Calcium and Phosphate Homeostasis
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
45 Terms
-Freely soluble in blood plasma
-Bind to cell surface receptors
-Activate 2nd messenger systems within the cell
-Rapid action
-Short half-life
-Most are metabolised by the liver and then excreted by the kidney
Describe water soluble hormones
-Mostly bind to cytosolic/nuclear receptors
-Protein-bound in blood plasma
-Protein-bound component is not physiologically active but acts as a store of the free hormone
-Less immediate action
-Longer half-life
-Are affected by disturbances in plasma protein concentration
Describe lipid soluble hormones
Water-soluble.
Without extraneous factors, which hormone is likely to act faster, a lipid-soluble hormone or a water-soluble hormone?
Lipid-soluble.
Which type of hormone must be bound to a protein for transport in the blood?
Insulin because it is water-soluble.
Insulin is a water-soluble hormone, where as oestrogen is a lipid-soluble hormone, which is more likely to have a shorter half life? Why?
Testing for lipid-soluble hormone levels in the blood requires further discrepancy as you can either test for the free-substance or for the protein-bound substance.
Why is it clinically relevant to know whether a hormone is lipid or water-soluble?
Hormone reservoir:
-The hormone can be bound to a protein in the circulation which serves as a reservoir
Hormone buffer:
-Proteins still have a remaining binding hormone capacity, therefore can prevent large spikes in active hormone concentration, absorption of short-term peaks in hormone synthesis, more stable long-term concentrations
Reduce loss of hormone:
-Proteins and therefore protein-bound hormones are not filtered out whilst free hormones are lost in the urine
Describe the advantages of using carrier-proteins for lipid-soluble hormone transport
Affected by disruptions in blood levels of carrier protein (e.g. albumin):
-A decrease in carrier protein will decrease hormone-protein binding and increase the free hormone concentration
Competition from other substances (e.g. drugs for carrier proteins)
-Particularly with less specific carrier proteins (e.g. albumin)
Describe the disadvantages of using carrier-proteins for lipid-soluble hormone transport
-Oestrogen is a lipid-soluble hormone
-This means it requires a transport protein (albumin) for its transport
-The lack of albumin means that there is not enough transport protein for the oestrogen and hence more oestrogen remains in its free hormone form
Why would a bitch deficient in albumin have unusually high free oestrogen levels?
Regulated by two hypothalamic neuro-hormones:
-GHRH
-GHIH (somatastatin)
-These hormones have direct effect but also stimulates production of the hormone IGF-1 from the liver
How is growth hormone secretion regulated?
-Mediates growth
-Stimulates the effects of growth hormone
What is the function of IGF-1?
-Growth hormone (GH) has a longer AA chain
-IGF-1 is highly protein-bound where as GH is only 50%
-Both have a tyrosine kinase receptor
-GH synthesising cells are most abundant in the anterior pituitary where as IGF-1 synthesising cells are in the liver
-IGF-1 is similar in structure to proinsulin where as GH is similar in structure to prolactin
-GH exerts little negative feedback on GH-RH where as IGF-1 exerts potent negative feedback on GH secreting cells by stimulating GHIH in the hypothalamus
Compare growth hormone with IGF-1
-Inputs from the CNS
-Strenuous physical activity
-Starvation
-Stress
-Decreased plasma glucose and free fatty acids
-Increased plasma amino acid concentration
-Ghrelin from parietal cells and hypothalamus
-Thyroid hormone, androgens and oestrogens
What factors increase growth hormone secretion?
-Stimulates growth of body mass and elongation of the bones
-Essential for growth until skeletal development is complete
-Bone and cartilage growth
-Soft tissue growth
-Lactation
-Anabolism (protein synthesis, lipolysis)
-Inhibits tissue uptake and utilisation of glucose (opposes insulin effects)
What are the functions of growth hormone?
i) Gigantism
ii) Acromegaly
What occurs in animals with excessive growth hormone production
i) Before growth plate closure
ii) After growth plate closure
-Stimulates protein synthesis = Decreased amino acid level
-Lipolysis = Increased fatty acid levels
-Inhibits tissue uptake and utilisation of glucose = Increased glucose concentration
Summarise the metabolic functions of growth hormone and predict the effects on blood plasma concentrations of the effected substance
-Growth hormone
-Thyroid hormones
-Insulin
-Sex hormones at puberty
-Adequate diet, absence of chronic stressors and disease
What does normal growth require?
Bone:
-99%
-As hydroxyapatite
Intracellular fluid:
-Free Ca2+ and protein-bound
->1%
Extracellular fluid:
-Free Ca2+ and protein-bound
->1%
Where is calcium stored? Describe their proportions and type
-Extracellular
-Intracellular Ca levels are kept low so when it comes from the ECF, the signal is very powerful
Where do you get the greatest concentration of free calcium, intracellular or extracellular? Why is this important in terms of cell signalling?
-Very tightly
-Only varies within 2% of its limits
How tightly is calcium levels controlled?
-Intestinal absorption
-Renal excretion
-Release and uptake from bone
What are the 3 systems of calcium homeostasis?
-Obtains Vitamin D2 by eating plants
-Obtains Vitamin D3 by exposure to sunlight and integument manufacture
How does an animal obtain vitamin D?
-Active form = Calcitriol (1, 25 dihydroxycholecalciferol)
Activation:
-2 hydroxylation reactions
-First occurs in the liver (can be stored in adipose tissue here)
-Second occurs in the kidney
What is the active form of Vitamin D? How does it become activated?
-Lipid soluble
-So transported bound to vitamin-D-binding-globulin
-Binds to intracellular receptors
Describe calcitriol
-Metabolism of vitamin D is regulated
-Therefore the production of calcitriol is regulated
How is the effect of calcitriol on plasma calcium concentration controlled?
-Increases calcium uptake from the small intestine
-Increases renal absorption of calcium
-Increases mobilisation of calcium from bone
Overall effect = increase plasma calcium concentration
What is the effect of calcitriol on plasma calcium concentration?
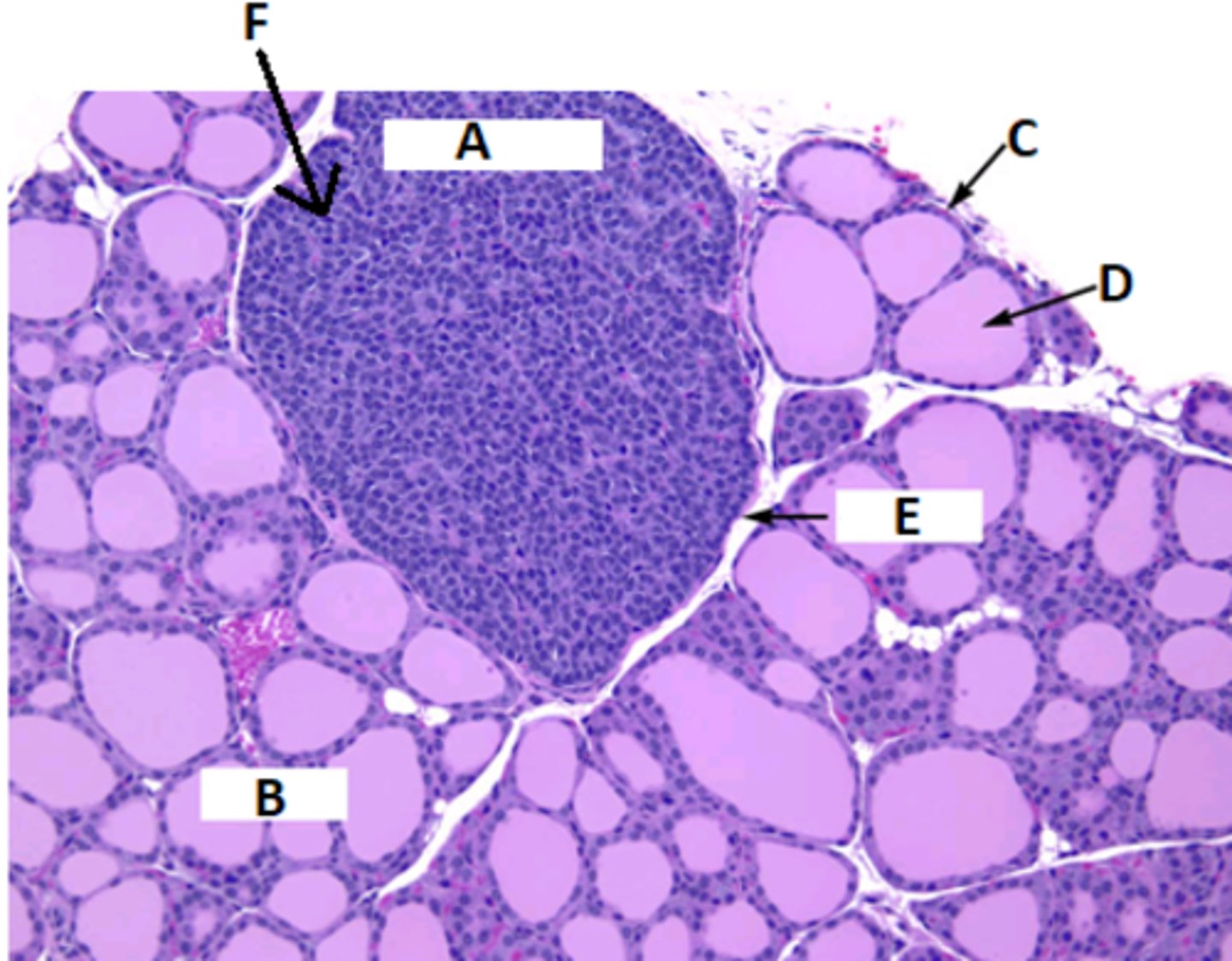
A = Parathyroid gland
B = Thyroid gland
C = Follicular epithelium
D = Colloid
E = Capsule
F = Chief cells
Label this histological slide of the thyroid and parathyroid gland
In cranial and caudal pairs at the poles of the 2 lobes of the thyroid gland.
Where are the parathyroid glands found in the body?
In the parathyroid gland by the chief cells.
Where is parathyroid hormone (PTH) produced?
-Cells in the gland directly detect very small decreases in free calcium and release PTH in response to this
Effects of PTH:
-Increases Ca2+ uptake from the GI tract
-Increases mobilisation of calcium from bone
-Decreases urinary excretion of calcium
Overall effect = increase plasma calcium concentration
How does the parathyroid gland control the levels of plasma calcium concentration? What is the effect of PTH on plasma calcium concentration?
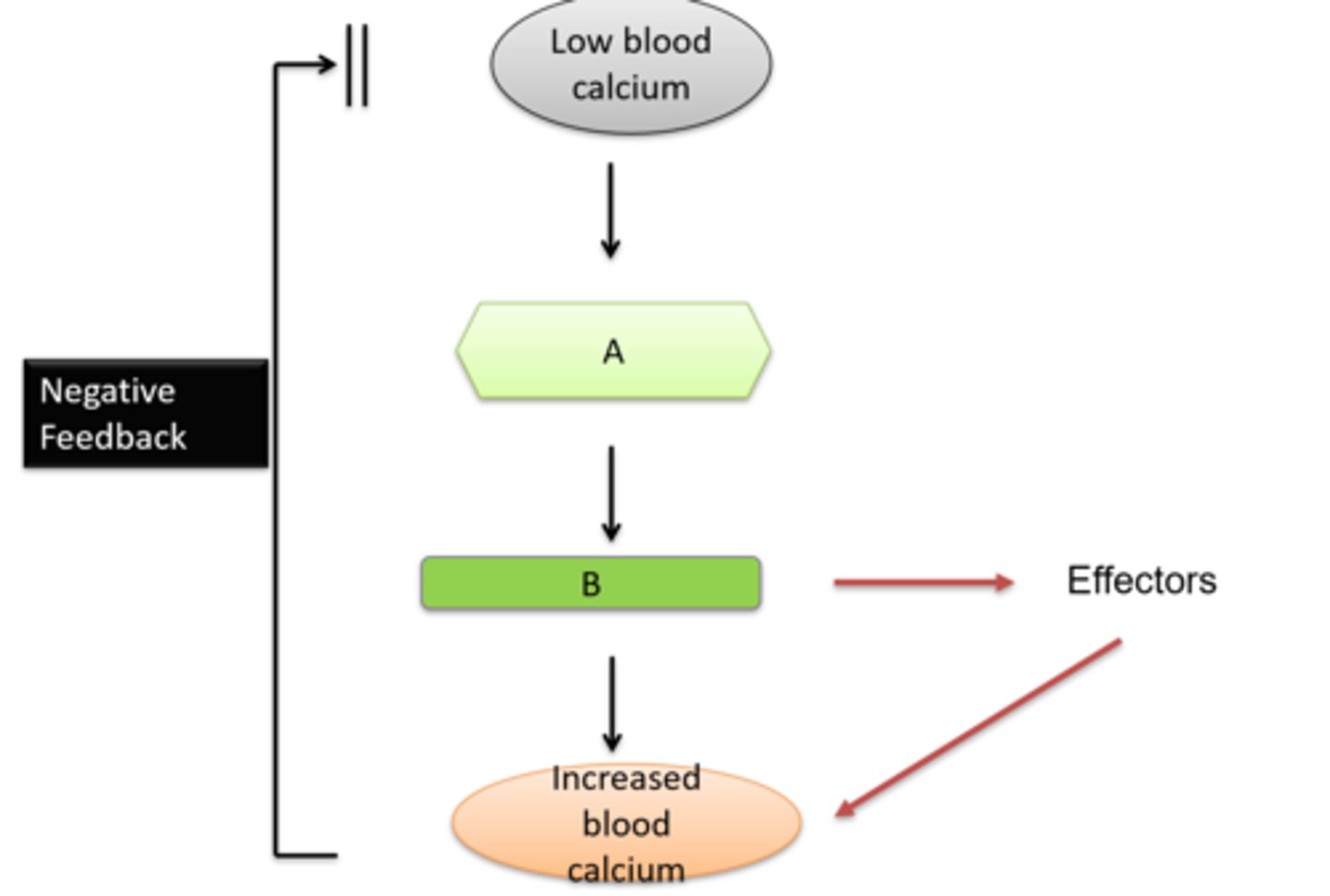
A = Parathyroid gland
B = Parathyroid hormone
Fill in the blanks of this flow diagram depicting how the parathyroid gland responds to low blood calcium
By most tissues in the body.
Where is PTH related Protein (PTHrP) produced?
-Same as PTH
-Has more diverse actions (e.g. cell proliferation)
What is the function of PTHrP?
-It is produced by certain types of cancers and cancer-producing cells
-This means that it will not be under negative feedback so overproduction occurs which can lead to hypercalcaemia
Why is PTHrP clinically important?
-C-cells (parafollicular cells) of the thyroid gland
-Secreted in response to an increase in free calcium ions
Where is calcitonin made? When is it made?
-Targets osteoclasts
-Makes bone remodelling less active
-Flux of Ca2+ and PO4 from bone to plasma decreases
-Increases urinary loss of Ca2+
-Decreases gut absorption of Ca2+
Overall effect is to decrease the concentration of plasma calcium concentration
What is the function of calcitonin (CT)?
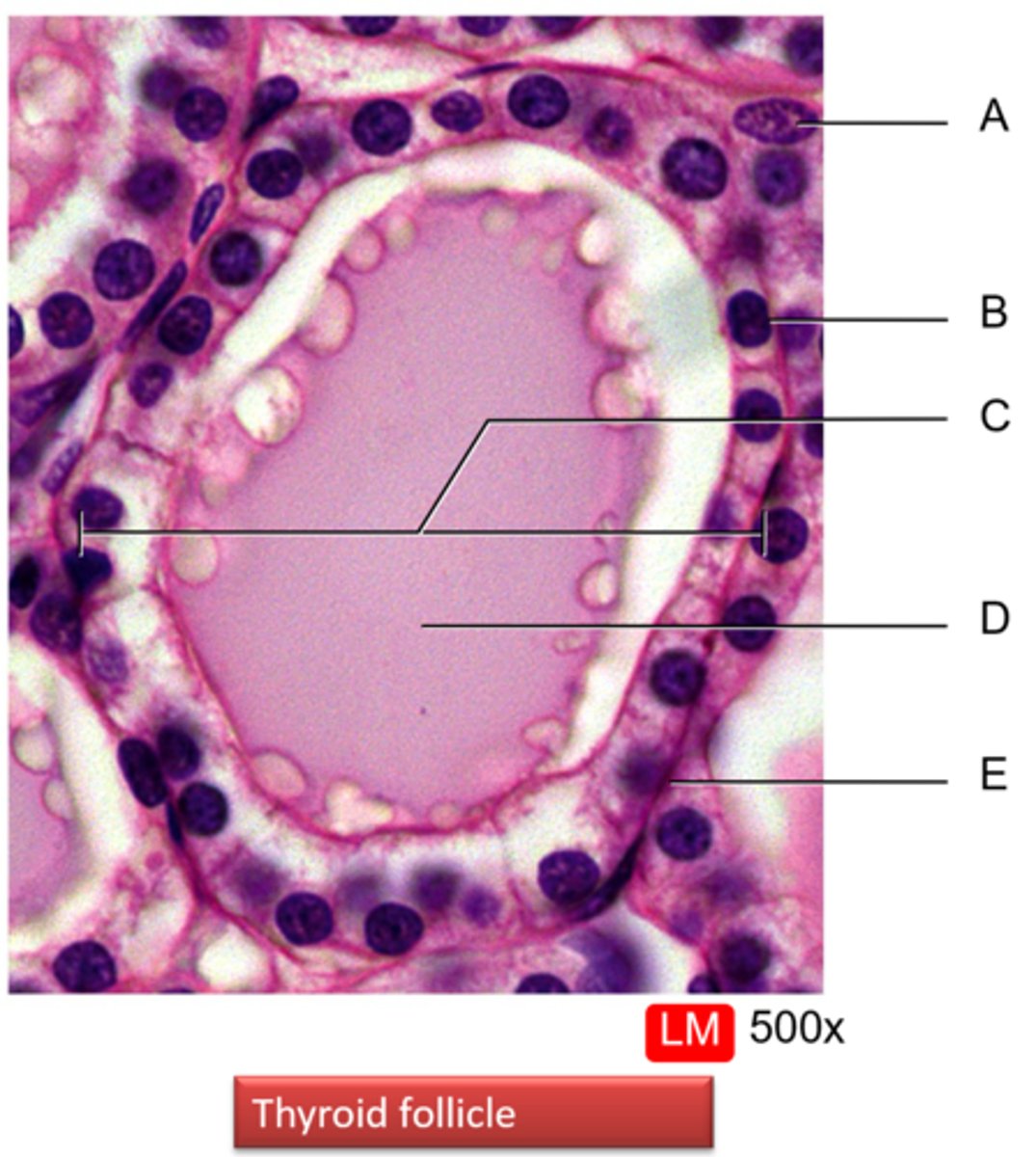
A = Parafollicular (C) cell
B = Follicular cell
C = Thyroid follicle
D = Thyroglobulin (TGB; Colloid)
E = Basement membrane
Label this histological slide of a thyroid follicle
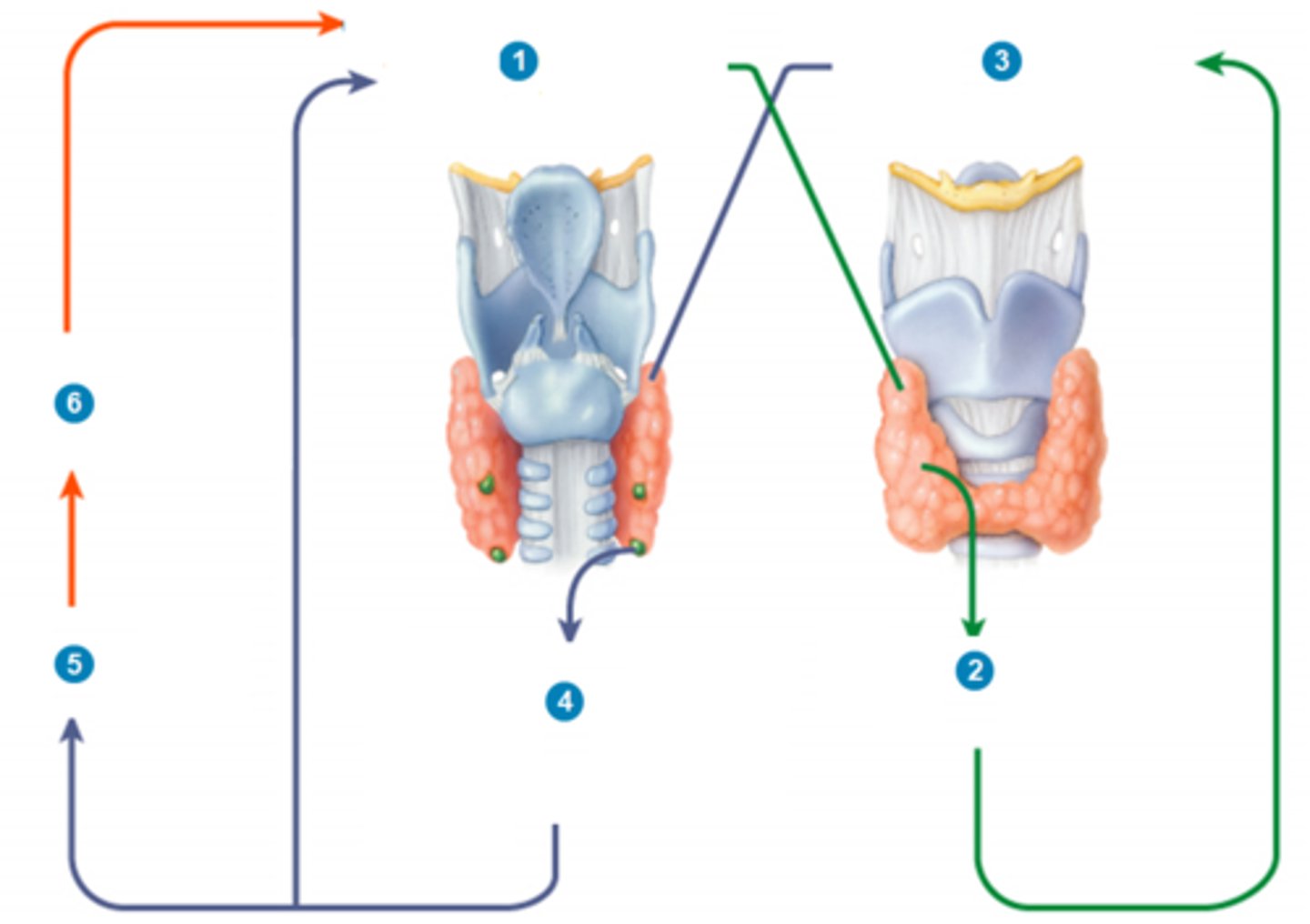
1) High levels of Ca2+ in the blood stimulate the thyroid gland parafollicular cells to release more CT
2) Calcitonin inhibits osteoclasts, thus decreasing blood Ca2+ levels
3) Low level of Ca2+ in blood stimulates parathyroid gland chief cells to release more PTH
4) Parathyroid hormone (PTH) promotes release of Ca2+ from bone extracellular matrix into blood and slows loss of Ca2+ in urine, thus increasing Ca2+ level
5) PTH also stimulates the kidneys to release calcitriol
6) Calcitriol stimulates increased absorption of Ca2+ from foods, which increases blood Ca2+ level
The cycle then repeats when Ca2+ raise again
Explain how calcium levels are controlled by a negative feedback loop mediated by the thyroid and parathyroid glands, starting from high levels of Ca2+ in the blood
Bone:
-85%
-Stored as hydroxyapatite
Cells:
-15%
-Both in ECF and ICF as inorganic phosphates and organic phosphates
Where is phosphate stored? Describe its proportions and its type
In the process of Ca2+ metabolism, phosphate is normally kept within normal limits
-E.g. absorbed in the intestines, filtered, reabsorbed, secreted in urine
How is phosphate homeostasis linked to the concentration of free plasma Ca2+?
-Decreases serum P but increases serum Ca
-Increases urinary excretion of P but decreases urinary excretion of Ca
-Increases calcitriol secretion for both system effects (but remember the stimulus is decreased Ca2+ concentration)
Compare what PTH does to calcium and phosphate
-Regulation of calcium largely depends on differential absorption of calcium from the SI
-Regulation of phosphate largely depends on urinary excretion
How is the regulation of phosphate different to the regulation of calcium?
Regulation of phosphate largely depends on urinary excretion so without this, phosphate levels are poorly controlled.
Why is chronic kidney disease particularly detrimental for phosphate concentration regulation?
-Stimulates PTH production
-Inhibits activation of vitamin D
What are the effects of hyperphosphatemia with regards to the regulatory system?
Late pregnancy and parturition:
-Mammary cells extract a large amount of Ca2+ from the ECF
-Mineralisation of the foetal skeleton occurs in late pregnancy which uses a lot of Ca2+
Laying hens:
-2 weeks before lay, hormones stimulate extra bone to be deposited in bone marrow cavities
-Increasing oestrogen induces increased calcium-binding plasma proteins
-Eggshell contains lots of Ca2+
What are some normal physiological challenges to calcium homeostasis? Describe why they are challenging