(24) Renal Acid/Base Regulation & Micturition
1/71
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
72 Terms
What are the 3 main chemical buffering systems in the body?
bicarbonate, phosphate, proteins
What is the most important extracellular buffer?
bicarbonate
What is the main important renal tubule and intracellular buffer?
phosphate
Are proteins an important intracellular or extracellular buffer?
intracellular
The renal system is involved in excretion of acidic or basic urine based on the balance between the secretion and reabsorption of what ions?
bicarbonate, H+
(excretion of nonvolatile acids plays a role too)
What are the 3 fundamental mechanisms in which the kidneys regulate ECF H+ concentration?
H+ secretion, bicarbonate reabsorption, production/absorption of new bicarbonate
In order to reabsorb bicarbonate, what must be secreted back into the renal tubules?
H+
Where does the majority of bicarbonate reabsorption and H+ secretion occur?
proximal tubule
Even though most H+ secretion occurs in the proximal tubule, it can actually occur in all parts of the renal tubules except which part(s)?
thin limbs of loop of Henle
True or false: H+ secretion is required for HCO3 reabsorption.
true
2 mechanisms of H+ secretion
secondary active transport via Na/H antiporter, primary active transport via H+ ATPase and H+/K+ ATPase
What transporter is involved in H+ secretion via secondary active transport?
Na/H antiporter
Where is the Na/H antiporter found? (3)
proximal tubule, thick ascending limb, early distal tubule
Na/H counter-transport 1: What provides the energy needed for Na/H counter-transport?
Na/K ATPase
Na/H counter-transport 2a: Does Na+ flow into or out of the tubular epithelial cell?
into
(from tubular lumen)
Na/H counter-transport 2b: Is H+ pumped into or out of the tubular epithelial cell?
out
(into tubular lumen)
Na/H counter-transport 3: Once H+ flows out of the tubular epithelial cell and into the tubular lumen, what happens to it? (Hint: How does it interact with what's around it?)
combines with bicarbonate to form carbonic acid
Na/H counter-transport 4: Once H+ flows out of the tubular epithelial cell and into the tubular lumen, it combines with bicarbonate to form carbonic acid. The carbonic acid then dissociates into what two components in the lumen? Via what enzyme?
CO2 and H2O, carbonic anhydrase
Na/H counter-transport 5: CO2 diffuses into the renal epithelial cells and recombines with H2O to reform what substances? Via what enzyme?
carbonic acid, carbonic anhydrase
Na/H counter-transport 6a: Carbonic acid forms from CO2 and H2O in the tubular epithelial cell. It then dissociates into bicarbonate and H+ (still in the tubular cell). What happens to the H+?
stored as a pool to be secreted
Na/H counter-transport 6b: Carbonic acid forms from CO2 and H2O in the tubular epithelial cell. It then dissociates into bicarbonate and H+ (still in the tubular cell). What happens to the bicarbonate?
released into the blood
Na/H counter-transport 7: Due to Na/H counter-transport, bicarbonate ions are indirectly reabsorbed in the renal tubules (since CO2 diffuses into tubular epithelial cells and then forms bicarbonate). What is the net result?
what gets filtered from the blood is replaced
What two transporters are involved in H+ secretion via primary active transport?
H+ ATPase, H/K ATPase
Where does primary active transport via H+ ATPase and H+/K+ ATPase occur?
late distal and collecting tubules
H+ primary active transport 1a: What specific kind of tubular cells are involved in primary active transport of H+ ions?
intercalated cells
H+ primary active transport 1b: What else are intercalated cells involved in besides primary active transport of H+?
K+ reabsorption
(via H/K ATPase)
H+ primary active transport 2: How is H+ secreted via primary active transport into the renal tubules?
H/K ATPase or H+ ATPase
(K+ is reabsorbed and pumped out into blood, H+ is pumped into renal tubules)
H+ primary active transport 3: If there's any remaining filtered ____ that makes its way far enough into the renal tubule system to get to the distal tubules where intercalated cells are, the H+ that's actively transported out of the cell and into the renal tubules (either via H/K antiporter or H+ ATPase), binds to the filtered ____.
forms carbonic acid in the renal tubule, and then dissociates into CO2 and H2O. Both of these are taken up into renal tubular epithelial cell.
bicarbonate
H+ primary active transport 4: Once H+ that is secreted into the renal tubules binds to filtered bicarbonate that makes its way far enough to get to the H+, this allows carbonic acid to form in the renal tubule, which then dissociates into CO2 and H2O. What happens to both of these?
taken up into tubular cells
H+ primary active transport 5: CO2 diffuses into the renal epithelial cells and recombines with water to reform what? Via what enzyme?
carbonic acid, carbonic anhydrase
H+ primary active transport 6b: Carbonic acid is formed and dissociates into bicarbonate and H+. What happens to the bicarbonate?
released back into the blood
H+ primary active transport 6a: Carbonic acid is formed and dissociates into bicarbonate and H+. What happens to the H+?
creates a pool of H+ to be secreted (via primary active transport)
When we've reabsorbed all of the bicarbonate that was filtered, but we're still pumping H+ into the renal tubule to get rid of the excess, what do we use as a buffer now?
**allows for the secretion of a large amount of H+ without reducing the urine pH below 4.5
phosphate
Why is it important to use phosphate as a buffer when bicarbonate is insufficient?
to prevent urine from being too acidic
In phosphate buffering, secreted H+ combines with phosphate to be excreted in what form?
H2PO4 (dihydrogen phosphate)
With the phosphate buffering system, there is a net gain of a 1 new HCO3 in the blood. Why?
H+ is not combining with HCO3
(combines with phosphate instead, so HCO3 can be used as a buffer in the blood)
Which buffering system in the renal tubules is more important: phosphate or ammonia?
ammonia
When does the ammonia buffering system in the renal tubules typically come into play?
when there is acidosis and phosphate system is saturated
One mechanism of the ammonia buffering system involves what substance being actively transported into the renal epithelial cells in the proximal tubule?
glutamine
Where is glutamine actively transported into the renal epithelium via the ammonia buffering system?
proximal tubule
What happens to glutamine once it is transported into the renal epithelium in the ammonia buffering system?
cleaved into 2 bicarbonate and 2 ammonium
In the ammonia buffering system, when glutamine is transported into the renal epithelium, it is cleaved into 2 bicarbonate and 2 ammonium. What happens to the ammonium?
secreted into renal tubule via Na/NH4 antiporter
What transporter secretes NH4 (ammonium) into the renal tubule lumen after it is cleaved from glutamine?
Na/NH4 antiporter
In the ammonia buffering system, when glutamine is transported into the renal epithelium, it is cleaved into 2 bicarbonate and 2 ammonium. What happens to the bicarbonates?
absorbed into the blood
With ammonia buffering via glutamine, there is a net gain of how many new bicarbonates into the blood?
2
(the 2 cleaved from glutamine)
One mechanism of the ammonia buffering system involves what substance being secreted and combined with H+, producing a substance that is excreted?
NH3
Where is NH3 secreted to be combined with H+ in the ammonia buffering system?
collecting tubule
In the ammonia buffering system, ammonia (NH3) is secreted in the collecting tubule, where it combines with what substance that is also secreted? What is ultimately formed, which is excreted?
combines with H+, forms NH4
The ammonia buffering system accounts for how much of the H+ that is excreted?
50%
The ammonia buffering system accounts for how much of the new bicarbonate produced?
50%
In the ammonia buffering system, for each new ammonium (NH4) excreted, how many new bicarbonates are generated and absorbed into the blood?
1
Which buffering system will the body rely on first: phosphate or ammonia?
phosphate
If we have acidosis, does this cause an increase or decrease in...
1. H+ secretion?
2. H+ excretion?
3. Bicarbonate production and reabsorption?
4. Bicarbonate excretion?
5. pH of urine? (Is it acidic or basic?)
6. pH of plasma? (Does it cause alkalinization or acidification?)
1. increase
2. increase
3. increase
4. stays normal (0, since all filtered is reabsorbed)
5. acidic
6. alkalinization (toward normal)
If we have alkalosis, does this cause an increase or decrease in...
1. H+ secretion?
2. H+ excretion?
3. Bicarbonate production and reabsorption?
4. Bicarbonate excretion?
5. pH of urine? (Is it acidic or basic?)
6. pH of plasma? (Does it cause alkalinization or acidification?)
1. decrease
2. decrease
3. decrease
4. increase
5. basic
6. acidification (toward normal)
Which of the following is NOT involved in renal regulation of ECF pH?
A. HCO3- filtration
B. HCO3- reabsorption
C. H+ secretion
D. H+ reabsorption
D
process by which the urinary bladder empties when it becomes filled
it fills progressively until the tension in its walls rises above a threshold level, which elicits a namesake reflex, which empties the bladder or causes a conscious desire to urinate
micturition
What allows urine to travel from the kidneys to the ureters to the bladder?
peristaltic muscle contractions
muscle surrounding the bladder responsible for compressing the ureter (with its normal tone), preventing back flow of urine when pressure builds up in the bladder
detrusor muscle
As the bladder fills, pressure increases and micturition contractions begin. What causes these contractions?
stretch reflex
(initiated by stretch receptors in the bladder wall)
What initiates the micturition reflex?
stretch receptors in bladder wall
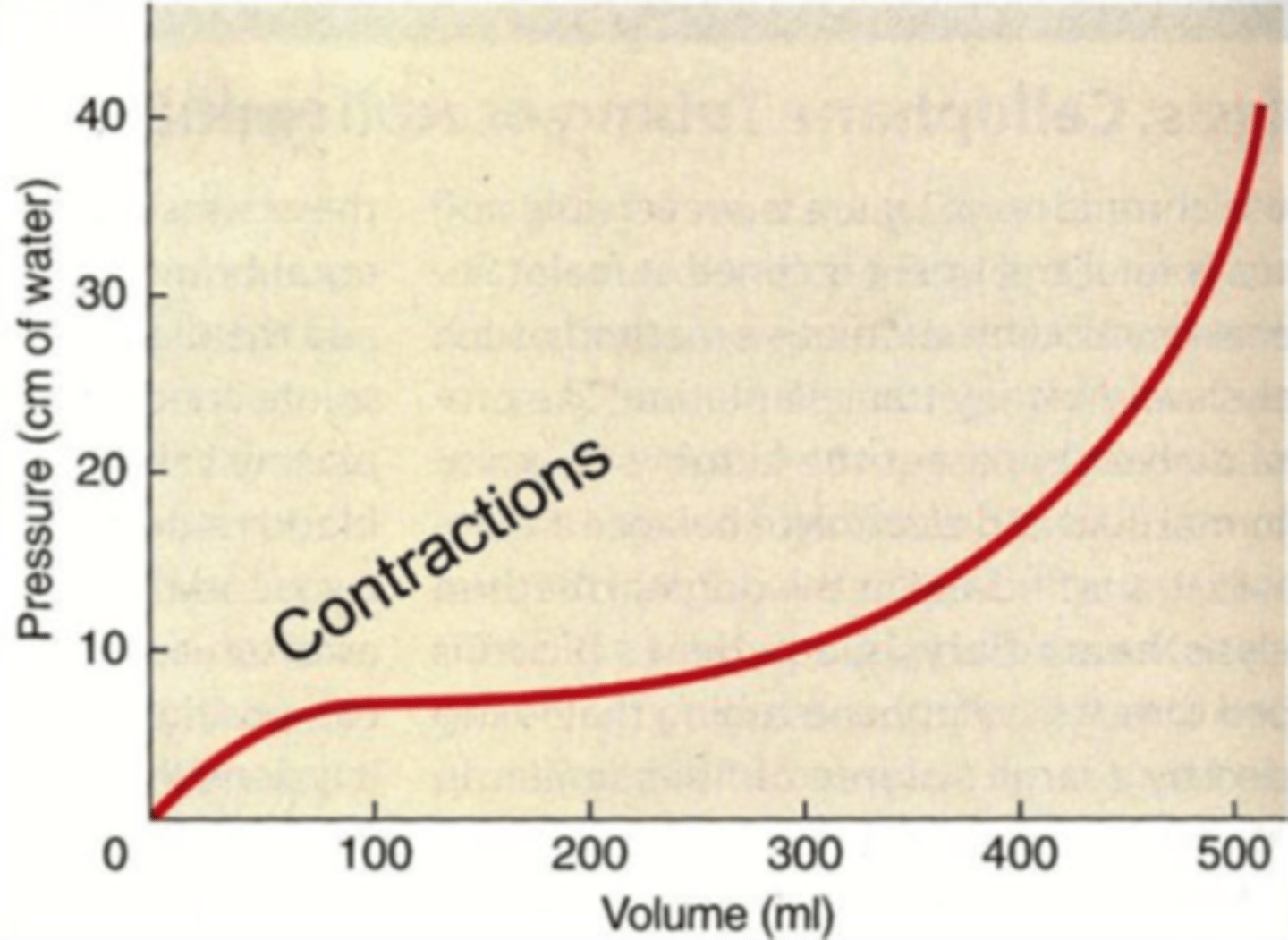
When the bladder is only partially filled, micturition contractions relax spontaneously after seconds. However, as the bladder continues to fill, the contractions become more frequent and stronger, causing relaxation of what structure?
internal sphincter
(external sphincter still remains closed)
Once the bladder reaches a strong degree of contraction, the micturition reflex fatigues and the cycle of contraction ceases, resulting in relaxation of the bladder. If the micturition contraction runs this full cycle and the bladder is not emptied, what happens to the reflex?
inhibited
(this is why you feel like you have to "go" for a while, but then the sensation subsides)
If the micturition reflex becomes powerful enough, this causes the eventual relaxation of what structure?
Note: If this reflex can overpower the constriction by this structure, micturition occurs.
external sphincter
Where does the micturition reflex occur?
spinal cord
(autonomic reflex, even though we can develop control of the external sphincter)
The micturition reflex can be inhibited or facilitated by centers in what two areas in the brain?
brainstem, cerebral cortex
How can we voluntarily cause micturition?
voluntary contraction of abdominal muscles
How does voluntary contraction of the abdominal muscles cause voluntary micturition?
increases bladder pressure and stimulates stretch receptors
Does voluntary contraction of abdominal muscles excite or inhibit the micturition reflex? The external sphincter?
excites the reflex, inhibits the sphincter
(causes relaxation of sphincter = micturition)
Is control of the micturition reflex sympathetic or parasympathetic?
parasympathetic
True or false: The internal urethral sphincter is under voluntary control.
false
If the tubular filtrate becomes too acidic, which of the following is secreted by the tubular epithelial cells to buffer the secreted H+?
A. HCO3-
B. OH-
C. NH3
D. NH4+
E. basic phosphate
C
The kidney tubular cells secrete NH3...
A. when the urinary pH becomes too high
B. when the body is in a state of alkalosis
C. to buffer the acid phosphate excreted in the urine
D. when there is excess NH3 in the body fluid
E. to enable further renal secretion of H+
E