RR- airway/histology/oxygen
1/96
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
97 Terms
what are the 5 roles of the airways and airspaces
move O2 in
move CO2 out
warm and humidify air
facilitate gas exchange
defense against unwanted intrusion
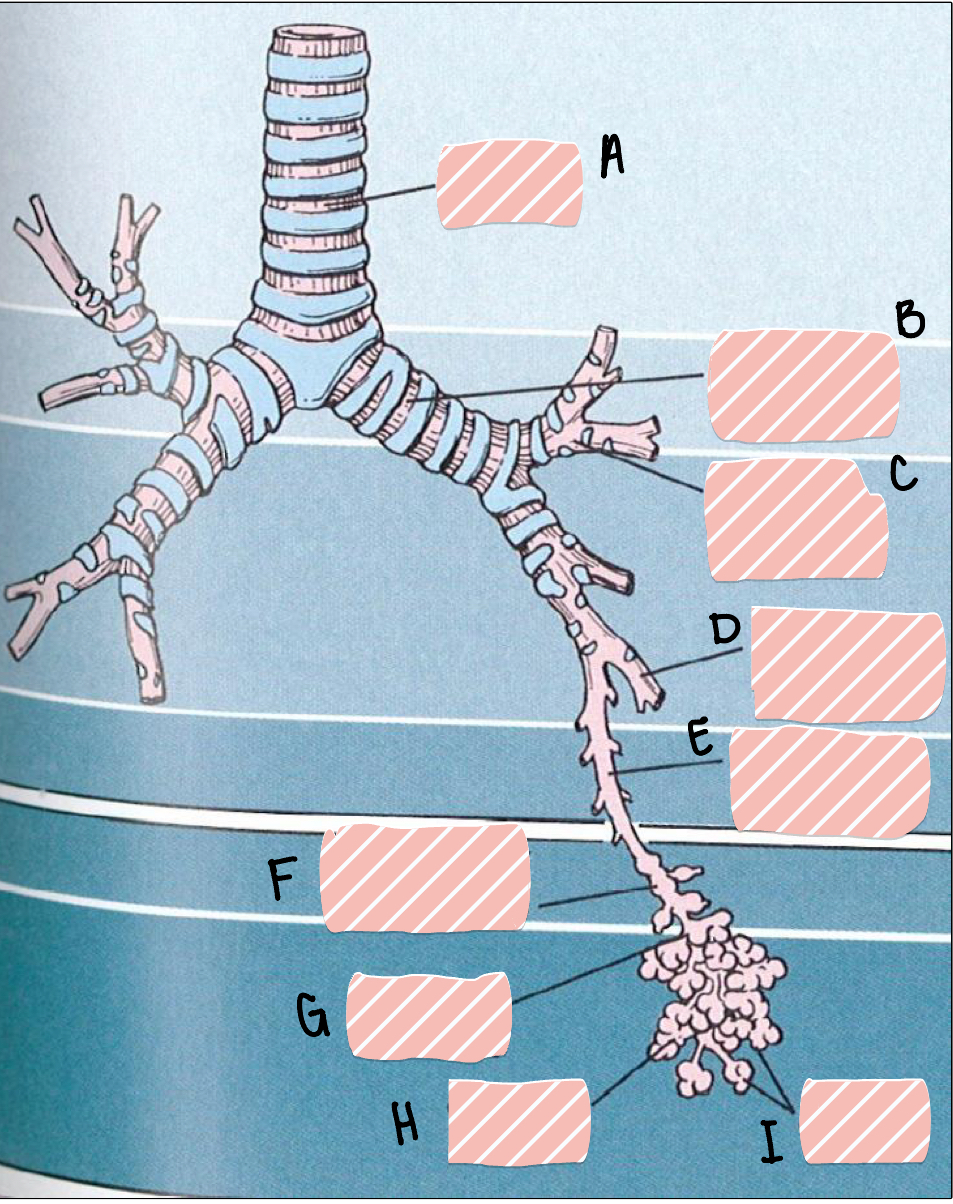
A
trachea
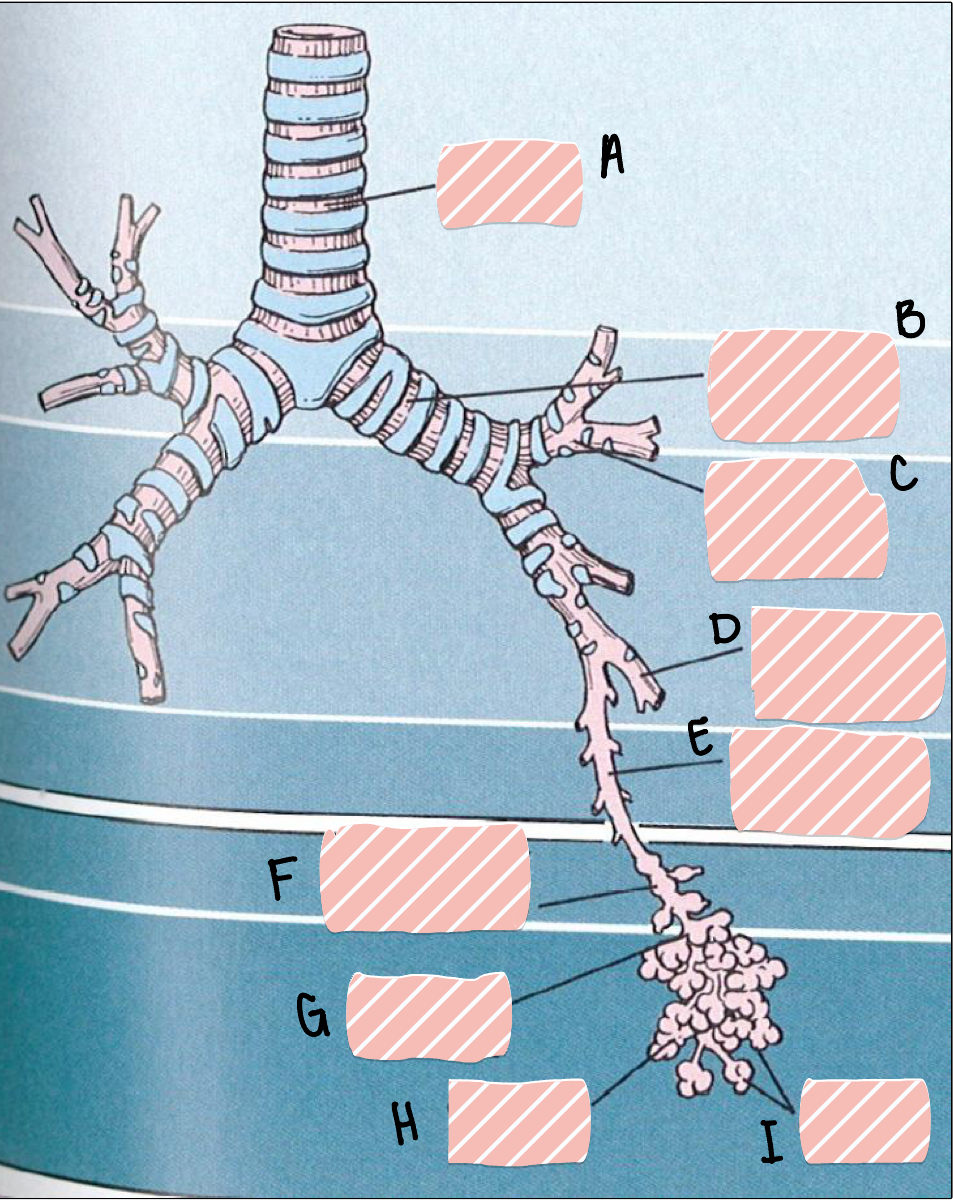
B
main bronchus
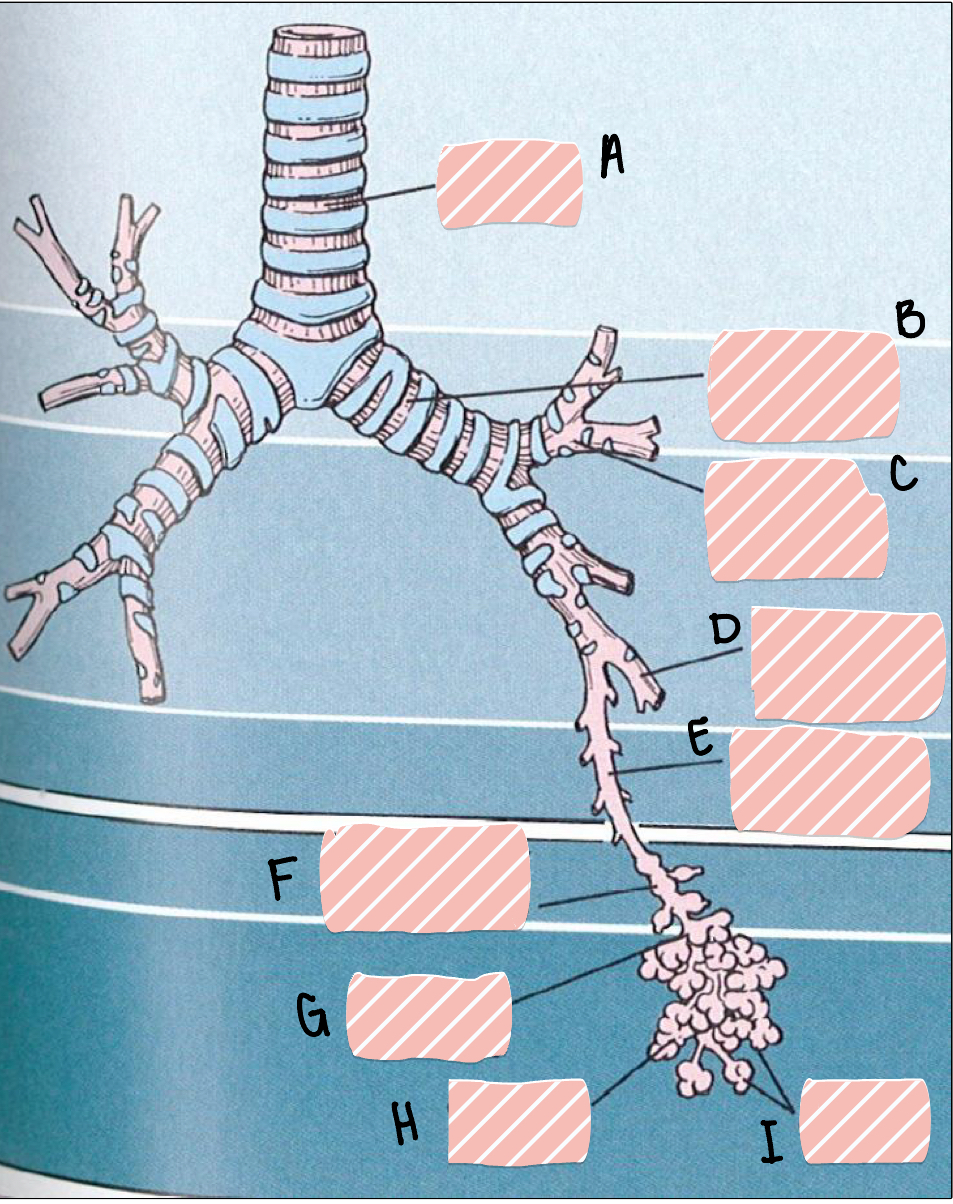
C
lobar bronchus
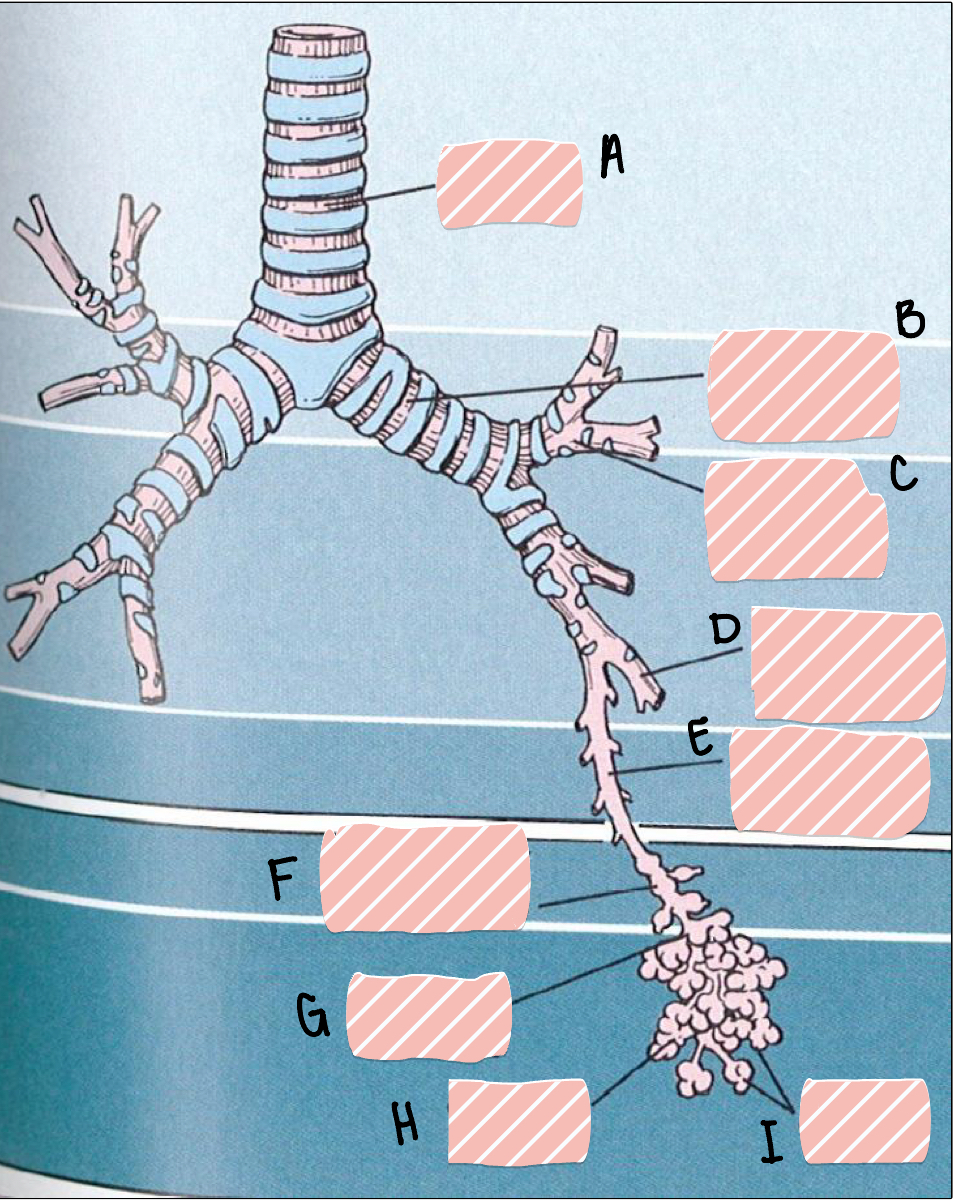
D
segmental bronchus
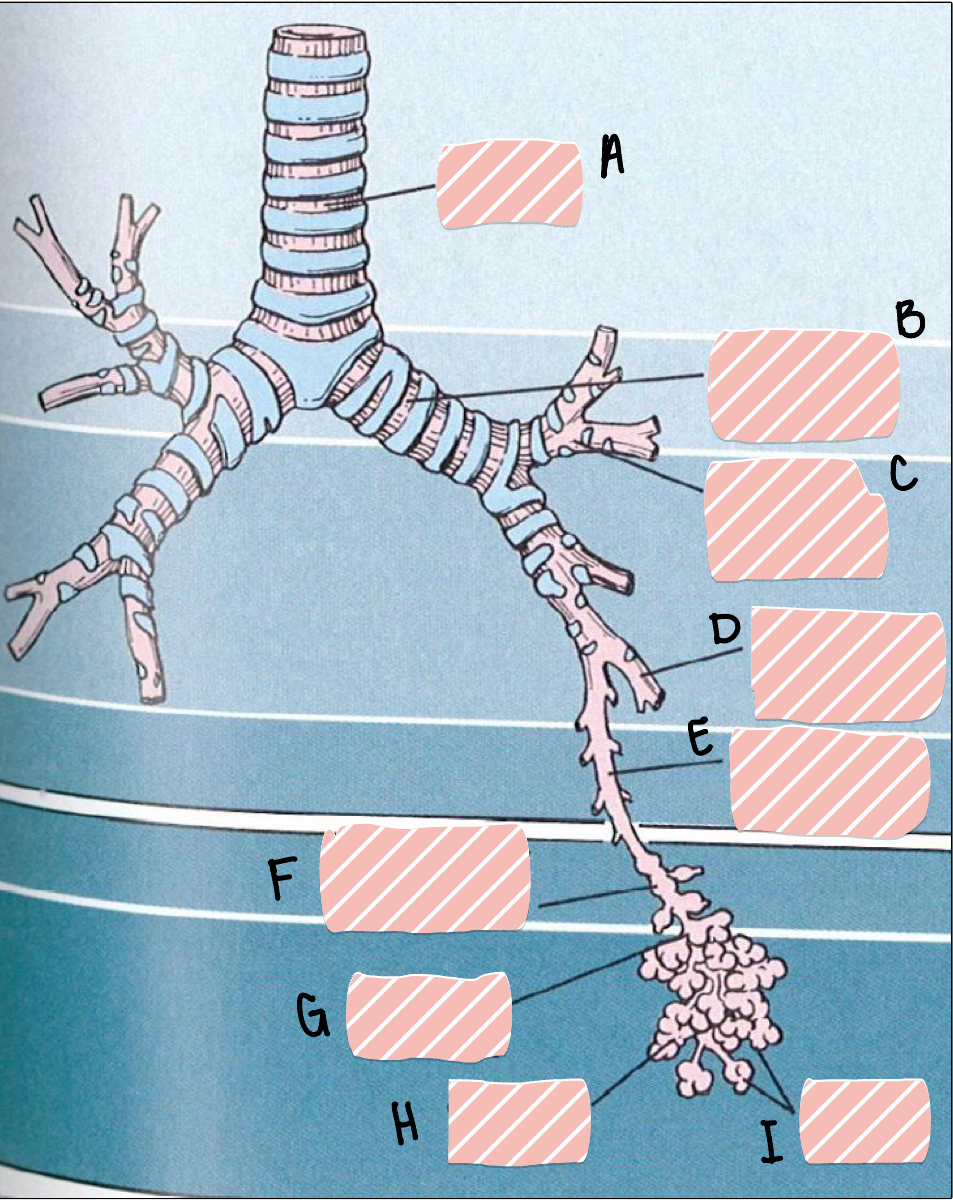
E
terminal bronchus
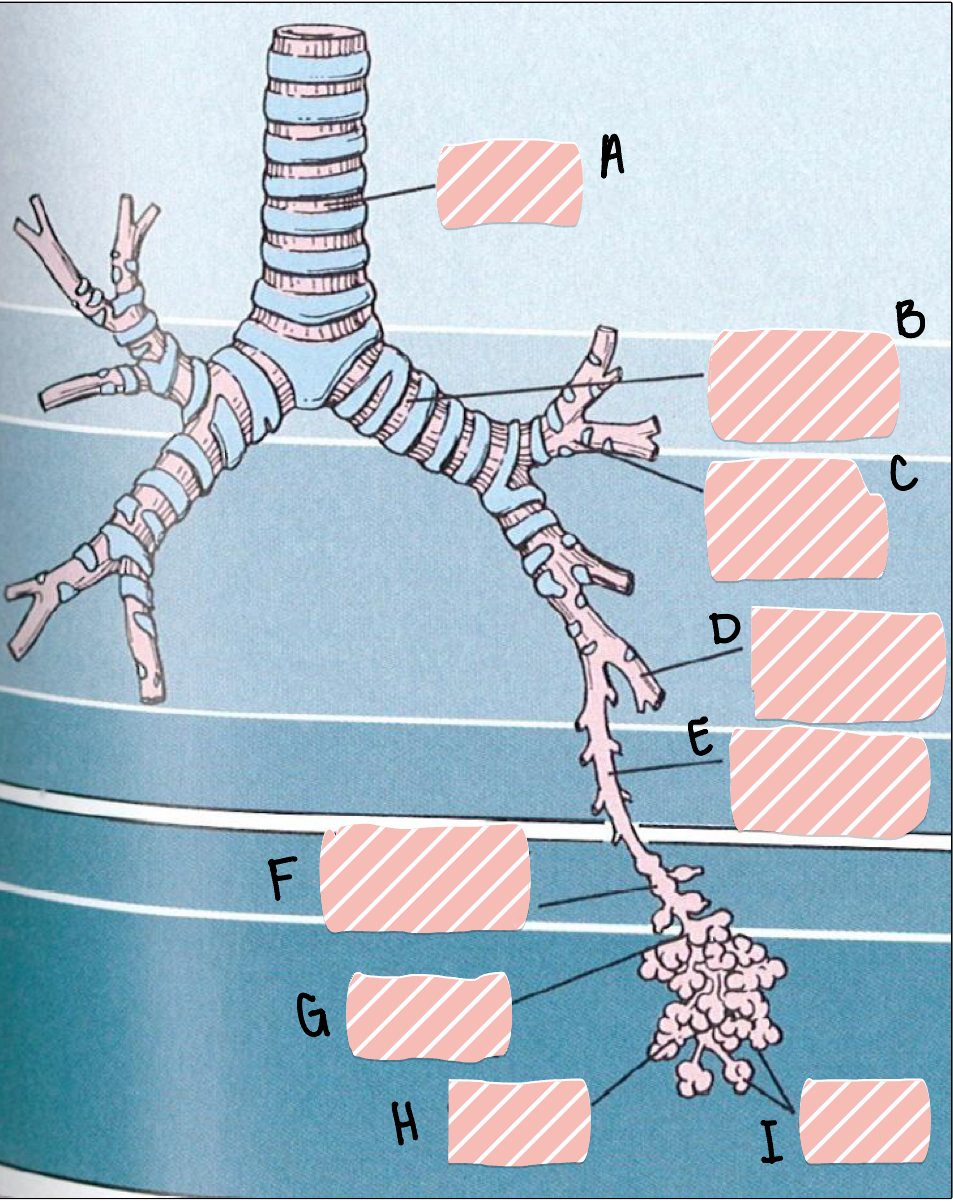
F
respiratory bronchioles
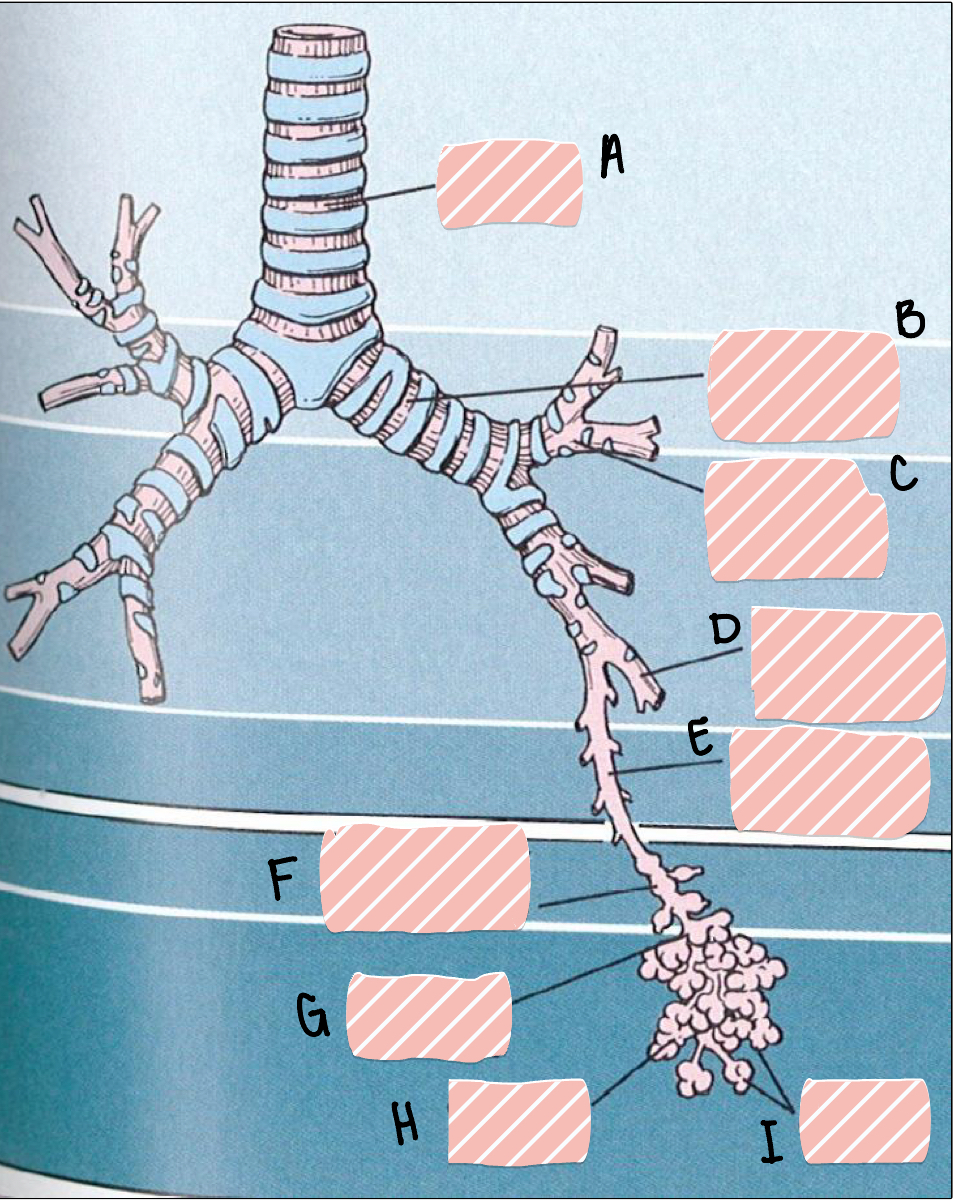
G
alveolar duct
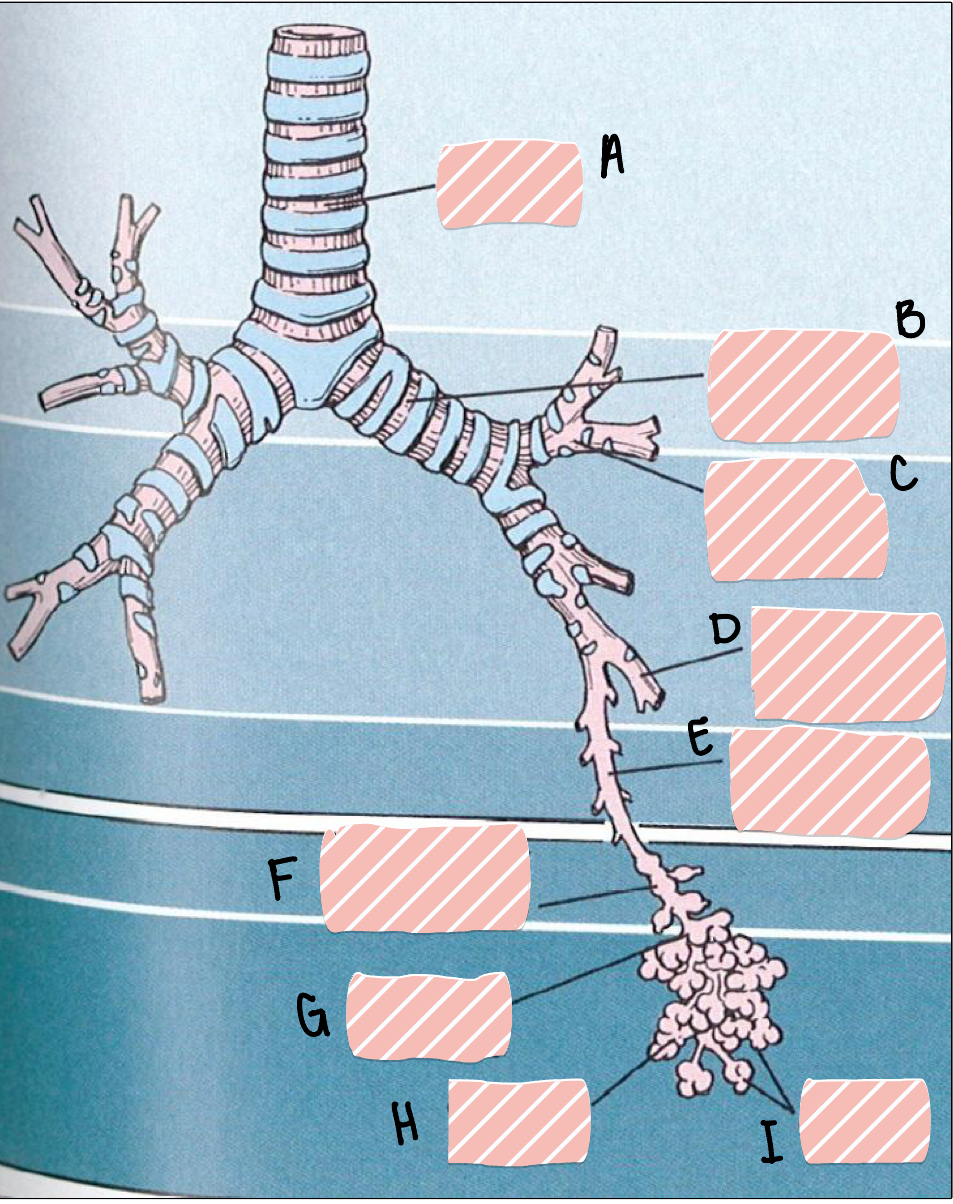
H
alveolar sacs
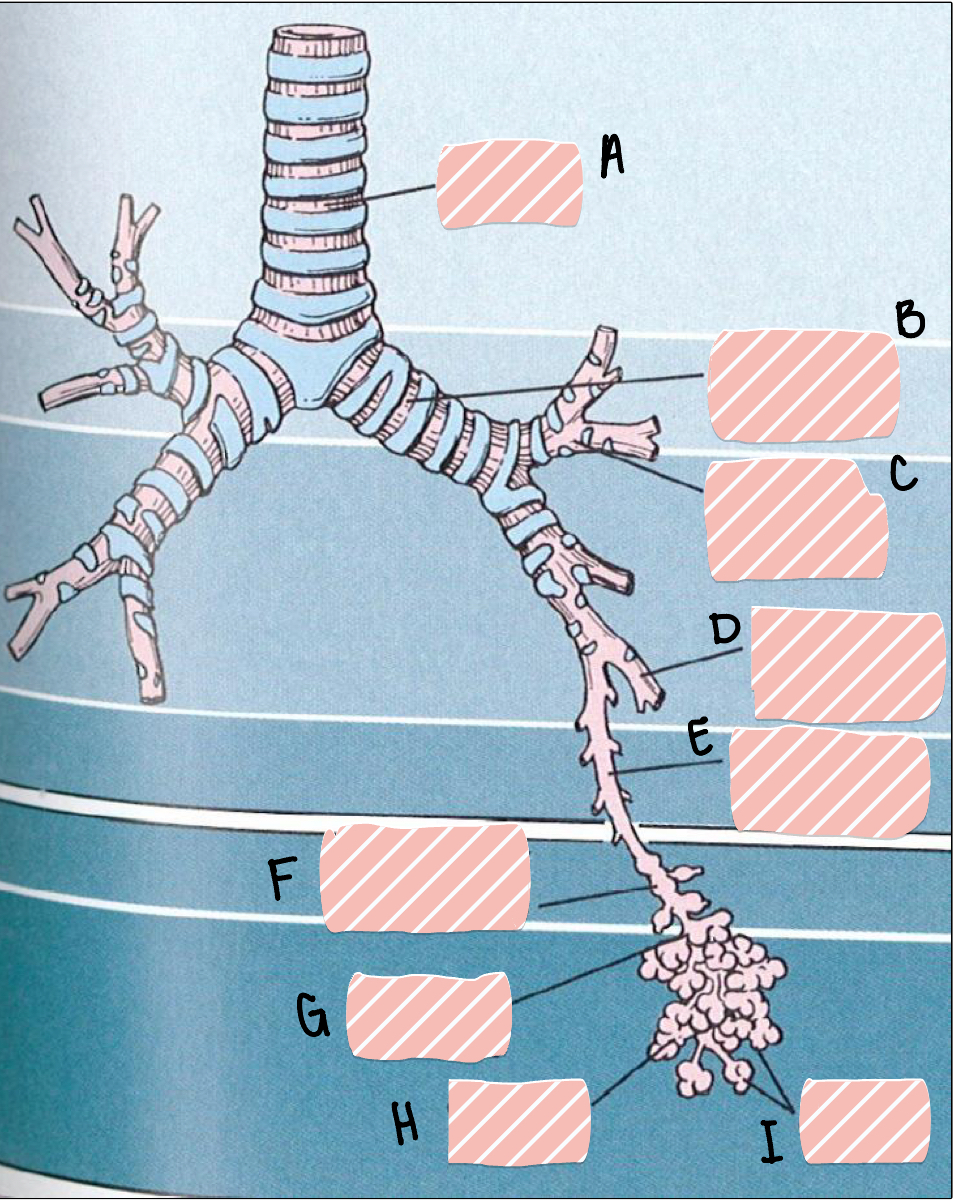
I
alveoli
if a pt were to aspirate something from the mouth into their lungs, what area would it likely lodge in the lungs, why
in the R lung in the middle or lower lobe- where the bronchus has the longest and straightest pathway to the lungs
describe the action of the larynx and epiglottis to protect the trachea when swallowing
larynx rises towards the epiglottis closing off the opening to the trachea
Does total resistance in the airways increase or decrease as the airways become smaller toward the end of the air pathway? Why is this?
As you move distally in the airway tree, the diameter of any single airway becomes smaller so resistance of any given airway increases. However, there is such a large increase in the total number of airways that the overall cross-sectional area for airflow is very high in the distal airways and the overall airways resistance is quite low in this region.
what is the major mechanism to protect the respiratory tract from invaders
mucociliary escalator
how can mucociliary escalator be damaged in infection
during post-influenza infections, the epithelium can be denuded and have no ciliary to move the invaders out
what is the main difference between the conducting zone and the respiratory zone
there is no gas exchange in the conducting zone
what structures are included in the conducting zone
trachea → bronchi → terminal bronchioles
what structures are included in the respiratory zone
respiratory bronchioles → alveolar ducts → alveolar sacs → alveoli
__________ is the key structural element of the distal airways
smooth muscles
how does smooth muscle control flow
contraction and relaxation regulates the distribution of air flow to help match ventilation w perfusion
why is it really important that capillary/alveoli barrier is very thin
allows easy diffusion for O2 in one direct and CO2 in the other direction
capillaries form a continuous sheet of blood in the wall of the alveolus that greatly _________ (inc/dec) the surface area
inc
there is a significant risk in the capillaries/alveoli barrier being so thin, what is this
susceptible to leakage and injury w inc intraluminal pressure
what pneumocyte coats most of the alveolar surface
type 1
which pneumocyte makes surfactant, can repopulate after injury/resistant to injury
type 2
what is the function of the conducting zone
conduct, filter, warm and moisten inhaled air
what is the conducting composed of
nose, pharynx, larynx, trachea, bronchi, terminal bronchioles
the conducting zone is lined by…
respiratory mucosa composed of ciliated columnar epithelium and submucosal seromucous glands
the respiratory zone participates in…
gas exchange
what is the respiratory zone composed of
respiratory bronchioles, alveolar ducts, alveolar sacs, and alveoli
what is the respiratory zone lined by
alveolar epithelium composed of type 1 and 2 pneumocytes- thin squamous epithelium
how many cartilage rings are there in the trachea, what are they shaped as
16-20 “c”-shaped rings
what is the function of the cartilage rings in the trachea
mechanical stability
the main bronchi have ____________________ and smaller bronchi have ______________
cartilage rings; irregular plates of cartilage
what is the branching order starting from bronchi
bronchi → lobar bronchi → segmental bronchi → terminal bronchioles → respiratory bronchioles
what structures consists of the following characteristics:
intralobular air tubes, 1-5 mm diameter, formed after ~10 generations of branching
bronchioles
describe the epithelium of large bronchioles
ciliated pseudo-stratified columnar
describe the epithelium in smaller terminal bronchioles
simple columnar becoming cuboidal
there are few _________ cells in bronchioles and entirely gone by the smallest bronchioles
goblet
_________ and __________ are abundant in bronchioles
elastin and smooth muscle
what is present in bronchi but not in bronchioles
cartilage and submucosal glands are present in bronchi but not bronchioles
what do pulmonary arteries carry
deoxygenated blood from the RV to the alveolar bed
pulmonary arteries travel alongside…
bronchial/bronchiolar tree
what do pulmonary veins carry
oxygenated blood from alveolar bed to LA
pulmonary veins are not associated w…
bronchial/bronchiolar tree
do pulmonary arteries or pulmonary veins have a thick wall
pulmonary arteries; contains elastic lamina
what is the role of smooth muscle in the respiratory tract
contracts/relaxes to narrow/dilate air tubes; regulates
the respiratory tract is under ____________ innervation
autonomic
_________ NS will dilate while the ___________ NS will constrict
sympathetic; parasympathetic
where is mucociliary apparatus located
ciliated epithelium lines the trachea and the bronchi all the way down to the smaller bronchioles
what is the function of the mucociliary escalator
constantly beats to move mucus and debris upward along the bronchial tree and trachea- most of this content is unconsciously swallowed
what structure marks the end of the conducting part of the pulmonary tree
terminal bronchiole
type 1 pneumocytes are _________ cells and cover ________% of alveolar surface area
squamous; 95
type 1 pneumocytes are thin for _________ and are part of the __________ barrier
diffusion; blood-air
type 2 pneumocytes are _______ cells and cover ___% of the alveolar surface area
cuboidal; 5
function of surfactant
acts a detergent and reduces surface tension to prevent airspace collapse
what are the three ways we measure the “amount of oxygen” and what are the units
gas tensions in ambient air and oxygen tensions in inspired air and alveolar air; all measured in mmHg
FiO2 (inspired fraction of O2) doesn’t change as long as the person is in the earth’s atmosphere, but the ambient PO2 does change, depending on where the patient is. Why?
scenario 1: in my house chilling, I am breathing normal 21% O2, feeling good, PO2 would be high
scenario 2: I am on everest- high elevation, there is not a lot of oxygen there, but there is still 21% technically, but still not enough, and my body is requiring more oxygen, this would mean my PO2 would be low
what is F1O2
inspired fraction of O2, always 21%;
what is P1O2
partial pressure of inspired O2
what is PAO2
alveolar partial pressure of O2
what is PaO2
arterial partial pressure of O2
explain PAO2
it is the partial pressure of O2 being delivered to the alveoli; influx of O2 from the air
influx of O2 into the alveoli is a funx of…
the ventilation (VA)
the inspired partial pressure of O2 (P1O2)
what is SaO2
O2 saturation % of arterial Hb; this does not give us information about how much Hb is available to carry the O2
what is the alveolar gas equation
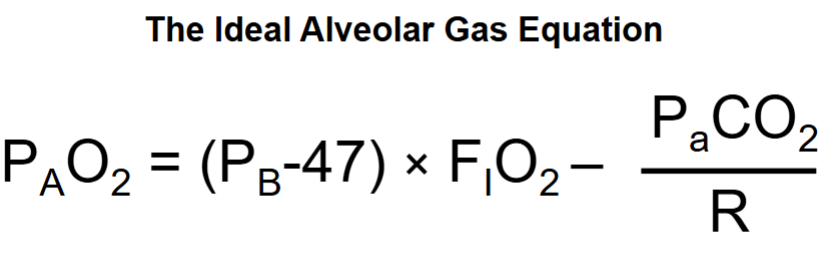
in words what is the alveolar gas equation
alveolar pressure of O2 = oxygen coming into the alveolus - oxygen going out of the alveolus going into the blood
in the case of a pts hypoxic event, how can we figure out the appropriate tx using the alveolar gas equation
compare PAO2 to PaO2
what does (PATM - PH2O) x FiO2 represent
how much O2 is brought into the alveolus (oxygen in); also can be represented as PiO2
what does (PaCO2)/R represent
how much oxygen is taken away from the alveolus (oxygen out) into the blood
what does R represent
respiratory exchange rate; the ratio of the amount of oxygen intake to the CO2 out-take; is ~0.8
at sea level, barometric pressure (PATM) is…
760 (this will change w altitude change)
what is saturated vapor pressure (PH2O) of water at body temperature
47
at sea level, PiO2 =
(PATM - PH2O) x FiO2 →→→ (760 - 47) x .21 = ~150
how does F1O2 change if altitude inc
it doesn’t… unless you go to all the way to space
how does P1O2 change if altitude inc
decreases- inc altitude would inc barometric pressure (PATM)
how does PAO2 change if altitude inc
will dec due to the dec in P1O2
how does PaO2 change if altitude inc
will dec bc PAO2 is dec
oxygen consumption in the body can be estimated by…
PCO2 / R
when going to an inc altitude, you resting heart rate can be elevated, explain this
this is your bodies response to acute decreases in PaO2 AKA acute hypoxia; your body is inc hr to inc CO to try to pump more O2 through the body by pumping blood faster through the body
can we measure PCO2 or PO2 more easily
PCO2
____________ diffuses quickly from blood into the alveoli and vise-versa so we can assume _______=___________
CO2; PACO2 = PaCO2
does CO2 or O2 diffuse faster
CO2
does diffusion of the oxygen from alveoli to the red cells in the blood happen quickly or slowly if a person is at rest and at sea level
quickly
give a scenario where the diffusion of the oxygen from alveoli to the red cells in the blood happens slowly
in an exercising individual; when the barrier is thickened; higher elevation
function of hemoglobin
transports oxygen in the blood
what is the oxygen-hemoglobin dissociation curve
plots how saturated the hemoglobin is in the presence of a given partial pressure o oxygen
pulse-oximetry measures ___________ of oxygen in the Hb but does NOT tell you about the _________ of oxygen
saturation; content (only tells you how well the Hb is carrying the O2 not how much Hb is there)
a person w anemia may show to have a normal oxygen saturation by pulse oximetry but have low Hb, what is rlly happening
it shows they have normal oxygen saturation bc the Hb that are present are saturated w O2, but this doesn’t tell us how many Hb are present
what is P50
describes the hemoglobin affinity for oxygen when 50% of hemoglobin binding sites are being used
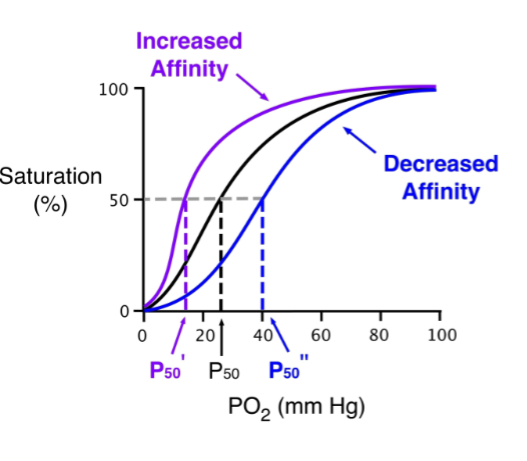
describe a right shift happening in the dissociation curve
right shift means there is an inc in P50 → decreased affinity for Hb holding onto O2 compared to normal
factors that can cause a right shift in the dissociation curve
dec pH
inc PCO2
higher temp
inc 2,3 DPG-diphosphoglycerate
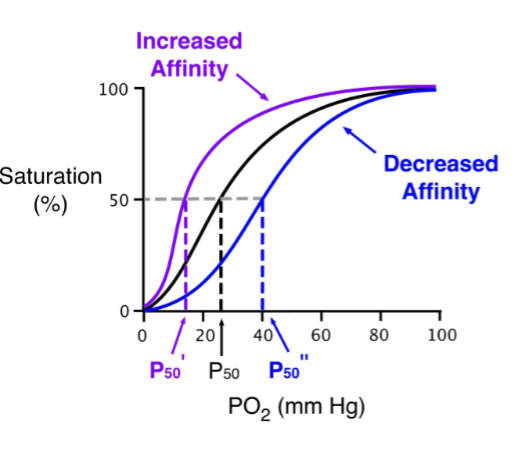
describe a left shift happening in the dissociation curve
left shift means there is a dec in P50 → inc affinity for Hb holding onto O2 compared to normal
factors that can cause a left shift in the dissociation curve
inc pH
dec PCO2
lower temp
think about the oxygen-Hb dissociation curve, in the lungs would be want a left or right shift
left shift- to get rid of CO2 and grab O2
think about the oxygen-Hb dissociation curve, in the tissues would be want a left or right shift
right shift- to get rid of O2 and grab CO2
is there more oxygen carried in hemoglobin or dissolved in the blood in the normal human
more dissolved in blood