Lesson 64 - Skin regeneration and repair
1/115
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
116 Terms
What are the two main categories of wounds?
open and closed
What gives tissue its tensile strength?
collagen
What is an abrasion?
superficial wound typically caused by rubbing or scraping on a rough surface
What is a burn?
partial or full-thickness wound caused by heat or chemicals
What do burn degrees depend on?
depth of tissues affected
What is a contusion/bruise?
injury to the soft tissues below the skin caused by a blow or impact that damages small blood vessels and causes them to leak
What is a degloving injury?
type of avulsion injury specifically involving the skin
What is an avulsion?
tearing away or separation of a body part from its normal point of attachment that can affect skin, bone, soft tissues (tendon, ligament, muscle)
What is a laceration?
wound that is characterized by a jagged, irregular tear or cut in the skin (or other soft body tissue) typically caused by a shearing force
What is a puncture wound?
penetrating wound caused by a pointed object (ex. nail, knife, or tooth)
What is a surgical wound?
cut or opening in the skin created by a surgical instrument, typically a scalpel, during a surgical procedure

burn

degloving

laceration
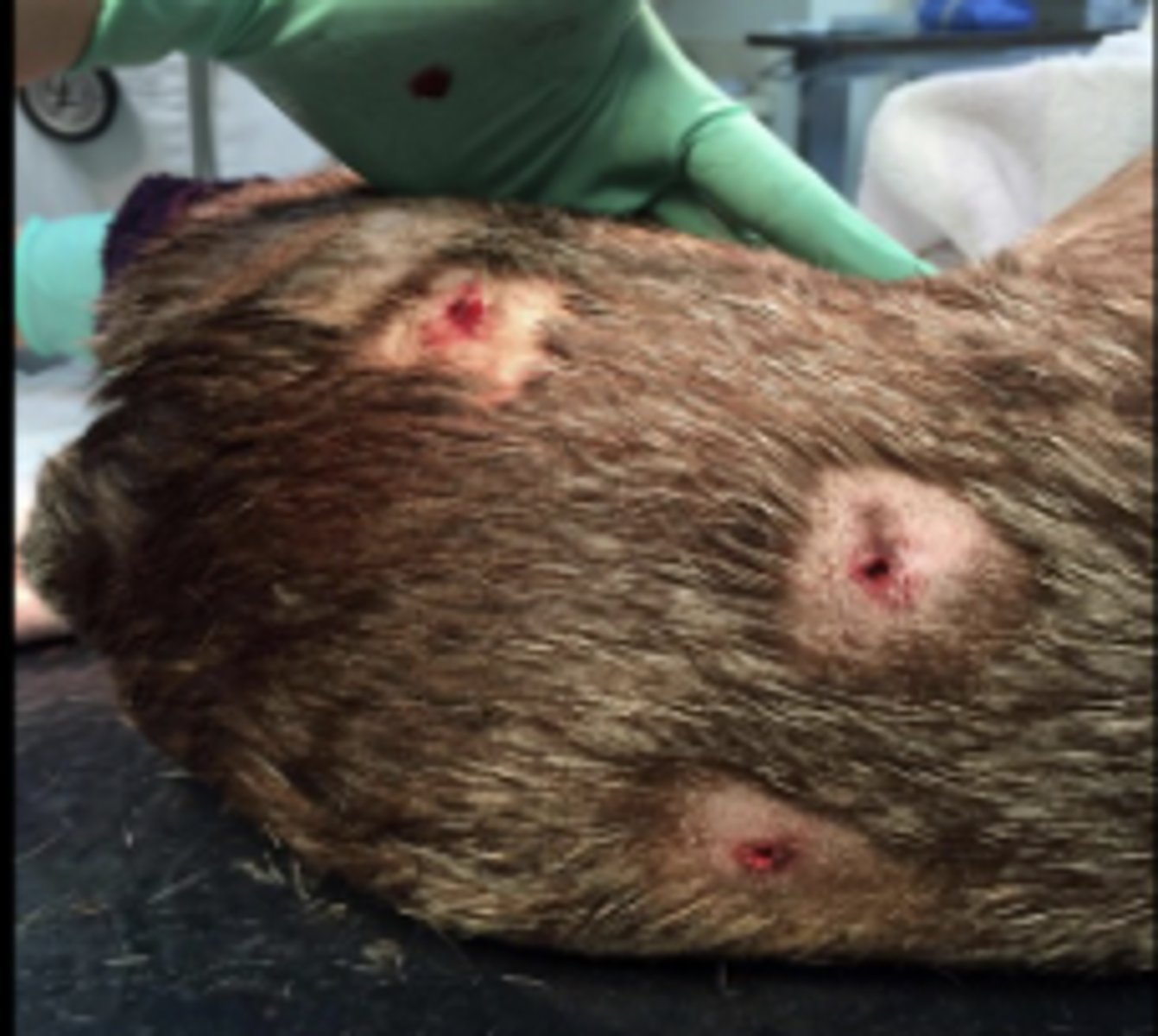
puncture

abrasion
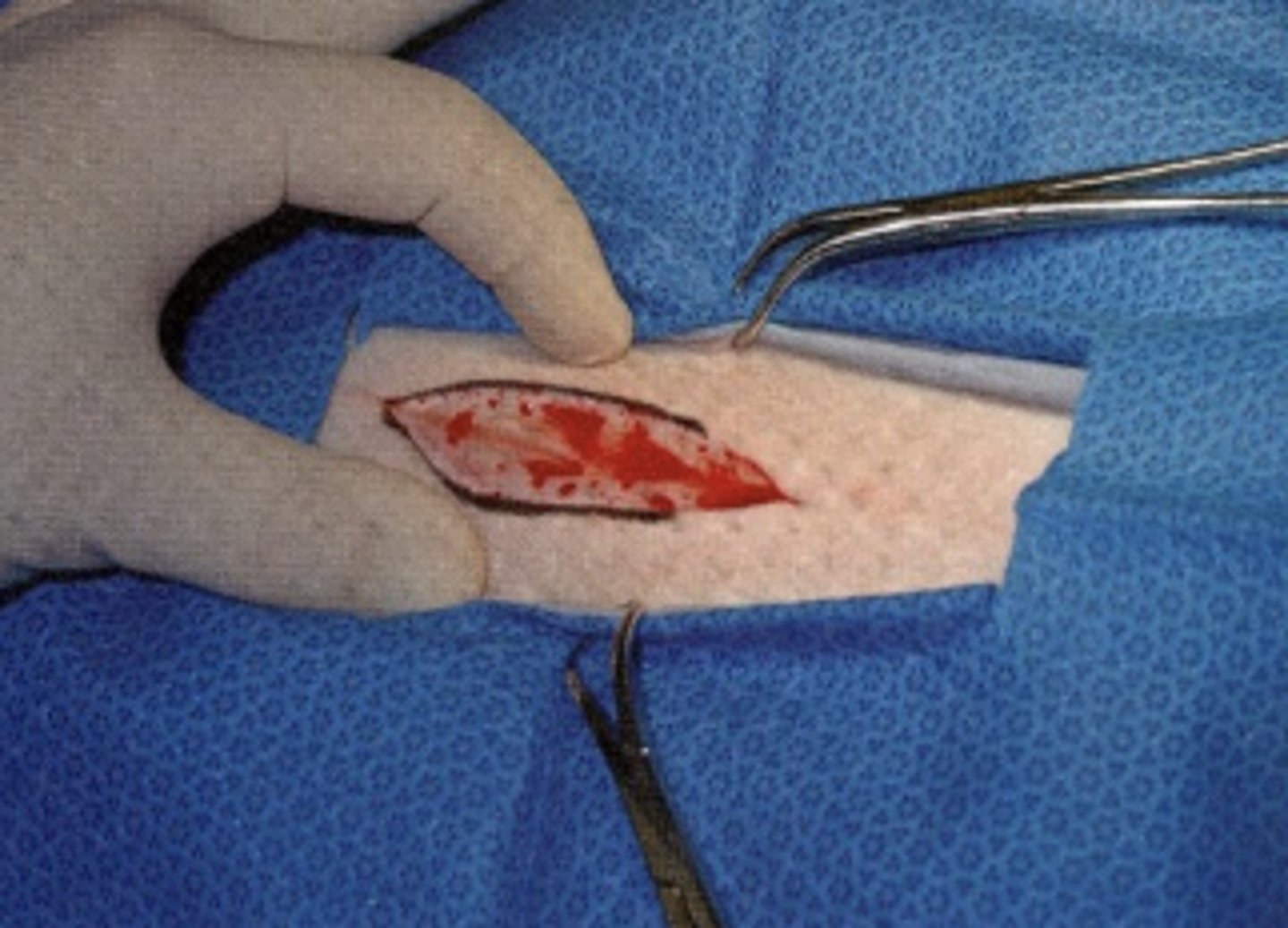
surgical
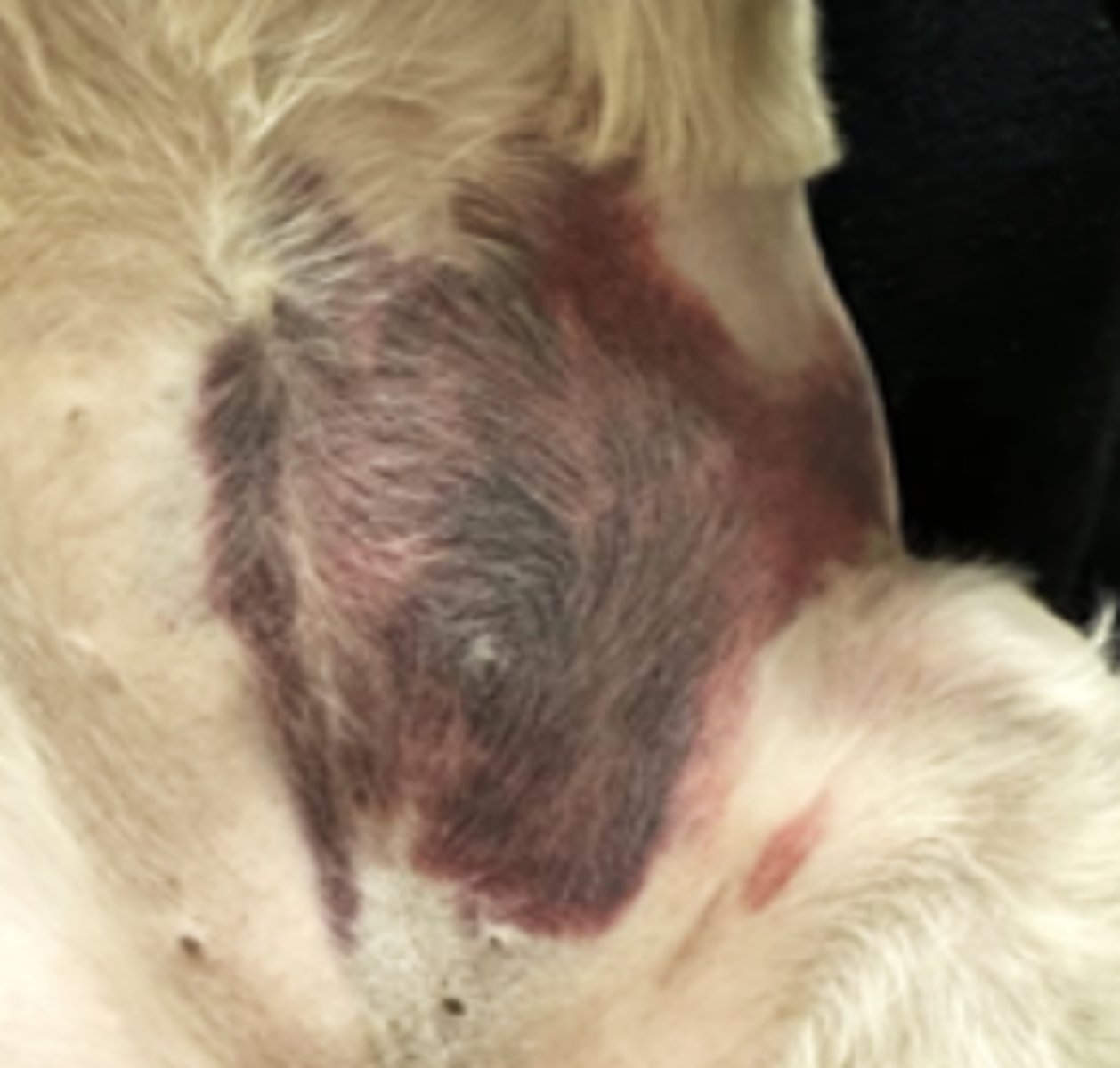
contusion
What is a wound?
disruption of anatomic and cellular continuity of tissue
What is wound healing?
dynamic, complex, and interactive process with the goal to restore the integrity of the tissue
What are the three phases of wound healing?
1. inflammatory
2. repair
3. remodeling
What is the goal of the inflammatory phase of wound healing?
minimize blood loss (coagulation) and prepare the wound site for repair by removing debris and contamination
Why is the inflammatory phase also called "lag" phase?
no significant increase in wound strength during this phase
What is the first process in wound healing?
coagulation
What happens during coagulation?
1. blood vessels constrict to control blood loss
2. vessels vasodilate to bring fibrinogen and other clotting elements into the wound
3. platelets activate when bound to exposed collagen at the wound site
3. clot is formed by sequestration of platelets within a fibrin clot
What is the timeframe for inflammation and debridement?
begins within minutes of injury and may continue for several days
What is the goal of inflammation and debridement?
prepares the wound site for repair through removal of bacterial contamination and debris
What cell predominates early inflammatory phase?
neutrophils
What cells arrive shortly after neutrophils in the inflammatory phase?
macrophages
Which two cells debride the wound site within 6 hours of injury?
neutrophils and macrophages
How long after the initial injury do macrophages replace neutrophils as the predominant cell type?
24-48 hours
What cells regulate the healing process?
macrophages
What are the predominant cells of the inflammatory phase?
1. platelets
2. neutrophils
3. macrophages
4. mast cells
What is the role of platelets in the inflammatory phase?
release cytokines and growth factors essential in wound healing
What is the role of neutrophils in the inflammatory phase?
decontamination and releasing cytokines that attract inflammatory cells to the wound site and activate keratinocytes, fibroblasts, and endothelial cells
What is the role of macrophages in the inflammatory phase?
1. regulate the healing process
2. decontamination
3. release growth factors that recruit and activate fibroblasts
4. coordinate the formation of the extracellular matrix
What is the role of mast cells in the inflammatory phase?
1. triggers inflammatory response via degranulation
2. play a role in vasodilation
What is the end result of the inflammatory phase?
provisional extracellular matrix (ECM) has been laid down at the wound site
What is the provisional extracellular matrix (ECM) at the wound site a precursor for?
granulation tissue
What does the ECM provide the wounded tissue?
form, structure, strength, and allows for cell adhesion and migration during the wound healing process
What is the goal of the repair phase?
formation of granulation tissue at the wound site and restore the integrity and increase strength of wounded tissue
What gives granulation tissue its red color?
vascularization
What is another name for the repair phase?
proliferative phase
What happens during repair phase?
1. dermis is rebuilt
2. collagen is deposited (=strength)
3. basement membrane is reformed
What are the simultaneous processes of the repair phase?
1. fibroplasia
2. angiogenesis (neovascularization)
3. epithelialization
4. wound contraction
What is angiogenesis?
formation of new blood vessels from pre-existing vessels
What is fibroplasia?
process of forming fibrous tissue
What is epitheliazation?
migration followed by proliferation of epithelial cells to cover a denuded (raw or exposed) epithelial surface
What is wound contraction?
natural process where the edges of a wound move inward, reducing the size of the wound
What happens to the fibrin clot and provisional extracellular matrix during repair phase?
replaced by granulation tissue
What are the characteristics of the granulation tissue created during repair phase?
grows from the base of the wound and is ever-evolving during the wound healing process
What are the components of granulation tissue?
1. fibroblasts
2. collagen
3. blood vessels
4. fibrous connective tissue
What is the goal of fibroplasia?
Formation of granulation tissue and re-collagenation
What are the steps of fibroplasia?
1. migration of fibroblasts into the wound
2. proliferation of fibroblasts
3. synthesis of the components of true extracellular matrix
What are the components of true ECM?
collagen, elastin, proteoglycans
How long does fibroplasia last?
2-4 weeks (depending on wound type & severity)
What is the goal of angiogenesis?
ensure adequate blood supply to wounded site
When does angiogenesis begin?
~2 days after injury
Why is adequate blood supply essential to wound healing?
brings nutrients and essential cells to the wound site
What are the steps of wound contraction?
1. fibroblasts within the granulation tissue differentiate into myofibroblasts
2. myofibroblasts have actin-containing microfilaments and contract to pull the wound margins together
3. reduction in wound size ~0.6-0.8mm per day
What is the timeframe of wound contraction?
may begin early in wound healing and peak within days or weeks
What can cause wound contraction to cease prematurely?
if tension of surrounding skin exceeds the force of contraction
What is involved in myofibroblast differentiation?
1. In response to TGF-β & mechanical tension, fibroblasts begin to differentiate
2. Cytoplasmic actin rearranges to form actin containing stress fibers terminating at focal adhesion sites
3. Focal adhesion sites enlarge & stress fibers become α-smooth muscle actin
4. The α-smooth muscle produces a contractile force, closing the wound
What is the goal of epithelialization?
restore the skin's epithelial layer
What is involved in epithelialization?
1. keratinocytes mobilize from the wound margin and migrate towards the center of wound
2. cell-to-cell contact at the center of the wound signals that the wound has epithelialized, and the process is halted (contact inhibition)
3. migrating epithelial cells (below the scab) secrete collagenase which serves to dissolve base of scab facilitating its removal
When does epithelialization occur faster?
in a moist wound environment
How long does epithelialization take for surgical wounds?
24-48 hours
What are the predominant cells of the repair phase?
1. fibroblasts
2. myofibroblasts
3. keratinocytes
4. endothelial cells
What is the goal of fibroblasts in the repair phase?
production of granulation tissue (collagen deposition)
What is the goal of myofibroblasts in the repair phase?
wound contraction
What is the goal of keratinocytes in the repair phase?
epithelialization
What is the goal of endothelial cells in the repair phase?
angiogenesis
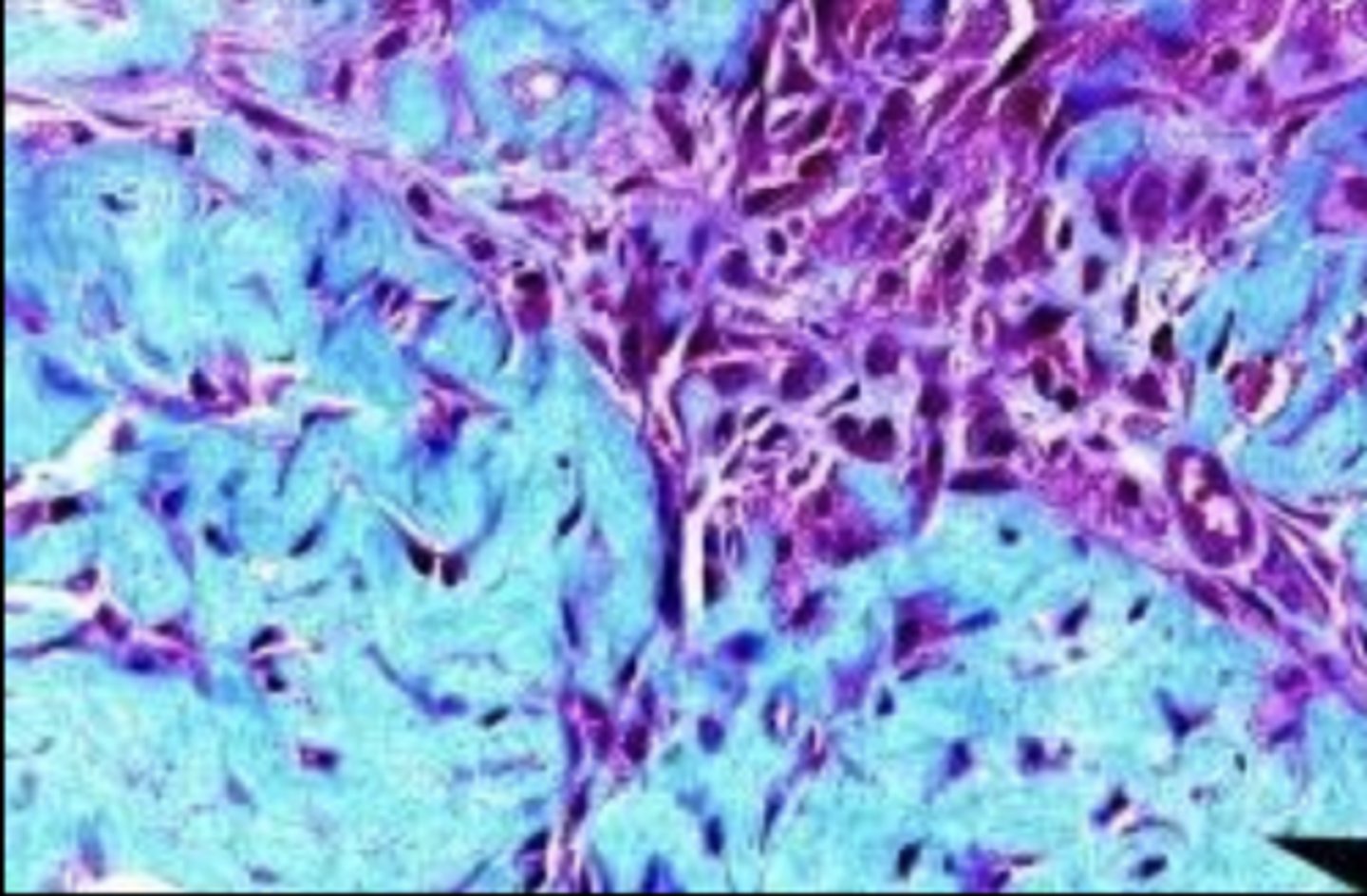
newly formed granulation tissue
mature granulation tissue
What happens during remodeling phase?
epithelialized granulation tissue transitions to a scar
Why does the cellularity of tissue decrease during remodeling?
apoptosis
Why is scar tissue pale?
apoptosis of capillaries
Why does the tensile strength of tissue increase during remodeling?
1. change of immature type III collagen to mature type I collagen
2. realignment of collagen fibers along the lines of tension
3. increased cross-linking of collagen fibers
When does remodeling phase occur?
~3 weeks post-injury and can continue for months or years
How much strength does most tissue regain after remodeling?
80% (except bone and bladder)
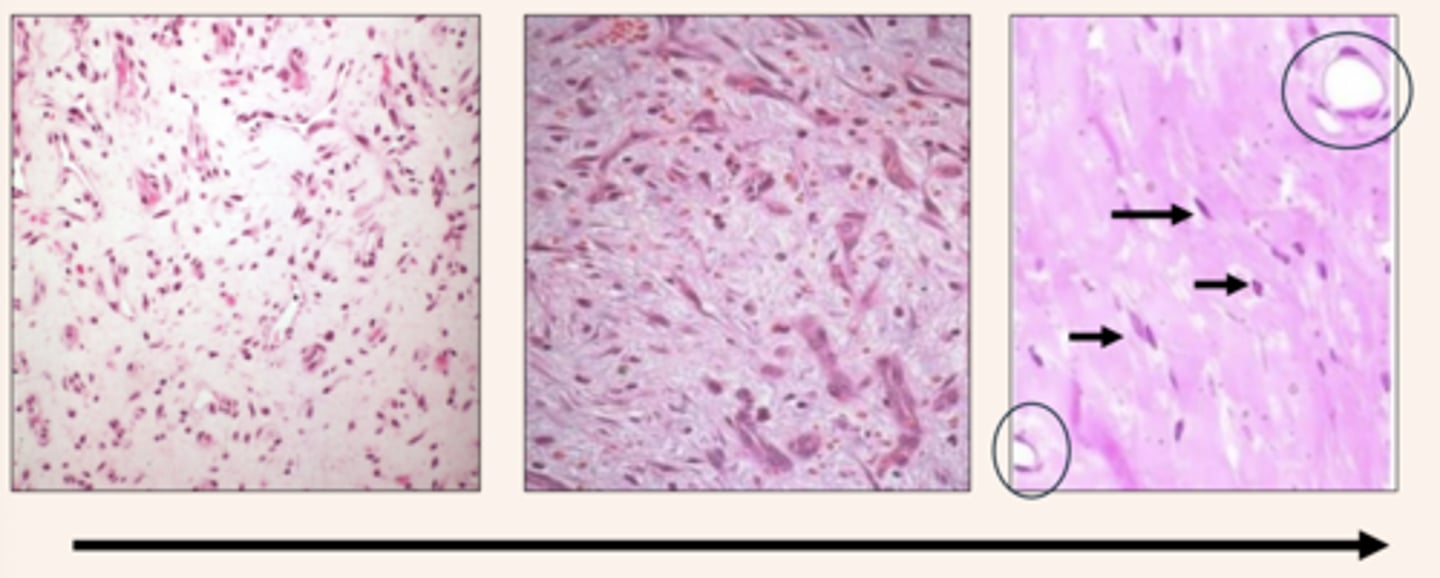
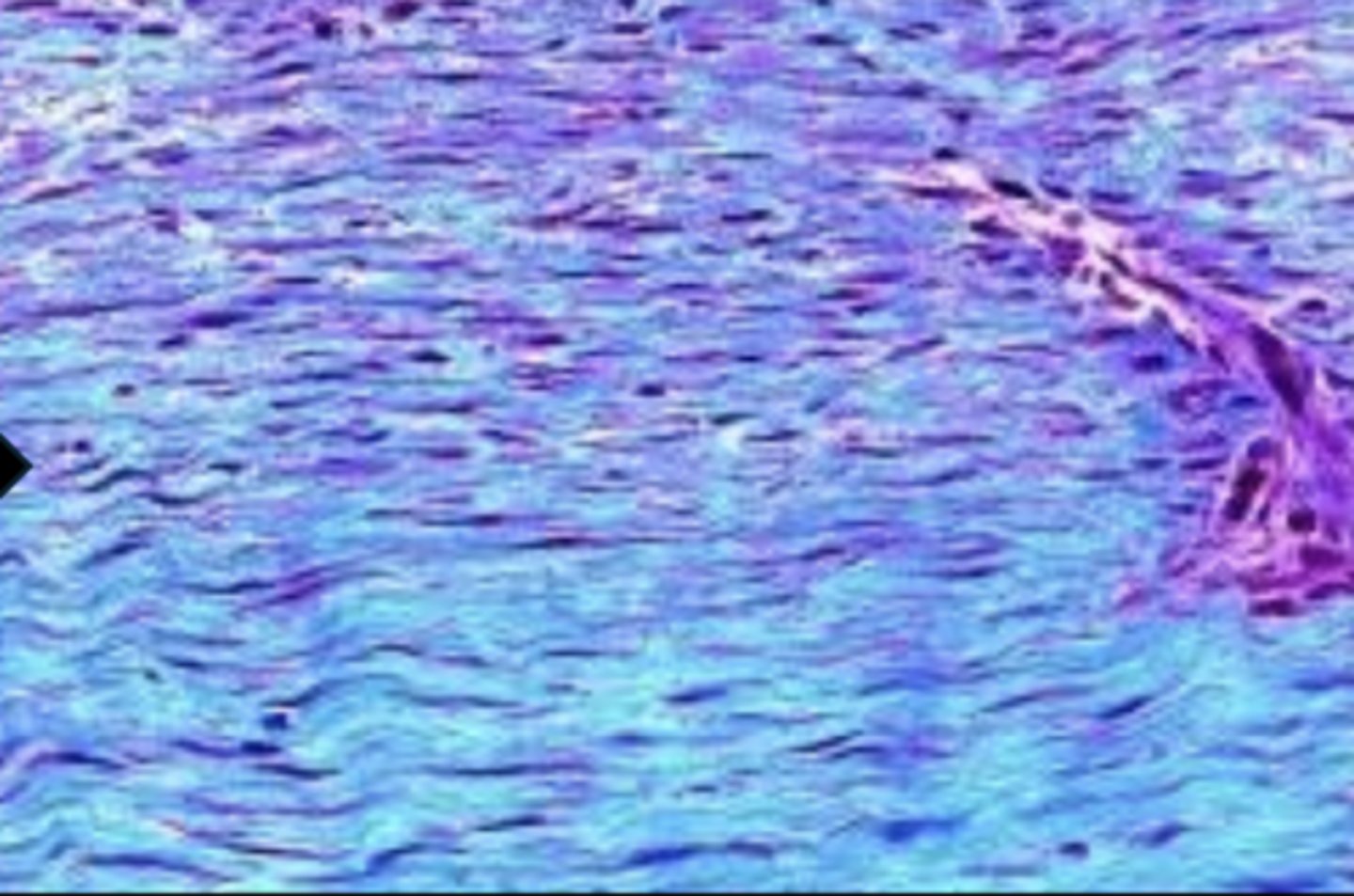
granulation tissue maturing into fibrous connective tissue
What does an increased density of collagen cause?
apoptosis of majority of blood vessels and fibroblasts (decreased vascular and cellular presence) and tissue contraction (myofibroblasts)
What is the predominant cell of the remodeling phase?
fibroblast
What is the goal of fibroblasts during remodeling?
deposition of type 1 (mature) collagen
What are some complications in wound healing?
1. exuberant granulation tissue
2. wound contracture
3. hypertrophic scarring
What is exuberant granulation tissue ("proud flesh")?
complication in wound healing that occurs when healing process is delayed
What can delay wound healing?
1. movement
2. infection
3. foreign body
4. poor blood supply
5. malnutrition
What species has a slower rate of wound repair including prolonged inflammatory phase relative to other animals?
horses
How do you treat exuberant granulation tissue ("proud flesh")?
need to address the underlying cause of delayed wound healing and then debulk with sharp dissection
What is wound contracture?
type of abnormal healing of the tissue that results in a functional impairment, typically around joints
When can wound contracture occur?
with wounds over the flexion surface of a joint
When will wound contracture impair a joint's ability to extend?
if collagen fibers bond while joint is flexed
What is hypertrophic scarring?
overproduction of collagen during the healing process resulting in thickened, raised scars that extend beyond the boundaries of the original wound
Where is hypertrophic scarring seen?
areas with minimal subcutaneous fat, such as the chest, ears, elbows, knees and shoulders
How common is hypertrophic scarring?
uncommon in animals
What is clinically significant about the use of topical therapies for wound healing?
can be helpful or impair wound healing if used during certain phases of wound healing
What are some topical therapies for wound healing?
1. aloe vera
2. preparation H
3. solcoseryl
4. honey
5. triple antibiotic
6. silver sulfadiazine
7. nitrofurazone
How does aloe vera aid wound healing?
1. antibacterial (efficacy against Pseudomonas)
2. promotes fibroblast replication
3. products containing Allantoin & acemannan (aloe plant derivatives)
How does preparation H aid wound healing?
promotes angiogenesis, epithelialization & collagen synthesis
How does solcoseryl aid wound healing?
1. stimulates fibroblast proliferation & migration
2. protein-free calf blood ultrafiltrate (expensive)