10/16/25-10/21/25 Anxiety disorders
1/66
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
67 Terms
What is anxiety?
Emotional state marked by the anticipation of danger of misfortune, intense distress, bodily tension, and nervousness
Accompanied by physical sensations
Why are people anxious?
It is a functional response- lack of anxiety is problematic, since it emerges in response to perceived threat
Throughout human history, anxiety played a pivotal role in the survival of our species
Creates physical change (aka fight or flight response) that mobilizes us to guard against or escape from danger successfully
What is the effect of anxiety being part of our evolutionary heritage?
We will all always experience it
What do anxiety disorders entail?
Levels of anxiety that are frequent, debilitating, and disproportionate to the circumstances
General prevalence of anxiety disorders
Among the most prevalent psychological disorders, ~1/3 of people will experience an anxiety disorder at some point
When does an anxiety disorder commonly start?
In childhood
What is one explanation for the high prevalence of anxiety disorders?
Humans who are alive today are the ones whose ancestors developed the keenest reactions to threats
How does evolution explain the early onset of anxiety?
Even a very young child needs to be prepared for fight or flight
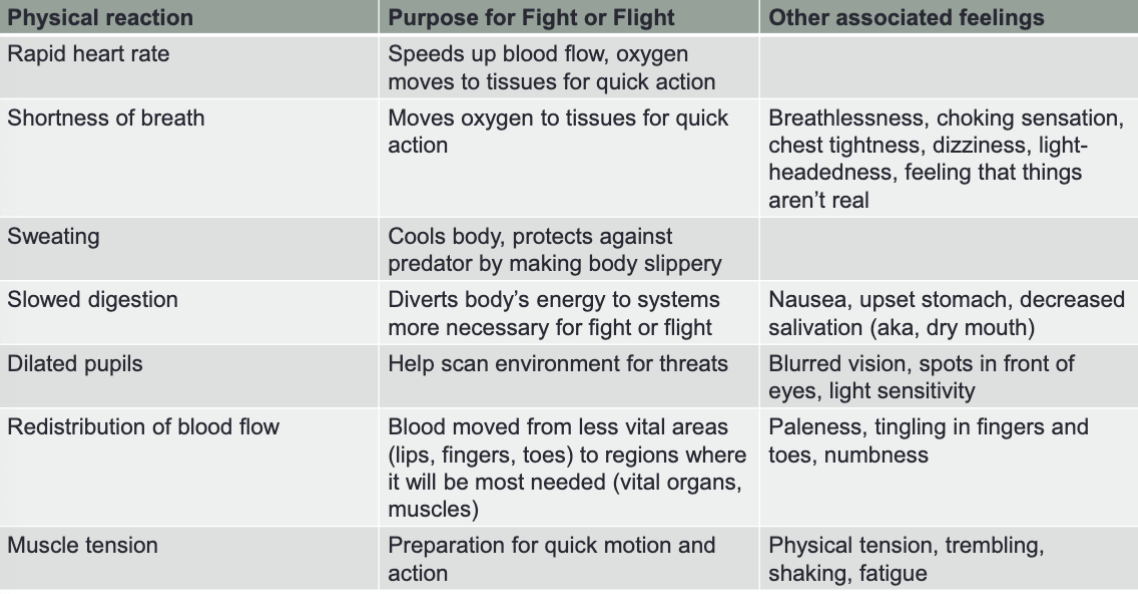
What are physical signs of anxiety derived from?
Derived from fight-or-flight response, it prioritizes directing energy to the most essential functions for survival
Does anxiety bring on the same or different symptoms depending on the circumstances?
The same symptoms manifest in you, regardless of the circumstances that bring them on, reflecting how fight-or-flight is effective against many types of threat
Examples of physical reactions / purpose for fight or flight / other associated feelings
2 main cognitive symptoms of anxiety
Fear/Perception of threat or danger- when we are anxious, we perceive ourselves as in danger even though we are physically safe
Worry- repetitive negative thoughts about the possibility of future danger, misfortune, or hardship
Are worry and perception of threat short-term or long-term?
Both worry and the perception of threat are often illusory
How are fear and worry different?
Fear and worry are related, but fear tends to be present-oriented (right now) whereas worry tends to be future oriented (anticipation)
“I’ve had a lot of worries in my life — most of which have never happened.” -Mark Twain
7 anxiety disorders in the DSM-5
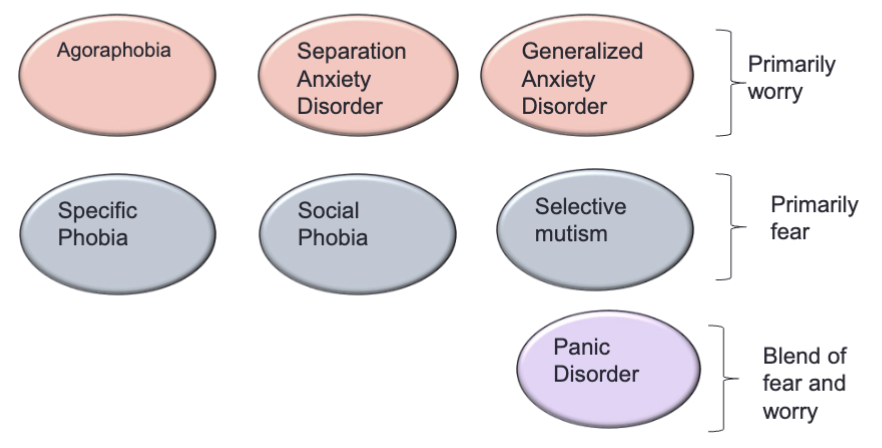
Comorbidity and anxiety disorders
Anxiety disorders are highly comorbid with each other.
People may often have predisposition towards anxiety, but will have different anxiety disorders at different points in their lives
Specific Phobia criteria
Marked fear or anxiety about a specific object or situation (e.g. flying, heights, animals, needles, blood, etc.)
Phobic object or situation almost always provokes immediate fear or anxiety. It is actively avoided or endured with intense fear or anxiety.
The fear or anxiety is out of proportion to the actual danger posed by the specific object or situation and to the sociocultural context.
The fear, anxiety, or avoidance is persistent, typically lasting 6+ months.
The fear, anxiety, or avoidance causes clinically significant distress or impairment in social, occupational or other important areas of functioning
Failure to meet the functioning criteria is why most of our normal fears are not considered phobias
Specific Phobia: main phobia categories
Blood, injection, injury
Situations (e.g. enclosed spaces, airplanes, elevators, bridges)
Natural environment (e.g. storms, heights)
Animals
In terms of evolutionary psychology, what is a theory about the main phobia categories?
These stimuli are things that posed a consistent threat to human survival throughout history, such as poisonous animals, dangerous environmental situations, and events that could cause injury or infection, like bleeding
Specific Phobia: if a phobic stimulus is encountered, what will happen?
The person will experience immediate fear/horror
What is the main behavioral symptom of anxiety?
Avoidance, because people do not want to feel that level of fear/distress
How is avoidance a paradox?
It reduces anxiety short-term, but will increase anxiety long-term, because it solidifies beliefs around phobic stimulus.
It also limits the opportunity to learn that seemingly threatening circumstances are not dangerous, so there is no formation of new beliefs or experiences.
Avoidant behavior provides negative reinforcement
Each time you engage in avoidant behavior, you eliminate aversive feelings of anxiety, making it more likely that you will engage in that behavior again/repeat it in the future
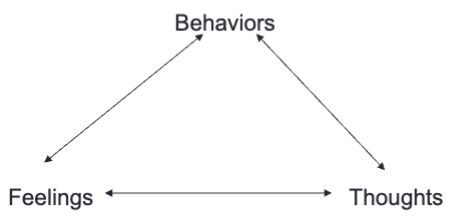
Treating phobias
The core of treatment is to eliminate reinforcement associated with avoidance.
If we consciously modify an avoidant behavior, we can change the beliefs that maintain anxiety and anxious feelings themselves
How can we eliminate the reinforcement associated with avoidance?
Through exposure therapy
Exposures (aka CBT for Specific Phobia)
The most effective treatments for phobias all involve exposure to a fear-provoking stimulus, but limiting the anxiety-reducing response (avoidance)
With prolonged exposure, people habituate (body acclimates to the feeling of anxiety), affirming that they can deal with a situation like this
Exposures help people form new beliefs about the feared situation and their ability to cope with it
What happens when confronting the phobic stimulus without avoidance?
Anxiety will be experienced → through this, exposure therapy is essentially making people more anxious right now, so that they will become less anxious in general
Fear and Avoidance Hierarchy
Part of exposure therapy
Developed collaboratively with therapist
Ordered list of situations in which a client experiences fear of phobic stimulus
Used as a guide for exposures in therapy, clients will work from least feared to most feared stimulus
Each situation gets rated in terms of how much fear it generates and the lengths to which a client will go to avoid that situation
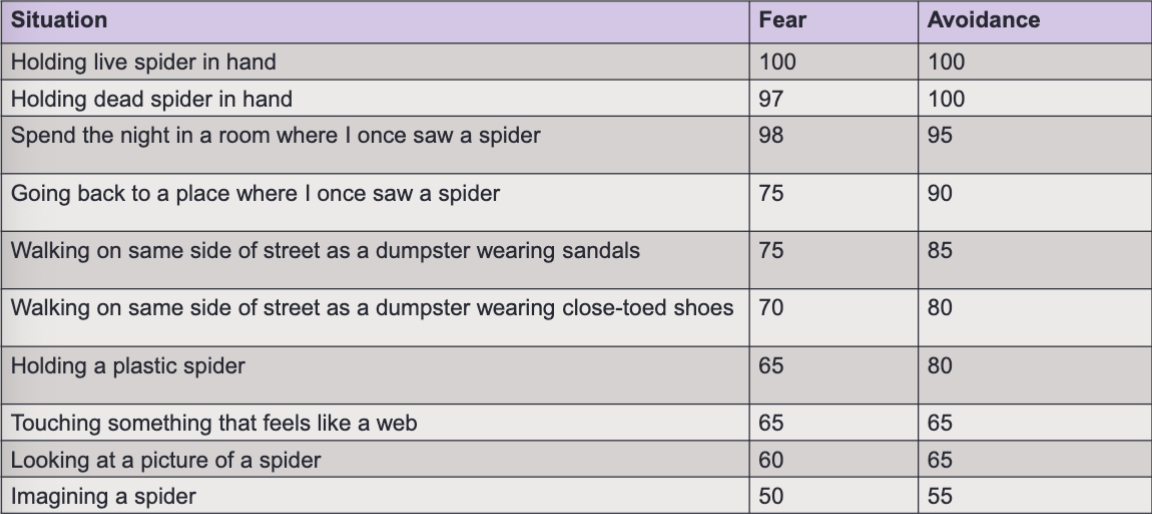
How are Fear and Avoidance Hierarchies individualized?
Every hierarchy is individualized to the client’s specific fears
Steps for effective exposure
Identify thoughts about situation before exposure occurs
Rate level of distress before exposure begins
During exposure, continue to rate distress every 5 minutes
During exposure, stay focused, do not try to distract self (avoidant behavior)
During exposure, maintain objective awareness of physical symptoms and thoughts
Continue exposure until anxiety goes down, 3 or 4 on a scale of 10 is optimal aka manageable feelings
After exposure, rate level of distress and evaluate thoughts again
Most important rule of anxiety treatment in general
Never stop an exposure before habituation occurs.
Otherwise, all that is reinforced is the sense that the anxiety producing stimulus is something that should be feared.
What are the 3 ways that exposures be conducted?
In session
In vivo (in life) - return to the place where the stimulus occurred
Imaginal
Goal for anxiety treatment
Realization that even though anxiety is uncomfortable, the risks of anxiety are minimal.
The goal is not to “get rid of anxiety”
Social Anxiety Disorder/Social Phobia (SAD) criteria
Marked fear or anxiety about one or more social situations in which the individual is exposed to possible scrutiny by others. Examples include social interactions (ex. having a conversation, meeting unfamiliar people), being observed (ex. eating or drinking), and performing in front of others (ex. giving a speech)
Fear that you will act in a way or show anxiety symptoms that will be negatively evaluated (i.e. it will be humiliating or embarrassing, it will lead to rejection or offend others)
The social situations almost always provoke fear or anxiety
The social situations are avoided or endured with intense fear or anxiety
The fear or anxiety is out of proportion to the actual threat posed by the social situation and to the sociocultural context
The fear anxiety or avoidance:
is persistent, typically lasting 6+mo
causes clinically significant distress or impairment in social, occupational, or other important areas of functioning
not attributable to substances or another medical condition
not better explained by the symptoms of another mental disorder (ex. panic, body dysmorphic, or autism spectrum)
if another medical condition (ex. Parkinson’s obesity, disfigurement from burns or injury) is present, the fear/anxiety/avoidance is clearly unrelated or excessive
SAD vs shyness
People who are shy do not show:
avoidant behaviors
fear of negative evaluation
physical symptoms of anxiety in social situations
impairment
Only about 12% of people who consider themselves shy and 10% of those described as shy by their family members meet criteria for SAD
SAD age of onset, prevalence
Early onset, often in adolescence
9-13% in the US, possibly more prevalent in females
Prevalence wanes over time
2x prevalent in people aged 18-29 years as in people over 60 years
SAD around the world
Some cultural components to SAD (the self vs the community)
less prevalent or presents in a different way in collectivist cultures (ex. many East Asian nations) which prioritize the well-being of the entire group, over individualistic cultures, which value independence, autonomy, and personal accomplishments
differing expectations for behavior
Example of culture interacting with SAD: Taijin kyofusho
A form of social anxiety present in Japan but not in the US, primarily centered around fear of offending or embarrassing others, rather than being embarrassed oneself
Treatment for SAD
CBT is first line treatment
Fear and avoidance hierarchy, focused on exposure to anxiety provoking social situations or events and re-eval of cognitions around these situations
Group and individual treatments are equally effective
How well does CBT work for SAD?
CBT worked better than Prozac+self exposure and Placebo+self exposur
cognitive therapy reduced symptoms more quickly and to a greater degree
gains were maintained at 1 and 5 year follow ups
Phobias and social anxiety disorder are often accompanied by what?
Accompanied by panic attacks
Panic attack
Abrupt surge of intense fear or intense discomfort that reaches a peak within minutes, and during which time 4 or more of the following symptoms occur:
Palpitations, pounding heart, or accelerated heart rate
Sweating
Trembling or shaking
Sensations or shortness of breath or smothering
Feelings of choking
Chest pain or discomfort
Nausea or abdominal distress
Feeling dizzy, unsteady, light-headed, or faint
Chills of heat sensations
Paresthesias (numbness or tingling sensations)
Derealization (feelings of unreality) or depersonalization (being detached from oneself)
Fear of losing control or “going crazy”
Fear of dying
Time limited aspect of panic attacks
Symptoms typically reach a peak in about 10 minutes and then decline
What do panic attacks feel like? Example from Kevin Love, pro basketball player
Heart racing
Trouble catching breath
Everything was spinning
Brain was trying to climb out of his head
Air felt thick and heavy
Body was trying to tell him he is about to die
2 types of panic attacks
Situationally bound: clear triggers like snakes, bugs, flying, social situations, etc.; part of the experience of Specific Phobia and SAD for some people
Not situationally bound: out of the blue, can even occur in the middle of the night, is a sign that you might have panic disorder
How can situationally bound panic attacks be reduced?
By treating the phobic stimuli that precede them
Frequency of panic attacks
Varies widely
some people have them daily, or even more than once a day
other people can go weeks or months without an attack, but worry about having one and show lots of avoidant behavior
Panic Disorder
Characterized by recurrent unexpected panic attacks
At least one of the attacks has been followed by 1 month (or more) of one or both of the following:
Persistent concern or worry about additional panic attacks or their consequences (e.g., losing control, having a heart attack, “going crazy”).
A significant maladaptive change in behavior related to the attacks (e.g., behaviors designed to avoid having panic attacks, such as avoidance of exercise or unfamiliar situations)
Agoraphobia
Anxiety about being in places in situations from which escape might be difficult (or embarrassing) or in which help may not be available in the event of having an unexpected or situationally predisposed panic attack or panic-like symptoms
Panic attacks may occur with or without comorbid agoraphobia
What are some forms of avoidance behaviors (to not panic) besides agoraphobia?
Restriction of caffeine and exercise (which increase heart rate)
Only doing certain activities when safety mechanisms are there (only driving with meds, only going certain places with a certain person, etc)
How common are panic attacks?
Panic attacks are common, 1/3 of people will experience a panic attack at some point during the lifespan
What percent of people who have a panic attack go on to develop panic disorder?
Only about 5%
Catastrophic Misinterpretations of Bodily Sensations
The tendency to interpret normal or innocuous physical feelings, such as a fast heartbeat or dizziness, as signs of a severe and dangerous medical condition, often leading to panic attacks
Believed to be the biggest reason some people develop panic disorder and others do not
Fear of Fear Model
Bodily sensations (heart pounding, rapid breathing, sweating, muscle tension, dizzy/lightheaded)
Uh oh reaction (I am having a heart attack, what if other people notice, what if I fall down or die)
Increased anxiety (worry about possibility of future panic, excessive focus on small changes in bodily state)
More symptoms (thoughts about the meaning of physical sensations keep body at high level of physiological arousal)
repeat
Treating Panic Disorder
Effective treatments for panic disorder blends exposures with cognitive restructuring about panic
if I panic, I won’t be able to handle it
I’m dying
Psychoeducation
what does a heart attack really feel like?
what are the evolutionary origins of panic symptoms
With panic, why do people perform avoidant behaviors?
People are trying to avoid the physical sensations of panic.
When treating panic, what should the focus of exposures be?
Exposures are a technique to extinguish the reinforcement associated with avoidance, so the focus for panic should be the same/similar kinds of physical sensations brought on by panic
Exposures for panic (2 stages)
Stage 1: Interoceptive exposures
exposures which are designed to mimic the physical sensations of panic in a controlled, intentional way
a Fear and Avoidance Hierarchy is constructed from these symptoms, rated according to intensity of symptom and similarity to panic
ex. breathing thru straw, head rolling, running in place, breath holding, body tensing, spinning in a swivel chair, hyperventilating, etc.
Stage 2: In vivo exposures
therapist and client construct/follow a new Fear and Avoidance Hierarchy for situations which typically bring on panic outside of therapy sessions
Generalized Anxiety Disorder (GAD) criteria
Excessive anxiety and worry (apprehensive expectation), occurring more days than not for 6+ months, about a number of events or activities (such as work or school performance)
Difficult to control the worry
Anxiety and worry are associated with 3 or more of the following 6 symptoms, with at least some symptoms having been present for more days than not for the past 6 months:
Restlessness or feeling keyed up/on edge
Being easily fatigued
Difficulty concentrating or mind going blank
Irritability
Muscle tension
Sleep disturbance (difficulty falling or staying asleep, or restless/unsatisfying sleep)
Anxiety, worry or physical symptoms cause clinically significant distress or impairment…
Disturbance not attributable to substance or medical condition
Not better explained by other mental disorders
How is GAD distinct from other anxiety disorders?
People with GAD mainly worry about everyday events (ex. chores, being late, family health or misfortunate, job)
Focus of worries shifts frequently
Meta worry: worry about not being able to control worry
Fewer “fight or flight” symptoms, more muscle tension
Less likely to present for treatment than other anxiety disorders, although some evidence that they may be more treated by primary care doctors than mental health field
More common in middle aged and older adults (avg age of onset is around 30yo)
GAD gender prevalence
More common in females
GAD comorbidity
Highly comorbid, especially with MDD and other anxiety disorders
Is GAD an acute or chronic disorder?
Chronic, with few remissions (when the signs and symptoms lessen or disappear)
GAD around the world
A huge study looking at 150k+ people across 26 different nations found that:
GAD is more common in higher income countries than lower or middle income ones
More impairment associated with GAD in higher income countries
Within high income countries, GAD is more prevalent in people with lower SES
Newman’s Contrast Avoidance Model
Suggests people with GAD are extremely sensitive to shifts in emotional state
Worrying keeps people in one emotional state and prevents sharp increases in negative emotions
The model reframes worry from a passive thought process to a logical, adaptive coping response
GAD and intolerance of uncertainty
Discomfort with not knowing the outcome of events, tends to be very high in people with GAD
Treatment of GAD
SSRIs, SNRIs are the biggest ones
Also CBT or third wave adaptations to CBT
these 2 treatments are equally effective in short term, but meds typically do not have benefits once discontinued and CBT is associated with reduced symptoms in the long term