Lecture 15, 16, 17: The Kidneys!
1/38
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
39 Terms
Describe the basics of the kidneys
The left kidney is higher than the right because the liver pushes down the right kidney
Adrenal glands and kidney have no communication with each other
Kidneys get 20% of your blood
Abdominal aorta → renal artery
Venous drainage
Renal vein (the renal artery is just behind the renal vein) → inferior vena cava
Urete goes to bladder and then through the urethra
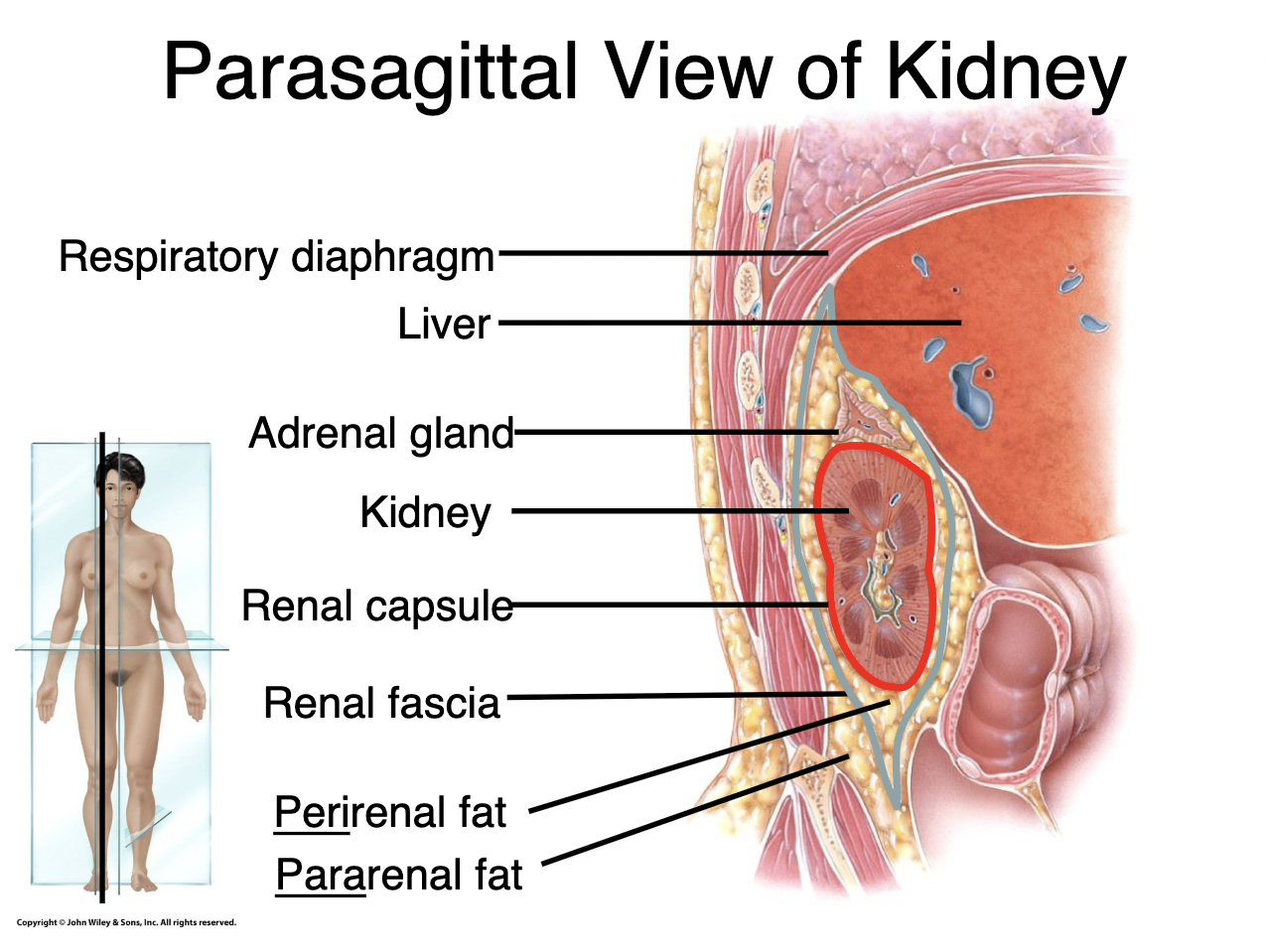
Describe the parasagittal view of the kidneys
Renal capsule → to hold in the pressure
Perirenal fat → to hold it up in place and together, also holds adrenal cortex
Renal fascia → also attaches to liver and respiratory
Pararenal fat
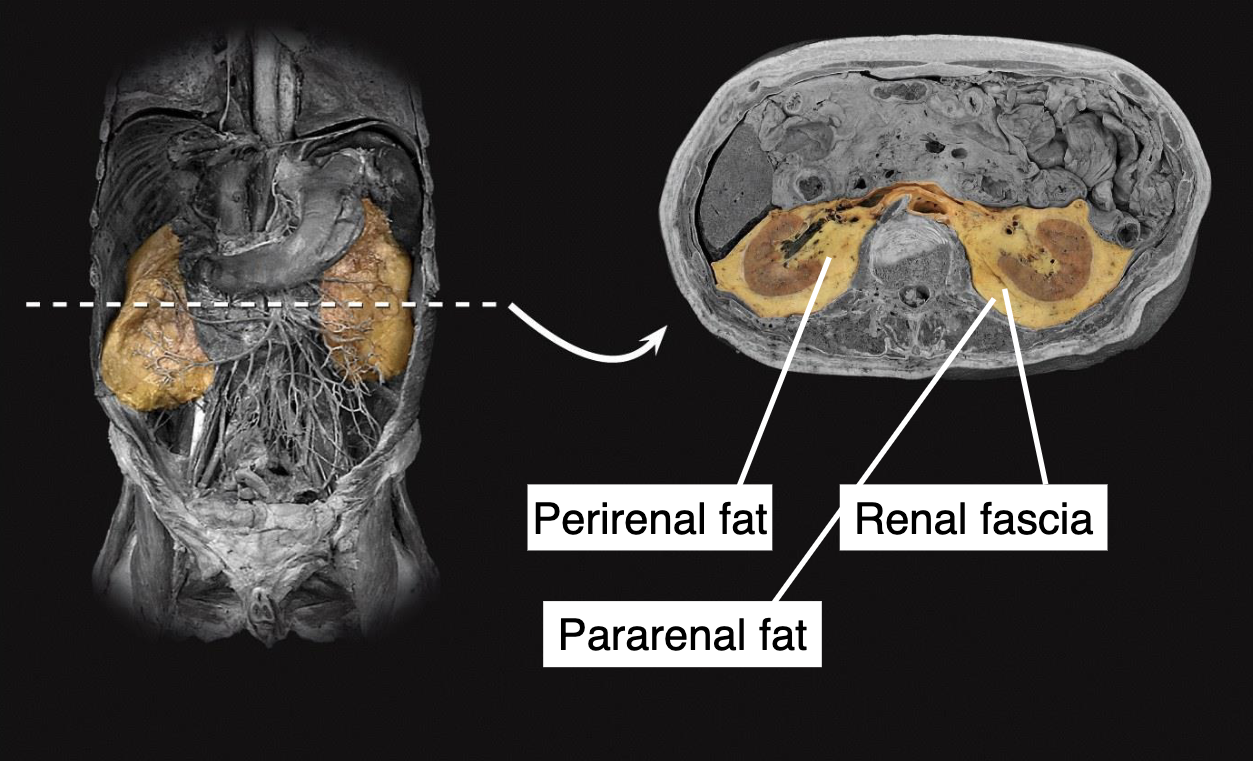
Describe the renal cross section
Renal fascia
Perirenal fat
Pararenal fat
You hold on to the fat, very hard to lose
Describe the renal hilum
Renal artery
Renal vein
Ureter
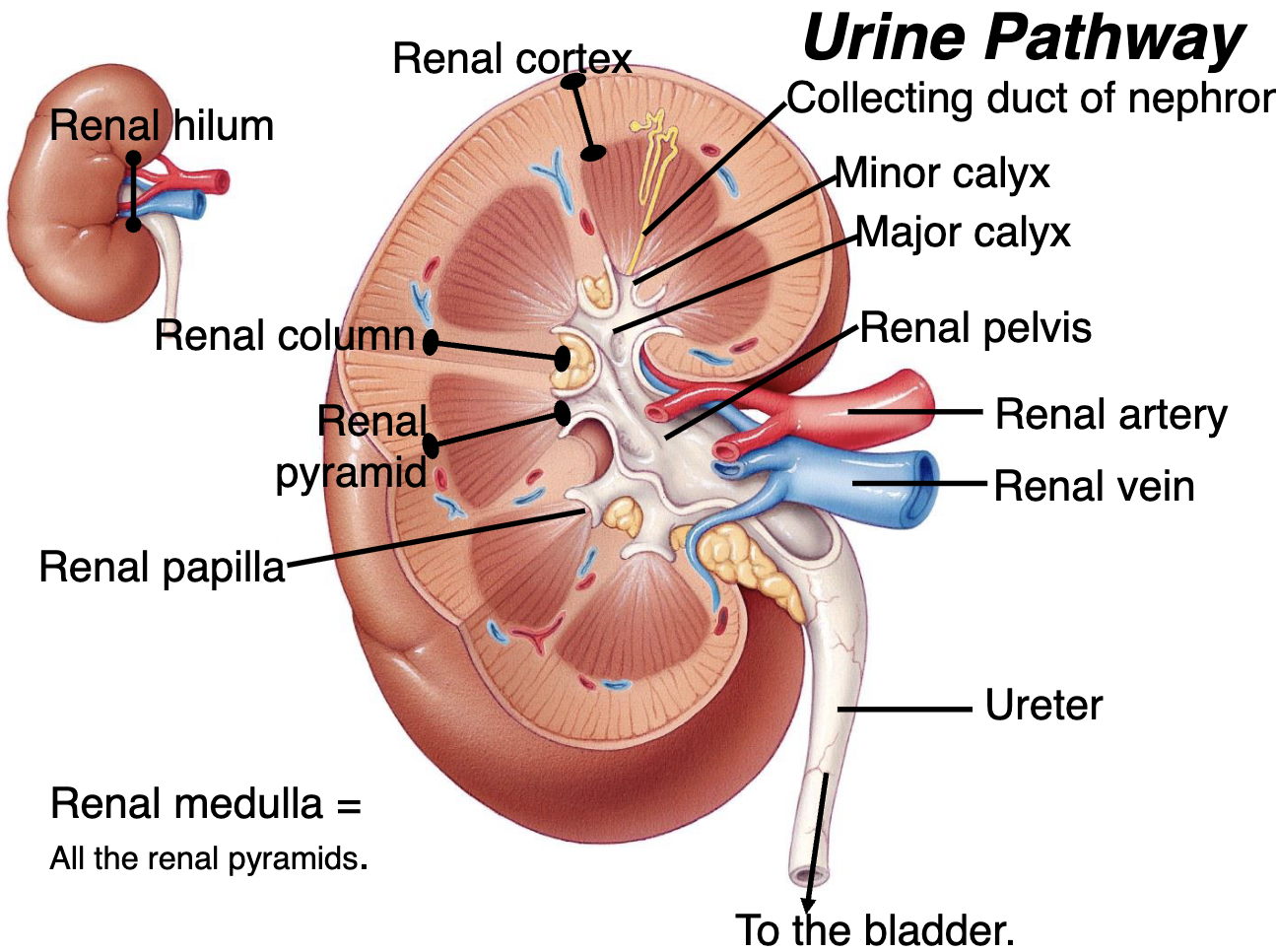
Describe the inside of the kidneys
Renal cortex
Renal column
Renal pyramid
Renal medulla = all the renal pyramids
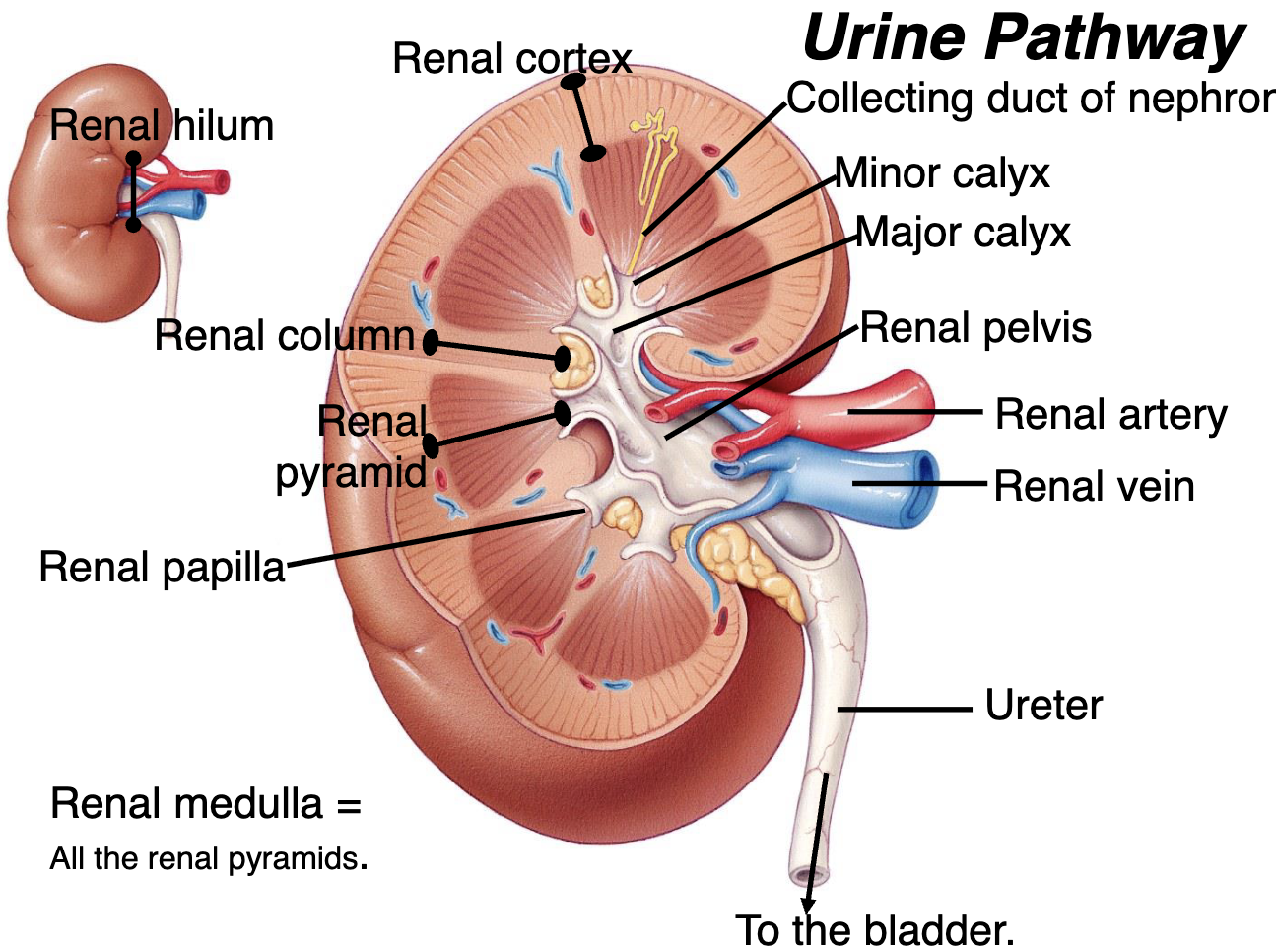
Describe the urine pathway
Nephron – Urine is produced here.
Collecting Duct
Renal Papilla
Minor Calyx
Major Calyx
Renal Pelvis
Ureter
Bladder
Describe developmental problems and pathologies for the kidneys
Polycystic kidneys
4 ureter (2 for every kidney)
The kidneys are hung together → horseshoe kidney
Ureter is extremely distended → hydronephrosis (swelling of ureter)
Describe the mystery of the kidneys
20-25% of blood goes to kidney, but kidney is only 1-0.5% of the body weight
From 20-25% → 180 L is made into filtrate by the nephron, however filtrate has virtually no protein or formed elements of the blood or any large molecule.
Even though filtrate has a lot of small molecules like glucose, amino acids, and bicarbonate ions, the urine has basically no protein, glucose, or bicarbonate.
Out of 180 L of filtrate, only 1 L of urine is made in a day (99% is reabsorb)
Describe the circulation of the nephron
Afferent arteriole → blood goes in
Efferent arteriole → blood goes out
Peritubular capillaries
Blood goes back to the venous circulation
Describe the parts involved in filtration
Renal corpuscle → filtrate making machine
Glomerulus → make filtrate
Renal tubule → makes filtrate into urine
Reabsorption of material from the filtrate in the tubule to the blood (ex. glucose)
Secretion of material from the blood to the tubule (ex. Drugs and penicillin)
Collecting duct → collects and concentrate the urine
Describe the juxtaglomerular apparatus
Macula densa
Granular cells
Mesangial cells
Sympathetic nerve on the afferent arteriole → constrict arteriole to prevent peeing
Describe the renal corpuscle function
The glomerular capsule is a continuous layer of tissue with the glomerular capillaries jammed into the centre
The space between the visceral and parietal layer is the capsular space, and that is what the filtrate is formed
Afferent blood comes in and pressure in the capillaries make filtrate into the capsular space
Describe the relationship between the heart and the kidneys
The kidneys work in partnership with the CV system
The CV system generates the pressure for glomerular filtration and drives the high flow needed to maintain a stable cortical interstitial solute composition.
The kidneys…
Maintain blood volume
Regulate plasma osmolality
Secrete mediators
Affect both cardiac performance and vascular tone
Describe net filtration pressure
Pressure pushing fluid out of the glomerular capillaries → positive pressure
Blood, hydrostatic pressure in the capillaries
Pressures holding fluid in the glomerular capillaries → negative pressures
Capsular hydrostatic pressure (i.e. the presence of fluid already in the capsule)
Blood osmotic pressure (i.e. the attraction of the dissolved materials in the blood for water)
Usually a net positive pressure of 10 mm of Hg.
This pressure is what pushes filtrate into capsular space and determines the glomerular filtration rate (GFR)
Describe auto-regulation of the glomerular filtration rate (GFR)
Kidney itself can act to alter the GFR by autoregulation and are normally trying to maintain a GFR
The GFR is easily altered by changing the blood pressure in the glomerulus or the leakiness of the capillaries of the glomerulus
The changes in the glomerulus pressure are done by the myogenic mechanism or tubuloglomerular feedback
Describe the myogenic mechanism
The smooth muscle of the afferent arteriole is stretched by the increase in blood pressure and afferent arteriole responds with constriction which decreases GFR.
Describe the tuboglomerular feedback
The macula densa of the juxtaglomerular apparatus detects high amounts of filtrate flow (i.e. lots of water and Na+ and Cl- flowing past) an increases adenosine release which causes Ca2+ release and constructs the afferent arteriole which decreases GFR.
High concentration of flow of Na+
Increase in adenosine
Constriction of afferent arteriole
Describe hormone regulation of GFR
Atrial natriuretic peptide (ANP)
Made in the atrium of your heart.
Distension of the atrium of the heart loads to the release of ANP
Relaxation of the mesangial cells between the glomerular capillaries, which becomes more spread out and relaxed so more filtration can occur.
ANP also relaxes afferent arteriole of the glomerulus and increases Na+ loss
Angiotensin II
Decreases GFR, because it constricts afferent arterioles.
However, it increases blood pressure because it constricts systemic arterioles.Angiotensinogen –(renin)→ Angiotensin –(ACE)→ Angiotensin II
Describe angiotensin and BP
Decrease in blood pressure/sympathetic nervous system stimulation
Juxtaglomerular apparatus senses that and releases renin
Which creates angiotensin II
Constriction of systematic and glomerular afferent arterioles
Blood pressure increases (negative feedback, turns off loop)
Describe neural regulation of GFR
The sympathetic branch of autonomic nervous system has inputs muscular walls of the afferent arterioles
The receptors are alpha1-adrenoceptors just like most of the rest of the arterioles in the body
WIth low blood flow, the glomerular hydrostatic pressure goes down and then filtration decreases
Describe renal filtration in terms of GFR
Sympathetic stimulation/Low BP
Increase in renin release
Increased BP from more angiotensin II and more Na+ reuptake in tubules.
What do we do with 180 L of filtrate
Completely absorbed → glucose, AA, bicarbonate ion
Regulated and thus is reabsorbed → water, sodium, potassium, chloride
Excreted as waste → urea, creatinine, drugs, and drug metabolites
What is gained and lost between filtrate and urine?
180 L of water in filtrate → 1-2 L of urine
162 g of glucose in the filtrate → but none in the urine
570 g of Na in the filtrate → but 4 g excreted
Uric acid 8.5 g in filtrate → 0.8 g in urine
Creatinine 1.6 g in filtrate and 1.6 g in the urine
Beyond the renal corpuscle the nephron is completely consumed with regulating these substances
Describe the blood supply/drainage of the renal tubules
Renal arteries
Lobar arteries
Arcuate artery
Branches into radial arteries
Coming off of that are afferent arteries
Capillary bed between afferent arteries and efferent arteries
Goes to venous drainage in arcuate vein
Describe how water/molecules move through the membrane
Reabsorption can occur by either
Active transport → requires energy
Passive transport → chemicals following their electrochemical gradients
The movement of water is by osmosis
Passive mechanism by which water follows its concentration gradient through semipermeable membrane
Describe passive transport
Does not need energy
Paracellular route → some solutes can slip between the tight junctions of the cell
Transcellular route → Into/out of the cells of the tubules by following electrochemical gradients (most common)
Diffusion may be facilitated by transport proteins in the movement of glucose from inside of the tubular cells to the interstitial fluid
Leakage channels also exist for some ions to facilitate their walk down the concentration gradient
What if the kidneys fail?
Salts (Na+, K+, Ca2+, and Cl-, all electrolytes) and waste products like urea build up and the pH of the blood goes down
Massive edema results from salt retention
Acidemia results from the inability to excrete acids
When potassium levels get too high (hyperkalemia) then cardiac arrest occurs
Describe therapeutics for kidney failure
Hemodialysis
Peritoneal dialysis
Kidney transplant
Describe peeing
Ureter
Derusor muscle → bug smooth muscle that expels urine
Ureteral opening
Urethral opening
Triangular area called trigone that does not contract
External urethral sphincter
For females, it goes ⅓ up urethra
For males, has additional internal sphincter at the neck of the bladder isolate prostate from bladder so that during ejaculation, the semen does not go backwards
Sits in deep transverse perineaus muscle
Levator ani → 3 muscles working together, because urethral sphincter is under your control, when the levator muscles pull, they help close
Pubic sphincter, external urethral a sphincter, and levator ani all work together to close your urethra
Describe the micturition reflex
Bladder fills about 200-400 ml of urine, the stretch receptors in the bladder wall are stimulated and send messages to the sacral portion of the spinal cord
Sensory input to this level triggers an autonomic reflex which sends parasympathetic motor signals to the detrusor muscle (a smooth muscle) to contract and the internal urethral sphincter (in males) to relax.
Internal sphincter is made of smooth muscle, thus regulated by ANS and not under voluntary control
The external urethral sphincter (in males and females) is striated muscle and thus can be consciously controlled.
Other muscles like the levator ani and deep muscles of the perineum can help too.
The somatic nerves holding this sphincter closed are inhibited by the micturition reflex → pressure build up is usually not enough to open the external sphincter.
In adults → conscious effort to relax the external sphincter before urine can pass through (although this does not last forever)
Describe diuretics (water pills)
Furosemide (LASIX) work by inhibiting the Na+-K+2CL- pumps in the ascending loop of Henle.
This means less ions are pumped into the interstitial fluid and thus less fluid is pulled out of the descending limb of the LOH and more urine.
List hormonal ways to regulate tubular reabsorption
Antidiuretic hormone
ADH aka vasopressin
Angiotensis II and BP
How to measure kidney function
Urinalysis and performing blood tests
Urinalysis analyzes the volume, physical, chemical, and microscopic properties of urine
Blood analysis involves looking at the levels of waste products
Describe blood urea nitrogen (BUN)
Measure of urea nitrogen which is produced due to protein breakdown and usually excreted by the kidneys
BUN will increase in the blood when the GFR decreases sharply (renal disease), and urine production is low such as with dehydration.
Describe plasma creatinine
Waste product from breakdown of creatine phosphate in the skeletal muscle.
Normally the levels remain steady in the blood since urine excretion equals its discharge from muscle.
Describe renal clearance
How much material is going out of the urine → how quickly the kidneys are removing a substance from your body
Drugs are often cleared by the kidney, so you need to know how much is going out to know how much to put in
Ex. antibiotics are excreted renally, for example penicillin can become dangerous for someone with kidney failure because they cannot get rid of the drug
Describe high and low renal clearance
High renal clearance indicates efficient excretion of a substance from plasma to urine (e.g. penicillin, metformin)
Low renal clearance indicates low excretion from plasma to urine (e.g. glucose)
Describe first order process
The more there is to do, the more the body works on it → first order process
Contrast: alcohol, you clear 1 drink per hour which is not a first order process
You saturate the enzymes in the oliver, but drinking more doesn't make the process faster because it is not a first order process.
This means 8 drinks cleared in 8 hours
Describe GFR
Measure of the rate of blood filtration by the kidneys. GFR is determined by the flow from the plasma into the glomerular capsular space.
To estimate this, you need a substance that is not reabsorbed nor secreted by tubules so renal clearance is equal to GFR. Inulin (not insulin) is one example.
GFR can be measured by injecting inulin and measuring rate of urine output and concentrations of inulin in the blood and urine.
Creatine is usually used for GFR measures though a tiny amount is reabsorbed by tubules. Inulin is typically used for specialized studies.