence suggests that the premature beat is coming from the atria, while absence suggests that the premature beat is coming from the ventricles.
Help determine the origin of the APC & guide further evaluation & treatment if necessary.
Presence suggests that the premature beat is coming from the atria, while absence suggests that the premature beat is coming from the ventricles.
Help determine the origin of the APC & guide further evaluation & treatment if necessary.
35
New cards
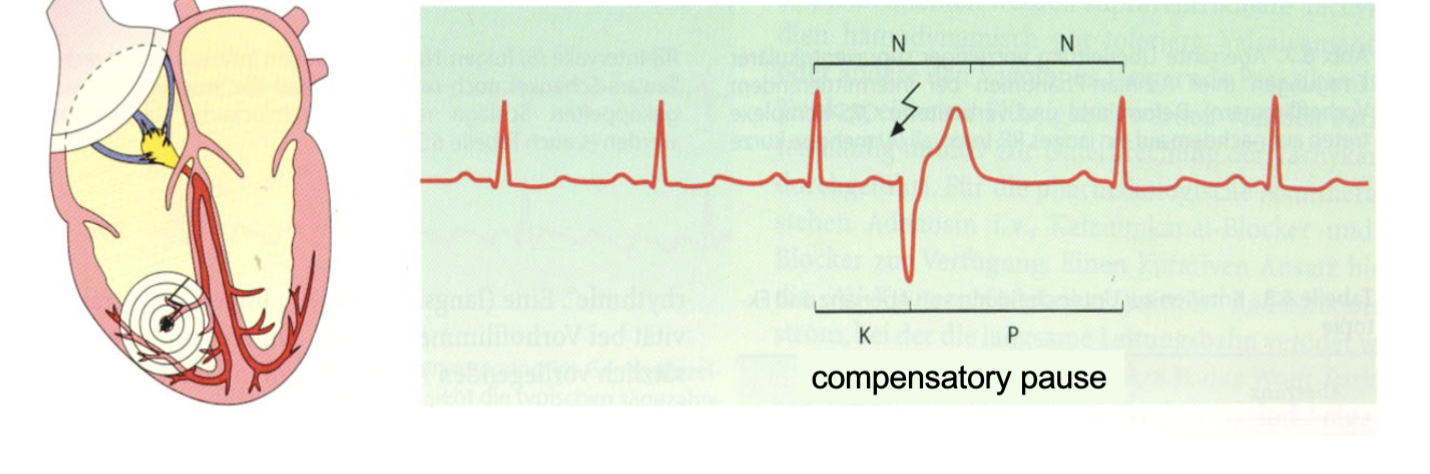
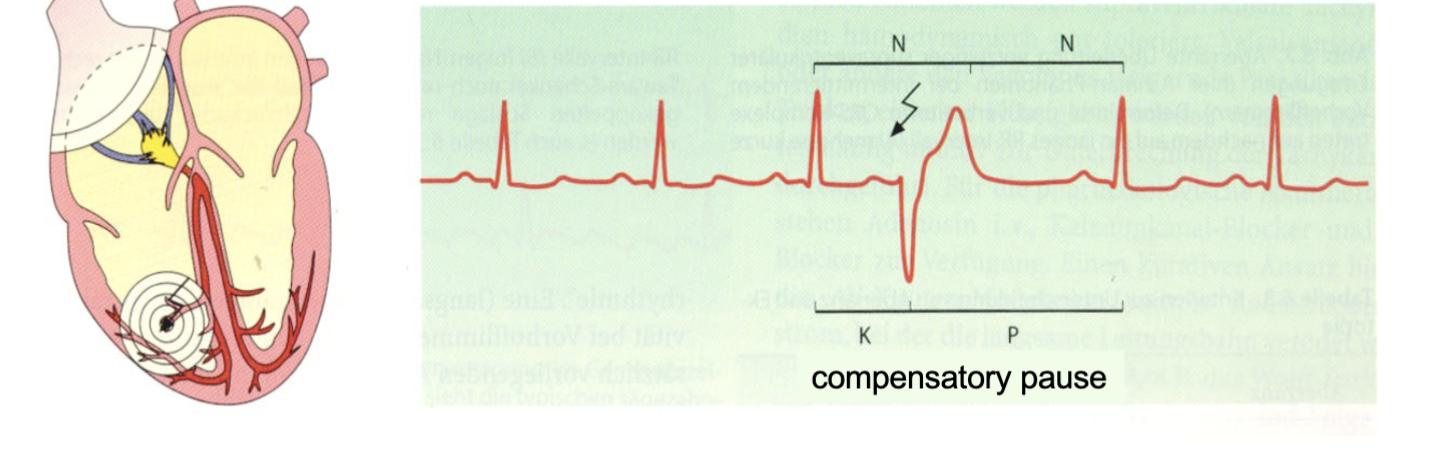
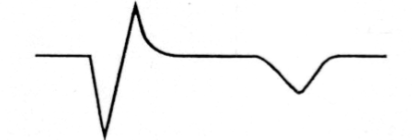
What are ventricular premature complexes (VPCs)?
Type of arrhythmia that originate from an ectopic focus in the ventricles, causing a premature depolarization of the ventricles before the next expected normal beat.
36
New cards
How does VPC affect ventricular conduction?
Premature depolarization occurs in the ventricles & can cause a delay in the normal electrical signal reaching the ventricles.
This can lead to a wide QRS complex on the ECG.
This can lead to a wide QRS complex on the ECG.
37
New cards
How does VPC affect the axis of depolarization?
Axis of depolarization is often altered in VPCs, as the electrical signal originates from an ectopic focus in the ventricles rather than the normal conduction system.
So change in the direction of the electrical signal & a shift in the axis of depolarization.
So change in the direction of the electrical signal & a shift in the axis of depolarization.
38
New cards
What is the typical appearance of the QRS complex & T wave in VPCs?
QRS complex in VPCs is typically wider & more abnormal in shape compared to the normal QRS complex.
T wave may also be abnormal in shape or direction.
T wave may also be abnormal in shape or direction.
39
New cards
How are ventricular premature complexes (VPCs) identified on an electrocardiogram (ECG)?
Pemature QRS complex that is wider & more bizarre in shape, & the T wave following the QRS complex may be in the opposite direction as expected.
Premature QRS complex may be preceded by a compensatory pause, & the rhythm may return to normal sinus rhythm after the VPC
Premature QRS complex may be preceded by a compensatory pause, & the rhythm may return to normal sinus rhythm after the VPC
40
New cards
Can VPCs occur in normal sinus rhythm?
Yes, VPCs can occur in normal sinus rhythm, but they may also occur in the setting of other arrhythmias such as ventricular tachycardia or ventricular fibrillation.
41
New cards
What are some potential causes of VPCs?
Underlying heart disease, electrolyte imbalances, stimulant use, & emotional stress. In some cases, no underlying cause can be identified.
42
New cards
What is the difference between a unifocal & multifocal VPC?
Unifocal VPC originates from a single ectopic focus in the ventricles, resulting in a consistent QRS morphology.
In contrast, a multifocal VPC arises from multiple ectopic foci, resulting in varying QRS morphologies.
In contrast, a multifocal VPC arises from multiple ectopic foci, resulting in varying QRS morphologies.
43
New cards
When should VPCs be evaluated further?
May be benign & not require treatment if they occur infrequently & are not associated with symptoms.
However, if they occur frequently or are associated with symptoms such as palpitations, lightheadedness, or syncope, further evaluation may be necessary to determine the underlying cause & appropriate management.
However, if they occur frequently or are associated with symptoms such as palpitations, lightheadedness, or syncope, further evaluation may be necessary to determine the underlying cause & appropriate management.
44
New cards
What is the potential risk of frequent VPCs?
More serious arrhythmias, such as ventricular tachycardia or ventricular fibrillation, which can be life-threatening. Therefore, it is important to monitor & manage VPCs appropriately to prevent the development of more severe arrhythmias.
How is ventricular conduction affected in ventricular premature complexes (VPCs)?
How is ventricular conduction affected in ventricular premature complexes (VPCs)?
45
New cards
What is the axis of depolarization in VPCs?
May be different from the normal axis, which can help identify the origin of the premature beat.
46
New cards
How do VPCs affect the T wave on the ECG?
Abnormal T wave, which may be opposite in polarity to the QRS complex & may be described as "discordant."
47
New cards
How is the compensatory pause related to ventricular premature complexes (VPCs)?
Following a VPC, there is a compensatory pause during which the heart "resets" & prepares for the next normal beat.
48
New cards
How long is the compensatory pause in ventricular premature complexes (VPCs)?
Equal to the length of two normal cardiac cycles (i.e., the time between the preceding normal beat & the VPC plus the time between the VPC & the subsequent normal beat).
49
New cards
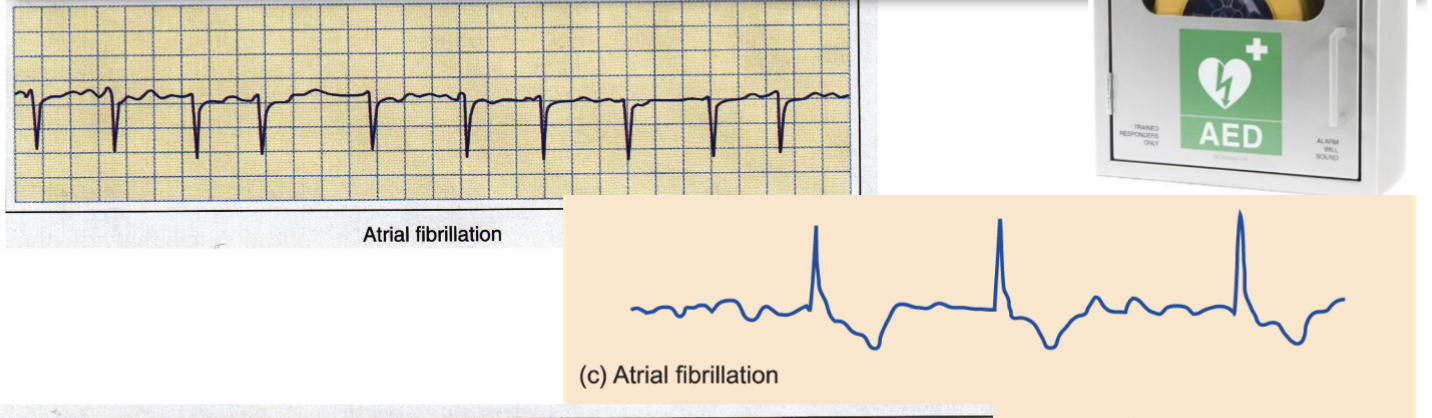
What is atrial fibrillation?
Arhythmia (abnormal heart rhythm) in which the upper chambers of the heart (atria) beat irregularly & faster than normal.
50
New cards
What are the causes of atrial fibrillation?
Age, ↑↑↑ blood pressure, heart disease, obesity, sleep apnea, thyroid disorders, & excessive alcohol or caffeine intake.
51
New cards
What are the symptoms of atrial fibrillation?
Heart palpitations, shortness of breath, fatigue, dizziness, chest discomfort, & fainting.
52
New cards
What is the treatment for atrial fibrillation?
Medications to control heart rate & rhythm, procedures to restore normal heart rhythm (such as cardioversion), & lifestyle changes to manage underlying conditions.
53
New cards
What does an ECG of atrial fibrillation look like?
Irregularly irregular rhythm with no discernible P waves & an irregular ventricular response.
54
New cards
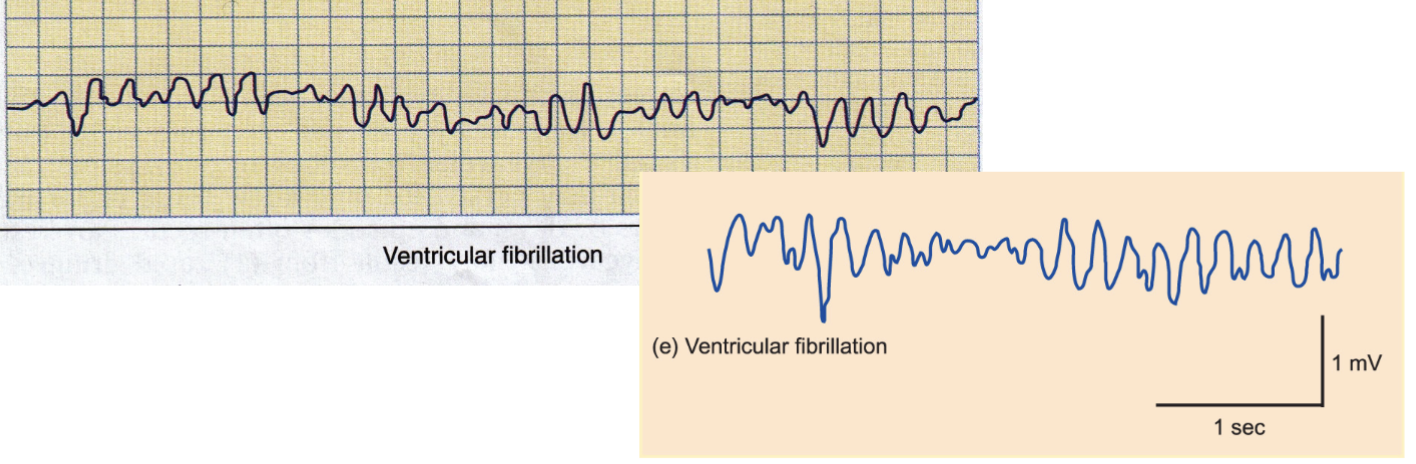
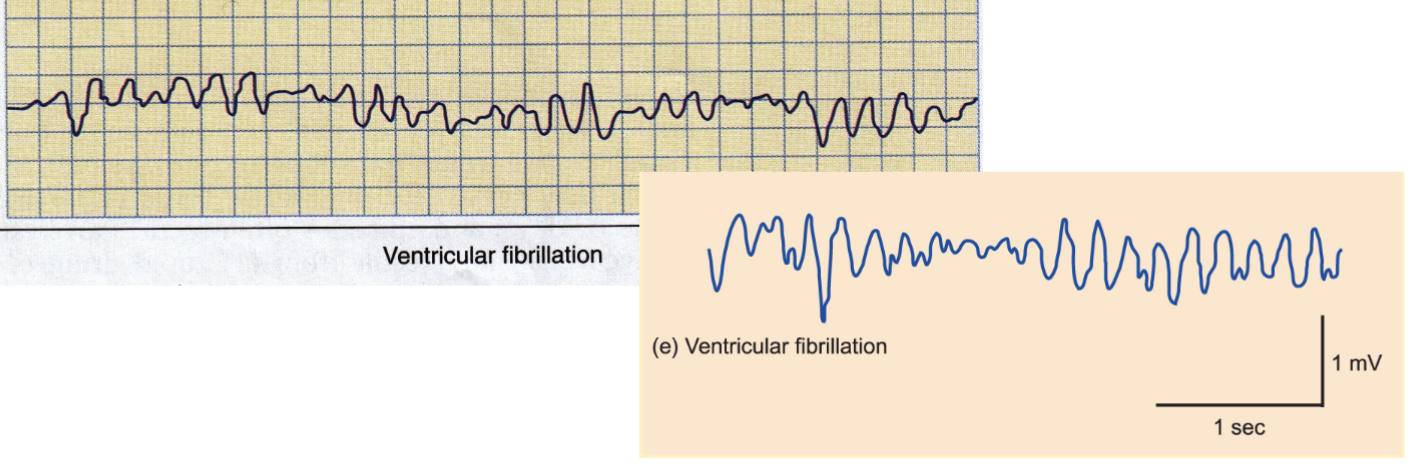
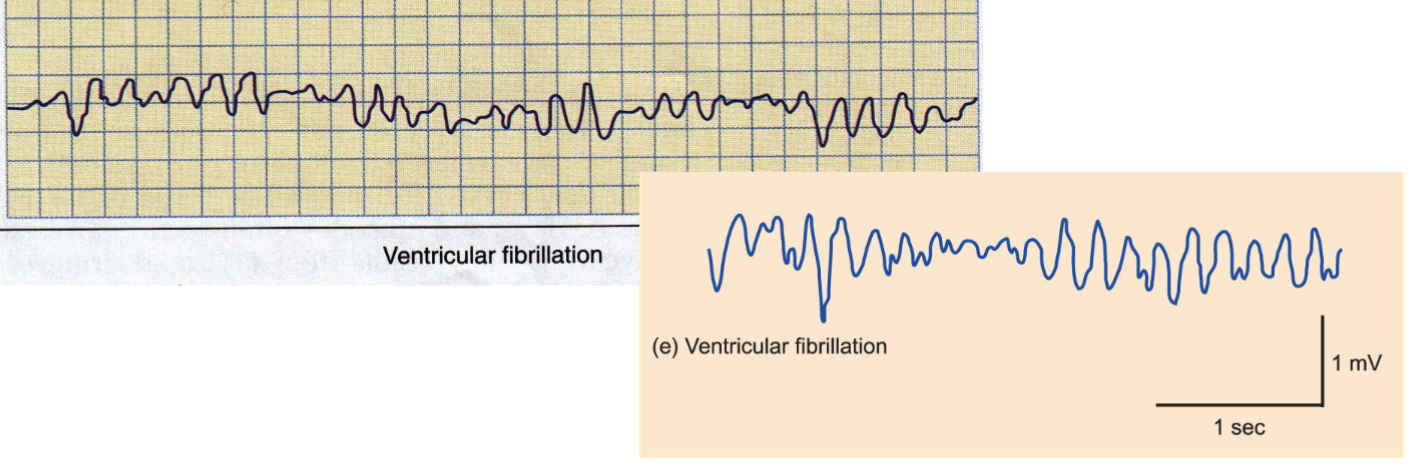
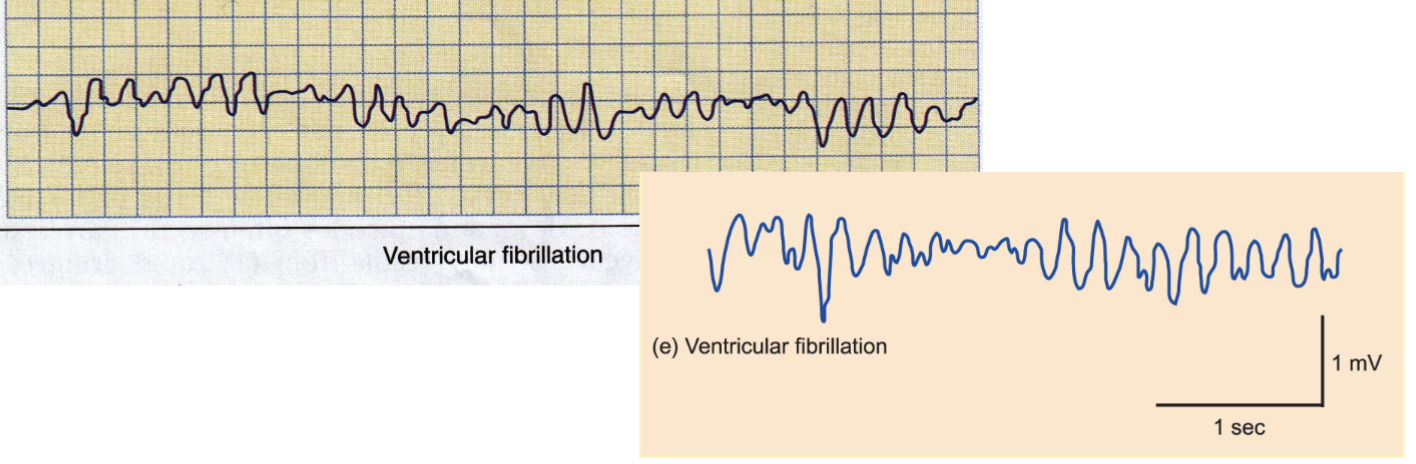
What does an ECG of ventricular fibrillation look like?
Chaotic & disorganized pattern with no clear P waves or QRS complexes, & irregularly irregular ventricular rhythm.
55
New cards
What is ventricular fibrillation?
Life-threatening arrhythmia in which the lower chambers of the heart (ventricles) quiver & cannot pump blood effectively.
56
New cards
What are the causes of ventricular fibrillation?
Heart disease, heart attack, electrocution, drowning, drug overdose, or trauma to the chest.
57
New cards
What are the symptoms of ventricular fibrillation?
Sudden loss of consciousness, no pulse, no breathing, & sometimes seizures.
58
New cards
What is the treatment for ventricular fibrillation?
CPR) & defibrillation with an automated external defibrillator (AED) or other medical equipment to shock the heart back into a normal rhythm.
Continued management may involve medications, implantable devices, & lifestyle changes
Continued management may involve medications, implantable devices, & lifestyle changes
59
New cards
What is ischemic heart disease?
A group of conditions that occur due to a reduced blood supply to the heart muscle, typically caused by narrowed or blocked coronary arteries.
60
New cards
What is normal myocardial blood flow?
Provides adequate oxygen & nutrients to the heart muscle to sustain its metabolic needs.
61
New cards
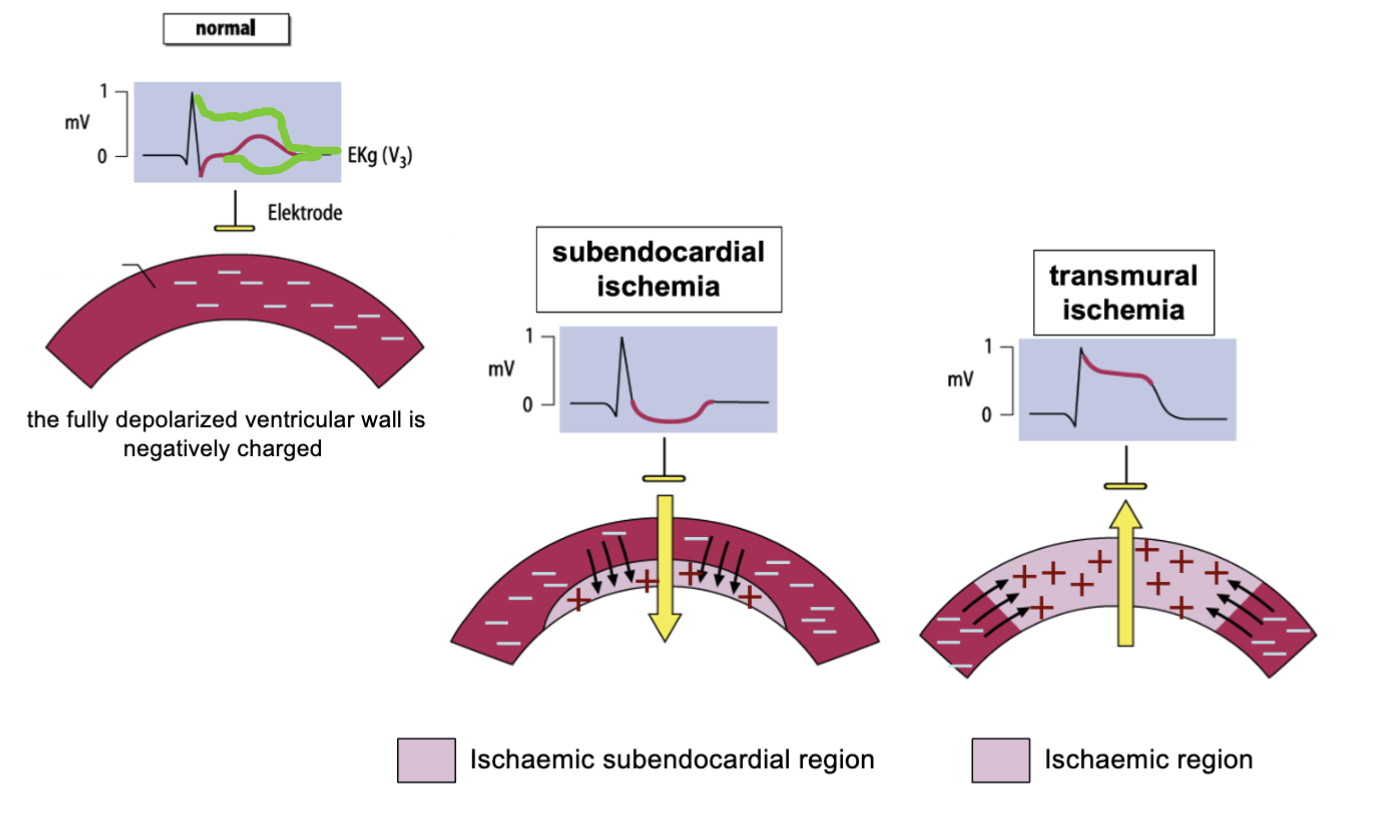
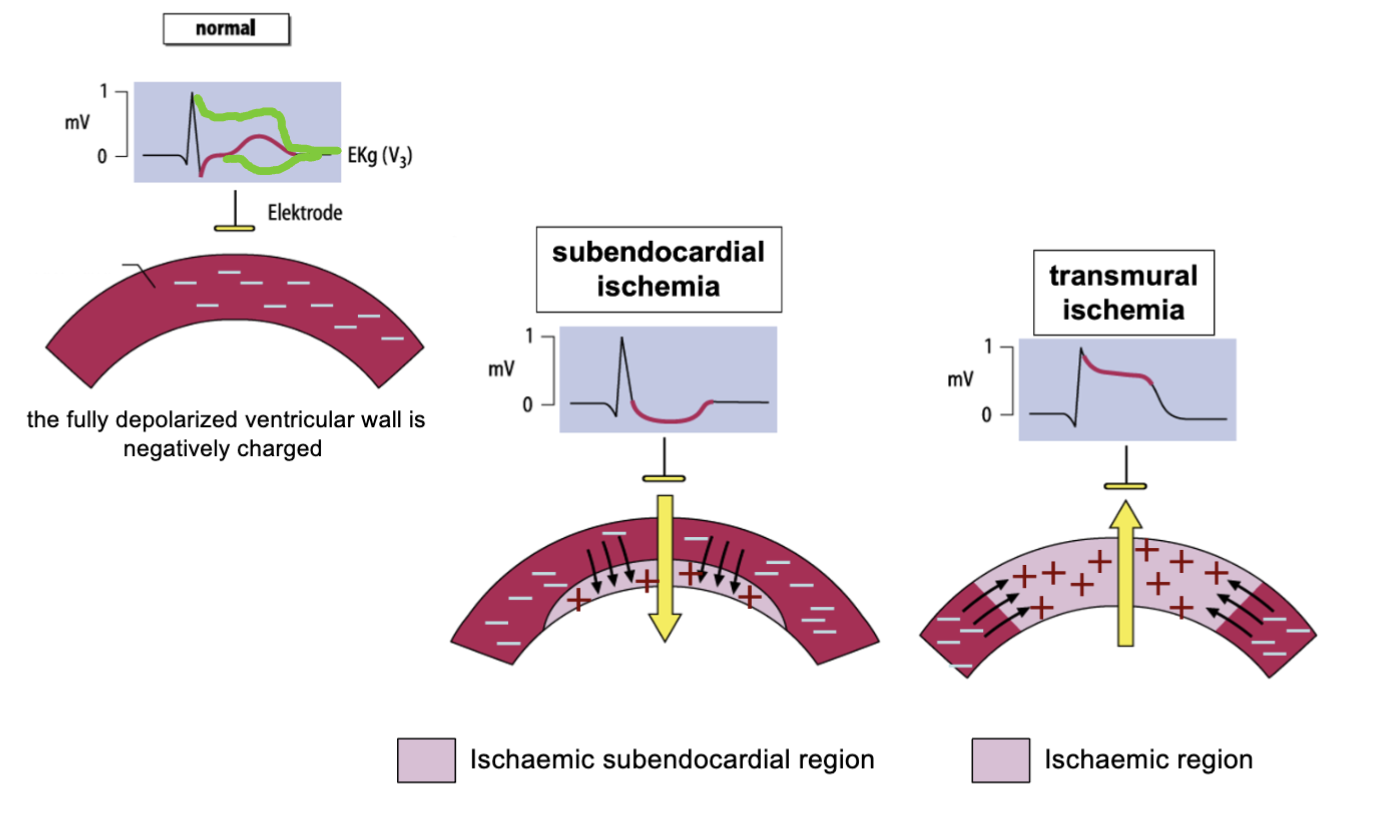
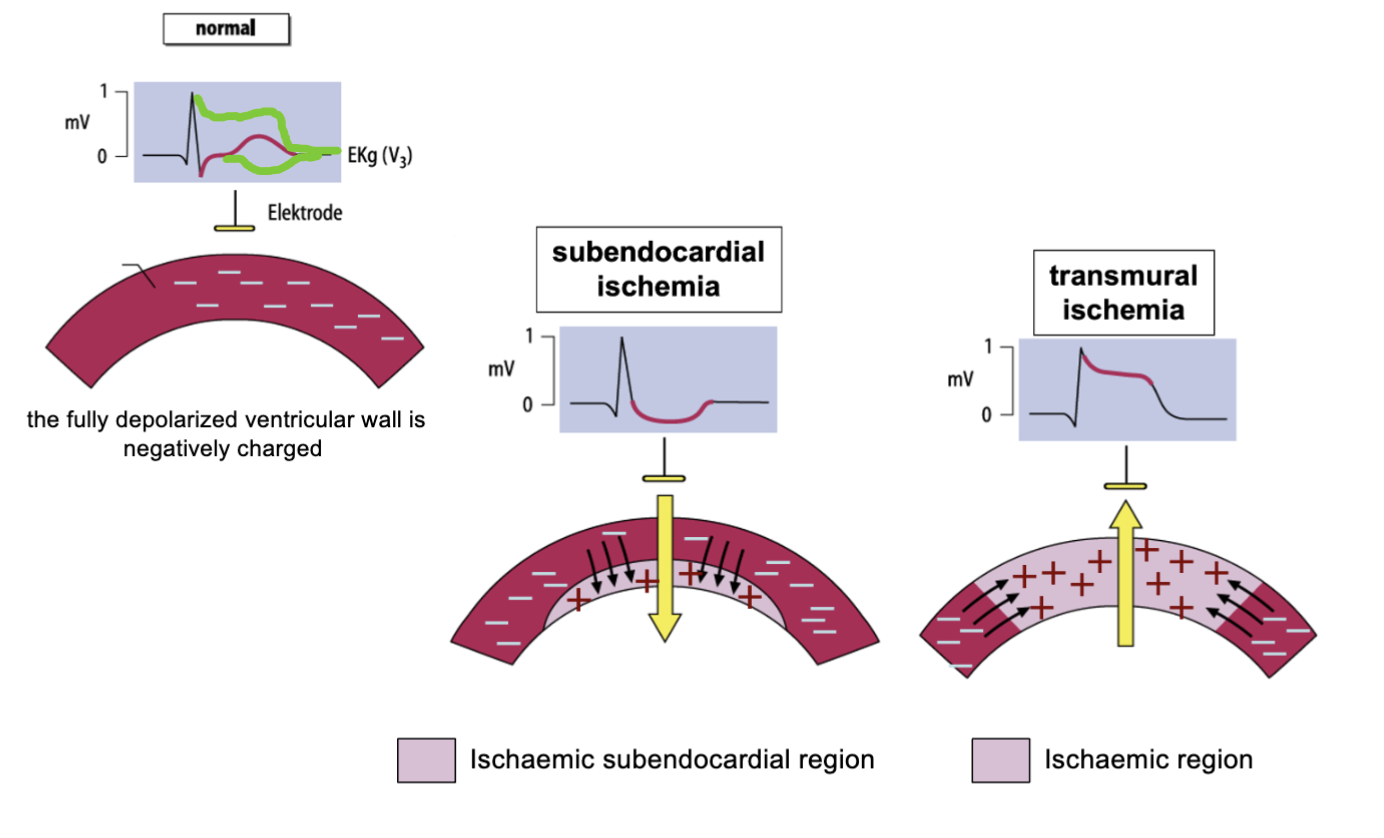
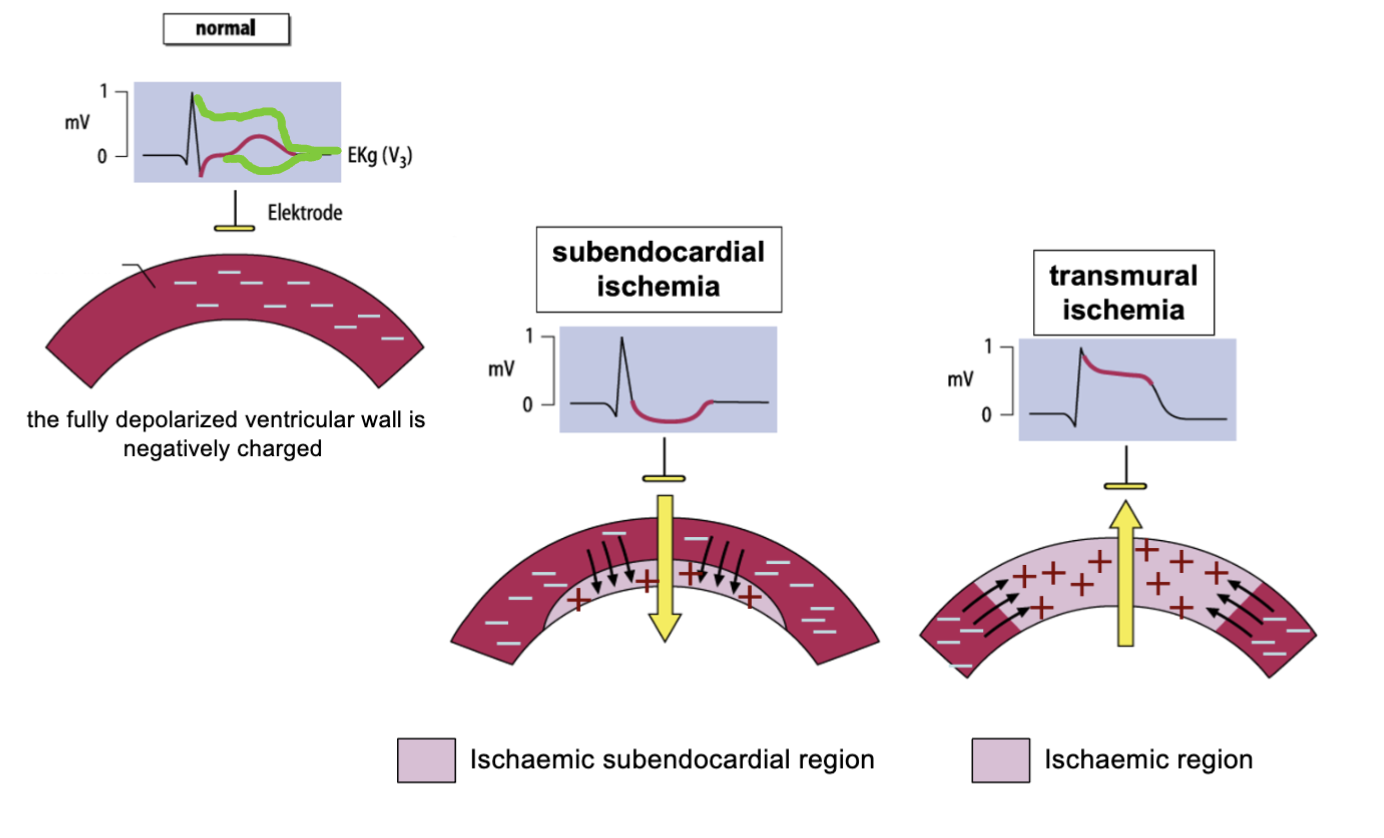
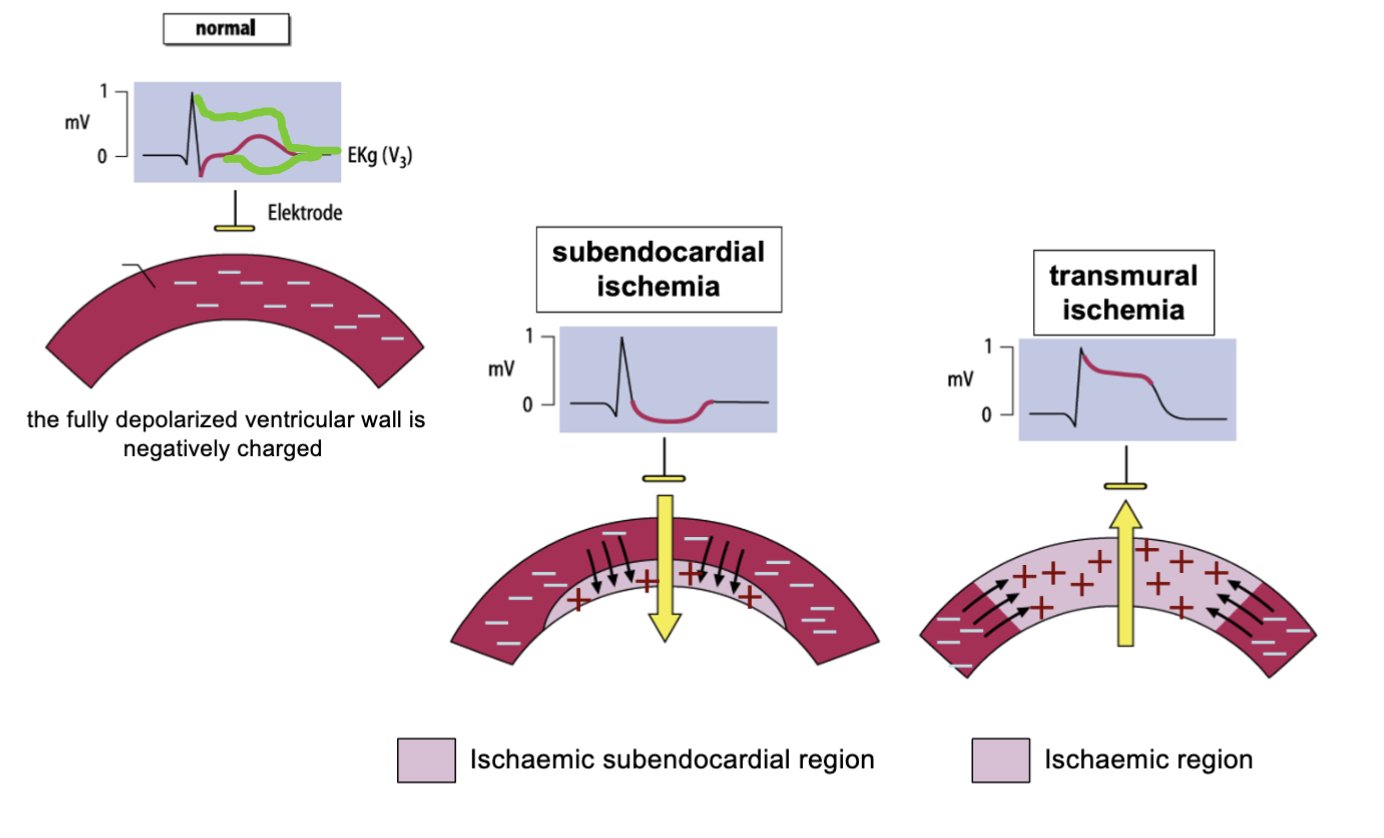
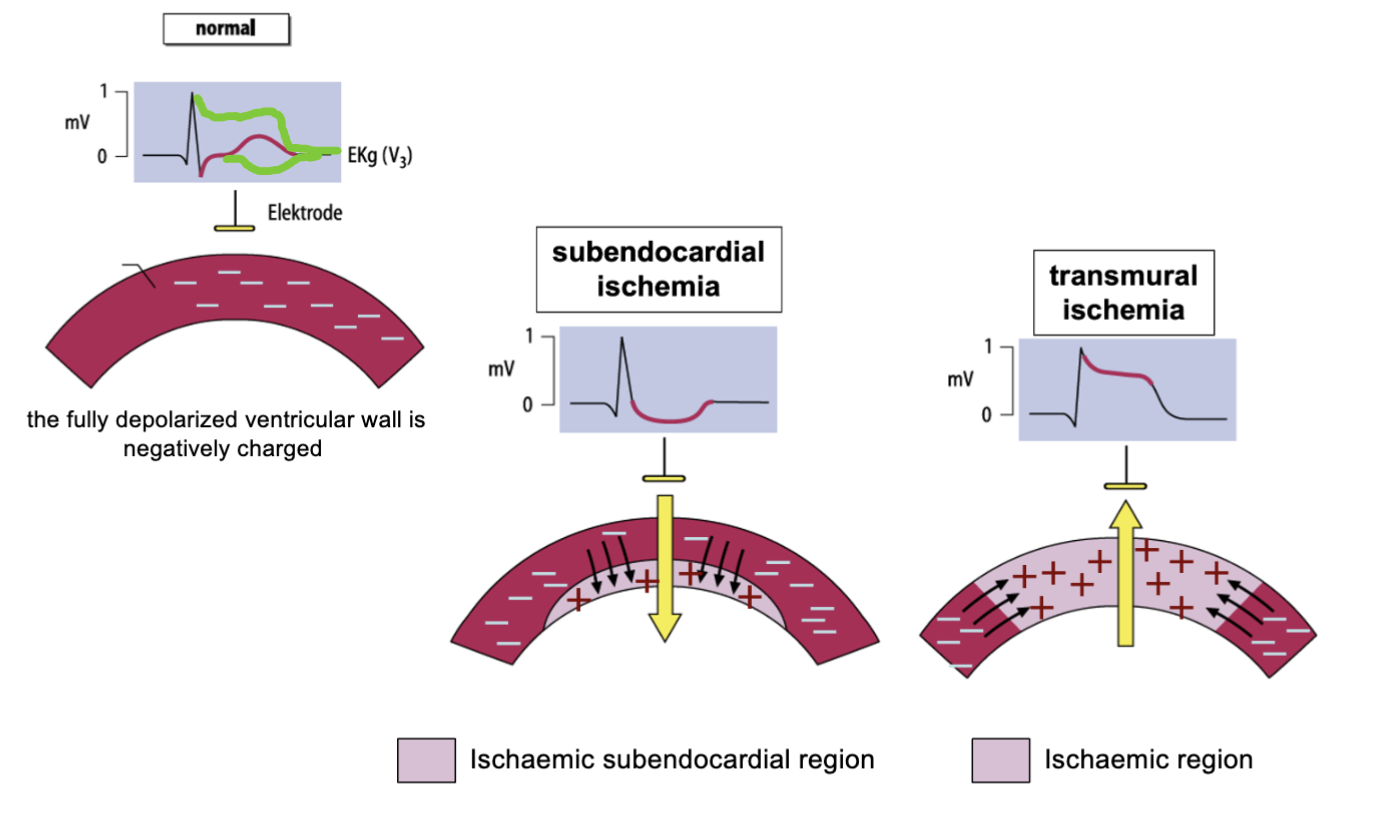
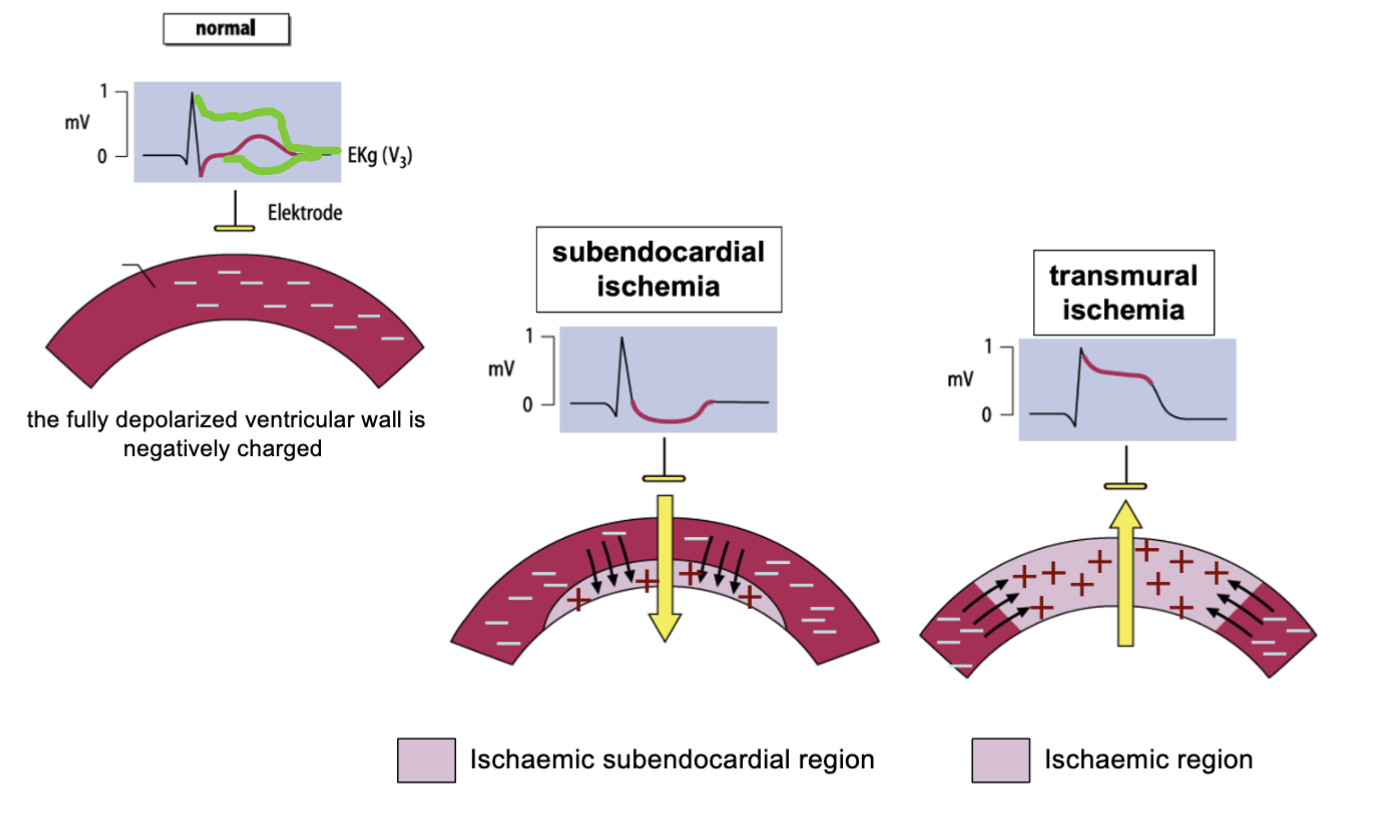
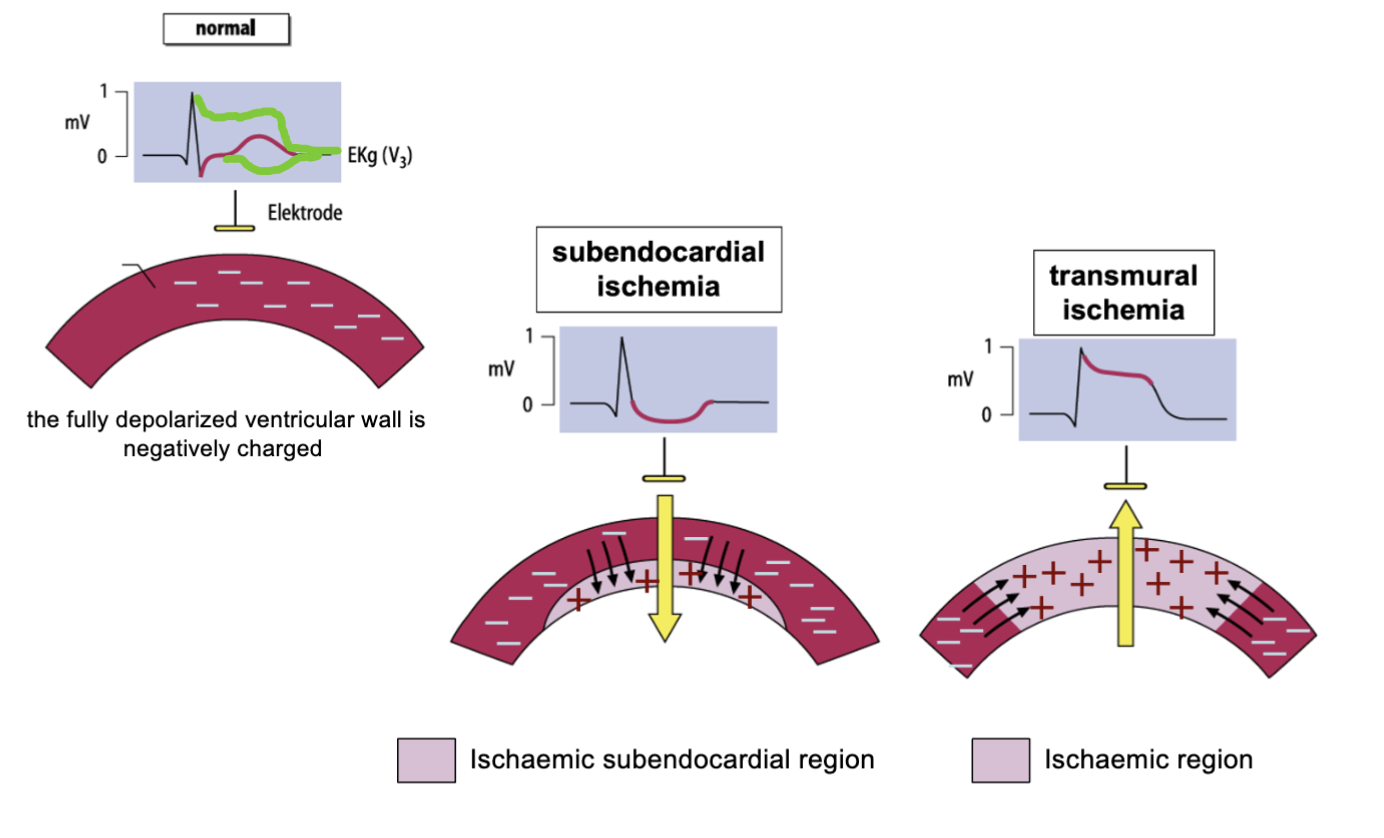
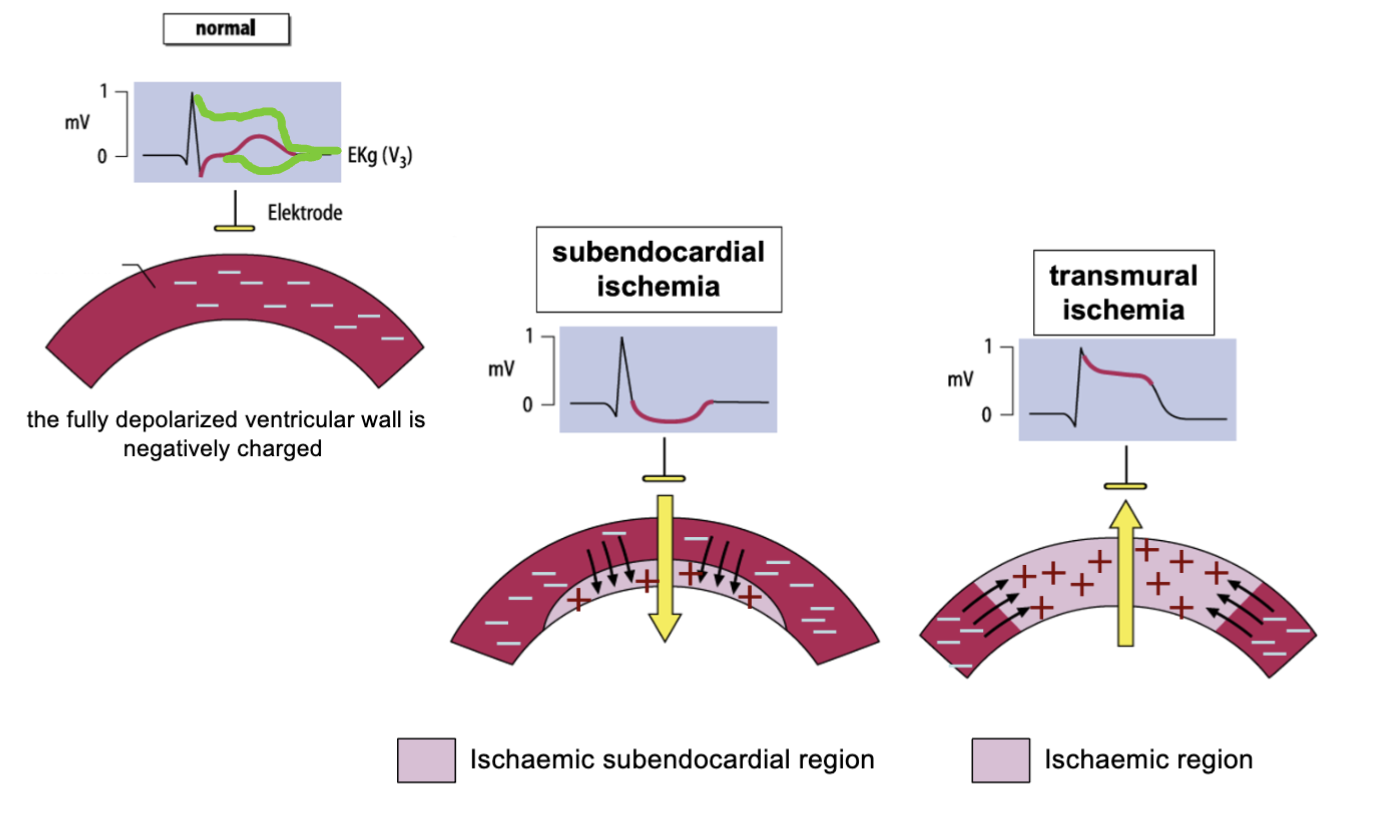
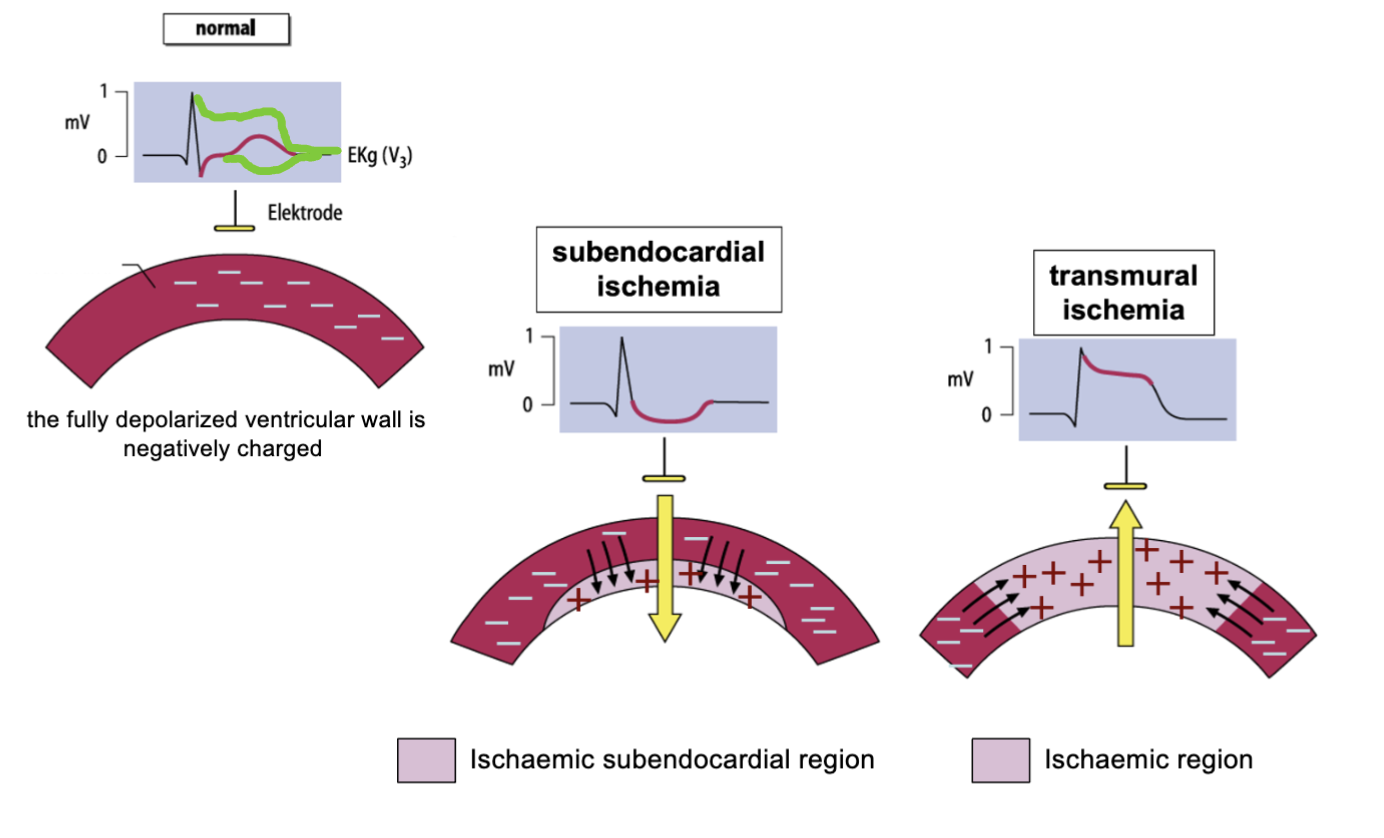
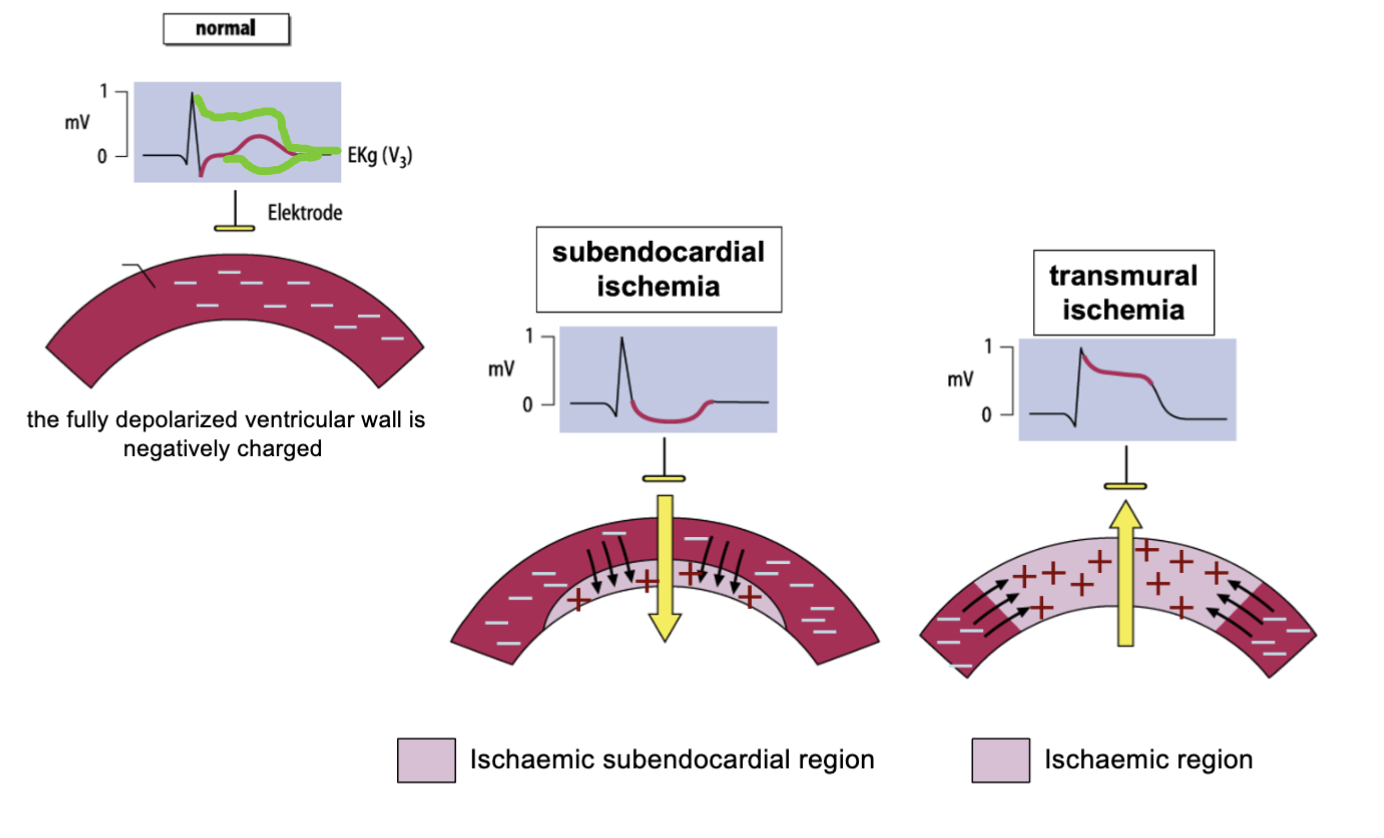
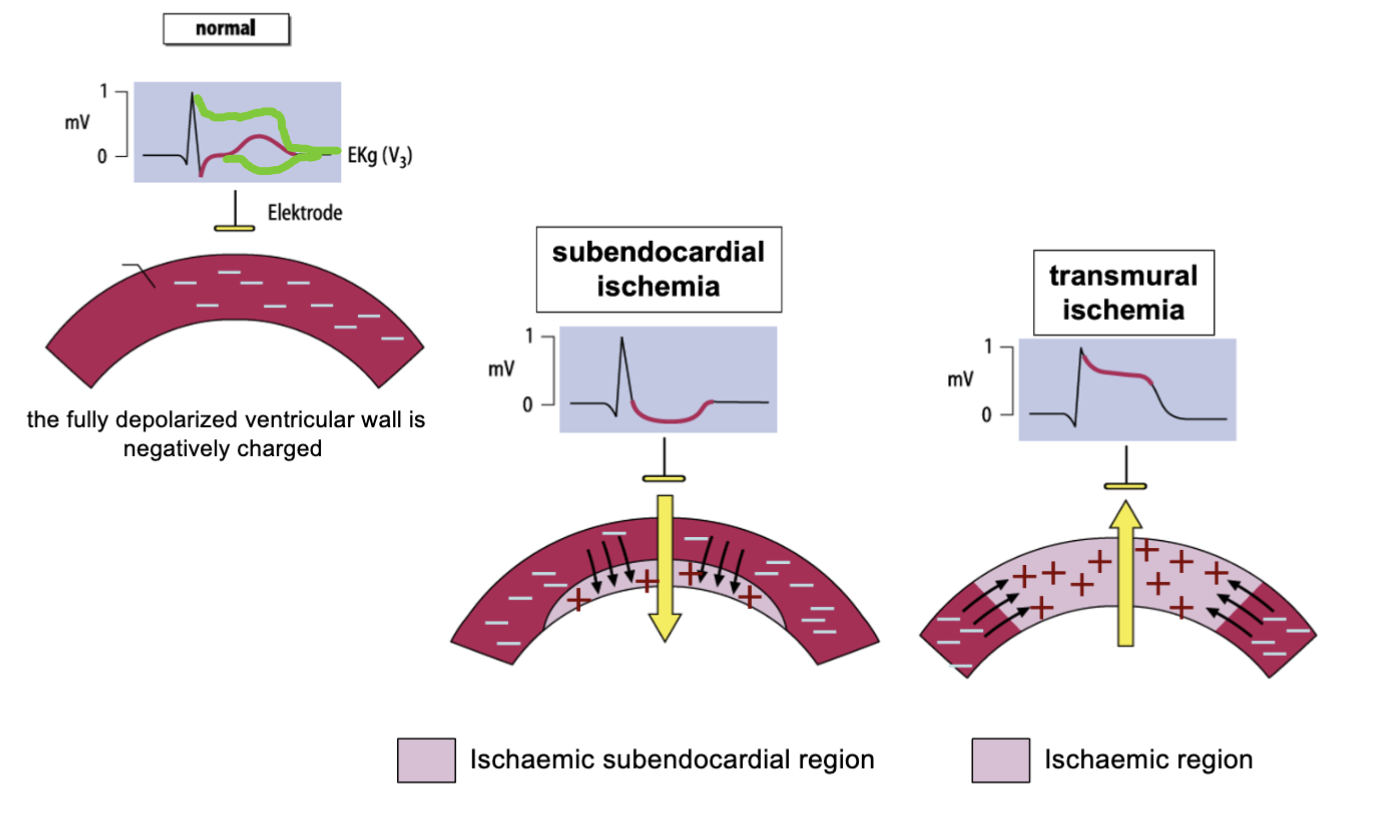
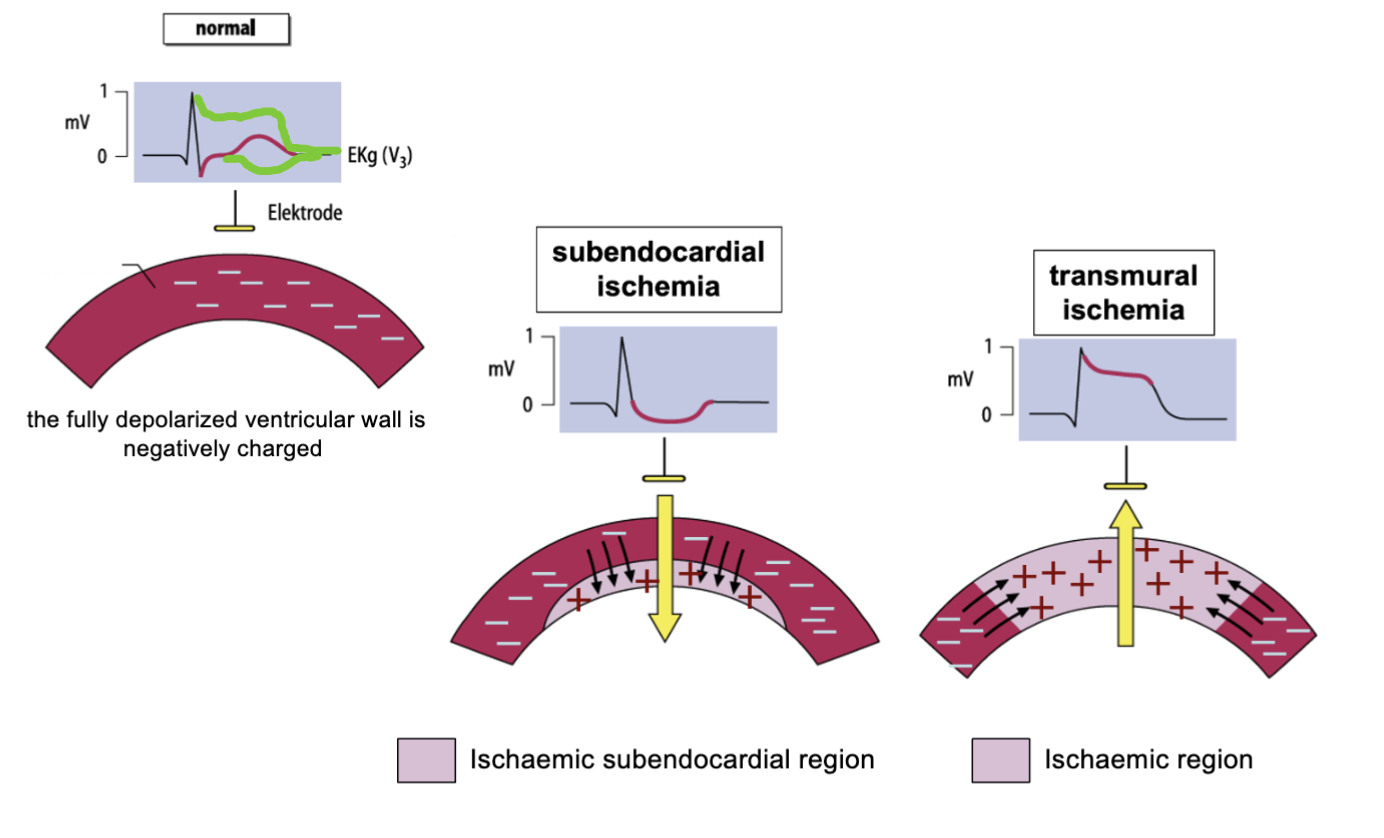
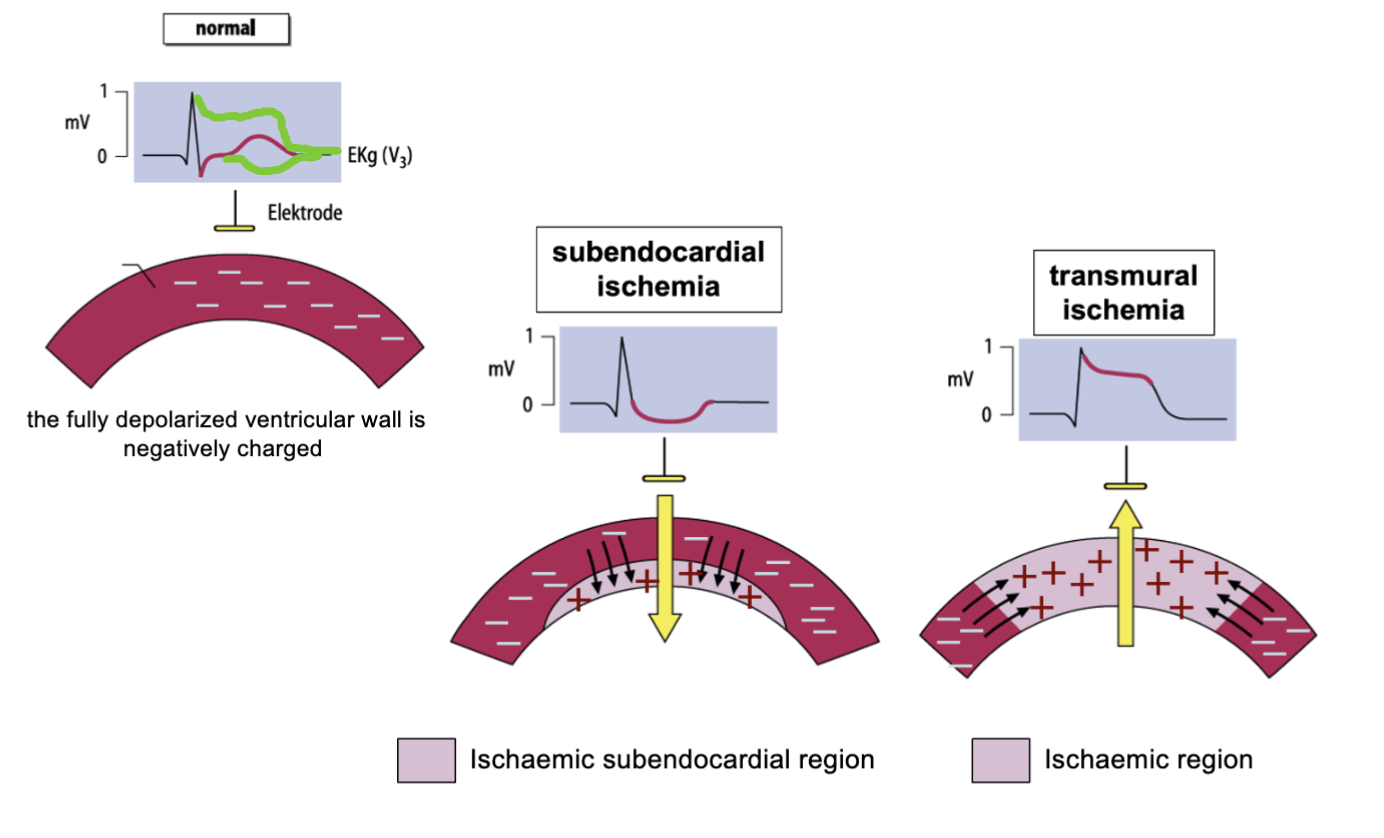
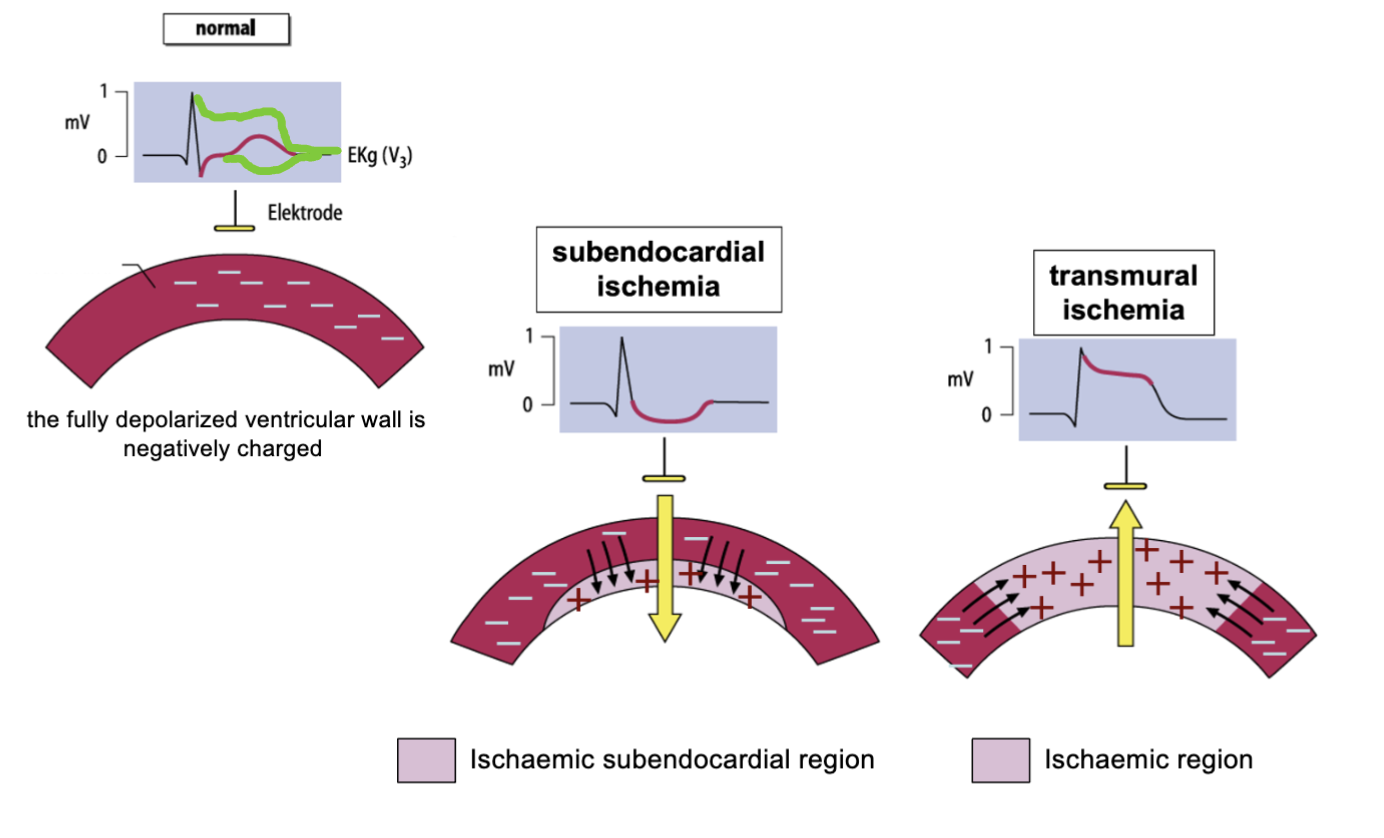
What is subendocardial ischemia?
Affects the innermost layer of the heart muscle (subendocardium) due to reduced blood flow in the coronary arteries.
62
New cards
How does subendocardial ischemia occur?
Due to a partial blockage of one or more of the coronary arteries that supply blood to the subendocardial layer of the heart muscle.
What are the symptoms of subendocardial ischemia?
What are the symptoms of subendocardial ischemia?
63
New cards
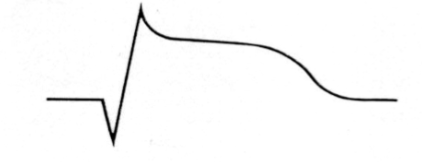
What is the ECG appearance of subendocardial ischemia?
ST segment depression &/or T wave inversion in the affected leads.
64
New cards
What is transmural ischemia?
Affects the entire thickness of the heart muscle due to reduced blood flow in the coronary arteries.
65
New cards
How does transmural ischemia occur?
Complete blockage of one or more of the coronary arteries that supply blood to the heart muscle.
66
New cards
What are the symptoms of transmural ischemia?
Severe chest pain or discomfort, shortness of breath, sweating, nausea, & vomiting.
67
New cards
What is the ECG appearance of transmural ischemia?
ST segment elevation in the affected leads.
68
New cards
How is subendocardial ischemia treated?
Medications such as nitroglycerin, beta-blockers, calcium channel blockers, & aspirin. In severe cases, procedures such as angioplasty or bypass surgery may be required.
69
New cards
How is transmural ischemia treated?
Medications such as nitroglycerin, beta-blockers, calcium channel blockers, & aspirin. Emergency procedures such as angioplasty or thrombolysis may be required to restore blood flow to the heart muscle. In severe cases, bypass surgery may be necessary.
70
New cards
What leads are affected in subendocardial ischemia?
Leads that correspond to the area of the heart supplied by the affected coronary artery, typically leads V5 & V6, & the inferior leads (II, III, & aVF).
71
New cards
What leads are affected in transmural ischemia?
Leads that correspond to the area of the heart supplied by the affected coronary artery, typically leads V1 to V6, & the inferior leads (II, III, & aVF).
72
New cards
What is the difference between ST segment elevation & depression on an ECG?
ST segment elevation on an ECG indicates myocardial injury or infarction, while ST segment depression indicates subendocardial ischemia or a non-ST segment elevation myocardial infarction (NSTEMI).
73
New cards
What is the significance of T wave inversion on an ECG?
Indicate subendocardial ischemia, myocardial infarction, or other cardiac conditions. It may also be a normal variant in some individuals.
74
New cards
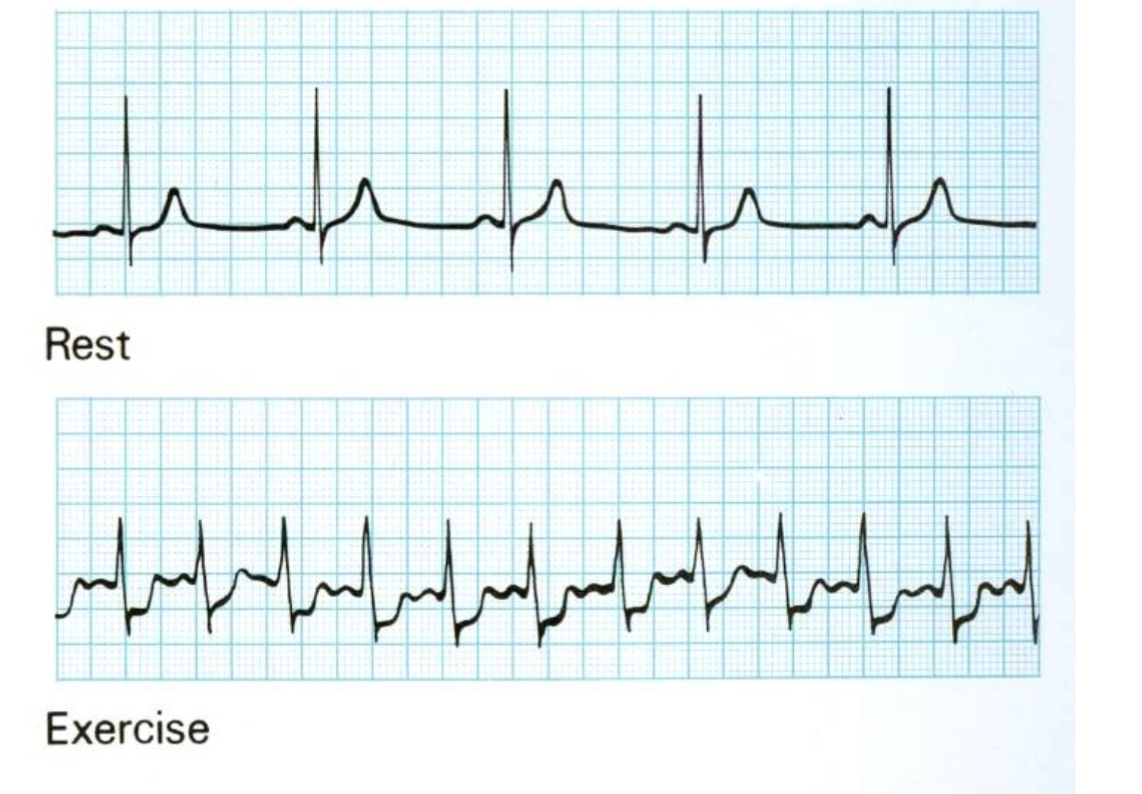
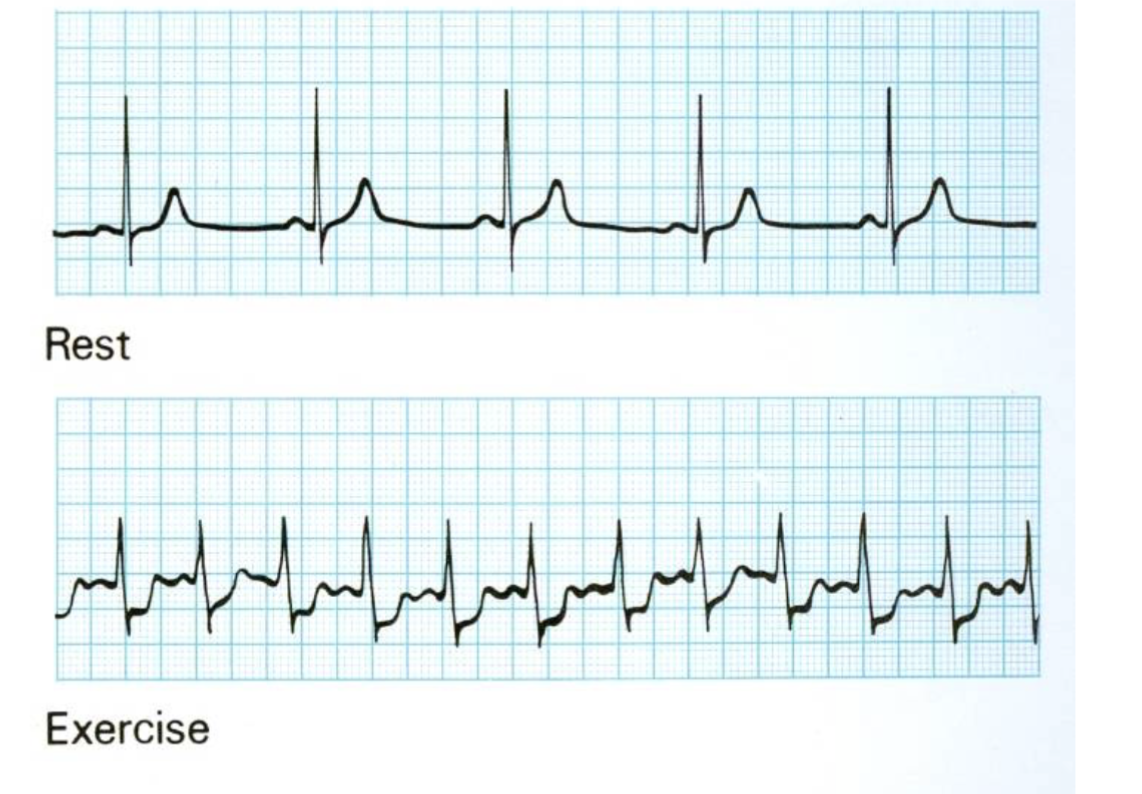
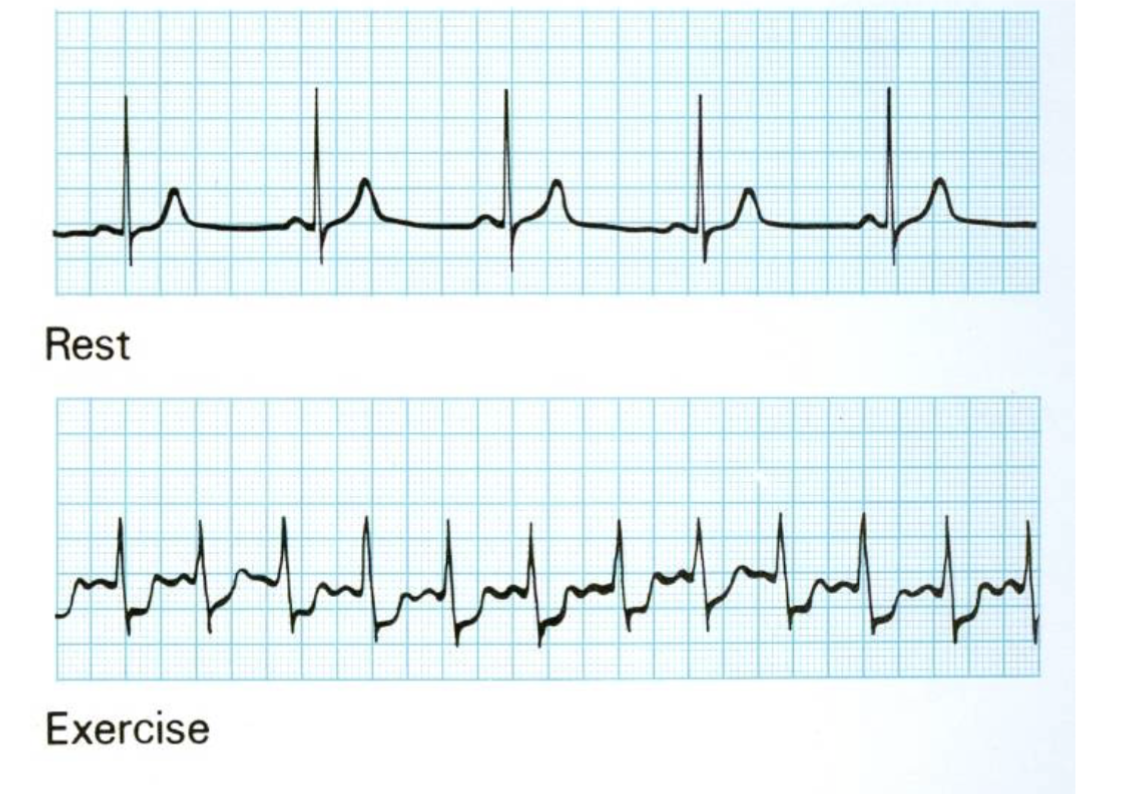
What is exercise-induced ischemic change?
Temporary reduction in blood flow to the heart muscle that occurs during exercise, typically due to narrowed or blocked coronary arteries.
75
New cards
What is the ECG appearance of exercise-induced ischemic change?
ST segment depression in the affected leads during exercise, which typically resolves shortly after exercise.
76
New cards
What leads are commonly affected in exercise-induced ischemic change?
Those that correspond to the area of the heart supplied by the affected coronary artery, typically the inferior leads (II, III, aVF) & the lateral leads (I, aVL, V5, V6).
77
New cards
What is the significance of exercise-induced ischemic change on an ECG?
Pesence of underlying coronary artery disease, & further diagnostic testing may be required to evaluate the severity of the disease.
78
New cards
How is exercise-induced ischemic change diagnosed?
Using a stress test, which involves exercising on a treadmill or stationary bike while connected to an ECG machine.
79
New cards
What is the treatment for exercise-induced ischemic change?
Lifestyle modifications, such as exercise, a heart-healthy diet, & smoking cessation.
\
In some cases, medications such as beta-blockers, calcium channel blockers, or nitrates may be prescribed to manage symptoms & reduce the risk of further complications.
\
In severe cases, angioplasty or bypass surgery may be necessar
\
In some cases, medications such as beta-blockers, calcium channel blockers, or nitrates may be prescribed to manage symptoms & reduce the risk of further complications.
\
In severe cases, angioplasty or bypass surgery may be necessar
80
New cards
What are the symptoms of exercise-induced ischemic change?
Asymptomatic or may cause symptoms such as chest pain, shortness of breath, or fatigue during exercise.
81
New cards
How is the severity of exercise-induced ischemic change graded?
Degree of ST segment depression observed on the ECG during exercise.
82
New cards
What diagnostic tests may be used to evaluate exercise-induced ischemic change?
Echocardiography, nuclear imaging, or coronary angiography.
83
New cards
What is silent ischemia?
Ischemia that occurs without accompanying symptoms.
84
New cards
What underlying risk factors for coronary artery disease may need to be addressed in the management of exercise-induced ischemic change?
Addressing underlying risk factors for coronary artery disease, such as hypertension, diabetes, or hyperlipidemia.
85
New cards
What is the ECG pattern seen before an infarction occurs?
Normal, with no significant abnormalities.
86
New cards
What is the ECG pattern seen in the very early stages of an infarction?
T wave elevation in the affected leads, which can appear within minutes of the onset of the infarction.
87
New cards
What is the typical ECG pattern seen about one hour after the onset of an infarction?
ST segment elevation in the affected leads, which can be visible for up to one week after the infarction.
88
New cards
What is the ECG pattern seen in the months following an infarction?
T wave inversion in the affected leads, which can be detectable for several months after the infarction.
89
New cards
What is the ECG pattern seen in persistent & usually irreversible changes following an infarction?
Pathological Q waves & loss of R waves.
90
New cards
What is the significance of changes in the ECG pattern over time following an infarction?
Timing, location, & severity of the infarction, & can be used to guide treatment & management decisions.
91
New cards
How does the timing of ECG changes following an infarction vary?
Depending on the location & extent of the infarct, as well as the individual patient's physiology.
92
New cards
What other ECG abnormalities may be seen following an infarction?
Arrhythmias, conduction delays, & ST segment depression in non-infarcted areas of the heart.
93
New cards
What is the pathophysiology underlying non-ST elevation myocardial infarction (NSTEMI)?
Mismatch between myocardial oxygen supply & dem&, leading to myocardial ischemia & subsequent myocardial injury.
This can be caused by an acute coronary syndrome, which can be due to a variety of underlying mechanisms such as non-thrombotic plaque rupture, partially occluding thrombus, or fully occluding thrombus.
This can be caused by an acute coronary syndrome, which can be due to a variety of underlying mechanisms such as non-thrombotic plaque rupture, partially occluding thrombus, or fully occluding thrombus.
94
New cards
What are the different types of NSTEMI based on the underlying cause of the ischemia?
Non-thrombotic plaque rupture, partially occluding thrombus, & fully occluding thrombus.
95
New cards
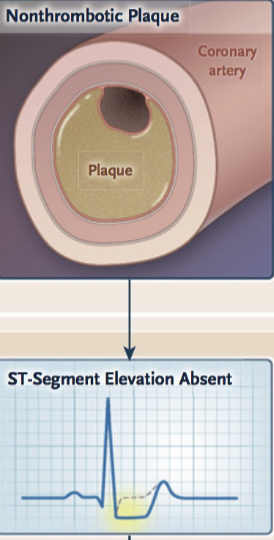
What is Non-thrombotic plaque rupture?
Caused by a ruptured atherosclerotic plaque, which leads to partial obstruction of the coronary artery & subsequent myocardial ischemia.
96
New cards
What is the ECG pattern in Non-thrombotic plaque rupture?
ST depression &/or T wave inversion in the affected leads.
ST segment elevaton is absent
ST segment elevaton is absent
97
New cards
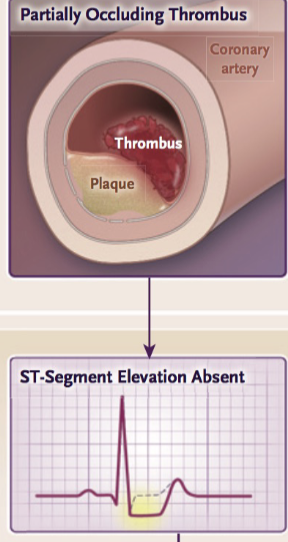
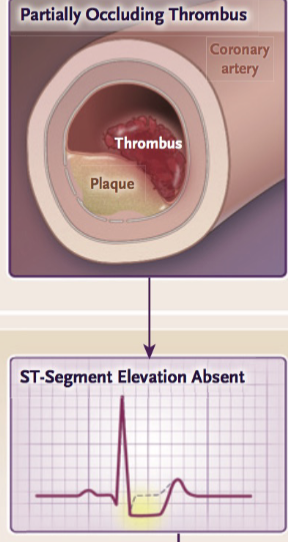
What is Partially occluding thrombus?
Partially obstructs the coronary artery, leading to myocardial ischemia.
98
New cards
What is the ECG pattern seen in Partially occluding thrombus?
ST segment elevaton is absent
99
New cards
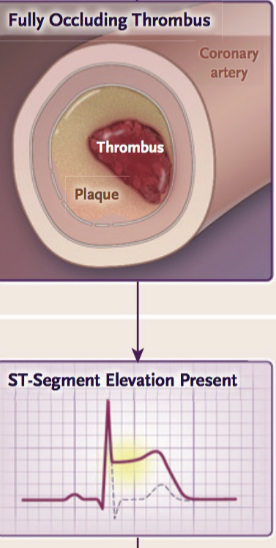
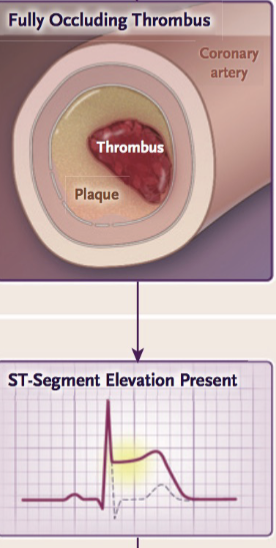
What is Fully occluding thrombus?
Completely obstructs the coronary artery, leading to myocardial infarction.
100
New cards
What is the ECG pattern seen in Fully occluding thrombus?
ST depression &/or T wave inversion in the affected leads, as well as possibly
ST elevation if the thrombus is associated with reperfusion.
ST segment elevation is present
ST elevation if the thrombus is associated with reperfusion.
ST segment elevation is present