NSE 221 FRACTURES
1/35
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
36 Terms
review from pain she did -
definition fo fracture
disruption or break in the The continuity of the structure of bone
majority of fractures come from traumatic injuries
some fractures secondary to disease process - cancer or osteoporosis
classification of fractures
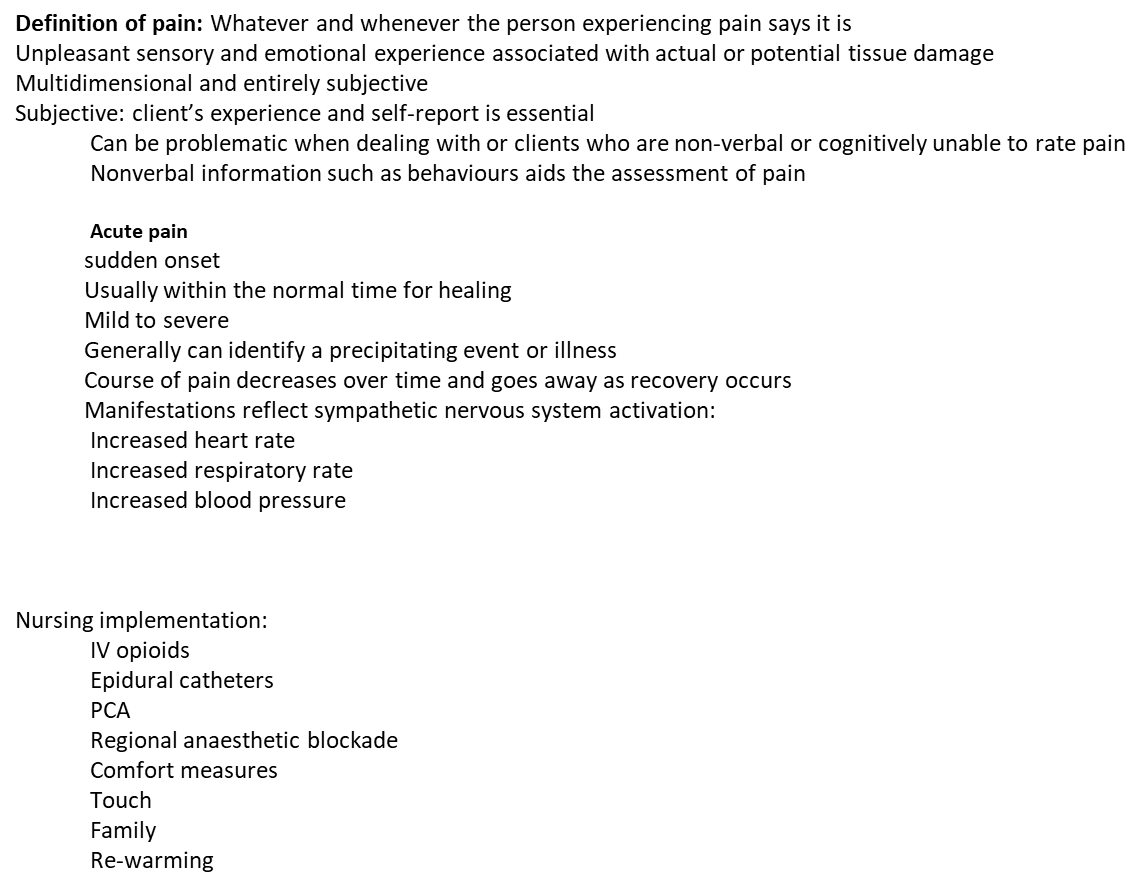
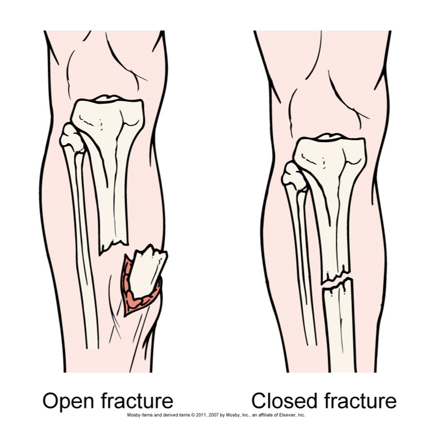
can be classified as open/closed
complete or incomplete
based on direction of fracure line
displaced or non displaced
fractures - open vs clsoed
open or closed
depends on communications or non cummonuication with external environment
open = skin broken adn bone and soft tissue exposed
closed = skin tact
fracture - incomplete vs complete
incomplete = fracture occurs partly across a bone shaft but the bone is still in one piece (non displaced)
complete fracture = break is completely through the bone (displaced)
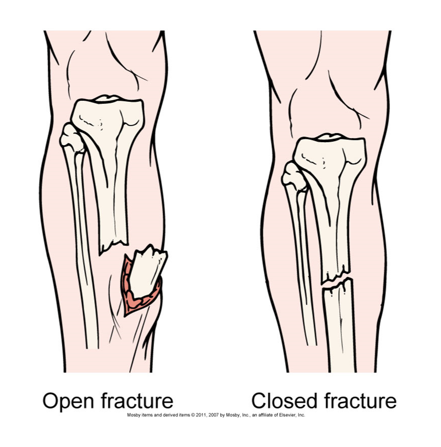
types of bone fractures image
what are the manifestations of a fracture
edema and swelling
it disrupts and penetrates of bone through skin or soft tissues or bleeding into surrounding tissues
significance - unchecked bleeding, swelling and edema in clsoed spaces cna occlude circulation and damage nerves (ex. risk of compartment syndrome)
pain and tenderness
muscle spasms as a result of involuntary reflex action of muscle, direct tissue trauma, increased pressure on nerves, movement of fracture parts
significance - pain adn tenderness encourage splinting of musculature around the fracture with reduction in motion of injured area
muscle spasm
irritation of tissue and protective response to injury and fracture
significance - muscle spasms may displace nondisplaced fracture or prevent it from reducing spontaneoulsy
what are the manifestations fo deformities
it is abnormal position of extremity or part as result of original forces of injury and action of muscles pulling fragment into abnormal position; seen as a loss of normal bony contours
sig - deformitity is cardinal sign of fracture; if uncorrected it may result in problems with bony union and restoration fo function of injured part
ecchymosis or contusion
discolouration of skin as a result of extravasation fo blood in subcut tissues
sig - ecchymosis may appear immediately after injury and amy appear distal to injury
reassure patient that the process is normal and that discolouration wil eventually resolve
loss of function
disruption of bone or joint, preventing functional use of limb/part
sig - fracture must be managed properly to ensure restoration fo function to limb/part
crepitation
grating or crunching together of bony fragments, producing palpable or audible crunching or popping sensation
significan - it increases chance for non union if bone ends are allowed to move excessively.
micromovement of bone end fragments (post fracture) assists in osteogenesis (new bone growth)
assessment for fractures
peripheral vascular assessment
colour
temp
cap refill (3secs)
PPP
edema
peripheral neuro assessment
sensation
motor function
pain
through both extemities are compared to obtain accurate assessment
what shes wrote in speaker notes:
Colour eg- pink, pale, cyanotic
Temperature hot, warm, cool, cold. Pallor or a cool (or cold) extremity below the injury could indicate arterial insufficiency. A warm, cyanotic extremity could indicate poor venous return.
Pulses strong, diminished, audible by Doppler, or absent
Peripheral pulses However, up to 12% of healthy adults do not have a palpable dorsalis pedis or posterior tibial pulse
Peripheral edema is also assessed, and pitting edema may be present with severe injury.
overall goals for fracture treatment
anatomical realignment of bone fragments
pain management
immobilization to maintain realignment
restoration of normal or near normal function of injured parts
collaborative care for fractures
Diagnostic • History and physical examination • Radiographs • CT scan, MRI Collaborative Therapy Fracture Reduction •Manipulation • Closed reduction •Skin traction •Skeletal traction •Open reduction with internal fixation (ORIF) | Fracture Immobilization • Casting or splinting •Traction •External fixation • Internal fixation Open Fractures • Surgical debridement and irrigation •Tetanus and diphtheria immunization • Prophylactic IV antibiotic therapy • Immobilization |
CT, computed tomography; MRI, magnetic resonance imaging. | |
fracture reduction - closed reduction
non surgical
usually under conscious sedation analgesia and sedation
manual realignment of bone to previous anatomical position
traction and countertraction manually applied to bone fragments to restore position, length, alignment
after reduction, injured part is immobilized by traction, casts, splints, external fixation, or braces to maintain alignment until healing occurs
internal fixation vs external fixation
internal fixation
pins, paltes, rods, screws and surgically inserted
stainless steel, titanium and vitallium are commonly used
proper alignment is validated by x ray
external
metallic device composed of metal pins - inserted into the bone and attached to external rods to stabalized the fracture as it heals
assessments for pin loosening and infection is critical
meticulous dressing changes are requires
notes on external
Infection control is critical.
Infection signaled by
Exudate
Erythema
Tenderness
Pain
Instruct patient and family on meticulous skin care.
extra notes on external fixation
External fixator metal with pins inserted in the bone and attached to external rods to stabilize the fracture while it heals
Infection = exudate, erythema, tenderness and pain. Pin care – follow hospital policy but usually half strength hydrogen peroxide with N/S
Sensation - Sensation and motor innervation in the upper extremity are assessed by evaluating the ulnar, median, and radial nerves. Neurovascular status can be assessed by abduction and adduction of the fingers, opposition of the fingers, and supination and pronation of the hand. In the lower extremity, dorsiflexion and plantar flexion provide information about motor function of the peroneal and tibial nerves. Sensory innervation is evaluated for the peroneal nerve on the dorsal part of the foot between the web space of the great and the second toes. Tibial nerve assessment is performed by stroking the plantar surface (sole) of the foot. Contralateral evaluation is critical. Paresthesia (abnormal sensation [e.g., numbness, tingling]) and hyperesthesia (hypersensation), may be reported by the patient. Partial or full loss of sensation (paresis or paralysis) may be a late sign of neurovascular damage. Reduced motion or strength in an injured extremity can alert the nurse to potential limb-threatening complications or disability.
what is traction
purpose
prevent or reduce pain and muscle spasm associated with low back pain or cervical sprain (ex., whiplash)
immobilize a joint or part of a body
reduce a fracture or dislocation
treat a pathological joint condition (ex. tumour, infection)
most ocmmon - skin traction and skeletal traction
traction is the application of a pulling force to an injured part of the body ro extremity while counter-traction pulls it in the opposite direction
notes:
Traction also indicated to
Reduce muscle spasm associated with low back pain or cervical whiplash
Expand a joint space
During arthroscopic procedures
Before major joint reconstruction
additioanly points on traction
forces are usually exerted on the distal fragment to obtain alignment with the proximal fragment
fracute alignment depends on the correct positioning and alignment of the client while the traction force remain constant
for the traction to be effective countertraction ro forces pulling in the opposite direction is needed to prevent client form sliding to the end or side of the bed
counter traction is commonly supplied by clients weight or may be augmented by elevated hob
nurses must maintain traction constantly and not interrupt the weight applied to the traction
2 types of traction - skin/skeletal
notes:
Fracture alignment depends on correct positioning and alignment while traction forces remain constant.
Forces must be pulling in opposite direction to prevent patient from sliding to end or side of bed.
Countertraction commonly supplied by patient’s body weight or augmented by elevating end of bed
Imperative that nurse maintains traction constantly and does not interrupt weight applied to traction
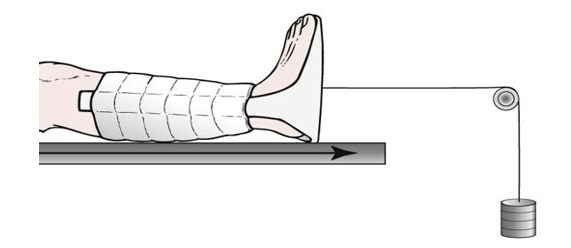
skin traction
short term treatment (48 hrs -72) until skeletal traction or surgery is avaialable
tape, boots, splints applied directly to the skin weights are 2.3 -4.5 kg
notes:
Skin traction is generally used for 48 to 72 hours.
•Pelvic or cervical skin traction may require heavier weights applied intermittently.
When traction is used to treat fractures, the forces are usually exerted on the distal fragment to obtain alignment with the proximal fragment. Several types of traction can be used for this purpose. Fracture alignment depends on the correct positioning and alignment of the patient while the traction forces remain constant. For extremity traction to be effective, forces must be pulling in the opposite direction (countertraction). Countertraction is commonly supplied by the patient's body weight or by weights pulling in the opposite direction and may be augmented by elevating the end of the bed. It is imperative to maintain traction continuously and keep the weights off the floor and moving freely through the pulleys. Someone needs to hold weights as patient moved up in bed.
Fracture alignment depends on the correct positioning and alignment of the patient while the traction forces remain constant.
skeletal traction
used to align injured bones and joints or treat joint contractures and congenital dysplasia
in place for longer periods of times compared to skin traction
provides long term pull that keeps ht einjured bones and joints aligned
physician insets pin or wire into the bone either partially or completely to align and immobilize the injured body part
disadvantage - risk for infection in the area of the bone where the skeletal pin has been inerted and the consequeces of prolonged immobility
notes;
Skeletal traction is in place for longer periods of time. Long-term pull keeps the injured bones and joints aligned. To apply skeletal traction, the physician inserts a pin or a wire into the bone either partially or completely. Weight ranges from 2 to 20kg.
Pin care – know hospital policy – usually wrapped in sterile N/S. Pin-site care varies but usually includes regular removal of exudates with half-strength hydrogen peroxide, rinsing pin sites with sterile saline, and drying of the area with sterile gauze.
Skeletal traction, generally in place for longer periods than skin traction, is used to align injured bones and joints or to treat joint contractures and congenital hip dysplasia. It provides a long-term pull that keeps the injured bones and joints aligned. To apply skeletal traction, the physician inserts a pin or wire into the bone, either partially or completely, to align and immobilize the injured body part. Weight for skeletal traction ranges from 2 to 20 kg. The use of too much weight can result in delayed union or nonunion. The major disadvantages of skeletal traction are risk for infection in the area of the bone where the skeletal pin has been inserted and the consequences of prolonged immobility.
When traction is used to treat fractures, the forces are usually exerted on the distal fragment to obtain alignment with the proximal fragment.
wound care for a skeletal traction
skeletal traction pin sites must be observed for sites of infection. includes regular removal of exudate with normal saline (chekc hospitla policy), cleaning pin sites with steril saline and drying the area with sterile gauze
ensure that the traction weight bag is hanging freely, the bag must not rest on the bed or the floor
if the rope ebcomes frayed replace them
the rope must be in the pulley tracks
ensure the bandages are free from wrinkles
tilt the bed to maintain counter traction
when slings are used iwth traction, exposed skin aea should be insepcted regularly
fracture immobilzation - casts
tmeporarily cicumferential immobilization deivce
allows patient to perform many normal activities of daily living
cst materials - natural, synthetic acrylic, fiberglassfree, latex free polymer, or hybrid of materials
common treatment for closed reduction
cast surrounds the joints above and below the fracture
care of a new cast
a thermochemical reaction occurs when the cast is first applied and begins to dry
client will feel increased warm around frature area, edema
cast is not strong enough for weight bearing until abt 24-72hrs
fresh palster cast - never covered by blanket
during drying proces - dont et , soil, subject any abnormal stress that can break the cast
handle the cast with palms as fingerprints can be areas of pressure
once throughly dry, edges may need to be petalled ot avoid skin irritation
cast care do and donts
do not get cast wet, remove any padding , insert any objects into casts or bear weight for 48 hrs (until dry)
do not insert any objects into casts ro remove any padding
apply ice directly over fracture for first 24 hrs
increase extremity above heart for the first 48 hrs
move joints above and below cast often
report increase pain, swelling with disoclouration of toe/fingers/pain during movement burning or tingling uner cast, sores or foul odours udner cast

fracture immobilization - sling
When a sling is used, the nurse must ensure that the axillary area is well padded to prevent skin excoriation and maceration associated with direct skin-to-skin contact. Placement of the sling should not put undue pressure on the posterior neck. Movement of the fingers (unless contraindicated) should be encouraged to enhance the pumping action of vascular and soft tissue structures to decrease edema. The nurse should also encourage the patient to actively move nonimmobilized joints of the upper extremity to prevent stiffness and contractures.
jones bandage
Jones bandages are bulky padding materials splints and an elastic wrap or bias cut stockinette
neurovascular assessment consist
upper and lwoer extremities
peripheral vascular assessment
colour
tmep
cap refill
ppp
edema
peripheral neuro assessment
sense
motor function
pain
notes:
Neurovascular Assessment Musculoskeletal injuries have the potential to cause changes in the neurovascular status of an injured extremity. With musculoskeletal trauma, application of a cast or constrictive dressing, poor positioning, and the physiological response to the traumatic injury can cause nerve or vascular damage, usually distal to the injury.
The neurovascular assessment should consist of a peripheral vascular assessment (colour, temperature, capillary refill, peripheral pulses, and edema)
Peripheral neurological assessment (sensation, motor function, and pain)
Throughout the neurovascular assessment, both extremities are compared to obtain an accurate assessment.
An extremity's colour (e.g., pink, pale, cyanotic) and temperature (i.e., hot, warm, cool, cold) in the area of the affected extremity are assessed. Pallor or a cool (or cold) extremity below the injury could indicate arterial insufficiency. A warm, cyanotic extremity could indicate poor venous return. A capillary refill (blanching of the nail bed) of 3 seconds indicates good arterial perfusion. Accurate documentation and ongoing neurovascular assessments are the cornerstones of nursing care for the individual with a musculoskeletal injury.
Pulses on both the unaffected and the injured extremity are compared to identify differences in rate or quality. Pulses are described as strong, diminished, audible by Doppler, or absent. A diminished or absent pulse distal to the injury can indicate vascular dysfunction and insufficiency.
In adults older than 45 years of age, occasionally either the dorsalis pedis or posterior tibial pulse may be difficult to locate
However, up to 12% of healthy adults do not have a palpable dorsalis pedis or posterior tibial pulse (Roberts & Hedges, 2010). Peripheral edema is also assessed, and pitting edema may be present with severe injury. Sensation and motor innervation in the upper extremity are assessed by evaluating the ulnar, median, and radial nerves. Neurovascular status can be assessed by abduction and adduction of the fingers, opposition of the fingers, and supination and pronation of the hand. In the lower extremity, dorsiflexion and plantar flexion provide information about motor function of the peroneal and tibial nerves. Sensory innervation is evaluated for the peroneal nerve on the dorsal part of the foot between the web space of the great and the second toes. Tibial nerve assessment is performed by stroking the plantar surface (sole) of the foot. Contralateral evaluation is critical. Paresthesia (abnormal sensation [e.g., numbness, tingling]) and hyperesthesia (hypersensation), may be reported by the patient. Partial or full loss of sensation (paresis or paralysis) may be a late sign of neurovascular damage. Reduced motion or strength in an injured extremity can alert the nurse to potential limb-threatening complications or disability.
nursing diagnoses - hypotheses
impaired physical mobility
risk for peripheral neurovascular dysfunction
acute pain
ineffective self health mangement
complications fo immobility
DVT
INFECTION
COMPARTMENT SYNDROME
PULMONARY EMBOLISM
complications of fractures
infection
high incidence for infections with open fractures and soft tissue injuries
tetanus
osteomyelitis
notes
Infection
High incidence in open fractures and soft tissue injuries
Massive or blunt soft tissue injury often has more serious consequences than fracture.
Devitalized and contaminated tissue is an ideal medium for pathogens.
dvt
veins of lwoer extremities and the pelvis are highly susceptible to thrombus formation after fracture
manifestation - unilateral leg edema, pain, tenderness on palpitation, warm skin, erythema, dialted superficial veins
FAT embolism
presence of systemic fat globules from fractures that are distributed into tissues and organs after traumatic skeletal injury
manifestations - chest pain, tachpnea, cyanosis, dyspnea, apprehension, tachycardia, decreased paco2
what is compartment syndrome - complication fo fractures
swelling adn increased pressure within a limited space (compartment) press on and compromise in the functin of blood vessels, nerves adn tnedons that run through that compartment
clasified as acut, subacute, chronic
causes
derceased compartment size resulting form restrictive dressing,s splints, casts, excessive traction ro premature closure of fascia
incresed compartment contents related to bleeding, edema chemical response to snake bite or IV filtration
early recogniition adn immediate interveniton si required

what are the 6 PS!
paresthesia - numbness and tinglging
pressure - increase in compartment
paralysis - loss of function
pain - distal to injury that is not releived by opiod analgesics and pain on passive stretch of muscle travelling thorugh compartment
pallor - coolness and loss of normal colour extremity
pulseslessness - diminished/absent peripherla pulses
notes:
Urine output - Because of the possibility of muscle damage, urine output should be assessed. Myoglobin released from damaged muscle cells precipitates as a gel-like substance and causes obstruction in renal tubules. This condition results in acute tubular necrosis and acute kidney injury. Common signs are dark, reddish-brown urine and clinical manifestations associated with acute kidney injury
Fasciotomy to ensure adequate soft tissue decompression. Infection resulting from delayed wound closure is a potential problem following a fasciotomy. In severe cases of compartment syndrome, an amputation may be required.
compartment syndrome collaborative care
prompt accurate diagnosis
extremity should not be eelvated above heart level
application cold compress may ersult in constictiona dn may exacerbate compartment synromeorome
eelvation may raise venous pressure and slow arterial perfusion
notes:
-Pain unrelieved by drugs and out of proportion to the level of injury is one of the first indications of impending compartment syndrome.
May be necessary to remove or loosen bandage or bivalve cast
Reduction in traction weight may
↓ external circumferential pressures.
Surgical decompression may be necessary.
signs and smyptoms fo pulmonary embolism
triad - dyspnea, chest pain , hemoptysis (20%)
slow ro suddenly
mild to moderate hypoxemia with a low paco2 - common findings
cough, pleuritic chest pain, hemoptysis , crackles, fevere
sudden change in mental status as a result of hypoxemia
massive emboli may produce abrupt hypotension, pallor, severe dyspnea, hypoxemia. chest pain may or not be present. ecg may indicate tachycardia and right ventricular strain
medium size emboli often cause pleuritic chest pain , dyspnea , sliht fever, productive cough with blooak streak sputum . a physical exam may reveal tachycardia adn pleural friction rub
nursing care PE
bed rest, semi fowlers
iv line - medications adn fluid therapy
o2 therapy as ordered, careful monitoring of vital signs, cardiac dysrhytmia monitoring, pulse ox abgs, lung sounds
monitor labs aptt and inr
nursing care = assessing for the complications of anticoagulant therapy (bleeding, hematomas, brusing) and PE (hypoxia, hypotension)
coughing and deep breathing should be encourage
patient suualy anxious because of pain, sense of doom , inability to breathe and fear of death. explain emotion support and reassurance to help releive the aptients anxiety
notes:
The prognosis of a patient with PE is good if therapy is promptly instituted.
The patient should be repositioned as little as possible before fracture immobilization or stabilization because of the danger of dislodging more fat droplets into the general circulation.
pulmonary embolism - dagnostic and collaborative therapy
• History and physical examination • Chest radiographic study • Continuous ECG monitoring • ABGs • Venous ultrasound • CBC count with WBC differential • Spiral (helical) CT scan • Ventilation-perfusion () • Lung scan • D-dimer level • Troponin level, BNP level • Pulmonary angiography | • Supplemental oxygen, intubation may be necessary • Fibrinolytic agent • Unfractionated heparin IV • Low-molecular-weight heparin (e.g., enoxaparin [Lovenox]) • Warfarin (Coumadin) for long-term therapy • Monitoring of aPTT and INR levels • Limited activity • Opioids for pain relief • Inferior vena cava filter • Pulmonary embolectomy in life-threatening situation |
ABGs, Arterial blood gases; aPTT, activated partial thromboplastin time; BNP, B-type natriuretic peptide; CBC, complete blood count; CT, computed tomography; ECG, electrocardiogram; INR, international normalized ratio; IV, intravenous; WBC, white blood cell. | |
discharge
•The patient is discharged after regaining ambulation skills, learning care of the cast or orthotic device, and learning how to cope with the safety and security imposed by injury and treatment.
•
•Regular follow-up care should be arranged for after discharge, including home health nursing.
•
•For the patient to be discharged home, the nurse should have the patient demonstrate the proper use of crutches or a walker, the ability to transfer into and from a chair and bed, and the ability to ascend and descend stairs.
nutrition is important
Discharge teaching should focus on Nutrition to promote bone healing
Proper nutrition is an essential component of the reparative process in injured tissue. An adequate energy source is needed to promote muscle strength and tone, build endurance, and enhance ambulation and gait-training skills. The patient's dietary requirements must include ample protein (e.g., 1 g/kg of body weight), vitamins (especially B, C, and D), and calcium, phosphorus, and magnesium to ensure optimal soft tissue and bone healing. Low serum protein levels and vitamin C deficiencies interfere with tissue healing. Immobility and callus formation increase calcium needs. Three well-balanced meals a day will usually provide the necessary nutrients. The well-balanced meal should be supplemented by a fluid intake of 2000 to 3000 mL/day to promote optimal bladder and bowel function. Adequate fluid and a high-fibre diet with fruits and vegetables will prevent constipation. If immobilized in bed with skeletal traction or in a body jacket or hip spica bandage, the patient should be instructed to eat six small meals so as not to overeat and thus avoid abdominal pressure and cramping.