Proton Pump Inhibitors (PPIs)
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
45 Terms
The Proton Pump
the final step in gastric acid secretion in the parietal cell is ______ ______ ______.
carried out by an enzyme ____/____-______ or the “proton pump” —> catalyzes the exchange of _______ ions for ______ ions in the stomach.
exchange is stimulated by ______ messengers (Ca2+ and cAMP) from ______ activation (histamine, gastrin, acetylcholine)
inhibitors of the pump will block both ______ and ______ secretion
extrusion of protons
H+/K+-ATPase, hydrogen, potassium
secondary, GPCR
basal, stimulated
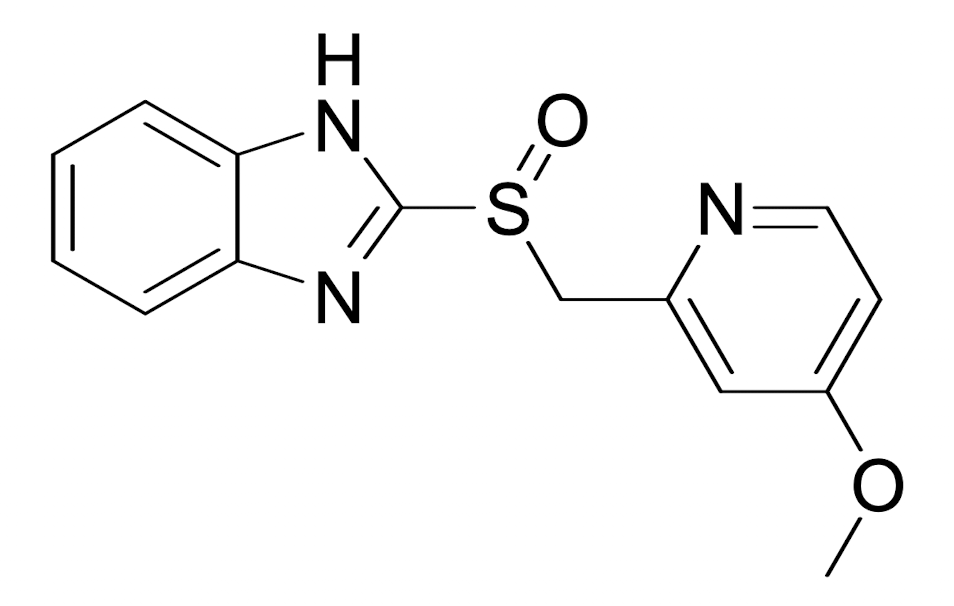
What does this structure represent?
the backbone for PPIs
The final step in gastric acid secretion in parietal cells is mediated by:
H⁺/K⁺-ATPase
The proton pump exchanges which ions across the parietal cell membrane?
Na⁺ out / K⁺ in
Which messenger pathways stimulate activation of the proton pump?
Ca²⁺ and cAMP
Which signaling molecules stimulate gastric acid secretion via GPCRs?
Histamine, gastrin, acetylcholine
Proton pump inhibitors (PPIs) block:
Both basal and stimulated secretion
Which statement correctly describes the action of the gastric proton pump (H⁺/K⁺-ATPase)?
Pumps hydrogen ions into the stomach → increases proton concentration → decreases pH
Which statement best explains why proton pump inhibitors (PPIs) are more effective than H2-receptor antagonists in reducing gastric acid secretion?
H2 antagonists block stimulated gastric acid secretion, but PPIs inhibit the proton pump itself, blocking both basal and stimulated secretion.
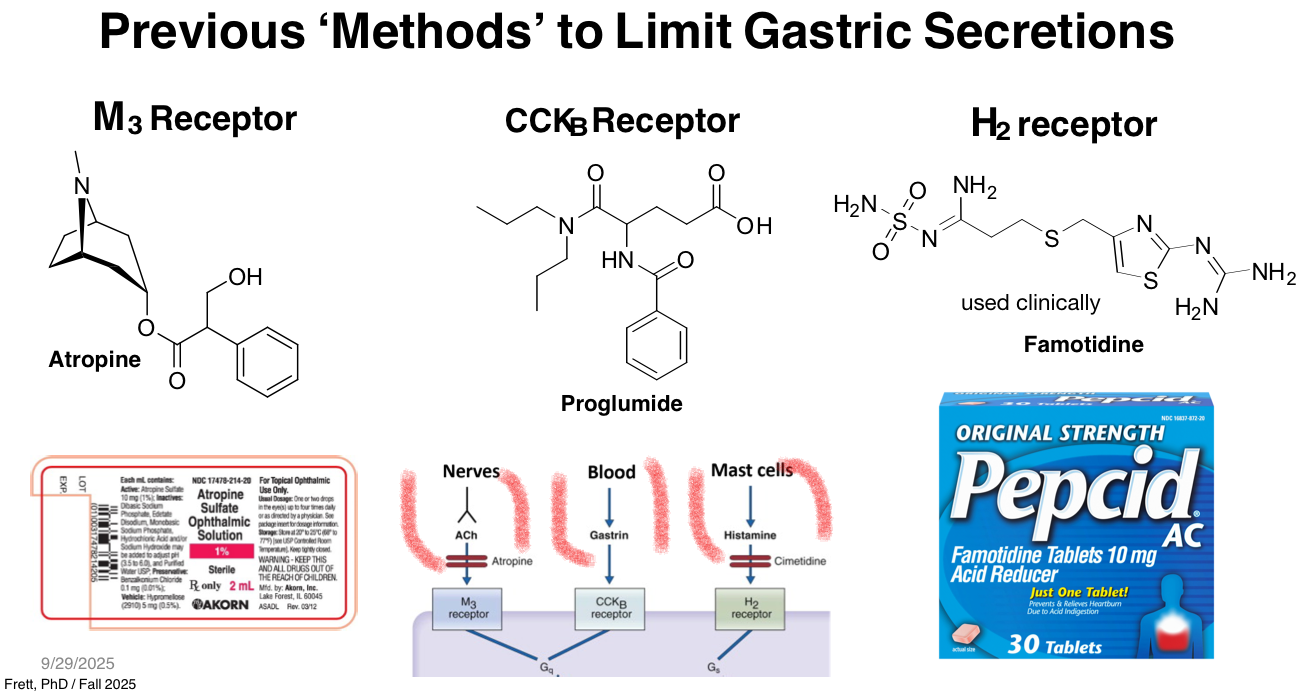
Which statement best explains why older methods (e.g., atropine, proglumide, H₂ antagonists) are less effective than PPIs for reducing gastric acid?
They block only upstream stimulatory pathways (ACh, gastrin, histamine) and do not block the proton pump itself
The drug becomes acidic → increases solubility and dissolution
What happens if a PPI is formulated with HCl?
The drug becomes basic
Proton pump inhibitors are best described as:
Prodrugs activated in acidic environments
Where do PPIs become activated?
Secretory canaliculus of parietal cells
PPIs react with which functional group on the proton pump?
Thiol group
At neutral pH PPIs are:
Inactive, chemically stable, lipid-soluble, weak bases
How do PPIs reach the parietal cells?
From the bloodstream
Why do PPIs accumulate in the secretory canaliculi?
They become protonated and trapped
Parietal cell canaliculi are unique because they:
Have the lowest pH in the body
Once protonated, PPIs convert to:
Sulfenamide and sulfenic acid
PPIs bind to the pump by:
Covalent bond formation
PPIs convert to their active form fastest at:
Very low pH (acidic environment)
Why do PPIs require enteric coating?
To prevent premature activation in the acidic stomach
Where are PPIs absorbed after oral administration?
Small intestines
What happens as pH increases?
Conversion rate decreases
Why must PPIs avoid activation in the stomach?
They would be trapped and not reach parietal cells
Most drug absorption occurs in intestines because:
Larger surface area
PPIs irreversibly inhibit the H⁺/K⁺-ATPase by:
Covalently reacting with thiol groups on cysteine residues of the pump
At least ______ molecules of the PPI sulfenamide form must react with thiol groups on the H⁺/K⁺-ATPase to fully inhibit the pump.
two
Which cysteine residue is a key target on the H⁺/K⁺-ATPase for covalent binding by PPIs?
Cys-813
PPI specificity is primarily derived from:
Requirement for acidic conditions and trapping in the canaliculus
Trapping of the protonated PPI occurs in the:
Acidic secretory canaliculus adjacent to the enzyme
Omeprazole administration results in:
Permanent inhibition of H⁺/K⁺-ATPase in vivo
Acid secretion resumes only when:
New H⁺/K⁺-ATPase pumps are synthesized and inserted in the membrane
PPIs are formulated as:
Enteric-coated microcapsules or granules
Why are PPIs enteric-coated?
To prevent activation in the mouth and stomach
What happens if the enteric coating is disrupted in the mouth before swallowing?
Neutral pH releases drug prematurely
Premature release in the mouth or esophagus leads to:
Cyclization in the stomach lumen and drug inactivation
In which GI region do PPIs normally dissolve and absorb due to pH?
Duodenum (pH ~6.8)
Which statement best describes esomeprazole?
S-enantiomer of omeprazole
Phase I metabolism of PPIs typically includes:
O-dealkylation and sulfone formation
Phase II metabolism of PPIs primarily involves:
Glucuronidation
OTC PPIs like omeprazole should be used for a maximum of:
14 days
Why is long-term PPI use avoided without supervision?
Raises stomach pH, increasing infection risk
PPIs MOA
PPIs are prodrugs
Inactive at neutral pH
Lipid-soluble, weak bases → can cross membranes
Absorbed into the bloodstream and delivered to parietal cells
Diffuse into the secretory canaliculi
Only location in body with very low pH
Become protonated (acidic environment)
Acid activates them and causes them to become trapped in the canaliculus
Chemical rearrangement
Protonated parent drug → forms sulfenic acid and sulfenamide
Covalent binding
Sulfenamide reacts with thiol (–SH) groups on H⁺/K⁺-ATPase
Forms covalent disulfide bond
Permanent enzyme inactivation
Pump is irreversibly inhibited
Acid secretion stops
Recovery only when new pumps are made
Parietal cell must synthesize and insert new pumps into membrane
(Hence long duration despite short half-life in plasma)