Psychopathology & Mental Health Exam #3
1/74
Earn XP
Description and Tags
Ch. 10, 11, 13
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
75 Terms
positive symptoms of schizophrenia
do not refer to "good" symptoms, but to an excess or distortion of normal functions. Hallucinations and delusions.
hallucinations
sensory experience that seems real to the person having it, but occurs in the absence of any external perceptual stimulus, can be experienced in each of the 5 senses. Ex: auditory (hearing voices/sounds that aren’t there, voices narrating day, screaming, whispering), visual (seeing things that aren’t there, UFO in a backyard), olfactory or gustatory (smelling or tasting things, smelling decaying bodies). These often have relevance for the patient, become incorporated into people’s lives, command hallucinations together.
delusions
rigidly held inaccurate beliefs or misrepresented versions of reality. May be connected to hallucinations. Complications with assessing delusions, can be difficult to find the ultimate truths. Classified as "non bizarre" or "bizarre" based on whether they could possibly happen in real life.
types of delusions
persecutory (paranoia, people believe that others are out to get them)
referential (believing that something you see and hear are specifically meant to send you a message, lyric in a song)
somatic (bodily functions, something is wrong with them or their body)
religious (delusions where the context is religious in nature, believing they are a deity, ask if they are religious in general)
grandiose (people thinking they have a special power, role, that others don't, often these are linked together)
control (patient’s thoughts, emotions, perceptions or actions are under the control of a different agent: either another person, a spirit, a machine, or unknown forces.)
more unusual delusions
cotard: belief that you are dead (either literally or figuratively)
capgras: belief that a loved one has been replaces by an identical looking imposter
when is a belief delusional?
degree of conviction (how convinced is this person), preoccupation (how much do they think about it, how distressing is it, how are they changing their behavior), not shared by others, personal (vs. broad) reference, difficult to resist, behavior change
negative symptoms
Aspects of normal behavior and social relationships that should be present are absent.
Diminished verbal and non-verbal expression (aka expressive negative symptoms): blunted affect (facial and verbal), alogia
Diminished motivation and pleasure (aka motivation and pleasure negative symptoms): avolition (a lack of interest or engagement in goal-directed behavior), asociality (social withdrawal), anhedonia.
anhedonia in schizophrenia vs. anhedonia in depression
MDD: diminished capacity for anticipatory AND consummatory pleasure
SZ: finding more mixed across studies, people with SZ may have negative symptoms and/or depression. associated with reduced anticipatory but not consummatory pleasure. some work suggests negative symptoms are related to a reduced ability to predict future pleasure overall.
anticipatory pleasure
wanting, pleasure from thinking about future activities
consummatory pleasure
liking, in the moment pleasure from activities
disorganization
Reflect bizarre behaviors and disturbances in thinking
Disorganized speech: speech that is very difficult to follow, conveys little, if any, meaning, slips form one topic to another, word salad (saying a lot of words, but not sure what you're saying, makes sense to them)
Catatonic behavior: decreased awareness of an reactivity to environment (immobility, marked muscular rigidly, purposeless/repetitious motor activity)
Grossly disorganized behavior: may range from childlike silliness to unpredictable agitation, should be distinguished from aimless or un-purposeful behavior, agitated behavior (if reason is understandable)
cognitive impairments in people with SZ
working memory, executive functioning, social cognition (theory of mind), level of cognitive impairment is associated with everyday functioning. cognitive impairments are not diagnostic criteria.
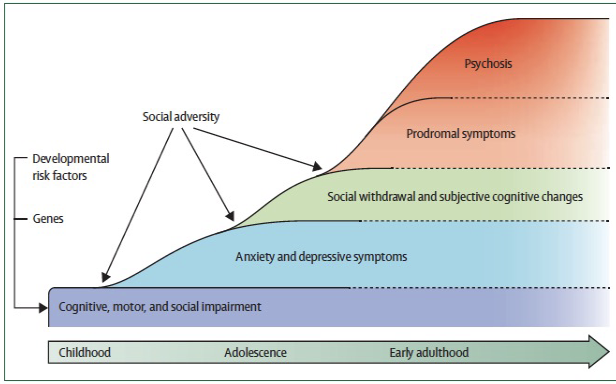
phases of SZ
1) prodromal phase: more social isolation, reduction in cognitive functioning
2) active phase: most severe, symptoms of psychosis like delusions, hallucinations, and jumbled speech and thoughts
3) residual phase: not as extreme, but symptoms still pop up
clinical high risk for psychosis
Individuals with onset of prodromal-like symptoms/behavior change (attenuated psychotic symptoms, worsening school performance, social withdrawal)
Large research area (identification of individuals at-risk for developing a psychotic disorder, goal is early detection and prevention to improve outcomes)
SZ criteria
Meet 2+ of the following symptoms (delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior), negative symptoms. At least one symptom must be delusions, hallucinations, or disorganized speech. Other criteria: impairment, disturbance is greater than 6 months, rule out related disorders.
differential diagnoses for SZ
schizophreniform disorder: consider overall duration of symptoms,
brief psychotic disorder: consider overall duration of symptoms,
schizoaffective disorder: consider extent of psychotic vs. mood symptoms
mood disorder with psychotic features: consider extent of psychotic vs. mood symptoms
delusional disorder
overall duration of sz
brief psychotic disorder: 1 day - 1 month. need 1+: delusions, hallucinations, disorganized speech, disorganized behavior. return to premorbid level of functioning after 1 month.
shizophreniform disorder: 1-6 months. same criterion A symptoms as sz, but shorter duration, impairment not necessary in diagnosis.
schizophrenia: >6 months, duration includes prodromal, active, and residual phases. active stage must be >1 month.
mood vs. psychotic symptoms
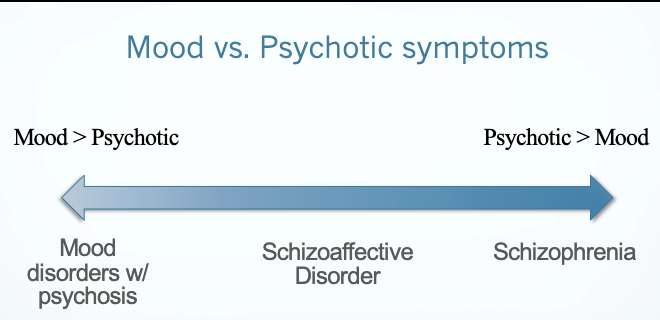
mood disorders with psychosis
bipolar disorder w psychotic features or MDD w psychotic features. psychotic symptoms only occur during a mood episode (mania or depression), mood congruent psychosis
schizoaffective disorder with psychosis
delusions or hallucinations for 2+ weeks in absence of mood symptoms. mood symptoms present for majority of psychosis (active and residual).
sz and psychosis
if depression and/or mania symptoms are present, their duration must be brief compared to sz symptoms.
delusional disorder
presence of 1 (or more) delusion with duration of 1 month or longer. criterion A for sz not met, functioning not markedly impaired.
culture and auditory hallucinations study
question: how do individuals with sz, who live in very different cultures around the world, experience their auditory hallucinations?
method: participants from san mateo, california, accra, ghana, chennai, india. N = 20 for each location. all individuals were diagnosed with sz or schizoaffective disorder and experienced auditory hallucinations. results: similarities across cultures (good and bad voices, conversations with voices, voice of God). differences across cultures (in chennai and accra: more likely positive voices, voices as humans or human-like spirits, more likely to be kin, decreased description of them as part of an illness, in america: violent, harsher, many told to hurt others or themselves; more hated, symptoms of brain disease).
hypothesis for differences in culture
social expectations about minds and persons shape the voice-hearing experience of those with serious psychotic disorders. implications: stigma, changing one’s relationship with the voices, the utility of the medical model for all disorders.
history of sz
1) "madness" has existed since ancient times
2) in 1893: psychiatrist Emil Kraepelin begins using term dementia praecox
3) 1911: Eugen Bleuler renamed it to schizophrenia (splitting of the mind)
4) 1920s: word of schizophrenia came to the US became a disease of the familial. Idea of psychological break from reality as relatable, associated w white housewives struggling with pressures of housework.
5) Late 60s and 70s: transformation of schizophrenia during the civil rights movement. SZ as an illness of "violent" Black men. DSM-II: added hostility and aggression to SZ diagnosis. Diagnosis of prominent Black political activists (Malcolm X)
6) Race and SZ today. DSM updates and progress. APA apologized to POC. Continued considerations: Serious mental illness and correctional facilities, Possibilities of over diagnosis; Diathesis stress model and development of SZ: Perceived racial discrimination, Living conditions based on continued impact of systemic racism.
epidemiology of sz
lifetime prevalence of disorders in population is about 4%, 1% have sz. risk may vary by group. sex differences: men (vs. women) tend to have higher rates, earlier age of onset (men: 15-19, women: 26-29), worse premorbid functioning, a more severe course.
etiology of sz
biological factors: genetics (genetic predisposition), neural (brain structure and function, neurochemical irregularities), environmental: early (prenatal complications, early adversity), later (stressors, drug abuse).
sz and genes
polygenic (several genes have a very small but measurable impact). heritability (the likelihood that someone will develop sz if it runs in the family): offspring w both parents w sz = 46%, identical twins = 48%
pregnancy and birth complications in sz
ppl with sz are more likely to have been exposed to problems in-utero and/or at time of birth )ex: illness, nutritional deficiency, substance abuse during pregnancy, breached labor)
sz and ses
people w lower ses have a higher prevalence of sz
Hypo 1: social causation: negative factors related to low SES lead to dev of illness
Hypo 2: social selection: due to cog/social impairments, those who dev the illness are less able to progress to college or higher paying jobs drifting to a lower SES
urban vs. rural living in sz
urban birth, upbringing and/or residence increases risk for schizophrenia
migration and sz
higher rates of sz among people who have migrated to a new country. Risk appears to be related to the density of individuals from the same ethnic group (the more ppl the less risk for sz)
drug use and sz
linked to dev of sz, esp for those w genetic predis who use at a young age, kids at 15 who use marijuana regularly are 4x more likely to dev sz at 26
brain abnormalities and sz
no single lesion or neural cause of sz. It is common for abnormal structure and function in frontal cortex.
Brain structure: reduced gray matter volume, enlarged ventricles particularly in temporal lobe (amygdala, hippocampus, thalamus), reduced total brain volume
Brain function: abnormal patterns of connections btwn regions of the brain - dyconnectivity disorder, reduced activation in the prefrontal cortex associated with negative symptoms
dopamine hypothesis for szz
Dopamine is a neurotransmitter associated with reward, motivated behavior, cognitive functions, motor control.
original hypo: sz symptoms caused by excess dopamine
revised hypo: sz symptoms are caused by imbalance of dopamine system: hyperactive dopamine transmission in mesolimbic area --> positive symptoms, hyperactive dopamine transmission in prefrontal cortex --> negative symptoms.
Dopamine dysregulation in additional regions as well, and additional neurotransmitters are associated with sz.
neurodevelopment model of sz
genetic risk + early environmental factors can impact early brain development and thus increases likelihood of psychosis onset upon maturation with increased demands. ongoing stressors, substance use, lack of social support can further increase this risk.
medicinal treatments for sz
Classical/traditional antipsychotics (1st gen): 1950s: something works, but has adverse effects like extrapyramidal symptoms, tardive dyskenesia.
2nd gen atypical antipsychotics: 1990s, adverse effects: weight gain/obesity, still more risk of tardive dyskenisa. Clozapine additional factors (can get low white blood cells)
Both block dopamine receptors in the cortical and limbic areas. After recovery there are high relapse rates (65-70% in first yr after hospitalization if med is discontinued; 40% if treated with antipsychotic drugs). Patients encouraged to take meds after recovery, difficulties with med compliance
expressed emotion and sz
patients' families can be classified as high or low on expressed emotion. High EE: negative, critical and hostile attitudes and behavior on the part of the family and/or emotionally over-involved and intrusive towards patient. Evidence that relapse rates are higher among sz living with at least one family member w high EE
psychosocial treatments for sz
Focus on long-term strategies to improve qualities of life, usually alongside psychopharmacology. Types: individual therapy (CBTp), assertive community treatment, family-based therapy, social skills training
Goals: reduce stress and improve functioning
Step 1: engagement, 2: info gathering and formulation, 3: intervention, 4: relapse prevention
Working with delusions: approach depend on variety of factors: level of conviction, associated distress, behavior changes, functional impairment. May not be able to target with cognitive techniques: target associated distress/impairment, continue to track triggers and patterns, serve as a support, reduce risk of neg outcomes. Attempting to cognitively target content of delusions: collaborative empiricism. Tracking automatic thoughts and evidence, generating alternative explanations (3cs: catch it, check it, correct it). Behavioral experiments: reality testing, investigation analysis worksheet.
Working with hallucinations: may be able to target in conjunction with delusions. Additionally strategies: tracking, identifying associated thoughts/feelings/behaviors, coping skills/distraction to reduce stress, questioning the voice, selective attention exercises, target potentially associated lifestyle factors
Working with disorganized/negative symptoms: focus on targeting functional disruption, identification of barriers and motivators, example activities: tracking expected behavior vs. Experienced pleasure, daily scheduling, goal setting and assistance,
prognosis and outcome of sz
50% go on to recover or significantly improve post diagnosis. many live independently and work. several factors predict course. impact of stigma. there are many resources available, consideration of policy-level factors as support.
dependence
Psychological: the urge to take a psychoactive substance for reasons sych as alleviating negative moods, avoiding withdrawal symptoms, and preparing for an activity
Physiological: tolerance and withdrawal are seen as indicators
tolerance
the nervous system becomes less sensitive to the physiological effects of that chemical over time (needed 5 drinks when before needed 3). Heavy users of opioids, cocaine develop tolerance, don't develop for LSD
withdrawal
physiological symptoms a person experiences when one stops taking a drug. Specific symptoms depend on the type of substance used (nicotine: drowsiness, muscle tremors, and nausea, alcohol: delirium tremens, agitation confusion, psychotic symptoms, treated but needs immediate medical care). Withdrawal not seen with hallucinogens.
Drug of abuse (psychoactive substance)
a chemical substance that alters mood, changes perception, or changes brain functioning (legal, prescription, illegal). Types: alcohol, caffeine, cannabis, hallucinogens, inhalants, opioids, sedatives, stimulants, tobacco
addictive potential
drug-specific factors influence how the drug works, dosage to achieve desired effect and its route of administration, potential for harm
methamphetamine
highly addicting stimulant, provides quick, long-lasting high. Short term: increases dopamine, coming down: feel weak, lethargic, depressed. Long term use: produces structural changes in the brain, psychiatric problems associated with length of use
opioids
dream-like euphoria, pleasure rush, positive effects short-lasting. Deaths from prescriptions: 1999-2021: nearly 280,000 people dies in the US from overdoses involving prescription opioids. Overdose deaths involving prescription opioids in 2021 nearly five times that of 1999.
county variability of opioids received per resident
smaller cities or larger towns. higher percentage of white residents. higher number of dentists and primary care physicians. more people who are uninsured or unemployed. more residents who have diabetes, arthritis, or a disability.
overdose prevention
illicitly manufactured fentanyl, heroin, cocaine, or methamphetamine were involved in about 85% of drug overdose deaths first half of 2019. more than 3 out of 5 overdose deaths had at least one potential opportunity to intervene.
fentanyl
synthetic opioid drug, developed in 1959, FDA approved for pain relief and anesthesia, more potent than morphine and heroin
DSM-4 classification of substance abuse
Abuse: a person's ability to function becomes impaired, no tolerance, withdrawal or compulsive use
Criteria for substance abuse: during a 12-month period, 1 or more of the following causes significant impairment or distress. recurrent substance use: resulting in failure to fulfill role obligations; in situations in which it is hazardous; resulting in substance-related legal problems; continued use despite continued social or occupational problems caused by the drug.
DSM-4 classification for substance dependence
Dependence: repeated use of a drug that often results in tolerance, withdrawal, or compulsive drug taking behavior (also referred to as addiction)
Criteria for substance dependence: maladaptive pattern of use, leading to clinically significant impairment or distress, as manifest by 3 or more, occurring at any time in the same 12-month period. 1) tolerance 2) withdrawal 3) substance taken in larger amounts, or for longer periods of time, than intended 4) persistent desire or failed efforts to reduce drug use 5) great deal of time spent trying to obtain the drug, use the drug, or recover from effects of the drug 6) important social or occupational activities are given up or reduced because of drug use 7) continuous substance use despite knowledge of consequence of drug use.
DSM-5 classification of ___ use disorder
combines categories of abuse and dependence. each substance (but caffeine) is addressed as a single disorder (alcohol use disorder, cannabis use disorder, hallucinogen-related disorders, inhalant use disorders, etc.), drug craving added, problems with law enforcement eliminated.
DSM-5 alcohol use disorder criteria
during a 12-month period, 2 or more of 11 symptoms caused significant impairment or distress. impaired control, social impairment, risky use, tolerance and withdrawal. specify severity (mild, moderate, severe), remission (in early remission, in sustained remission).
gambling disorder
new in the DSM-5. activates reward systems, behavioral symptoms.
effects and course of alcohol use disorder
at higher levels, alcohol depresses brain functioning. at lower levels, alcohol stimulates certain brain cells and activates brain’s “pleasure areas.” acute alcohol effects: impaired speech and vision, interference in complex thought, poor coordination, loss of balance, depression and withdrawal. the course and the age of onset vary from person to person. alcoholism research indicates that individuals alternate between periods of heavy use and periods of relative abstinence.
alcohol city men/college men study
longitudinal study examined 456 inner-city adolescents from boston and 268 former harvard undergrads. met for alcohol abuse (35% of city men, 21% of college men), most alcoholic men went through repeated cycles of abstinence followed by relapse.
long-term psychological effects of alocholism
malnutrition, cirrhosis of the liver, stomach pains, chronic fatigue, oversensitivity, depression, poor judgment, loss of pride.
korsakoff syndrome
severe syndrome that can occur following many years of heavy alcohol use. memory deficit, confabulation, hallucinations.
lifetime prevalence of drug use
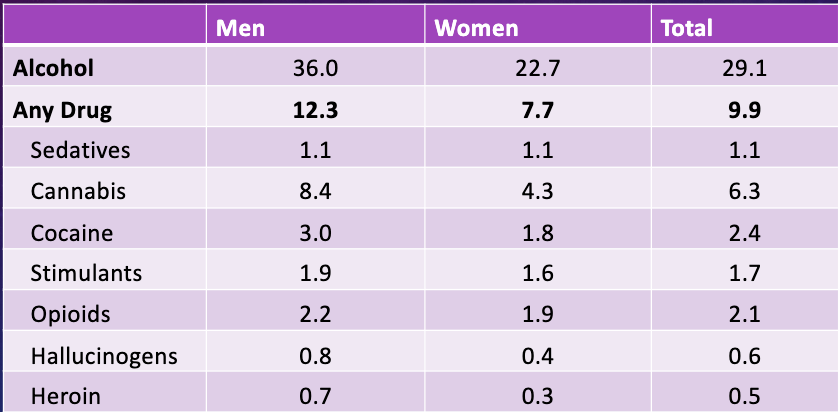
college students and substance use
83% drink alcohol, 24% use other substances (cannabis 98%), 80% indicated drinking as a leisure activity, 85% reported usually being with friend when drinking or using other substances. 50% of college students drank alcohol in the past month, 27% engaged in binge drinking.
binge drinking
national institute on alcohol abuse and alcoholism: binge drinking is a pattern of drinking that brings blood alcohol concentration levels .08 g/dL. this typically occurs after 4 drinks for women and 5 drinks for men - in about 2 hours.
national survey on drug use and health: binge drinking is drinking 5 or more alcoholic
alcohol use disorder in the workplace
N= 110,701 adults. 9.3% met criteria for aud, # of workdays missed is greater for aud, # of workdays missed increased in a stepwise fashion with increasing aud severity. Avg. # of missed days is 32 compared to 12
substance use disorder comorbidities
higher prevalence of mental disorders among patients with drug use disorders: substance use may increase vulnerability for other disorders, many use substances to cope w other symptoms and disorders (social anxiety disorder precedes aud)
AUD comorbidities w other substances: 40-50% have had another lifetime substance use disorder, 3 xs more likely to smoke tobacco
AUD comorbiities: internalizing psychopathology: prevalence of aud in those w lifetime mdd: 27-40% (median 30), prevalence of mdd in people with current aud: 4-22%. odds ratio of the 12-month comorbidity between aud and anxiety disorders: 2.1-3.3, someone is 2.1-3.3 times more likely to have that. prevalence of comorbid aud and ptsd ranges between 34-55%. aud in ppl with adhd is prevalent: adolescents and young adults (19-26%); adults (33%)
etiology of substance use disorders
2 out of every 3 men drink alcohol regularly, but very few have problems with it
biopsychosocial model: biology/genes, environment
Reasons for why people use substances: feel good, feel better, to do better, curiosity
Drug factors: speed of delivery. drug metabolism, tolerance, activation of the brain reward system (dopamine pathways)
genetics: genetic factors operate at all stages of addiction
psychological: classical and operant conditioning, opponent process theory
environmental/social: risk of addiction in adolescence: academics and times of transitions, home and parents, extroversion, expectancy effects (beliefs about drugs)
treatment goals for substance use disorder
acute treatment: detoxification, readiness to change. post-acute (long-term) treatment: abstinence, harm reduction
substance use disorder treatment type: CBT short-term
motivational interviewing: empirically supported non-confrontational therapy to help resolve ambivalence. core skills: open questions,
residential treatment for substance use disorder
both 24-hour care. short-term:
outpatient programs for substance use disorder treatment
less expensive, vary in type, intensity, and s
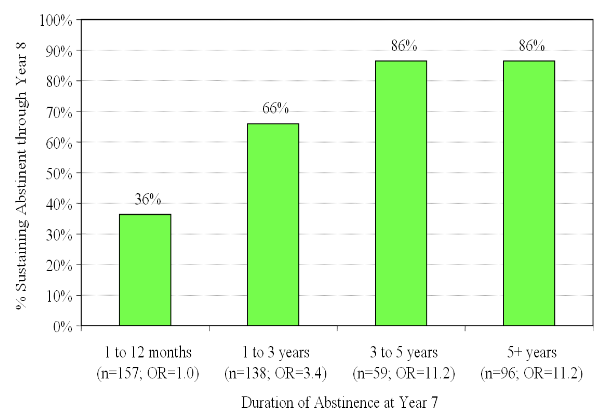
treatment efficacy for substance use disorder
longer treatment is more effective, relapse is not uncommon.