10. Vascular Disorders: Hemorrhage, Emboli, & Shock
1/75
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
76 Terms
What does failure of hemostasis often result in?
hemorrhage or thromboses or in certain disease states, a combination of both
What does damage or loss of/abnormal function to one of the four major factors that influence hemostasis result in?
hemorrhage
What are the 4 major factors that influence hemostasis?
E
B
P
C
endothelium
blood vessel
platelets
coagulations factors
What are causes of hemorrhage?
T
I
C
T
D
N
S
trauma
infectious agents
collagen disorders
thrombocytopenia or decreased platelet function
disseminated intravascular coagulation (DIC)
neoplasia
severe liver disease
What infectious agents can lead to hemorrhage?
B
V
F
I
E
bacteria
viral
fungal
immune complexes
endotoxemia
Hemarthrosis is most often a result of what type of deficiency in guinea pigs? Why is this typical?
vitamin C; guinea pigs cannot synthesize ascorbic acid (vitamin C) from glucose like most mammalian species
What is vitamin C deficiency known as?
scurvy
What is vitamin C required by and why?
fibroblasts, odontoblasts, and osteoblasts to form collagen, dentin, and osteoid
What happens when you are deficient in vitamin C?
lack of bone deposition as well as hemorrhage
Why does hemorrhage occur with vitamin C deficiency?
the collagen is weaker, resulting in increased vessel fragility
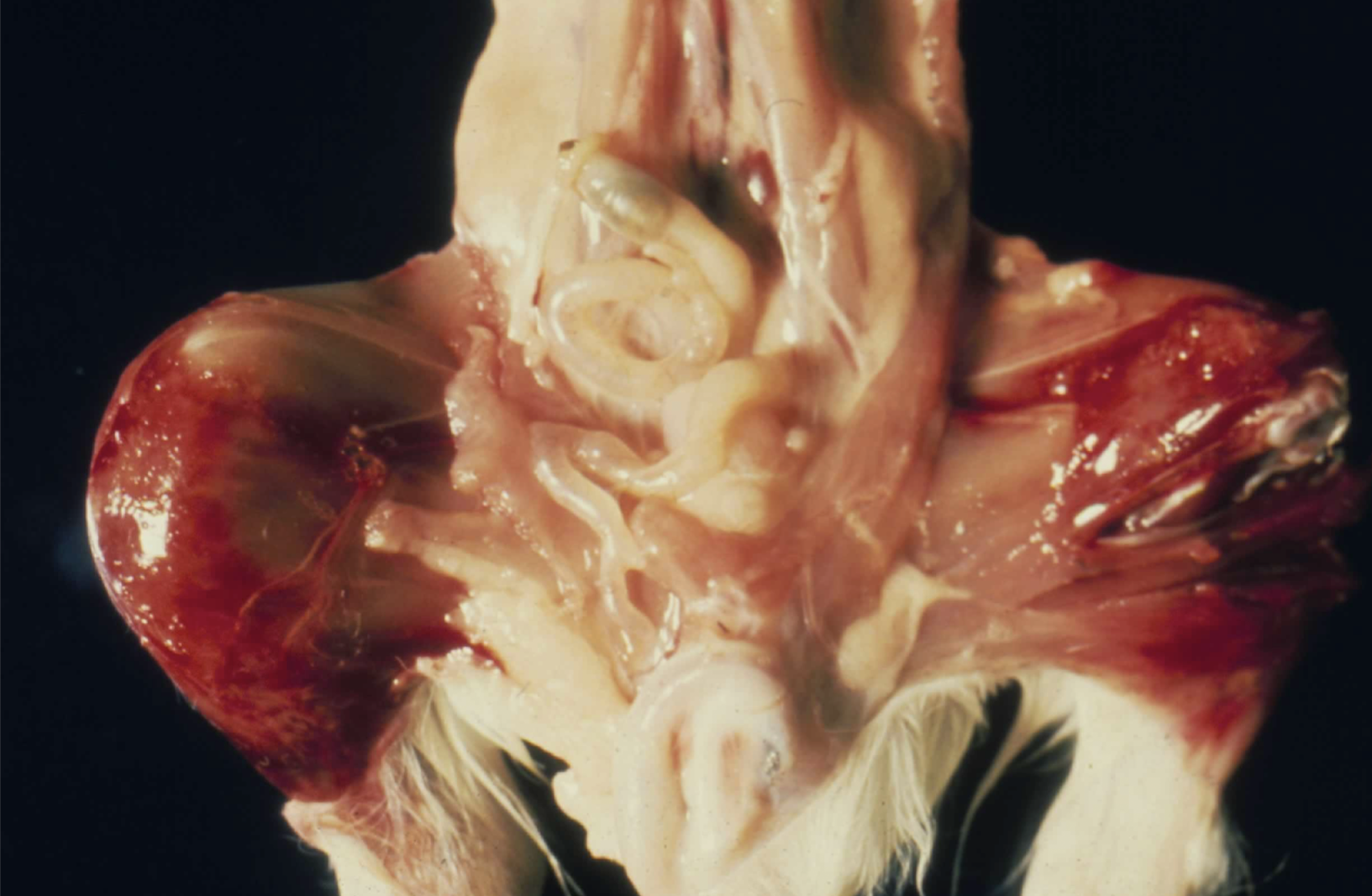
What is this image showing? Why is it probably occurring?
hemarthrosis; vitamin C deficiency

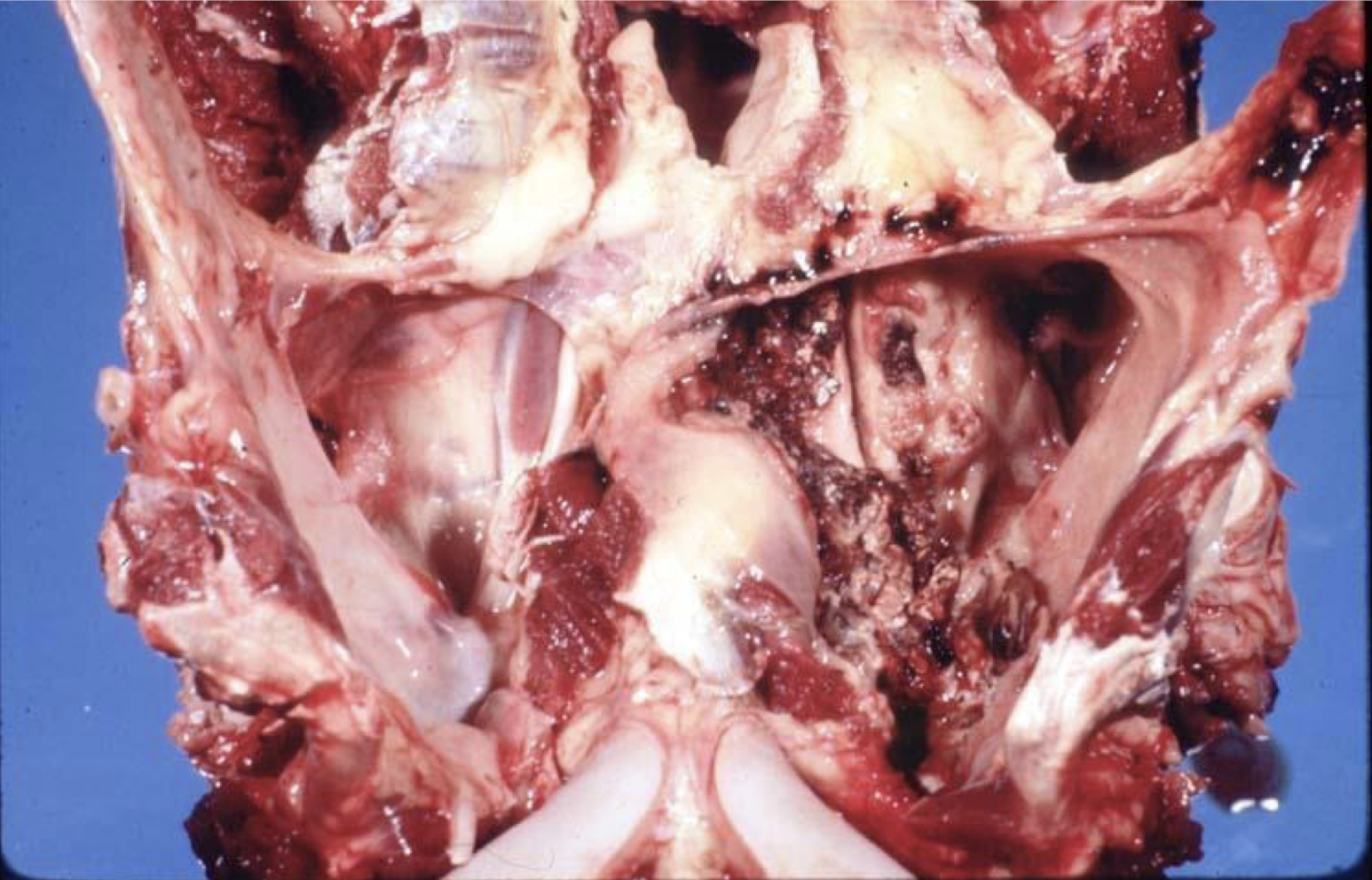
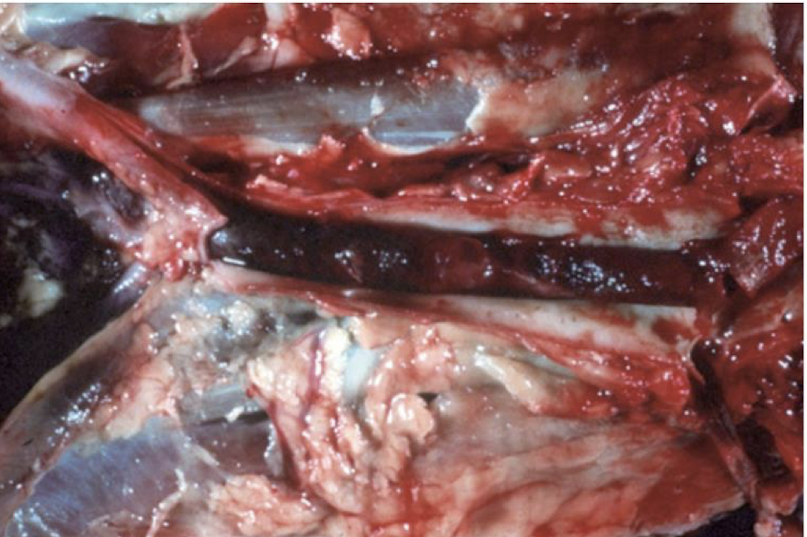
What is this image showing?
extensive hemorrhage of the right hind limb due to anticoagulant rodenticide toxicosis
What do anticoagulant rodenticides do?
inhibit the vitamin K dependent coagulation factors (factors II, VII, IX, and X)

What is this image showing?
collagen disorder
What do collagen disorders result in? Why?
weakening of the vessels and hemorrhage; vessels have collagen in and surrounding them to support them
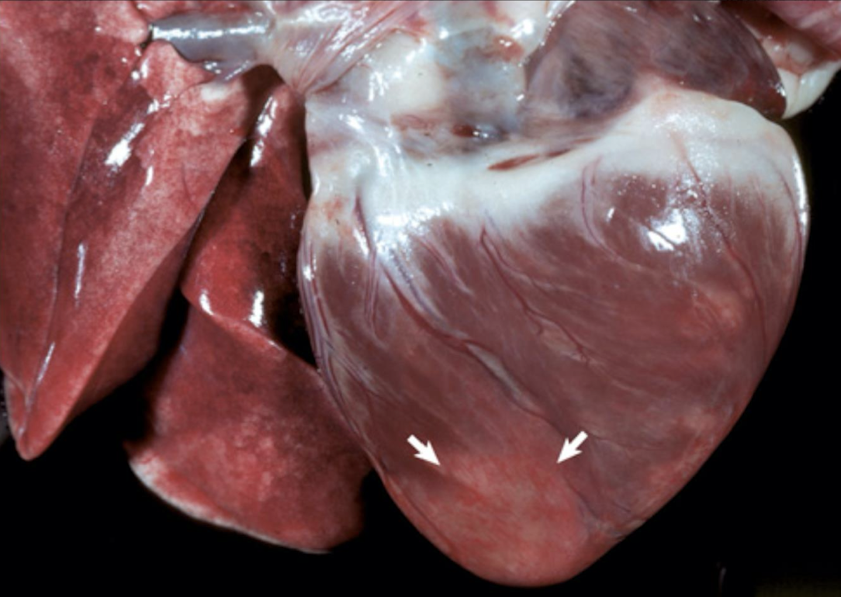
What is this image showing?
horse gutteral pouch mycosis
extensive hemorrhage into the pericardial sac that can result in the inability of the heart to expand and contract properly, which is a condition known as cardiac tamponade which often results in sudden arrest
hemopericardium
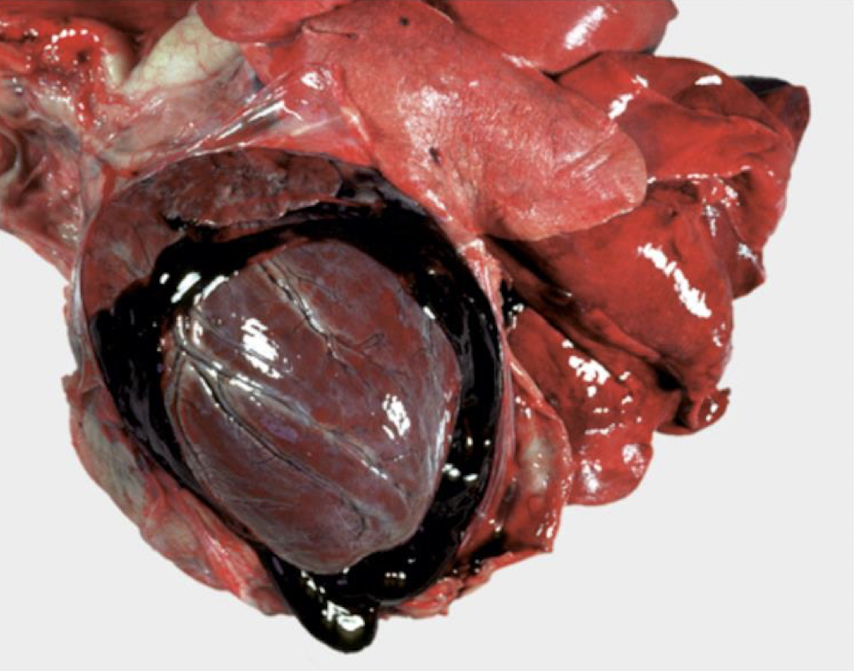
What is this showing?
hemopericardium
What are the general causes of thrombocytopenia?
C
I
I
I
P
B
can’t produce enough platelets
increased platelet destruction
increased use of platelets
iatrogenic
platelet sequestration in sinusoids of the spleen
blood loss
What are reasons that an animal could not produce enough platelets?
E
R
V
L
estrogen toxicity
radiation/drugs
viral
liver failure
What is a main reason for increased platelet destruction?
autoimmune
What is the main reason for increased use of platelets? Why?
DIC; intravascular coagulation and consumption of platelets and coagulation factors

What is this an image of?
androgen producing adrenal tumor (decreased production related thrombocytopenia)
What are reasons for decreased platelet function?
I
V
U
N
inherited along with coagulation factor inherited deficiencies)
von willebrand’s disease (autoantibodies against vWf leads to decreased platelet aggregation)
uremia
NSAIDs (aspirin)
mechanism involved in the formation of an excessive or inappropriate thrombus (blood clot) within an injured blood vessel
thrombosis
mixture of platelets, fibrin, erythrocytes, and inflammatory cells which are adhered to the vascular wall (blood or lymphatic vessel)
thrombi
explains the major determinants of thrombosis
Virchow’s triad
What are the 3 major determinants of thrombosis?
A
H
E
abnormal blood flow
hyper coagulability
endothelial injury
What is the most important factor of thrombosis? Why?
endothelial injury; potent stimulus for platelet aggregation and coagulation
What are examples of abnormal blood flow?
reduced blood flow and turbulent flow
In veins, what is the most important determinant of thrombosis? Why?
reduced blood flow; have a slow rate of flow anyway
What can reduced blood flow cause?
accumulation of activated coagulation factors and increase their contact with platelets and the endothelium
Where are sites of reduced blood flow? What does this mean for that animal?
dilated heart chambers and dilated vessels; predispose an animal to thromboses
What is the effect of turbulent blood flow?
disrupts lamina flow such that the thin layer of plasma which separates the cellular constituents of blood, such as platelets and coagulation factors, now come into contact with the endothelium
What else can turbulent blood flow do?
directly damage the endothelium
What is hyper coagulability generally due to?
increase or decrease in the concentration of activated hemostatic proteins either from enhanced activation or decreased degradation of these proteins
What is the most common cause of hyper coagulability?
inflammation
Arterial thrombi often form a ________ ________. They are ________ ________ to the wall of the vessel or the endocardium. They are ________ than venous thrombi because they tend to not have a lot of ________ embedded within in. This is because they are formed under ________ pressure and ________ flow rates rather than venous thrombi. They are also ________ and ________.
tapering tail; loosely adherent; paler; RBCs; higher; higher; dull; friable
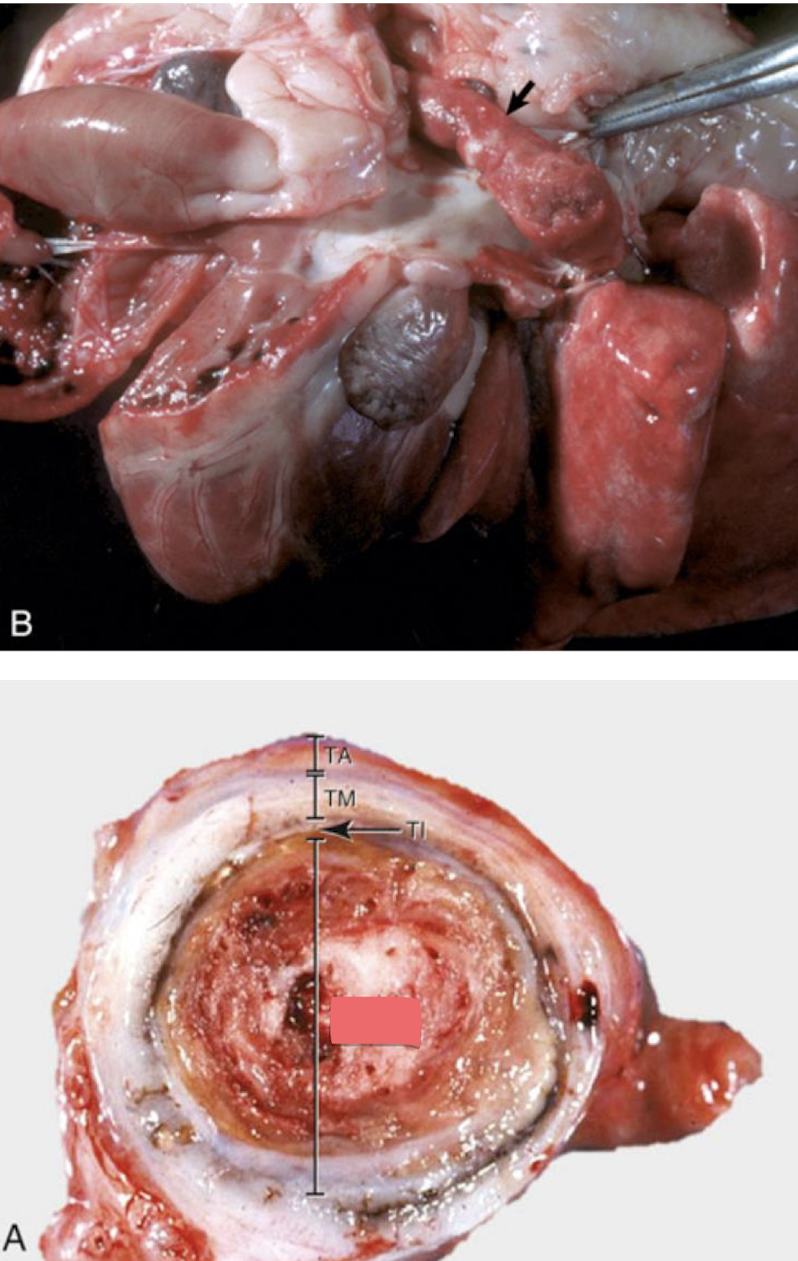
What is this showing?
arterial thrombus
Venous thrombi become ________ to the vessel wall, as they are formed under ________ pressure circumstances with increased ________ ________. They tend to have more ________ within the thrombus. They are ________, mottled ________ ________ with regions of ________ ________ to ________. They are ________ ________ to the wall but will occlude the entire ________ and often do not have an apparent ________ as the arterial thrombi do.
molded; low; blood stasis; erythrocytes; dull; dark red; pale tan; red; loosely adherent; lumen; tail
If you see a dull thrombus, what should this tell you?
it is not a postmortem change

What is this showing?
venous thrombi
How are small thrombi removed? What about larger ones?
via thrombolysis; often unable to be completely cleared
How are larger thrombi cleared?
phagocytes come in and clear as much of the debris as possible but invasion by fibroblasts occurs and formation of a new vascular lumen called recanalization occurs
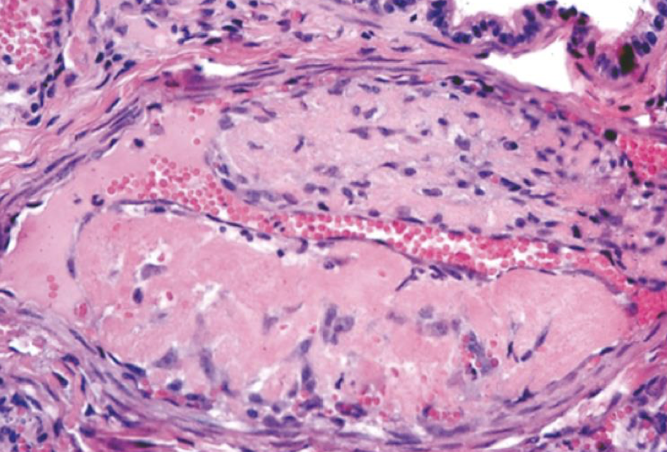
What is this showing?
recanalization
What are the two types of postmortem clots?
C
C
current jelly clots
chicken fat clots
What is the appearance of postmortem clots? What else is unique about them?
smooth and glistening; they are not adhered to the vessel wall at all
What is the appearance of current jelly clots?
dark-red/purple

What is this showing?
postmortem clots
piece of free-floating foreign material within a vessel
embolus or emboli
What are types of emboli?
T
B
P
F
F
N
A
thromboemboli
bacterial
parasitic
fat
fibrocartilagenous
neoplastic
air
A saddle thrombus is not a _________ but a ________. That is because it is not ________ to the ________, but instead comes from the ________.
thrombus; thromboemboli; adhered; wall; heart
What is this showing?
saddle thrombus
What is significant about these pictures?
showing the emboli that the saddle thrombus came from
What is shock also known as? What is it?
cardiovascular collapse; circulatory dyshomeostasis
True or false: The causes of shock are very diverse but the results are similar.
true
What will persistent shock lead to?
irreversible cell injury and death
Shock causes ________, which results in impaired ________ ________, ________ ________, a shift to ________ ________, followed by ________ ________ and ________.
hypotension; tissue perfusion; cellular hypoxia; anaerobic metabolism; cellular degeneration; death
reduced vascular perfusion due to underlying cause
shock
What are the three types of shock?
C
H
B
cardiogenic
hypovolemic
blood maldistribution
failure of the heart of adequately pump blood due to decreased stroke volume and cardiac output
cardiogenic shock
What are the causes of cardiogenic shock?
M
V
F
A
O
myocardial infarction
ventricular tachycardia
fibrillation or other arrhythmias
advanced dilated or hypertrophic cardiomyopathy
obstruction of blood flow (pulmonary thromboembolism, pulmonary or aortic stenosis, caval syndrome)
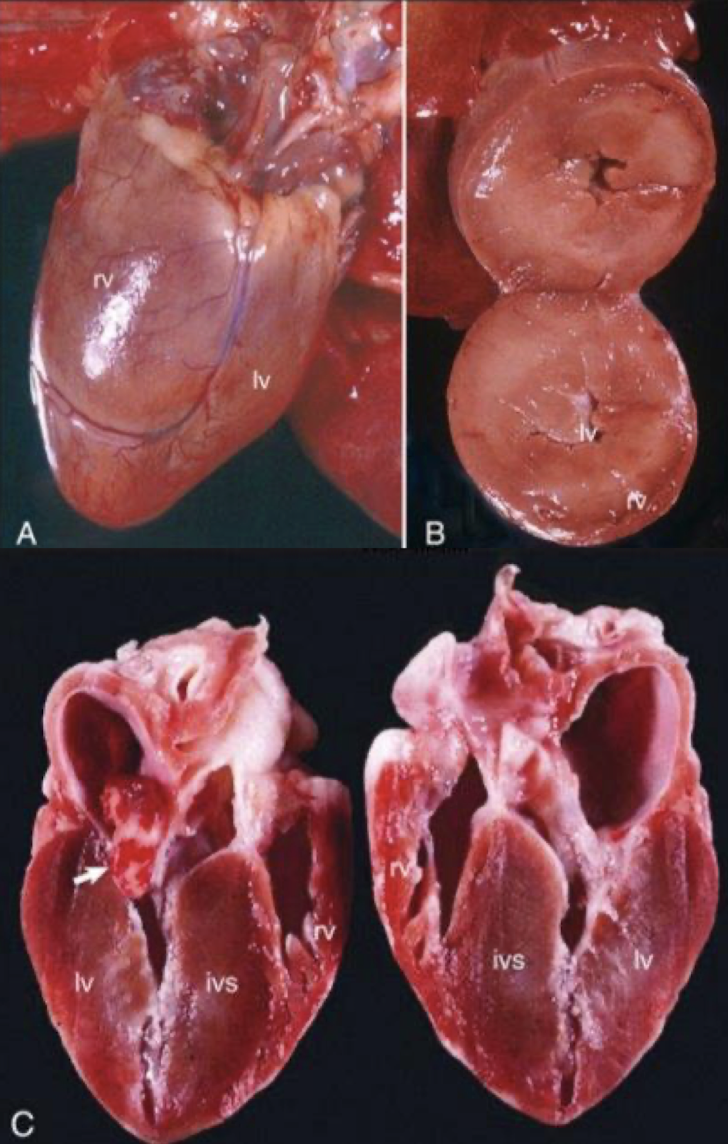
What is this showing?
myocardial infarction (cardiogenic shock)
reduced circulating blood volume leading to tissue hypo perfusion, peripheral vasoconstriction, and an increase in blood flow to vital oprgans such as the heart, brain, and kidney
hypovolemic shock
What are causes of hypovolemic shock?
H
F
hemorrhage
fluid losses (vomiting, diarrhea, burns)
Blood loss of up to what percent can be easily compensated for?
10%
Blood loss which approached what percent results in dramatic drops in blood pressure and cardiac output?
35-45%
decreased peripheral vascular resistance resulting in pooling of blood in peripheral tissues
blood maldistribution
What are the types of blood maldistribution?
A
N
S
anaphylactic
neurogenic
septic
type I hypersensitivity (IgE induced) reaction, which results in the release of histamine resulting in peripheral vasodilation among other signs (pulmonary bronchoconstriction)
anaphylactic shock
vasodilation results from autonomic discharges followed by venous pooling and hypoperfusion (trauma, electrocution, fear)
neurogenic shock
What is the most common type of blood maldistribution?
septic shock
peripheral vasodilation caused by the infectious agent (bacteria or fungus) which induces excessive release of inflammatory mediators
septic shock
What is the most common type of septic shock?
endotoxic shock from endotoxin which is an LPS in the cell wall of gram negative organisms
What are the clinical and morphological features of shock?
H
W
T
H
R
H
L
hypotension
weak pulse
tachycardia
hyperventilation with pulmonary rales
reduced urine output
hypothermia
late stage decompensated leads to organ and system failure
characterized by compensatory mechanisms which counteract hypoperfusion
nonprogressive stage of shock