Fungal and Parasitic Infections/Antifungals
1/75
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
76 Terms
are fungi prokaryotes or eukaryotes?
eukaryotes (therefore, many aspects of the cellular physiology of fungal and human cells are very similar)
what are the few antifungals that are available?
Fluconasole
Target: biosynthesis of ergosterol (cell membrane lipid)
Caspofungin
Target: cell wall
Amphotericin B
Target: cell membrane
Very toxic
Fungal Infections: Encounter
Typically, from the environment
Exception: Candida albicans is a human commensal
Fungal Infections: Entry
• Inhalation
• Traumatic implantation
• Disruption of natural barriers (skin, mucosal surfaces)
Fungal Infections: spread/multiplication
• Fungal infections are usually mild and self-limiting
• Host response typically eliminates fungi
what is an important mechanism of the host response when eliminating fungi?
Phagocytosis by neutrophils
Fungal Infections: damage
Indirect damage due to the inflammatory response
Occlusion of organs
If invasive, can cause destruction of host tissues
what are some examples of occlusion of organs caused by fungal infections?
Fungus balls occlude bronchi in lung or tubules or ureters in kidney.
Fungus mats growing on heart valves may break off and travel through blood causing arterial occlusion (Aspergillus)
The following statements about fungal infections are correct EXCEPT one. Which is the EXCEPTION?
A. Fungal infections are always acquired from the environment.
B. Fungal infections are usually mild and self-limiting.
C. Fungal pathogens are eukaryotes, which limits the targets for
antifungal drugs.
D. Immunosuppression can predispose to severe disease.
A. Fungal infections are always acquired from the environment.
Mortality due to fungal infection is high in what groups?
the immunocompromised
primary vs opportunistic fungal pathogens?
Primary → Can cause disease in immunocompetent host
Opportunistic → Typically, cause disease in the immunocompromised hosts
Coccidioides immitis is endemic to what region? and encounter?
Southwestern US, Mexico, parts of South America
encountered via soil/dust storms
Coccidioides immitis: entry
inhalation
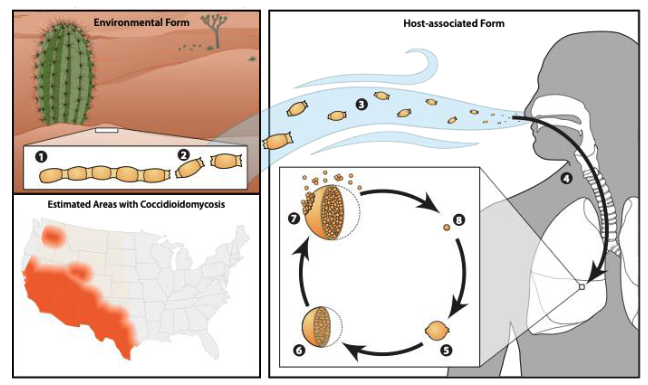
Coccidioides immitis: disease
Coccidioidomycosis (aka Valley Fever)
Not contagious
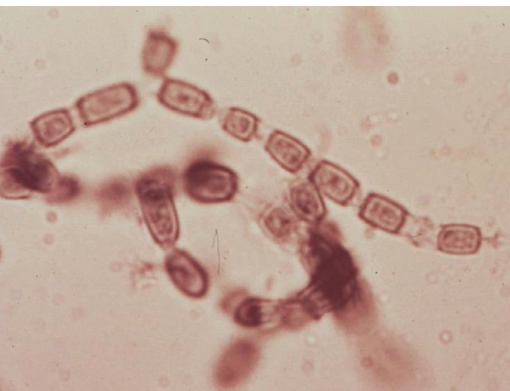
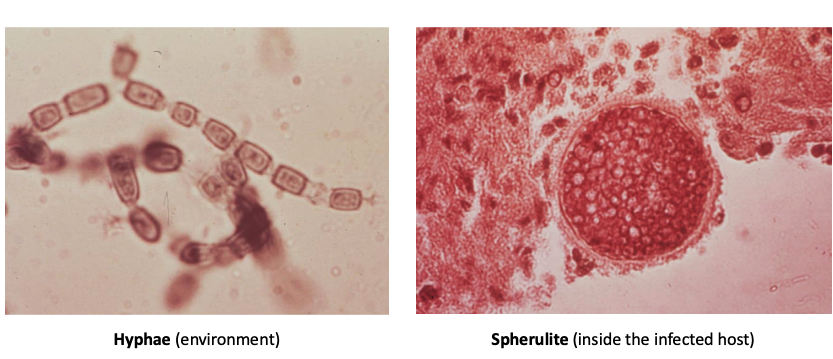
Coccidioides immitis
what does it mean that Coccidioides immitis is a dimorphic fungus?
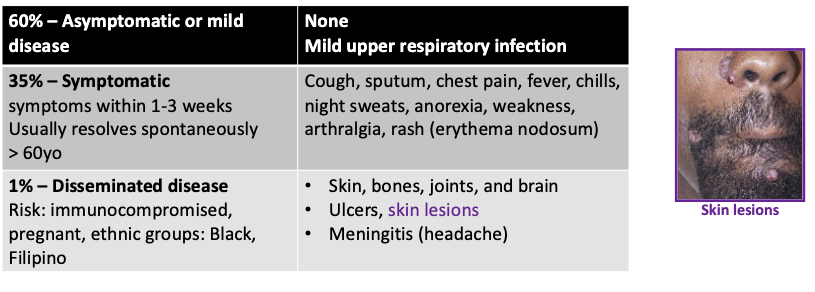
Symptoms of Coccidioidomycosis
60% – Asymptomatic or mild disease
None
Mild upper respiratory infection
35% – Symptomatic (symptoms within 1-3 weeks
resolves spontaneously
Cough, sputum, chest pain, fever, chills, night sweats, anorexia, weakness, arthralgia, rash (erythema nodosum)
1% – Disseminated disease
Risk: immunocompromised, pregnant, Black, Filipino
Skin, bones, joints, and brain
Ulcers, skin lesions
Meningitis (headache
Coccidioides immitis: treatment
oral itraconazole
For severe or disseminated infection, immunocompromised host: Amphotericin B until improved then oral itraconazole
Korean female, 74 years old
Visits daughter in Phoenix, Arizona for several months. Upon return home to Korea, develops a dry cough, night sweats.
Treated symptomatically. Symptoms resolve.
Several years later, routine chest radiograph shows pulmonary nodule.
Nodule is thought to be a malignancy and is removed. Fungal stain shows Coccidioides immitis.
Patient recovered from surgery and required no further treatment.
Diagnosis?
Pulmonary coccidioidomycosis without spread.
72 years old, resident of Ohio, spends winters in Arizona.
Presents to clinic in Ohio with hypothermia, dehydration, “generalized, pruritic maculopapular rash”.
A clear chest radiograph. Later, developed fever, cough, had left lower lobe infiltrate.
Given broad spectrum antibiotics but worsened. Required mechanical ventilation and received systemic steroids. Initially improved but then deteriorated rapidly. A bronchoalveolar specimen revealed Coccidioides immitis.
diganosis?
Disseminated coccidioidomycosis with atypical rash
The following statements about Coccidioides immitis are correct EXCEPT:
A. It can grow in the human body.
B. It is a dimorphic fungus.
C. It is found in the United States in a particular geographic area.
D. It only causes serious infection in immunocompromised people.
D. It only causes serious infection in immunocompromised people.
t/f: Immunosuppression predisposes to disseminated disease
true
what are predisposing factors to a candida albican infections?
Immunosuppression
Broad-spectrum antibiotics
what are predisposing factors to a cryptococcus neoformans infections?
AIDS
Immunosuppression
t/f: Disseminated disease can occur in immunocompetent people
true
characteristics of candida albicans
commensal (oropharynx, gut, and skin)
of endogenous origin
opportunistic
nosocomial
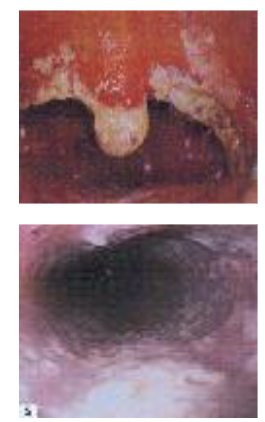
A 24 years old female partner of an IVDU presents with weight loss, pain on swallowing (odynophagia), and nausea
Superficial, raised white plaques on mucosal surface of esophagus viewed through endoscope.
Patient found to have HIV infection and advanced AIDS at presentation
Oropharyngeal/Esophageal candidiasis
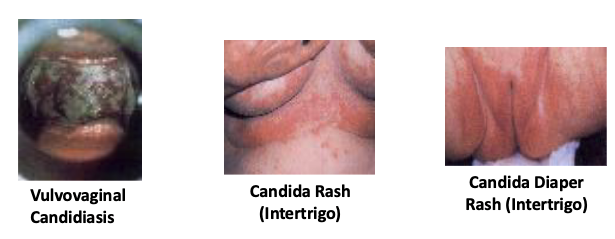
what are some different forms of mucocutaneous candidiasis?
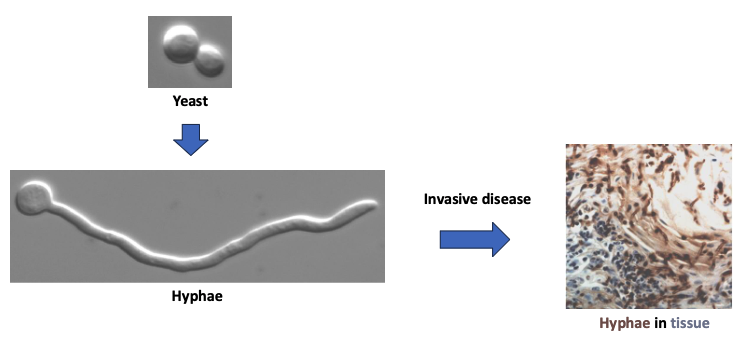
what does it mean that Candida albicans is a dimorphic fungus?
55 years old male was admitted to ICU after perforated duodenal ulcer. Underwent drainage of intraabdominal abscess and repair of ulcer 10 days ago. On IV nutrients and broad-spectrum antibiotics.
Develops fever of 39.9 C, hypotension
WBC = 18,200 with 90% neutrophils
Blood cultures in 2/4 bottles positive for “yeast”
Invasive candidiasis
mortality rate of Invasive candidiasis
40%
Predisposing factors for invasive candidiasis
Cancer, organ and bone transplants, AIDS
Burns, surgeries, trauma, long-term use of intravenous or intra-arterial catheters
Treatment with broad-spectrum antibiotics
characteristics of invasive candidiasis?
• Critically ill or post-surgical patients
• Neutropenic (neutrophil deficient) hosts
• Dissemination
• Skin, Eyes, Bone
• Difficult to diagnose
Treatment strategies for Invasive Candidiasis
remove vascular catheter
reduce immunosuppression
treat with antifungal agent
A 25-year-old male patient has creamy white patches with a cottage- cheese-like appearance on his tongue. The patient notes that he has difficulty swallowing. The patient was healthy as a child and has not consulted a physician for several years. He is not currently taking any medications. Infection with what agents would you suspect?
A. Candida albicans and Streptococcus mutans
B. Candida albicans and Streptococcus pneumoniae
C. HIV and Candida albicans
D. HIV and Streptococcus mutans
C. HIV and Candida albicans
what is the most common cause of fungal meningitis?
Cryptococcus neoformans
what can cause reactivation and dissemination to CNS of Cryptococcus neoformans?
immunosuppression
what is the most common predisposing factor of reactivation/dissemination of Cryptococcus neoformans?
AIDS
Cryptococcus neoformans is ______ in the environment and is typically cleared but can cause…?
ubiquitous
latent infections
Cryptococcal meningitis: onset
acute or gradual
Cryptococcal meningitis disease correlates with
level of immunosuppression
In AIDS patients, there is often another site of infection → Skin, lung, blood
Cryptococcal meningitis disease symptoms
– Headache, lethargy, coma, personality changes, memory loss
– Fever sometimes present
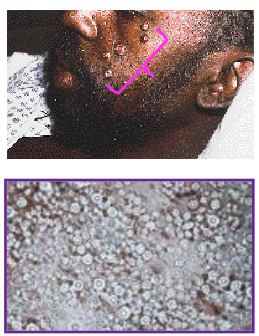
32 years old male, HIV+.
Presents with papules, often umbilicated, on his face and body.
Sample obtained by curettage from one of the papules showed an encapsulated yeast.
Cultures of CSF, blood and skin grew Cryptococcus neoformans.
He was successfully treated with Amphotericin B, followed by daily oral fluconazole
Cryptococcal meningitis
what is an example primary fungal pathogen?
Coccidioides immitus
what is an example opportunistic fungal pathogen?
Candida albicans (colonize oropharynx, GI, skin)
Cryptococcus neoformans
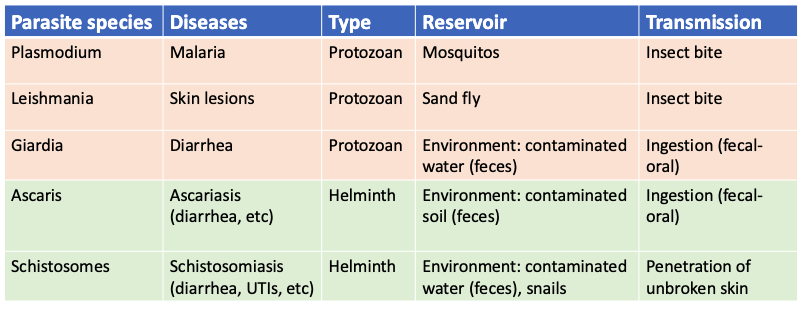
parasites are prokaryotes/eukaryotes?
eukaryotes (therefore, they share many aspects of the cellular physiology with humans)
Unicellular parasites are called ..?
Multicellular parasites are called …?
protozoa
helminths (worms)
what are the different grwoth strategies of parasites?
extracellularly
Some protozoa and all helminths
Often, fecal-oral transmission
intracellularly
Some protozoa
Vector transmission (insect bite)
unstable in environment
what’s an example of a parasite that replicates extracellularly?
Giardia species (diarrhea) grow/multiply in lumen of GI tract
what’s an example of a parasite that replicates intracellularly?
Plasmodium species (malaria) grow/multiply in RBCs
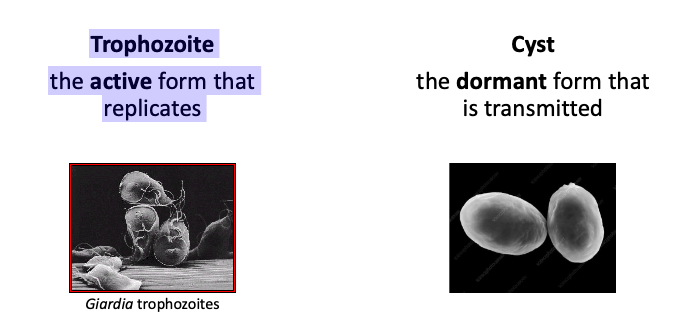
Protozoa are unicellular organisms that typically, exist as two forms:
trophozoite (active form that replicates)
cyst (dormant form that is transmitted)
malaria infects 2 hosts:
humans and mosquitor=s
Malaria: encounter, entry, and multiplication
Encounter: infected mosquitoes
Entry: bite
Multiplication: inside red blood cells (RBCs)
malaria: disease/symptoms
• flu-like illness, fever, chills, headache, muscle aches, and tiredness
• nausea, vomiting, and diarrhea may also occur
• Ranges from very mild illness to severe disease and even death
malaria: treatment and prevention
Prevention: insect repellent, bed nets, drugs
Treatment: drugs
Leishmaniasis has 2 hosts:
humans and sand flies
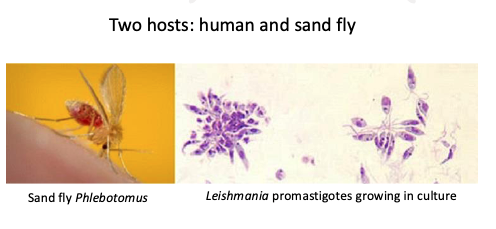
Leishmaniasis: encounter, entry, and multiplication
Encounter: infected sand flies
Entry: bite
Multiplication: inside macrophages

Leishmaniasis: disease/symptoms
• Cutaneous: volcano-like skin sores
• Visceral: fever, enlarged spleen and liver, weight loss, low blood counts
• Asymptomatic
Leishmaniasis: prevention/treatment
Prevention: insect repellent
Treatment: drugs
Giardia: encounter, entry, and multiplication
Encounter: contaminated water, mountain streams
Entry: fecal-oral route
Multiplication: lumen of the GI tract
Giardia: disease, prevention, and treatment
Disease: diarrhea
Prevention: drinking clean water
Treatment: drugs
The following statements about protozoa are correct EXCEPT:
A. Despite being unicellular, protozoa can exist in multiple developmental stages.
B. Protozoa are prokaryotes, so their infections are treated with antibiotics.
C. Protozoa are single-celled, microscopic organisms that can perform all the necessary functions of metabolism and reproduction.
D. Protozoa are typically transmitted indirectly.
B. Protozoa are prokaryotes, so their infections are treated with antibiotics.
Helminths are multicellular organisms that grow and multiply _________ because of their large size
extracellularly
how many hosts do helminths infect?
Complex lifecycles with more than one host.
Often unable to complete their lifecycle in one host, so they cannot increase in number within that host.
what is the most common human helminthic infection globally?
Ascariasis
Ascariasis is transmitted via
fecal/oral route
Occurs in warm climates where untreated human feces are present
Ascariasis lifecycle
Ascaris eggs are excreted in stool
Eggs must mature into larvae in a warm environment
Larvae are ingested and grow into worms in different organs in the human host (GI and lung)
Ascariasis: encounter, entry, and multiplication
Encounter: untreated feces
Entry: ingestion
Multiplication: complex lifecycle
Ascariasis: disease and treatment
Disease: Abdominal pain, intestinal obstruction (Mild symptoms)
Treatment: drugs
Schistosomiasis infect 2 hosts:
humans and freshwater snails
Schistosomiasis: entry, encounter, and multiplication
Encounter: skin contact with contaminated water (grows in freshwater snails)
Entry: penetrates unbroken skin
Multiplication: complex lifecycle (Human→ liver, bowel, bladder)
Schistosomiasis: disease and treatment
Disease: rash, hepatic scarring that causes obstruction of blood flow and build up of fluid in the abdominal cavity
Treatment: drugs
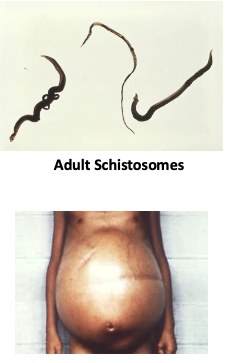
Schistosomiasis lifecycle
Eggs in water infect snails and mature into cercariae (juveniles)
Cercariae leave the snail and penetrate the skin of a human, enter the blood, mature to worms in abdominal veins
Female worms produce eggs that migrate to the GI and the bladder
Eggs are excreted in stool and urine and end up in fresh water
Which of the following statements about the prevention and control of parasitic infections is TRUE?
A. Consumption of well-cooked beef reduces the risk of malaria.
B. Good oral hygiene protects against giardiasis.
C. Insect repellents and insecticide treated bed nets represent effective methods for the prevention of ascariasis.
D. Wearing of protective footwear in locations where humans have defecated protects against schistosomiasis.
D. Wearing of protective footwear in locations where humans have defecated protects against schistosomiasis.