Compartment Syndrome, Fixation, Trauma I
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
49 Terms
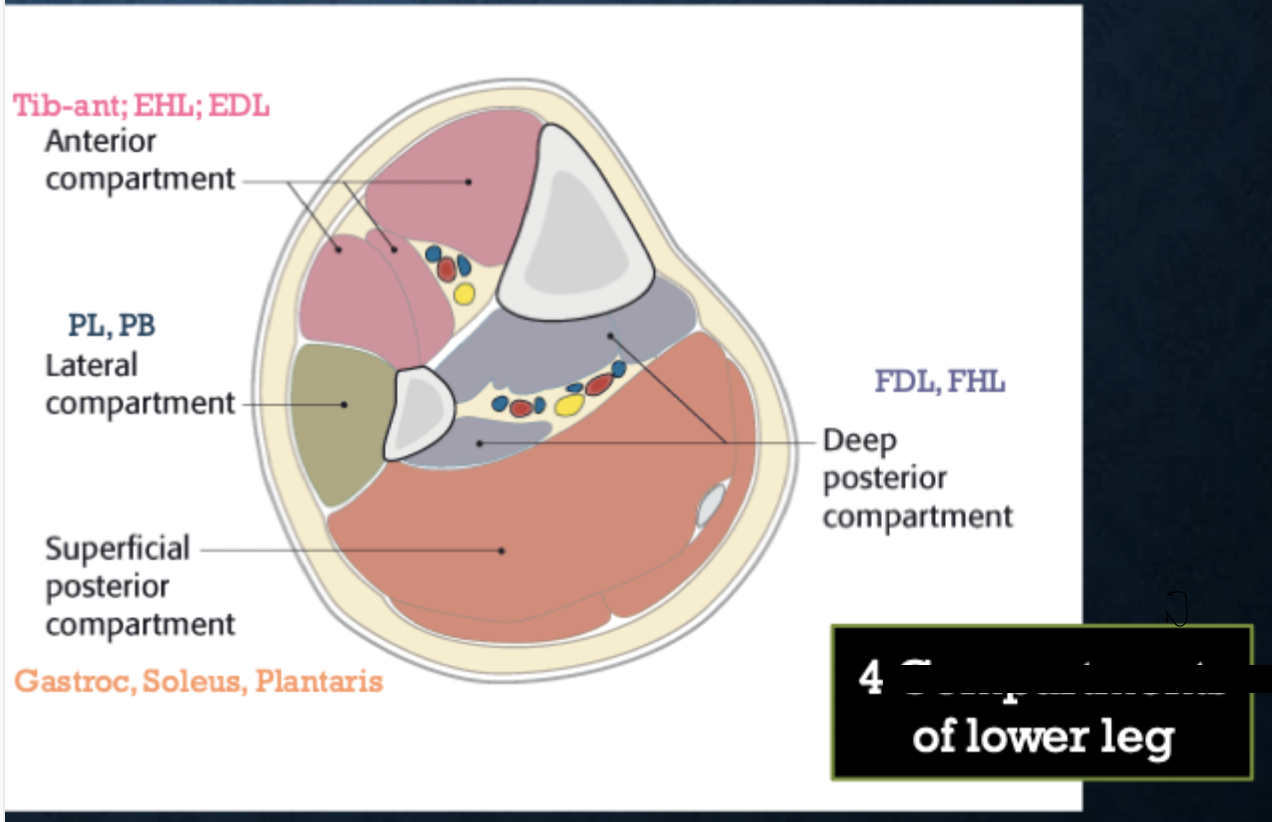
Compartment
Grouping of muscles, nerves, and blood vessels covered by fascia
Compartment Syndrome
What occurs when the pressure within a compartment increases restricting blood flow to muscles and nerves leading to extreme pain OR irreversible damage to surrounding soft-tissue structures
acute
Which compartment syndrome has symptoms that are severe and short-lasting that is a MEDICAL EMERGENCY and can lead to PERMANENT DAMAGE
Chronic (exertional compartment syndrome)
Which compartment syndrome has symptoms of pain and swelling that can be long lasting and is usually caused by running, cycling, etc → reversible with rest
Severe injury (crush, fracture (75%)), reprofusion after blocked circulation (tourniquets in surgery, prolonged lining on extremity), constricting bandage (tight ace bandage, cast → leave room for swelling)
What can cause acute compartment syndrome
***Pain is out of proportion with passive stretch (earliest sign)***, pallor, paralysis (late), parethesia (late), pulselessness, poikothermia (cold skin)
6 signs of compartment syndrome
Clinical, Needle Manometry over 30 mmHG (20 in hypotensive) - definitive, not necessary, must measure all compartments
Diagnosis of compartment syndrome
Call ortho, remove restrictive casts/dressing, keep extremity at heart level, prevent hypotension, obtain compartment pressure (if you’re really overzealous), serial physicals and compartment pressures hourly, Fasciotomy with wound vac - GOLD STANDARD, Skin grafts in the future
45 y/o male presents to the ER for extreme leg pain 10/10, he states that his ex-girlfriend SLAMMED it in a car door. On physical exam you note that the pain is out of proportion with what you would expect and that the pain is exacerbated on passive stretch. What is your game plan?
arterial thrombus, DVT, cellulitis, necrotizing infection, rhabdo
DDX for compartment syndrome
Within 6 hrs (100% recover), after this there may be irreversible damage (high infection risk, amputation)
Prognosis for Compartment syndrome
Reduction and fixation to restore anatomy, Fixation provides stability, Preserve the blood supply, mobilize patients early
AO Principles
Treating soft tissue injuries/fracture/dislocations/reconstructive surgery, provide stability, maintain alignment of the bones
What is the purpose of fixation?
external (splint, cast, external frame), internal (medical implants, screws, plates, intra-medullary nail/rods)
Types of fixation
Splint
What type of fixation is non-circumferential and ideal for initial and temporary management?
Cast
What type of fixation is circumferential providing superior immobilization for complex and/or definitive non-operative management but complications like chronic pain, joint stiffness, muscle atrophy, etc.
external fixators
What type of fixation is accomplished by placing pins or screws into the bone on both ends of the fracture and secured together OUTSIDE the skin with clamps and rods (external frame) there is however a risk of infection were the pins are inserted
Open reduction internal fixation (ORIF)
Medical implants used to stabilize and hold bone fragments in place after fractures or other injuries - plates and screws (restrict weight bearing), BIG incisions more infection risk?
Intramedullary nail (IMN)
What type of fixation is inserted into the bone marrow canal in the center of the long bones of the extremities (femur, tib, humerus) - shares the load so weight bearing can occur more quickly and has smaller incisions
indirect
Bones heal with micromotion leading to callous formation (rod)
Direct
Bones come together with NO motion and fragments are compressed together (plates and screws)
Reduction (closed = no incision, open = incision, closed wasn’t working)
Used when the bone is fractured and out of alignment/unstable → reset into a more stable position
removes skin tension, reduces swelling/bleeding, decreases pain, relaxes pain, relaxes muscle, improves alignment
Benefits of reduction
Which bone, Which part of bone (distal, proximal, mid-shaft), pattern of fracture (transverse, oblique, spiral, comminuted, butterfly, impacted), presence of deformity (angulation - varus, valgus, dorsal, volar, anterior, posterior), intra vs extra-articular, right vs. left
When describing a fracture to an ortho bro, how do we not look like idiots?
Closed (simple)
A fracture that has no open wounds of skin
Open (compoud)
A fracture with disruption of skin at the area of the bone → call ortho IMMEDIATELY for surgical
Check neurovascular status, tetanus, IV antibiotics, Irrigate bedside, call ortho, surgical irrigation, closed reduction, wound dressing
Gameplan for any open fractures
abduction, extension, external rotation
Anterior shoulder dislocations (90%) are caused by
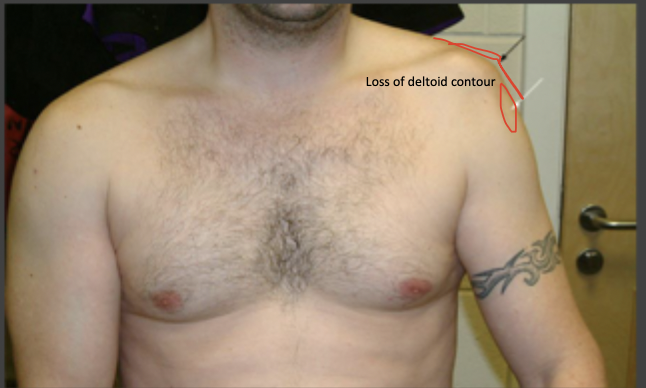
Axillary
Which nerve are we worried about for anterior shoulder dislocations?
Pre-/post- reduction NV exam, sling for 1-2 weeks with gentle, progressive ROM exercises (avoid frozen shoulder)
Gameplan for anterior shoulder dislocations
seizure, electric shock, forced adduction internal rotation
While posterior shoulder dislocations are rare what are they commonly caused by
Internal rotation and adduction (often find the shoulder locked in internal rotation)
MOI for posterior shoulder dislocation
Milch maneuver
Most common way to put a shoulder back into place

Normal axillary view for reference
Normal axillary view for reference
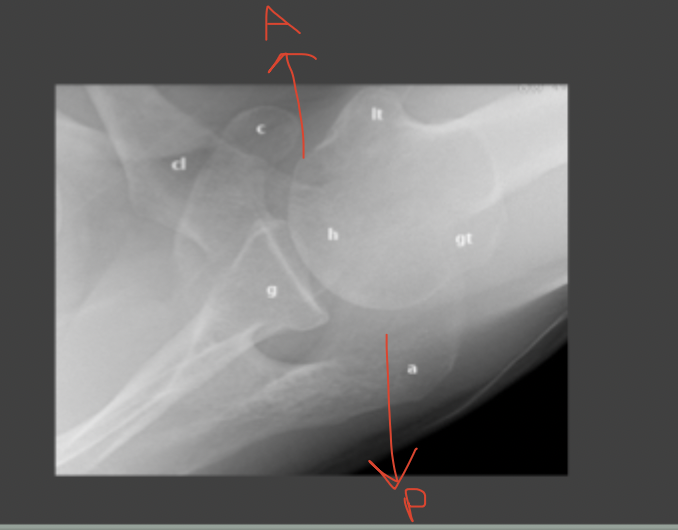
axillary
To determine which direction a shoulder dislocation occurred what view do you need?
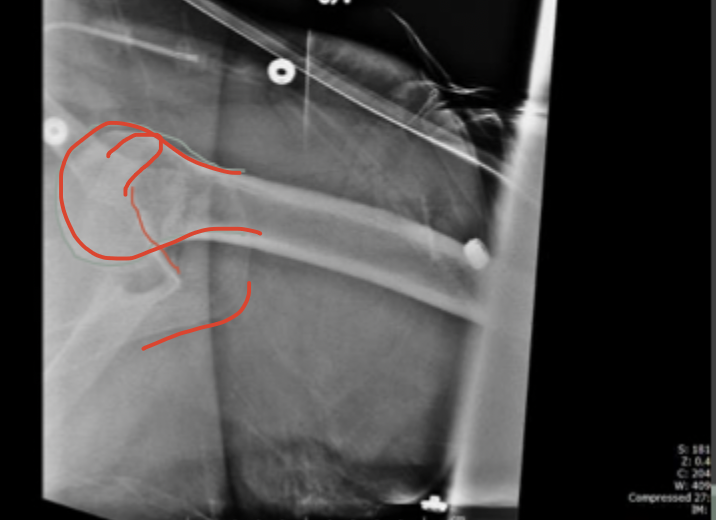
anterior dislocation
Which direction
Posterior
A lightbulb sign in the AP view is what type of dislocation
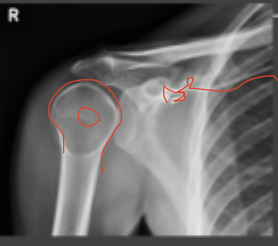
Bankart lesion
An injury of the anterior (inferior) glenoid labrum associated with shoulder dislocations - surgery indication (glenoid labrum is disrupted)
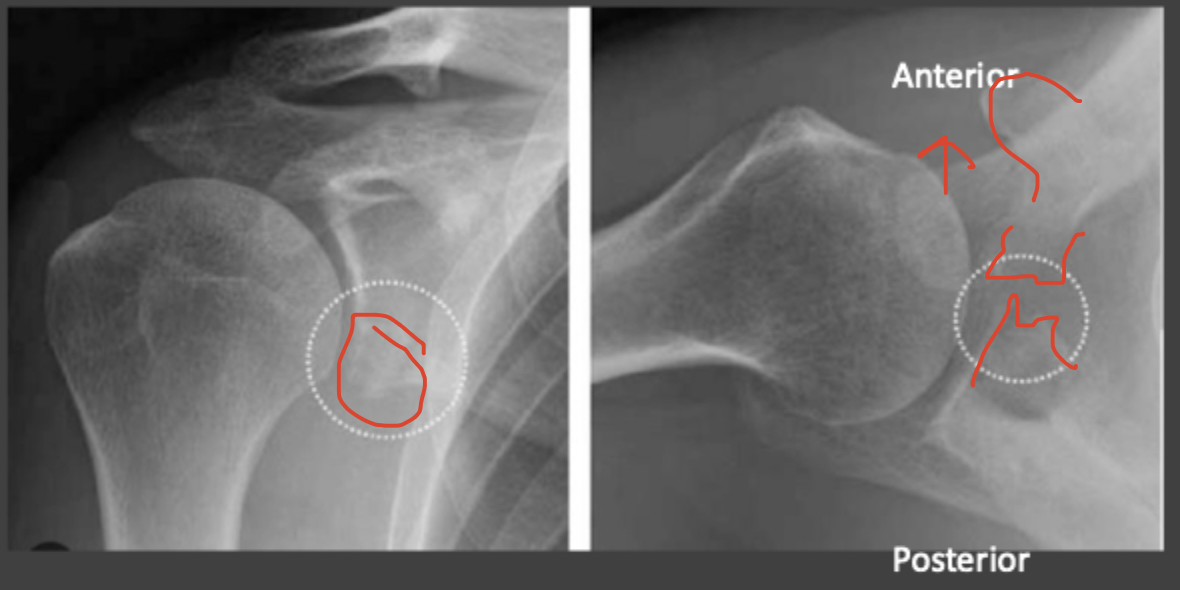
Hill-sachs lesions
Cortical depression in the posterolateral head of the humerus that results from a forceful impaction of the humeral head against the glenoid rim when the shoulder is dislocated anteriorly

midshaft (80%), Lateral/distal (15%), Medial proximal (5%)
Tell me about the anatomy of the clavicle
MVC, MCC, bike injuries (direct trauma to shoulder), direct shoulder to shoulder blow
MOI for clavicle fractures
Skin tenting, r/o brachial plexus injury
Clavicle fracture physical exam findings
non-op (high union rate), associated with high energy impacts to thoracic chest, CT scan to eval neurovascular structures and SC joint
Tell me about medial clavicle fractures

non-op (unless open or skin tenting), FOOSH injuries, treat with sling or figure of 8 brace (3-4 month recovery)
Tell me about mid-shaft clavicle fractures

fall onto lateral shoulder, Most treated non-op (depends on NEER classification), higher risk of non-union, Operatively treated with a hook plate
Tell me about distal clavicle fractures
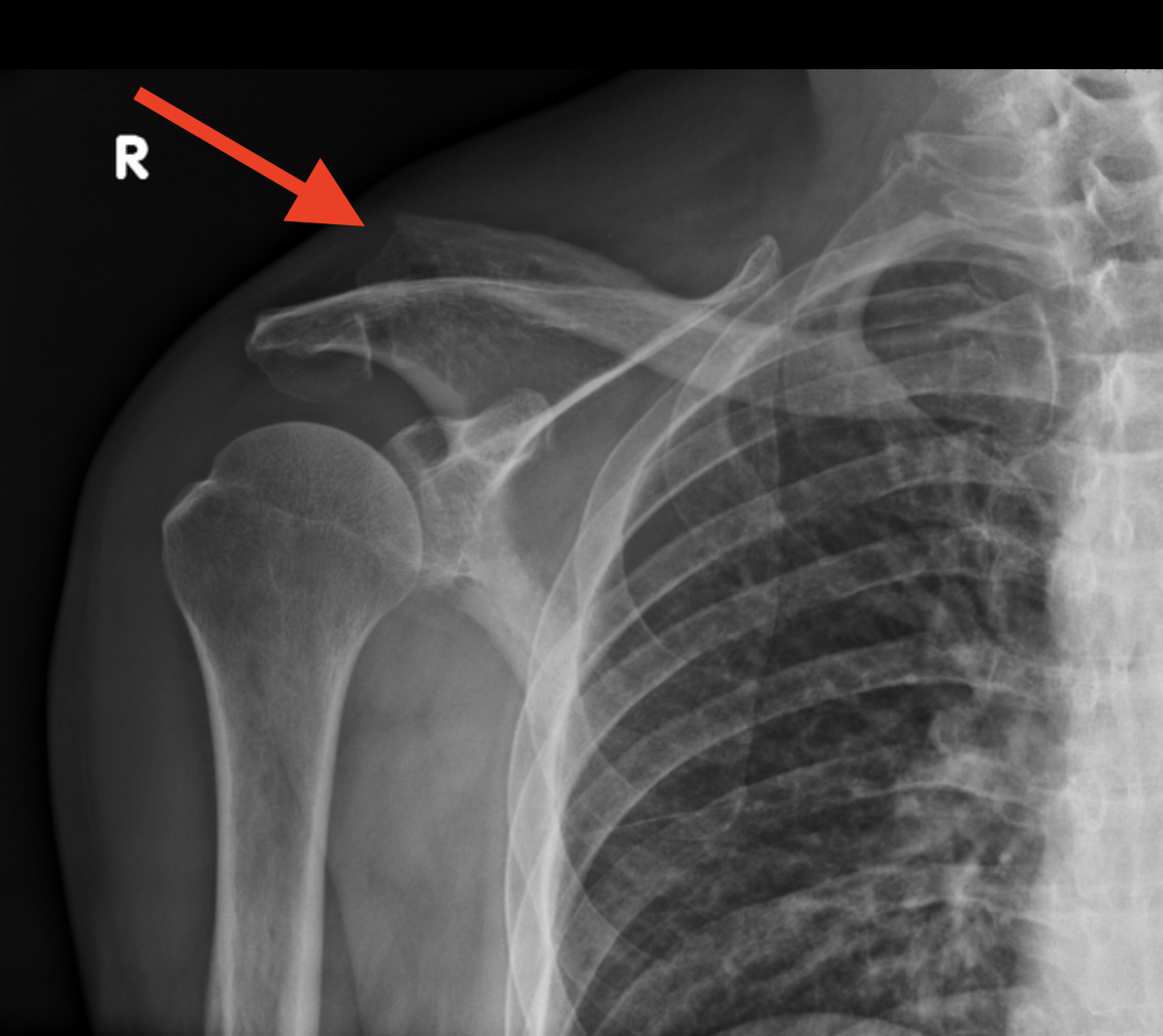
Proximal humerus fracture
What type of fracture is most common in elderly women with osteoporosis and is associated with low energy injuries (fall from standing, FOOSH)
axillary (45% - surgical neck sites)
What nerve are we worried about with proximal humerus fracture
surgical neck (2-part are most common), anatomic neck, greater tuberosity, lesser tuberosity
Anatomical location of Proximal humerus fracture (normal xray)
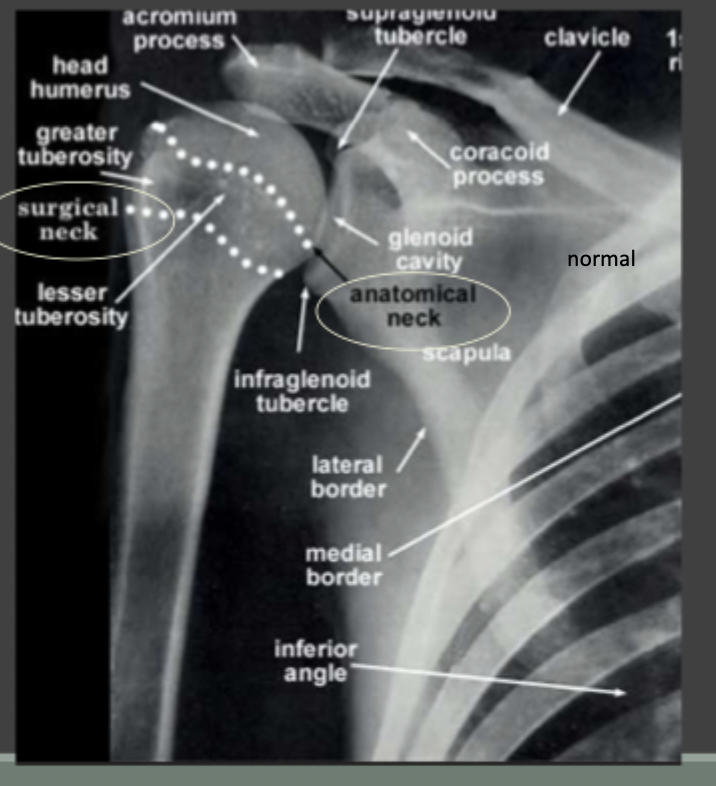
age, fracture type, displacement, bone quality, dominance, medical condition, concurrent injuries
While 85% of Proximal humerus fracture are non-op, this depends on
sling while preserving ROM
How are you managing this - in most cases?
