Clinical and communication skills
1/224
Earn XP
Description and Tags
Veterinary nursing
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
225 Terms
Why is it important to communicate?
Building trust, Accurate diagnosis, client education, emotional support
What are the 5 key skills when communicating?
Active listening, Clarity and simplicity, empathy, non-verbal communication, and questioning techniques
What are the 3 challenges when communicating in the veterinary practice?
Emotional situations, Time constraints, cultural differences
How do we improve veterinary communication in practice?
Training and workshops, feedback and reflection, technology (like emails)
Why is effective communication essential?
For providing high-quality care and ensuring positive outcome for pets and owners
What can a nurse do during a consultation to be an effective communicator?
Active listening, clear explanations, body language, open questions
What is verbal communication?
Use of spoken workds to convey messages
Occur face to face, phone calls, video conferences, public speaking
Requires clarity, active istening and appropriate responses to ensure message is understood as intended
What is tone of voice, and how can we use it in practice?
Involves voice volume, emphasis on words and the emotion that you communicate
it can change what is said to client and how clients interprets the information
What are some non-verbal communication components?
Facial movements and expression (and micro expressions)
Gaze and eye contact
Head movements
Body movements and posture
Proximity
Interpersonal touch
Voice or paralinguistic features
Personal appearance (clean clothes, neat hair, clean hands etc.)
Environmental cues
Time
Why do we use non-verbal communication?
Convey emotional states
Convey feelings towards another person
Can support or contradict the verbal communication
Give the receiver cues about what is being communicated
Adds meaning to verbal communication
Substitute for language when speech not possible
Regulatory function
What are the 2 types of listening?
Passive and active listening
What are some barriers to effective communications?
Client no understanding or misunderstanding, medical terms, time constraints, lack of accessibility, clients’ acceptance of medical advice, difficult clients, client impairments, language barriers, cultural differences
What are the impacts of communication barriers?
Quality of care, client satisfaction
How can we address communication barriers?
Using clear, non-technical language, giving enough consultation time, accessible for follow-up, collaborative environment, building strong relationships
Why do we use communication models?
To structure our client consultations
What is an example of a communication model?
Calgary-Cambridge model
What are the 5 steps to the Calgary-Cambridge model
Initiating the session
Gathering Information
Physical examination
Explanation and planning
Closing the session
What do we do in step one of the Calgary-Cambridge model?
- Preparation
- review patient history and reason for visit and a welcoming environment.
- Building rapport - greet the client and patient warmly, established through small talk (ice breaker, showing an interest to the client)
- Understanding the client perspective - Ask open ended questions to understand concerns and expectations. This encourages clients to open up, tell a story, discuss issues, can get unexpected information. Close questions are yes/no answers, easier to control, can make client feel threatened. Other question include: reflective, probing questions.
What do we do in step two of the Calgary-Cambridge model?
- Biomedical perspective
- ask specific questions about animals symptoms, behaviour and medical history
- Client experiences
- Explore client observations and concerns
- Contextual information
- Gather information about animals environment, diet, lifestyle
What do we do in step three of the Calgary-Cambridge model?
-Integration with communication
- Explain each step of the examination to the client, Use layman's terms to describe findings. Context to what is happening and normal
- Nonverbal communication
- Maintain eye contact and use appropriate body language, Show empathy and attentiveness
What do we do in step four of the Calgary-Cambridge model?
- Sharing findings
- Summarize the results of the examination clearly, Use visual aids if necessary
- Decision-making partnership
- Discuss treatment options and involve the client in decision-making, Address any questions or concerns the client may have
What do we do in step five of the Calgary-Cambridge model?
- Summarising the plan
- Recap the agreed-upon treatment plan and next steps
- Ensuring understanding
- Ask the client to repeat key points to confirm understanding
- Building long-term relationships
- Schedule follow-up appointments and provide contact information for further questions
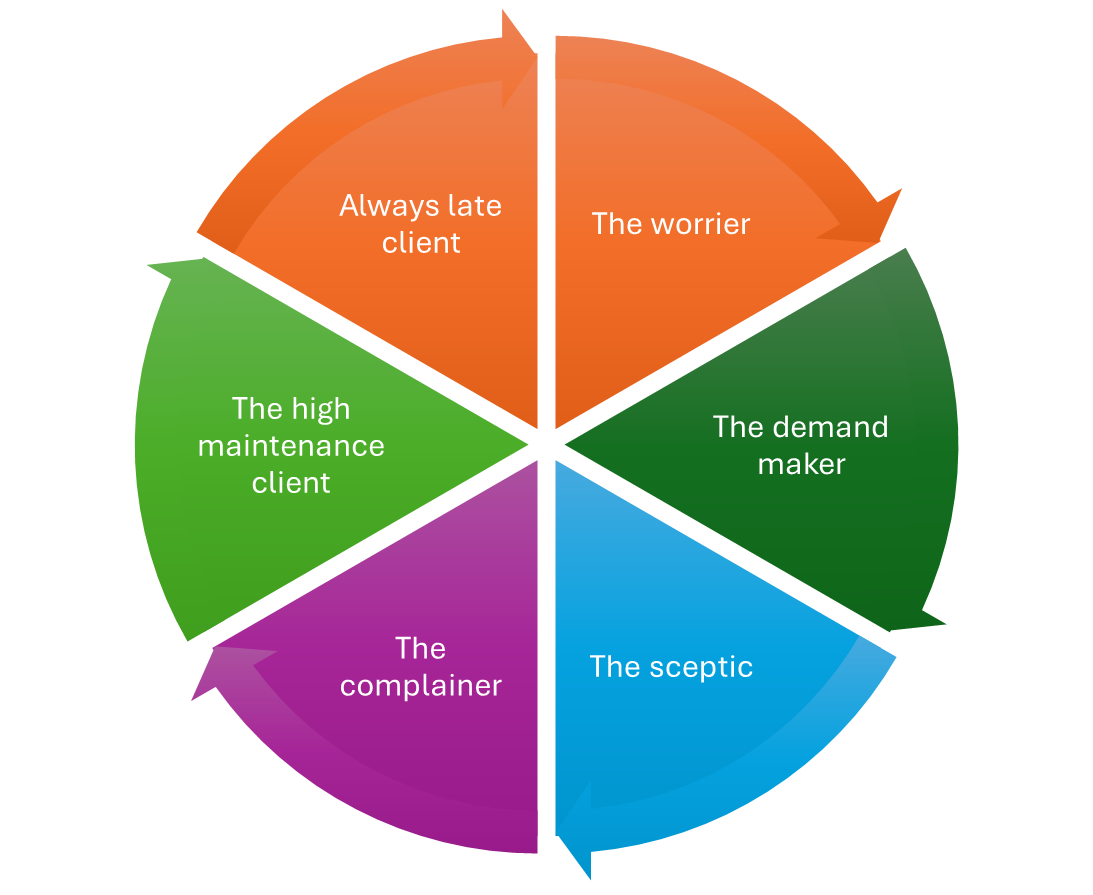
What are the 6 types of clients?
Worrier, Demand maker, sceptic, complainer, high maintenance client, always late client
What is a Human companion animal bond (HCAB)?
A mutually beneficial relationship between people and their animals.
What are the benefits of the human companion animal bond (HCAB)?
Improve mood, reduce depression
Lower blood pressure
Lower cholesterol levels
Lower the risk of a heart attack
Motivate and encourage exercise
Reduce and prevent stress
Help to prevent disease
Increase self-esteem and sense of personal competence
Lessen loneliness, encourage and enable socialisation
Provide a source of social support
Provide an unconditional acceptance and warmth
Boost the immune system
Decrease the number of visits to your GP
Act as a health warning; recently, dogs have been known to detect and identify certain cancers
What circumstances can lead to the loss of pets?
Acute illness
Life limiting condition
Euthanasia
Accidental death
Human illness
Rehoming pet
Moving abroad
Straying
Theft
Behaviour
Imprisonment
Divorce/separation
Forced to give up a pet
Mandatory euthanasia – dangerous dog
What losses are associated with pet bereavement?
Psychological loss (companionship, feeling needed and loved, fun)
Social loss (social conversation, reason to get up and go out, security)
Physical loss (opportunities/motivation to exercise)
Why do clients need support during the loss of a pet?
Pet loss is largely unrecognised as a loss in the UK
No compassionate leave
No tradition of community support
Not universally experienced, understood or recognised
Experiencing grief and mourning the death of a pet may be perceived by some people as ‘trivial’ or ‘ridiculous’
Often alone with their grief
What are the 5 stages of grief?
Denial, Anger, Bargaining, Depression, Acceptance
What happens in the denial stage of grief?
- Individual refuses to accept their loss or news of impending loss
- Denying the truth
- Demanding 2nd opinion, internet research, disappear from surgery
What happens in the anger stage of grief?
- Overwhelmingly angry, anger directed at vet, themselves, relatives/friends, medical community
- Rarely rational but overwhelming and consuming
- Physical, verbal, irrational
What happens in the Bargaining stage of greif?
-'If you take away the pain, then I will.....'
- The individual may beg for their pets life in exchange for whatever price such as bargain
- Money, prayer, time
What happens in the depression stage of grief?
- Individual begins to realise that there situation is irrevocable
- Must continue to live without the presence of their pet in their lives
- Feel sad, anxious, regret, guilt
- Apologising to pet, needing support, become withdrawn
What happens in the acceptance stage of grief?
- Accepting that their pet has limited time
- Acknowledging the fact that their pet is not returning
What is anticipatory grief?
Grieving that begins BEFORE that actual loss
A known life limiting condition - lymphoma, renal disease, heart disease
Type of grief requires provision of pre-euthanasia bereavement care
What is responsibility grief?
Veterinary euthanasia results in a distinct category of grief
Owners have actual personal responsibility for the death of their pet by euthanasia
This may result in feelings of guilt, self blame and doubt
How can we as VN respond to responsibility grief?
RVN continuing care clinics (palliative care, pre-euthanasia)
Involvement & empowerment of owner in palliative treatment and care of terminally ill patient
QOL assessment – include owners
Do not rush clients into euthanasia decision making
Choices & options to be explored e.g. location, after death body-care
Validation of euthanasia decision
Allow opportunities for discussion, questions
What is a Quality of Life (QOL) assessment?
An assessment that measures an individual’s overall well-being mentally and physically
What things get assessed in Quality of life assessment?
Hurt, Hunger, Hydration, Hygiene, Happiness, Mobility, More good days than bad
What are some reasons for euthanasia?
Terminal illness, palliative care is insufficient, behaviour/aggression, financial, unable to rehome
What are somthings’s to remember in the euthanasia process?
You need IV access, time, quite environment, give client personal space, provide option for linking items
How can we support our client in times of euthanasia?
Sensitive communication, show empathy, give client time to kink, speak slow, make procedure goes smoothly
What are some after-body care options?
Communal and individual cremation, burial at home or pet cemetery
What linking items can we offer to clients?
Smally amount of fur, collar, clay paw mould/ink footprint
What post euthanasia support can we offer?
Pet bereavement support (Blue Cross), Samaritans, contact number for pet loss group (trained counsellor), self and team care
What drug do we usually inject an animal with in the euthanasia process?
Pentobarbitone
Why do we see twitching or hear gasps of air after the euthanasia process after the injection is administered?
It’s the reflexes as the nervous system shuts down. They are NOT signs of life
What is rigor mortis?
It can start 10 minutes after death or a couple hours after. Its where the body goes stiff
What is SPIKEs model of communication around euthanasia?
Setting, Perspective, Invitation, Knowledge, Empathise, Summarise
What is compassion fatigue?
Is a state of emotional and physical exhaustion cause by continuous exposure to suffering
How does compassion fatigue develop?
Repeated exposure
Emotional investment
Cumulative stress
Lack of recovery time
What are the signs and symptoms of compassion fatigue?
Emotional symptoms: Feeling numb, detached, irritable, overly emotional
Cognitive Symptoms: Difficulty concentrating, decision-making challenges
Physical Symptoms: Fatigue, headaches, digestive issues
Behavioural Changes: Avoiding euthanasia cases, withdrawing from colleagues, decreased job satisfaction
What is moral stress?
It occurs when you know the ethically "right" things to do but feel powerless to act due to external constraints.
Unlike general stress, moral stress is deeply tied to ethical dilemmas and can create lasting emotional turmoil.
What is the purpose of an admit appointment?
Confirm purpose of admission
Check relevant history
Pre-admission examination of pet
Discuss what is going to happen
Discuss potential risks
Obtain consent for planned procedure
Who can admit patients?
Under the RCVS guidance, it would be the veterinary surgeon, but it can be delegated to someone else who is suitably trained and has sufficient knowledge of the procedure or treatment and understands the risks involved
Who can give consent for a procedure?
It can be given by the owner or an agent (acting on behalf of the owner)
Consent can be given from 16 years old, but they can’t enter a binding contract under 18 meaning they would not be liable for any fees
What is the purpose of discharging appointment?
To return the patient to the care of their owner
To advise the owner on post-procedure monitoring
To advise the owner on post-procedure care
To advise the owner of any prescribed medications and their use
To advise the owner of followup appointments needed
To advise the owner what to do in the event of any concerns including out of hours
What guidance do the RCVS give on discharging patients?
Discharging animals should be in place for on-duty staff
Plan the date and time of discharge early
Identify whether the patient has simple or complex discharge needs and consider how these will be met
Review the clinical management plan regularly, take any necessary action and update this towards the discharge date.
Coordinate the discharge process through effective leadership and handover responsibilities
Confirm that clients have been provided with the necessary information on discharge
Confirm that clients have been given any required medicines or items (e.g. collars, bandages) on discharge
What wound care instructions would you give an owner after a procedure?
Prevent interference with the wound. Wear a cone collar, inflatable collar or protective bodysuit while the wound heals (approximately around 10 days). Most animals can eat/drink fine with these on, but may need to remove and replace immediately after
Check wound a few times a day, looking for redness, swelling, discharge, tight or loose/missing sutures. It might be worth showing owner wound so they know what it looks like and what changes to look for.
When you bring the patient through, if possible show the client what the wound looks like now so they have something to compare to.
No cleaning or applying any creams to the wound unless advised by the vet
What bandage care instructions would you give an owner after a procedure?
Check bandage at least once a day, looking for:
Slipping or complete loss of the bandage.
Signs of chewing/scratching at the bandage.
Any wet areas.
Any bad smell or leaking fluid.
Rubbing of the edges of the bandage on your pet’s skin.
Swelling of the skin around the bandage
Must be protected from getting wet/dirty - cover bandage if they go outside
Do not try and reapply bandage at home if any issues contact practice
When should you seek immediate veterinary attention after a procedure?
Make sure you are aware of any procedure specific concerns
Extreme tiredness/unable to stand
Low energy for over 48 hours post anastatic
Pain or discomfort - pain management in place i.e. pain relief
Problems toileting
Excessive redness, swelling, bleeding, or discharge around wounds
Vomiting- more than 2 episodes in 24 hours
Diarrhoea- more than 2 episodes in 24 hours
Refusing to eat for over 24 hours (dogs and cats)
What are some examples of non-surgical procedures?
Blood sample
Re-dessing
Vaccinations
IV caffiter
Nail clip
X-rays
Skin scapes
Urine sample
Consults/check-ups
What should you do before handling a patient?
Secure room
Transport all patients safely and securely
Muzzles and handling restraints - check previous notes
Assistant availability?
How long should an animal fast for for a fasting blood sample?
8-12 hours pre sampling
Why do we do fasting blood samples (what does it reduce)?
This reduces the risk of samples becoming lipemic - fat layer, which could affect the results
What are some examples of blood tests might an animal might need to be fed for?
bile acid stimulation, glucose levels
How would we prepare the site for a blood sample?
Clip sample site
Use of 'hibiscrub' as a skin cleanser, followed by alcohol swap
What are some common sites for blood samples for cats and dogs?
Jugular (neck)
Cephalic (fore limb)
Saphenous (hind limb)
What are some common sites for blood samples for rabbits?
Jugular vein (neck) - more blood volume
Cephalic vein (fore limb) - bigger breeds
Marginal vein (ear) - reserve for IV catheter, easily callaps
Auricular artery (ear) - haulier gas, oxygenated
What equipment do we need for a blood test?
Electric clippers with no. 40 blades
Skin cleanser e.g. chlorhexidene
Gloves
Surgical spirit
Cotton wool
Needle of suitable size (normally a green needle – 21Gx 5/8) smaller needle for rabbits (blue)
Syringe of appropriate size - usually 2 ml
Appropriate blood container - depends on test
What needs to be on the label after a blood test?
Clients name, patients name, date
How do we position a needle on the syringe correctly?
The bevel of the needle should face upwards

What are some methods of collection a urine sample?
Mid-stream collection, manual expression of the bladder, catheterisation, cystocentesis
How does cystocentesis work for a urine sample?
The procedure involves the passage of a needle, through the abdominal wall into the bladder
What are some methods of collect a faecal sample?
Ground collection, litter tray collection, rectal collection
How should we store and preserve a faeces sample?
Containers need to be sterile and airtight, need 2-5g to fill the container, label the container, examine the faeces 2 hours after collection or store at 4 degrees int the fridge to prevent anything developing for 7 days
why do we do bacteriology swabbing?
Bacterial culture is useful to check the antibiotic sensitivity of bacteria eg a chronic ear infection and doing a swab lets us know what bacteria is growing in the cavity, need to make sure 3 days before swab needs to stop antibiotics
How should you prep a patient for a Bacteriology swab?
Antibiotics should have been stopped three days prior to taking the sample
If swabbing a pustule, remove the hair over the site with scissors
Do not perform any skin preparation (Why? - disinfectant will kill the bacteria just needs to be clipped but use scissors not clippers)
Why don’t we perform any skein preparation for a bacteriology swab?
Disinfectant will kill the bacteria, just needs to be clipped, but use scissors, not clippers
What are the laboratory requirements for a sample?
Proper storage (refrigerating) and labelling
Complete and accurate paperwork (lab forms - details of: practice, owner, animal. Where sample was taken from)
Adherence to guidelines to prevent pre-analytical errors (fasting?, little detail for the test to get accurate results)
What are the packaging requirements for a sample?
Protecting handlers and sample integrity (e.g. person packaging it and the person resaving it)
Use of appropriate packaging materials (e.g., slide holders, bubble wrap, absorbent material, paper work doesn't go into the same pocket as sample)
Proper labelling and absorbent materials
posting bag - needs a 'biological substance' and a 'category ...' on it
How can we control the temparture of a sample when sending it off to a lab?
Wet ice for 2–8°C storage (negative - it melts = polystyrene box help with temp control)
Dry ice for -20°C to -80°C storage (safety precautions - burns)
What laws apply to waste management?
Environmental Protection Act 1990
Special Waste Regulations (amended) 1996
Hazardous Waste Regulations 2005
What commercial waste documentation does a practice need and why?
Section 35(5) of the Environmental Protection Act 1990 makes it essential for commercial properties to have evidence on where the waste is going and this needs to be kept for 7 years
What do you need to consider when handling waste?
Protect yourself!!
Have an understanding on the type of waste you are dealing with
Only handle what you have been trained to work with
Wear PPE (this will vary for each type of waste)
Good general/personal hygiene and infection control standards
What are some examples of Non-hazardous waste?
Domestic waste, Offensive waste, Pharmaceuticals, Cadavers (unless they have a notifiable disease)
What colour bin bags do offensive waste go into?
Yellow bag with a black strip in the middle of it
What are some examples of hazardous waste?
Infectious/clinical waste, sharps, cytotoxic and cytostatic waste, photographic/radiographic chemicals
What may offensive waste include?
Faeces, Bedding, clinical materials that are not infectious
What regulation regulates controlled drugs?
Regulated by the Misuse of Drugs Regulations 2001
What colour bag is used for Infectious/ clinical waste?
Yellow bag with a hazard sign
What colour bin do sharps go into that are contaminated with bodily fluids and pharmaceuticals?
Yellow lidded bins
What colour bin do sharps go into that are not contaminated with bodily fluids and pharmaceuticals?
Orange lidded bins
What does cytotoxic mean?
Toxic to cells (kills cells)
What does cytostatic mean?
inhibition of cell growth and multiplication (stop cells growing) - used more
What bins does cytotoxic and cytostatic waste go into?
sharps bin with purple lid
yellow bag with purple stripe or purple bag
What are some consequences of poor waste disposal?
Environmental damage
Infectious / zoonotic diseases
Risk of wildlife health with chemicals
Human injury
Sharps put in plastic bags
Risk of injury from chemicals
Prosecution of organisation and individual
Failure to produce commercial waste documentation, breach of Section 34(5) of the Environmental Protection Act 1990 (£300)
What is the definition of Cleaning?
the physical removal of dirt and organic matter
What is the definition of Disinfection?
the physical or chemical destruction of microorganisms (not all pathogens and spores)
What is the definition of Sterilisation?
the destruction of all microorganisms including bacterial spores (from equipment and surfaces)