11.2 kidney function
1/19
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
20 Terms
processes involved in producing urine
filtration (ultrafiltration)
reabsorption of filtered materials (back into the blood)
secretion into filtrate (to the urine)
at its proximal end, the nephron forms a cuplike structure — __, which is around a ball of capillaries (__)
Bowman’s capsule, glomerulus
process of filtration (think of where it occurs)
water, amino acids, ions, glucose, and nitrogenous waste molecules are forced from the glomerulus into Bowman’s capsule. the fluid in the Bowman’s capsule is called: filtrate
filtrate travels thru the nephron (where reabsorption and secretion occur) and drains into the collecting ducts and renal pelvis → ureter → urinary bladder → urethra
afferent arterioles deliver blood to the glomerulus
there are small spaces btwn the endothelial cells of the glomerular capillaries and the cells of the Bowman’s capsule. blood cells and proteins are too big to pass thru these spaces, but water, amino acids, ions, glucose, and nitrogenous waste molecules in fluid can pass through
pressure drives the mvmt of this fluid into the Bowman’s capsule
__ of arteries and glomerular capillaries maintains the __ needed to drive fluid into __
larger diameter (less resistance), pressure, Bowman’s capsule
efferent arterioles
receives blood from the glomerulus; has smaller diameter → blood “backs up” (dam) in glomerulus, keeping pressure high
the __ forces small molecules such as water, glucose, amino acids, sodium chloride, and urea through the filter, from the blood in the __ across the basement membrane of the __ and into the __. THIS TYPE OF HIGH PRESSURE FILTRATION IS __. THE FLUID FORMED IN THIS WAY IS CALLED __.
high pressure, glomerular capsule, Bowman’s capsule, nephron, ULTRAFILTRATION, GLOMERULAR FILTRATE
filtration in Bowman’s capsule begins the process of
excretion
__ and __ take place in the remainder of the __
reabsorption, secretion, nephron
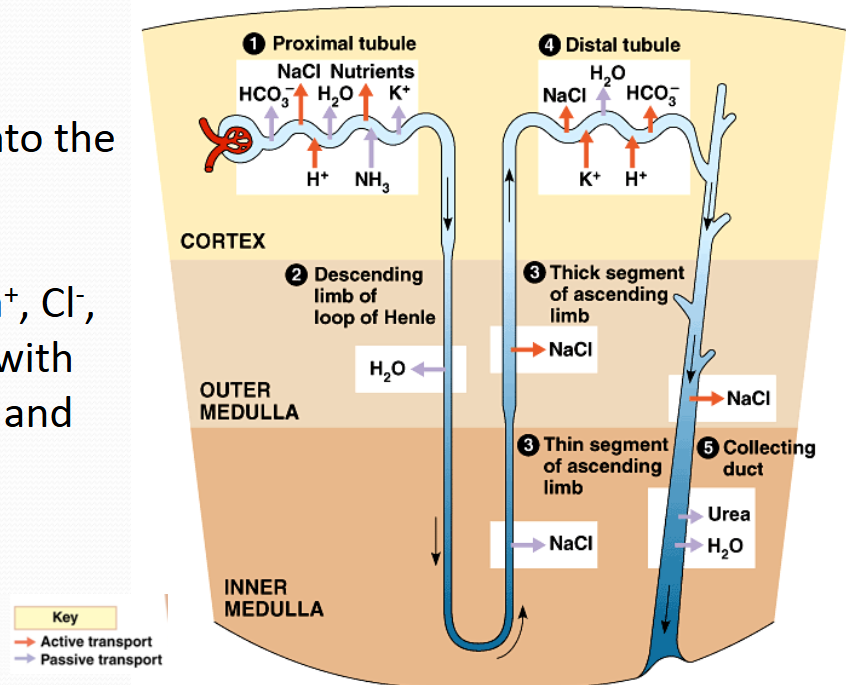
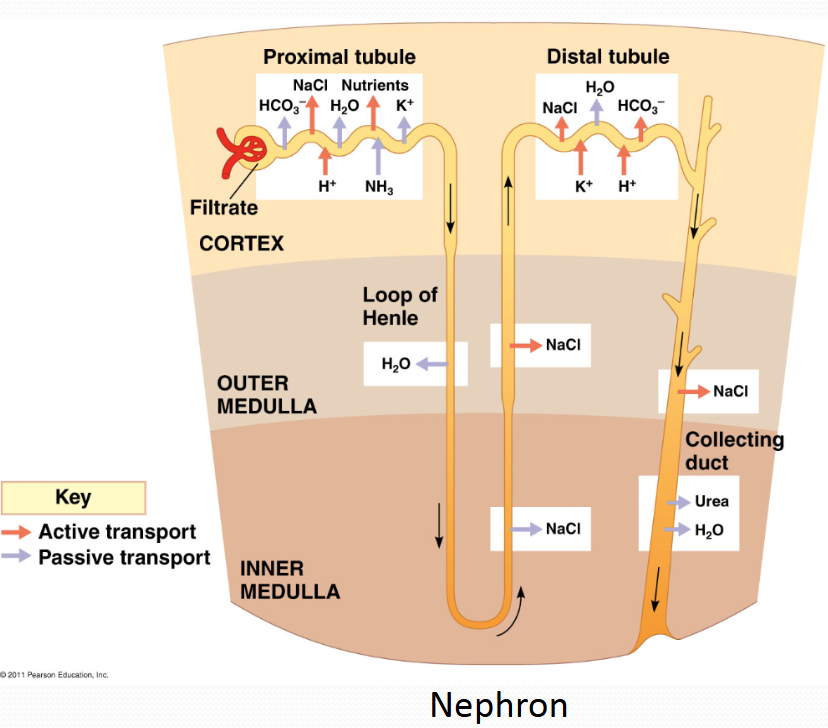
proximal tubule
secretes H+ into the filtrate
reabsorbs Na+, Cl-, and K+ along w water, HCO3-, and nutrients
main function: reabsorption of water, ions and nutrients back into the interstitial fluid
Na+/H+ exchangers and Na+/K+ pumps in epithelium of the tubule move Na+ from the filtrate into the interstitial fluid
movement of these positive ions results in a voltage gradient which causes Cl- ions to follow (that is, move from the filtrate into the interstitial fluid or get reabsorbed)
specific membrane proteins actively transport glucose, amino acids, and nutrients from the filtrate in the tubule to the interstitial fluid (reabsorption)
filtrate is now hypoosmotic to the interstitial fluid, so water moves from the tubule to the interstitial fluid via aquaporins) due to osmosis. water “follows” salt
nutrients, water, and HCO3- move from the interstitial fluid into the peritubular capillaries, and return to the circulation
loop of Henle
sets up a gradient of solutes in interstitial fluid
very high solute concentration towards pelvis of kidney
descending segment is for water reabsorption by osmosis
ascending segment is for Na+ and Cl- reabsorption
allows production of urine that is hyperosmotic to blood
descending loop of Henle
tubule passes thru increasingly higher regions of solute concentrations of interstitial fluid in medulla
thus, water moves out from the tubule
this, then, concentrates the filtrate in the tubule
by the bottom of the loop, osmolarity of fluid in tubule = osmolarity of medulla fluid
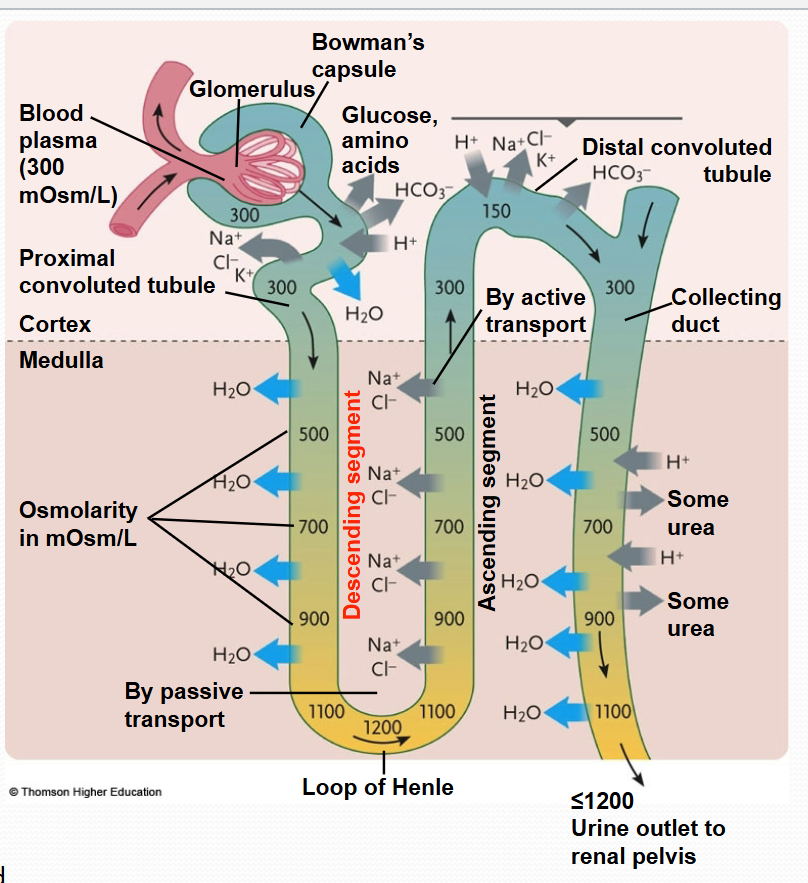
ascending loop of henle
Na+ and Cl- are reabsorbed (move from tubule to interstitial fluid)
as tubule ascends, Na+ and Cl- are actively transported out of the tubule, fluid in tubule has a lower osmolarity as tubule ascends toward Cortex
ascending limb is IMPERMEABLE to water bc of a lack of aquaporins
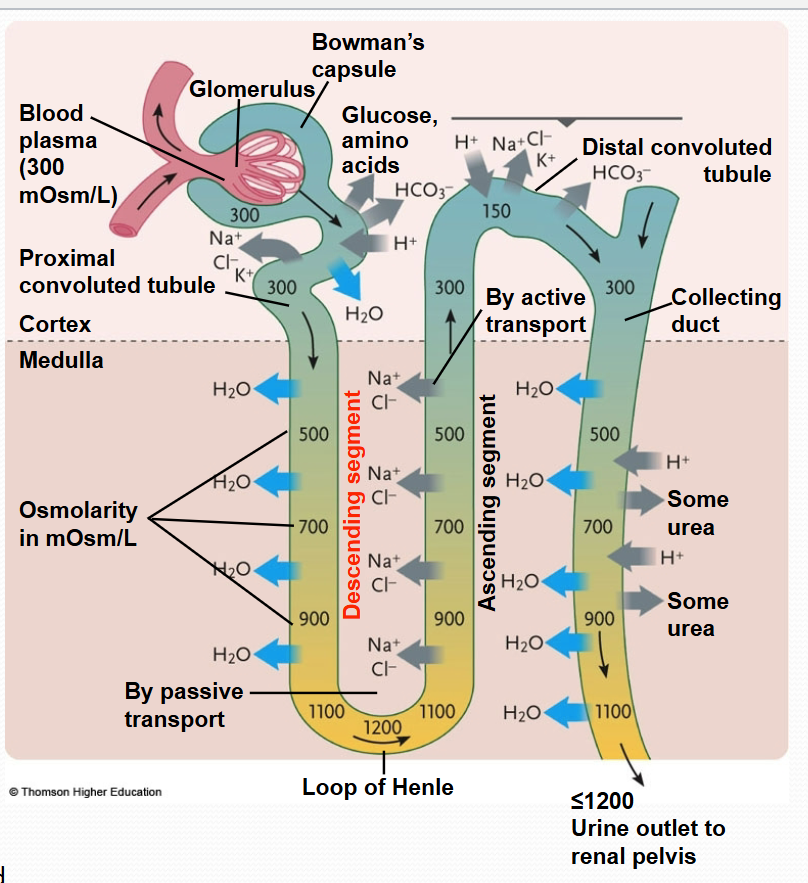
the design of the Loop of Henle and vasa recta give rise to the __ which enables interstitial fluid in kidney (cortex and medulla) to maintain a __. this concentration keeps the blood coming from the __ to the __ to not be too __, allows for __, and for __
counter-current multiplier, concentration gradient, vasa recta, renal vein, hyperosmotic, water reabsorption, the production of concentrated urine
counter current multiplier (counter current + multiplier)
counter current
flow of filtrate thru descending LoH is opposite to the flow thru the ascending LoH
flow of filtrate thru the LoH is in the opposite direction from the flow of blood thru the vasa recta
multiplier
as salt is transported out of the ascending LoH, the surrounding interstitial fluid becomes more concentrated, which causes water to move out of the descending loop (permeable to water but not salt)
this mvmt of water out of the filtrate of the descending LoH into the interstitial fluid causes the filtrate in the descending LoH to be more “salty”/concentrated, which makes the pumps in the ascending LoH pump out more salt
this positive feedback gives rise to the term “multiplier”, and it ends when max concentration is achieved, which is dependent on the capacity of the pumps on the ascending LoH
why doesn’t the water that moves out of the descending LoH dilute the concentration of the interstitial fluid?
because the vasa recta is reabsorbing the water (due to oncotic pressure of blood)
descending LoH is permeable to __, not __. as filtrate moves down, __ moves into __, thereby concentrating the filtrate in the part of the tubule that is deep in the __. here, blood flow in __ is moving __ and the water that is being __ by the descending LoH is being __ the bloodstream, so this water is not __ the interstitial fluid and ruining the concentration gradient in medulla.
water, salt, water, interstitial fluid, medulla, vasa recta, up, released, reabsorbed into, diluting
vasa recta capillaries have __ that make them highly permeable to __ and __, allowing for equilibration. thus the blood in the vasa recta remains nearly __ to the __ at each level so it doesn’t undo the osmotic gradient in the interstitial fluid.
fenestrae (pores), water, solutes, isosmotic, interstitial fluid
urea
contributes to the total osmolality of the interstitial fluid
the main nitrogen-containing substance in the urine of mammals; is highly soluble in water, and practically non-toxic
vasa recta also has urea transporters (for facilitated diffusion)
solutes (such as salt) and urea diffuse into the descending vasa recta. these same solutes then diffuse out of the ascending vasa recta and back into the interstitial fluid
why? bc at each lvl of the medulla, the concentration of solutes is higher in the ascending vasa recta vessels than the interstitial fluid AND the concentration of solutes is higher in the interstitial fluid than in the descending vasa recta vessels
what is reabsorbed and secreted by the distal convoluted tubule?
Na+, Cl-, H2O, and HCO3- are reabsorbed
K+ and H+ is secreted
collecting duct
function: to concentrate urine
as duct descends, there is an increasing solute gradient in the medulla
H2O moves out of the duct
some urea is passively transported out of the duct, which adds to the increasing solute gradient in the medulla
H+ is secreted into the duct