PPA Module 2 (Lectures 2.6-2.9)
1/162
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
163 Terms
Catecholamine Synthesis
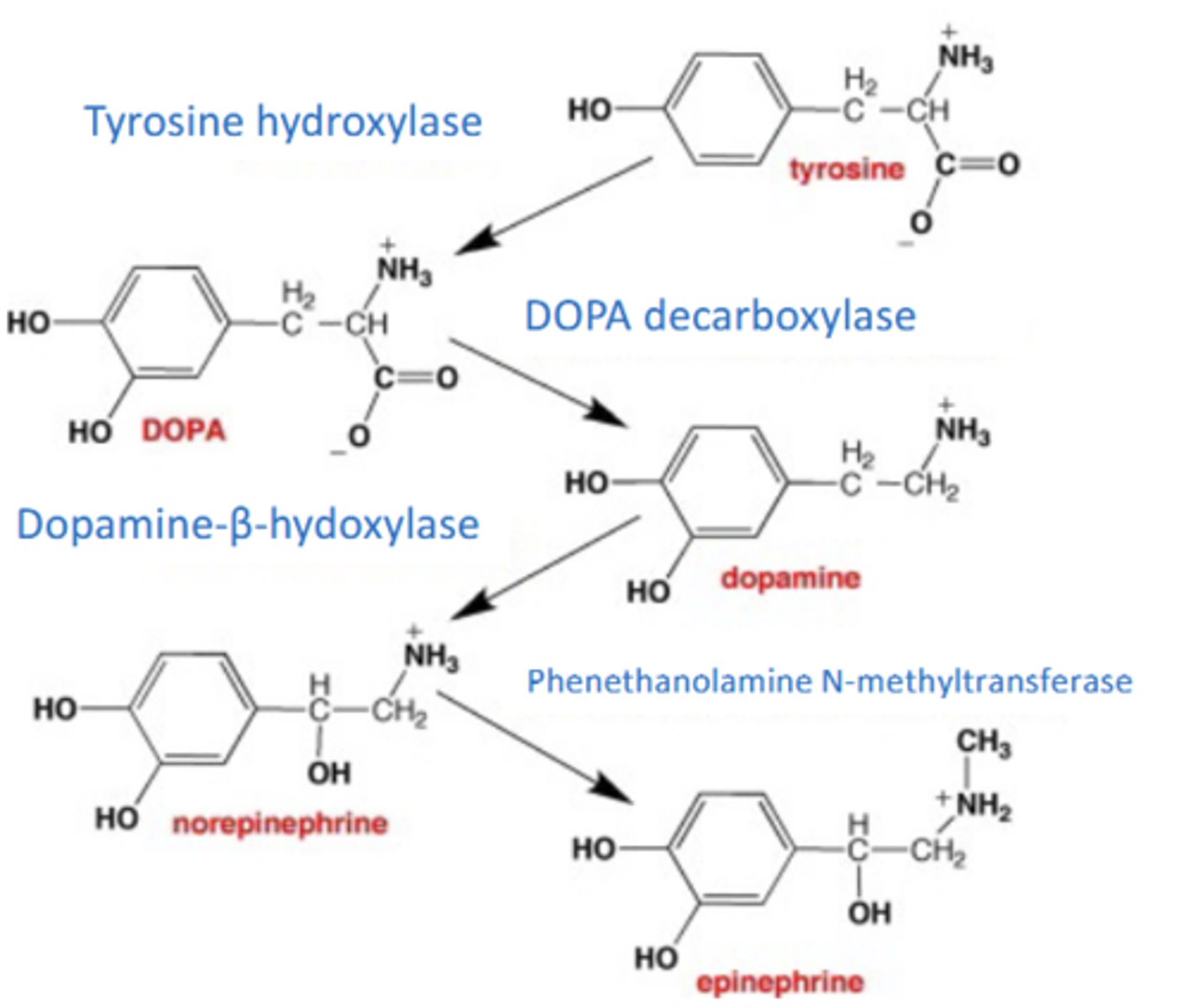
NE Synthesis
Oxidized from dopamine by dopamine β-hydroxylase in cytosol
o Reaction rate limited only by supply of dopamine, coming from a multi-step process
Movement of NE across membranes requires ___________________
Active Cotransport
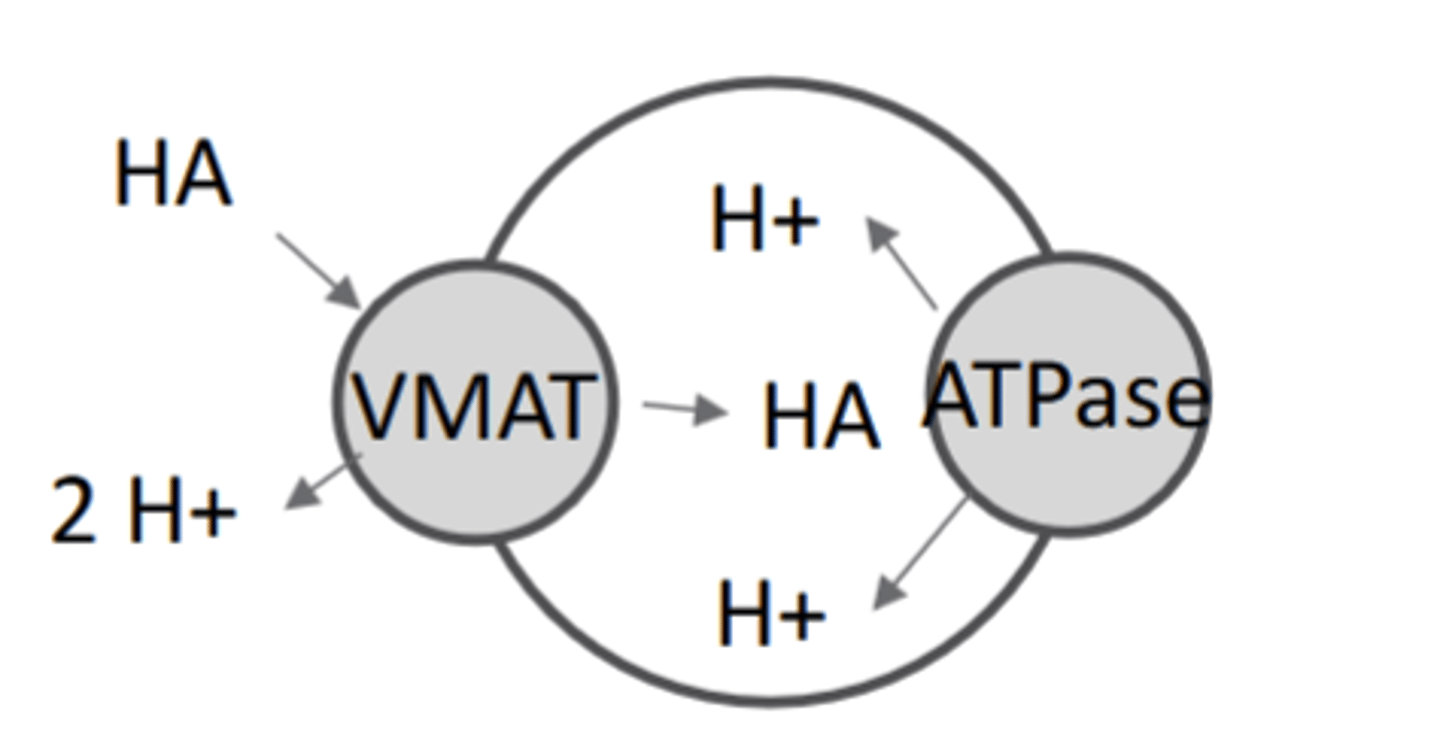
NE is stored in synaptic vesicles by
-vesicular monoamine transporter (VMAT1 or 2)
− Ion co-transport used, exchanging H+ pumped into vesicle by vesicular-ATPase for NE
Reuptake of NE
-Reuptake from the synaptic cleft by the norepinephrine transporter (NET) terminates signaling
~90% recovery. Ion co-transport required, coupling NE entry with influx of 1 Na + + 1 Cl
Key neurotransmitter of the sympathetic nervous system
Epinephrine
EPI synthesis
-Methylation from NE by phenylethanolamine N-methyltransferase (PNMT)
-PNMT found mostly in endocrine cells. Stress indirectly increases EPI synthesis
-PNMT reaction rate limited only by supply of norepinephrine
EPI transport
Transport: EPI storage and reuptake is performed by VMAT and NET as described with NE
NE and EPI are neurotransmitters for _______receptors
Adrenergic (all metabotropic 7-TM GPCR-class receptors)
Alpha 1 Receptors
-apha1A, alpha1B, alpha1D
-Gq
-Adrenergic receptors
-Excitatory
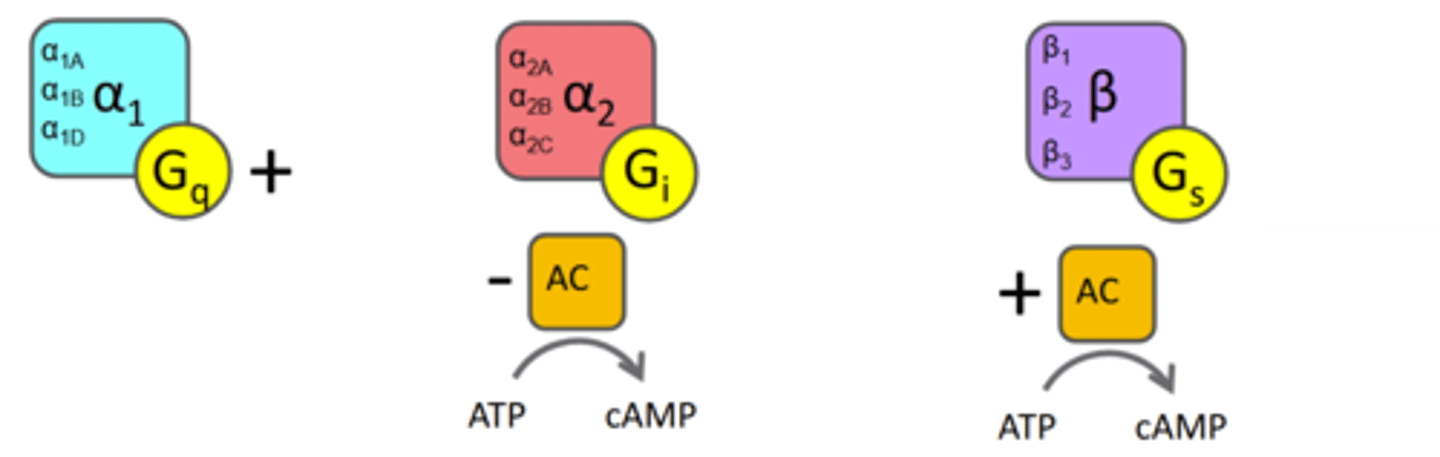
Alpha 2 Receptors
-alpha2A,alpha2B,alpha2C
-Gi
-inhibitory
-dec cAMP
-Adrenergic receptors
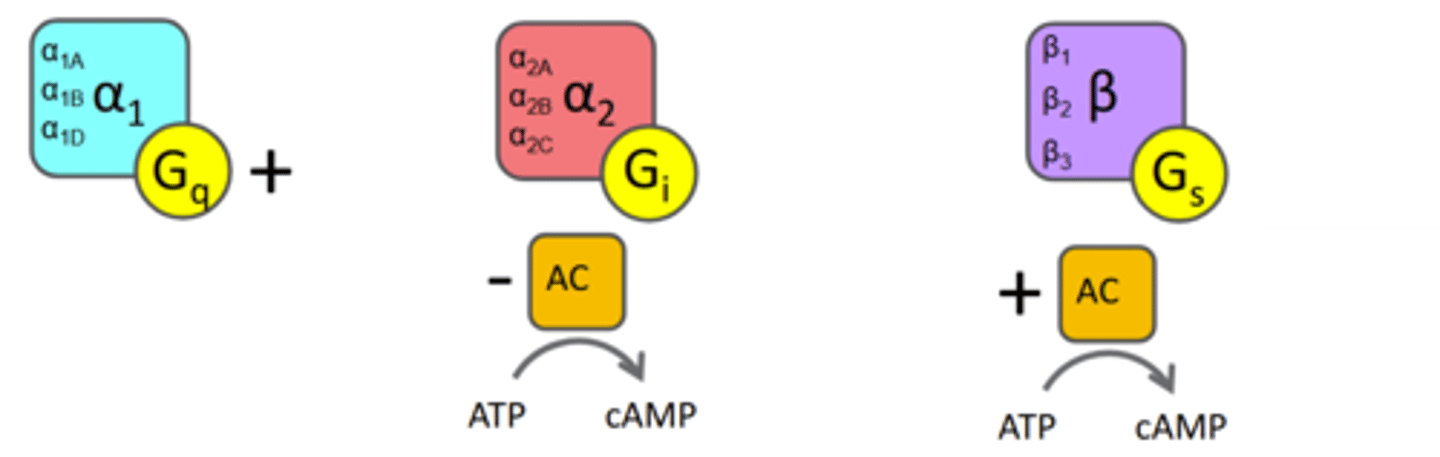
Beta Receptors
-Beta1,Beta2,Beta3
-Excitatory
-Gs
-inc cAMP
-Adrenergic receptors

Alpha 1 Drugs
-Phenylephrine:alpha 1 agonist
-Prazosin: alpha 1 blocker
Alpha 2 Drugs
-Clonidine: alpha 2 agonist
-Yohimbine: alpha 2 antagonist
Beta Drugs
-Isoproternol: beta agonist
-Propranolol: Beta blocker, Beta antagonist
Uptake Inhibitors
block amine transporters to ↑NT, ADHD medication Atomoxetine
False Transmitters
packaged like and replace NT, but weak (or no) receptor affinity (phenylethylamine)
Degredation of NE and EPI
NE, EPI metabolized by monoamine oxidase (MAO) and catechol-O-methyl transferase (COMT)
EPI in CNS located in
medullary reticular formation
NE location in CNS
containing neurons concentrated in two pons-medulla tracts:
1)Locus Coeruleus:
-Regulate blood pressure via α2A centers in brain stem, ↑ baroreceptor reflex
-Project widely in brain, with wide ranging effects!
2) Lateral Tegmentum: Regulate nociceptive input: (analgesia): descending path activates SC interneurons to inhibit pain input
NE action on arousal
NE from the reticular activating system (RAS) activates α2A in the prefrontal cortex
Activation increases attention and focus and enhances sensory processing, increases cognition
NE action on memory
Enhances formation and retrieval of both long-term and working memory
NE action on cognitive performance
Enhances sensory processing, and brain's response time to input
NE action on reward
Effects mixed. Increases substance reward, but α1 activation decreases appetite.
NE action on mood
α2 agonists (e.g., clonidine) reduce anxiety, panic and PTSD. α2 antagonists may
be antidepressant (ex: yohimbine). MAO inhibitors ↑NE+DA: these are established antidepressants
Tyramine
Another tyrosine metabolite, also found in
fermented foods: beer, cheese, sausage, red wine
-Acts as false transmitter (weak "NT")
-MAO inhibitors counter indicated: MAO-I ↑ effect
Phenylephrine
α1 agonist. Decongestant.
Prazosin
α1 blocker; acts as inverse agonist. Treatment for high blood pressure; maybe alcoholism?
Clonidine
α2 agonist. Treatment for high blood pressure, ADHD, anxiety, PTSD; modest analgesic
Yohimbine
α2 antagonist (and others). Possible antidepressant; studied for erectile dysfunction.
Isoproterenol
nonselective β agonist. Treatment for bradycardia; historically used to treat asthma
Propanolol
"beta blocker"; nonselective β antagonist. Treatment for high blood pressure; migraine, anxiety.
Atomoxetine
NET inhibitor, treatment for ADHD.
The only small molecule neurotransmitter not an amino acid or synthesized from one.
Acetylcholine
The major NT at neuromuscular junctions and ANS, acts as CNS NT and neuromodulator
Acteylcholine
Cholinergic agonists
Nicotine
Muscarine
Cholinergic agonist toxic stimulant from Solanaceae
Nicotine
Cholinergic Agonist A convulsant from A. muscaria:
Muscarine
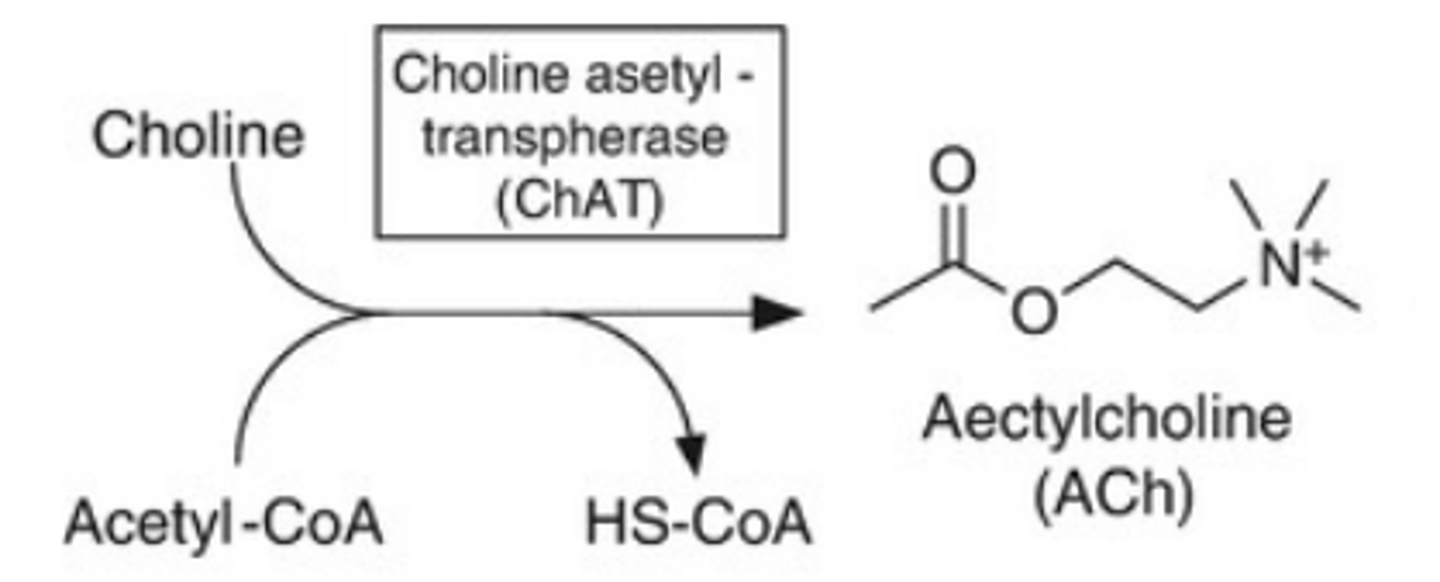
Synthesis of ACh
-acetylation of choline at the -OH catalyzed by choline acetyltransferase (ChAT)
-Consumes Acetyl coenzyme A, a key molecule in fatty acid metabolism + citric acid cycle
-While the only biosynthetic step, the limit on rate is availability of choline
-Choline is obtained primarily from diet. Used in cell membrane synthesis, but N+ charge prevents passage.
-Choline taken up into cell by Na + cotransport via choline transporter (CHT1)
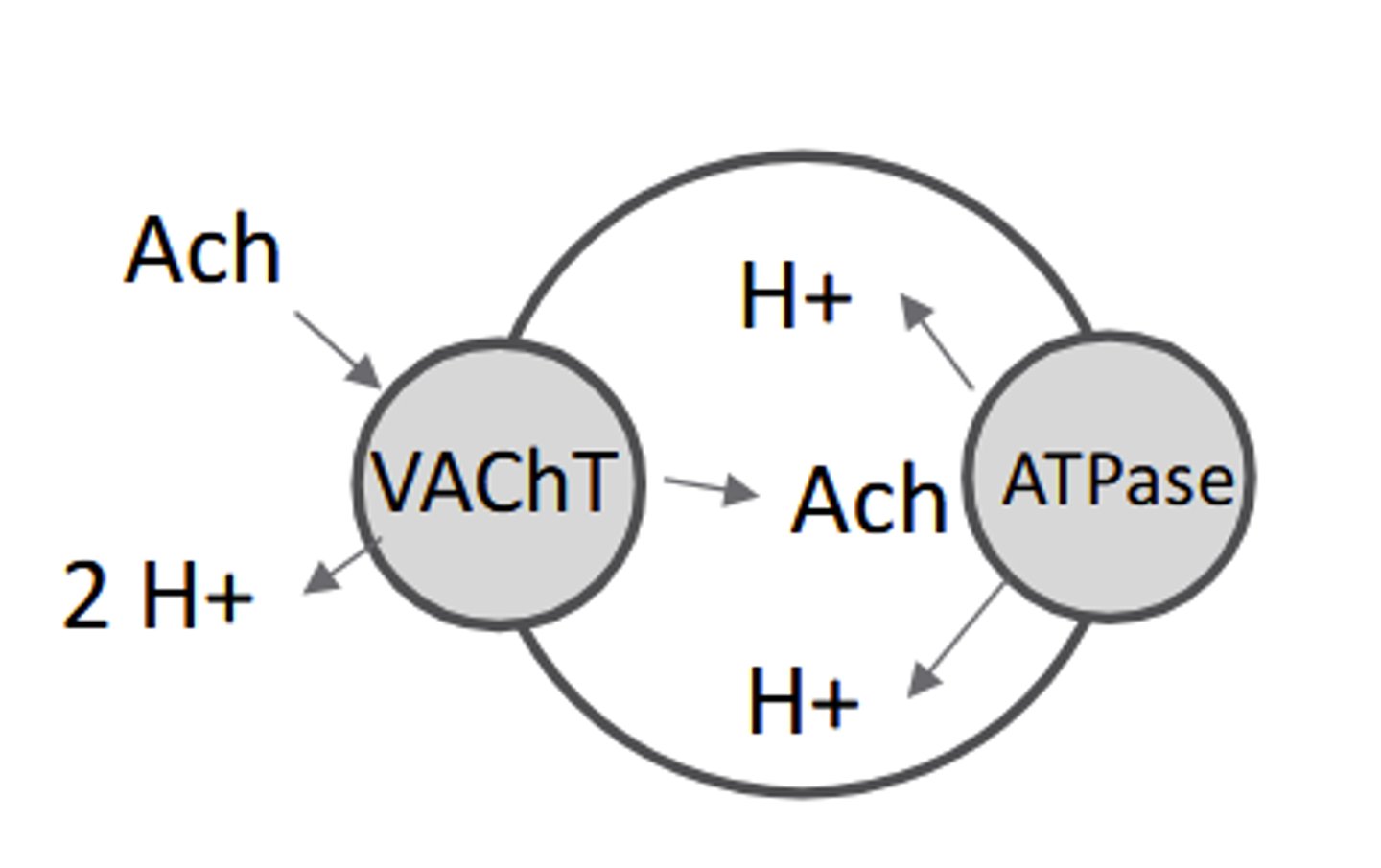
ACh Storage
-Presynaptic ACh stored in vesicles by vesicular acetylcholine transporter(VAChT),
-using ion co-transport to exchange pumped H+ for acetylcholine
ACh Transport
Once released into the synaptic cleft, charged acetylcholine cannot re-enter the
cell, and is NOT transported.
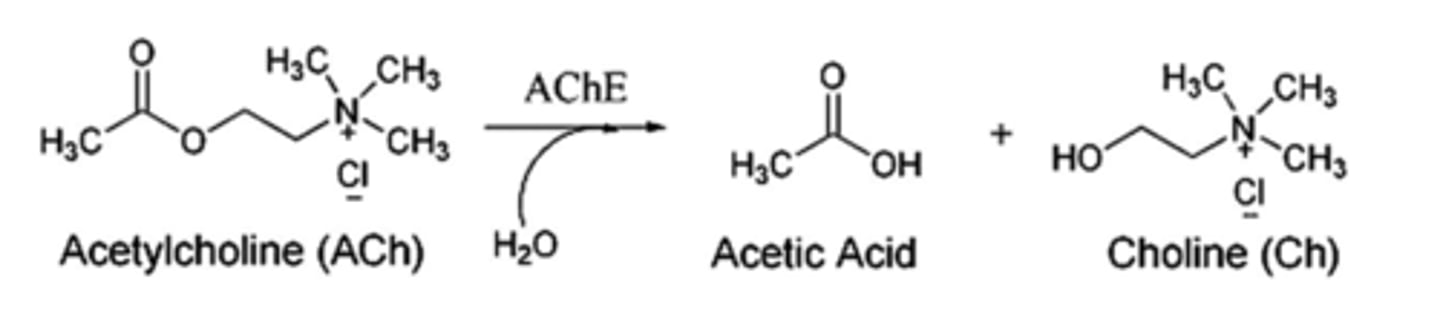
ACh signaling termination
Acetylcholine signaling is terminated by metabolism in the synaptic cleft
Metabolism of ACh
Acetylcholinesterase converts ACh into choline and acetate
-Acetylcholinesterase (AChE) is abundant in synaptic cleft and works extremely fast (< 1msec)
-A number of neurotoxins (Sarin, VX) and pesticides inhibit AChE, causing paralysis + heart failure
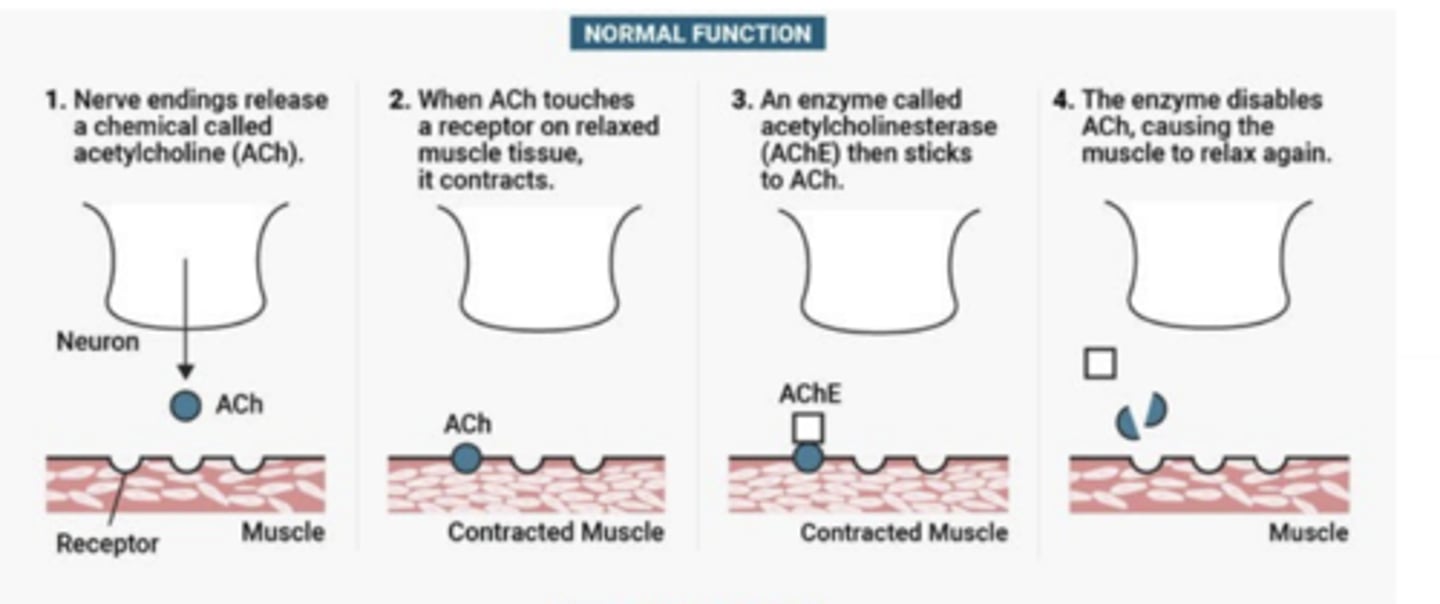
Nerve Agents (normal function)
1)nerve endings release ACh
2)when ACh touches receptor on relaxed muscle tissue it contracts
2)AChE sticks to ACh
4)AChE disables ACh causing muscle to relax
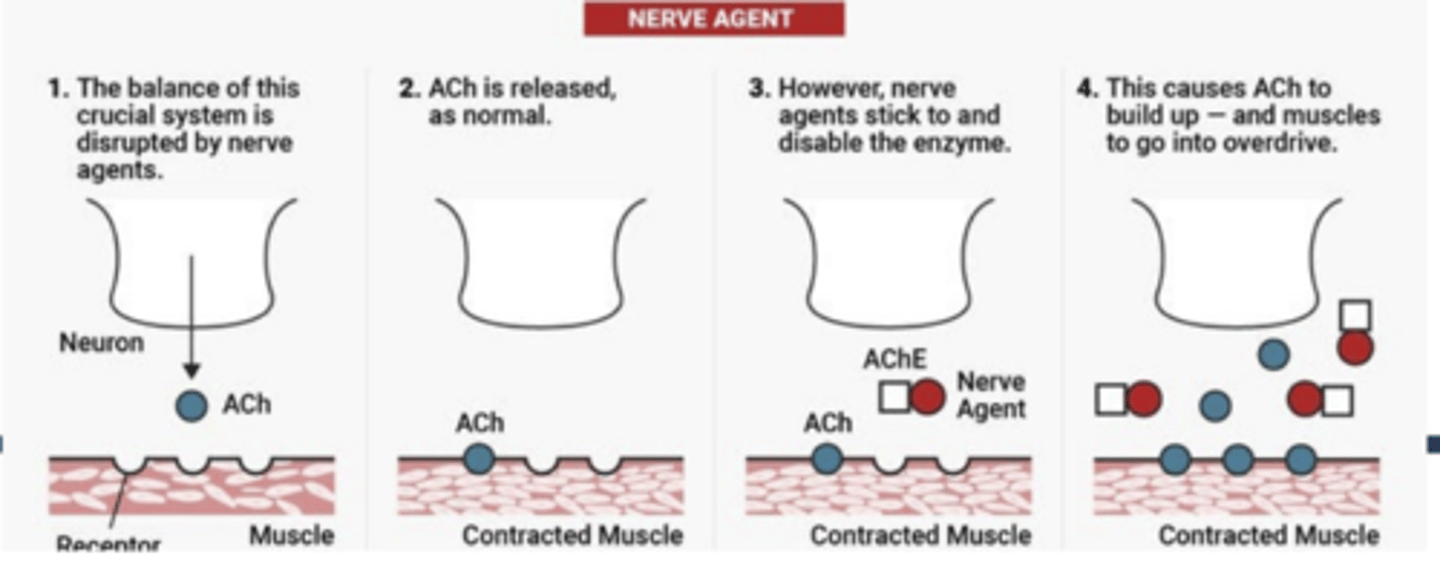
Never Agents
1)nerve agents disrupt balance of ACh system
2)ACh released as normal
3)nerve agents stick to and disable AChE
4)result is ACh build up muscles go into overdrive
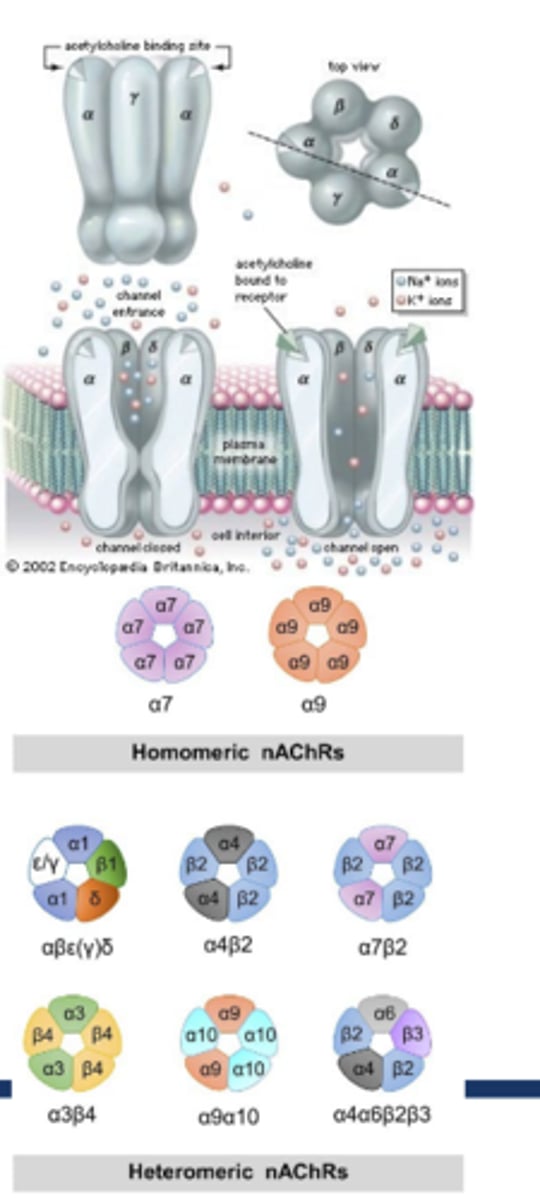
Which Cholingergic Receptor:
-ion channel
-excitatory
-↑Na+ influx,↑K+ efflux; some ↑Ca2+ influx
-Depolarizes very fast (msec)
-Nicotine an agonist
-Composed of 5 subunits forming pentameric channel w/pore
-ACh-gated
-17 subunits known to exist: 10α, 4β, γ, δ, ε
-Brain: ratio typically 2 α + 3 β
-Composition dictates drug affinity, Ca 2+ permeability, kinetics
-Non-selective cation channel, bu
Nicotinic acetylcholine receptors: (nAChR)
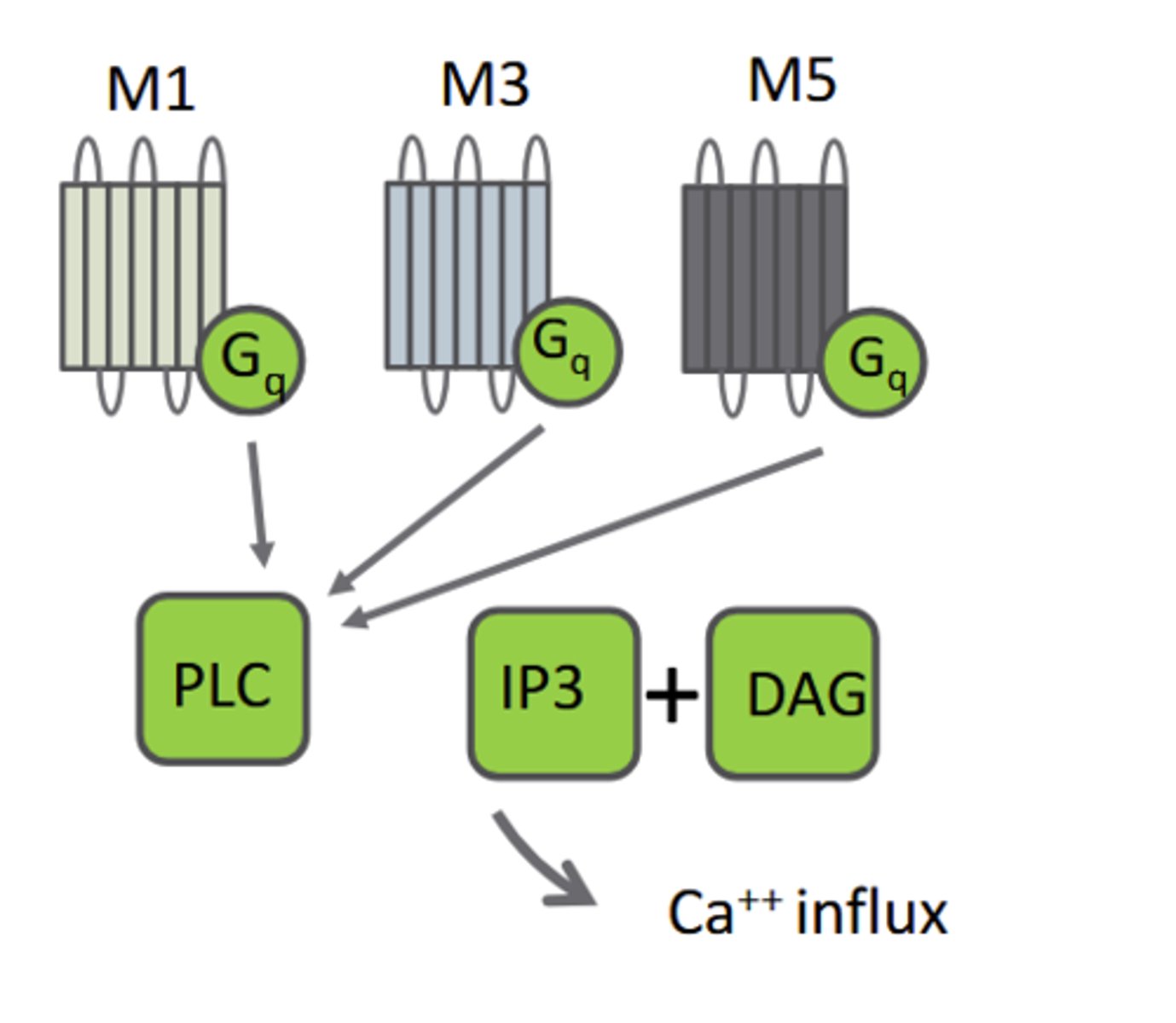
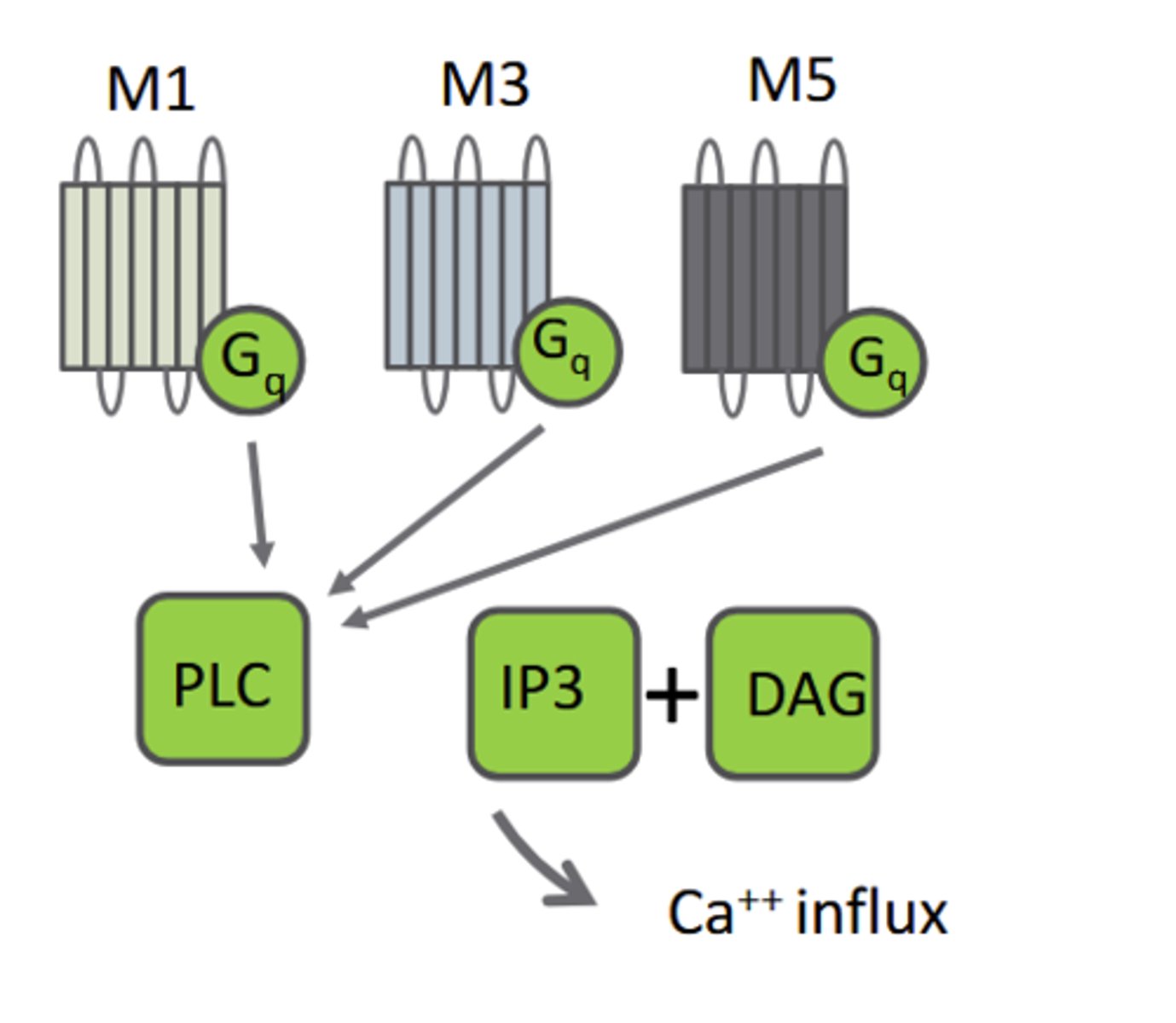
M1 mAChRs
M 1: Excitatory: Gq-linked: ↑PLC, ↑IP3, DAG
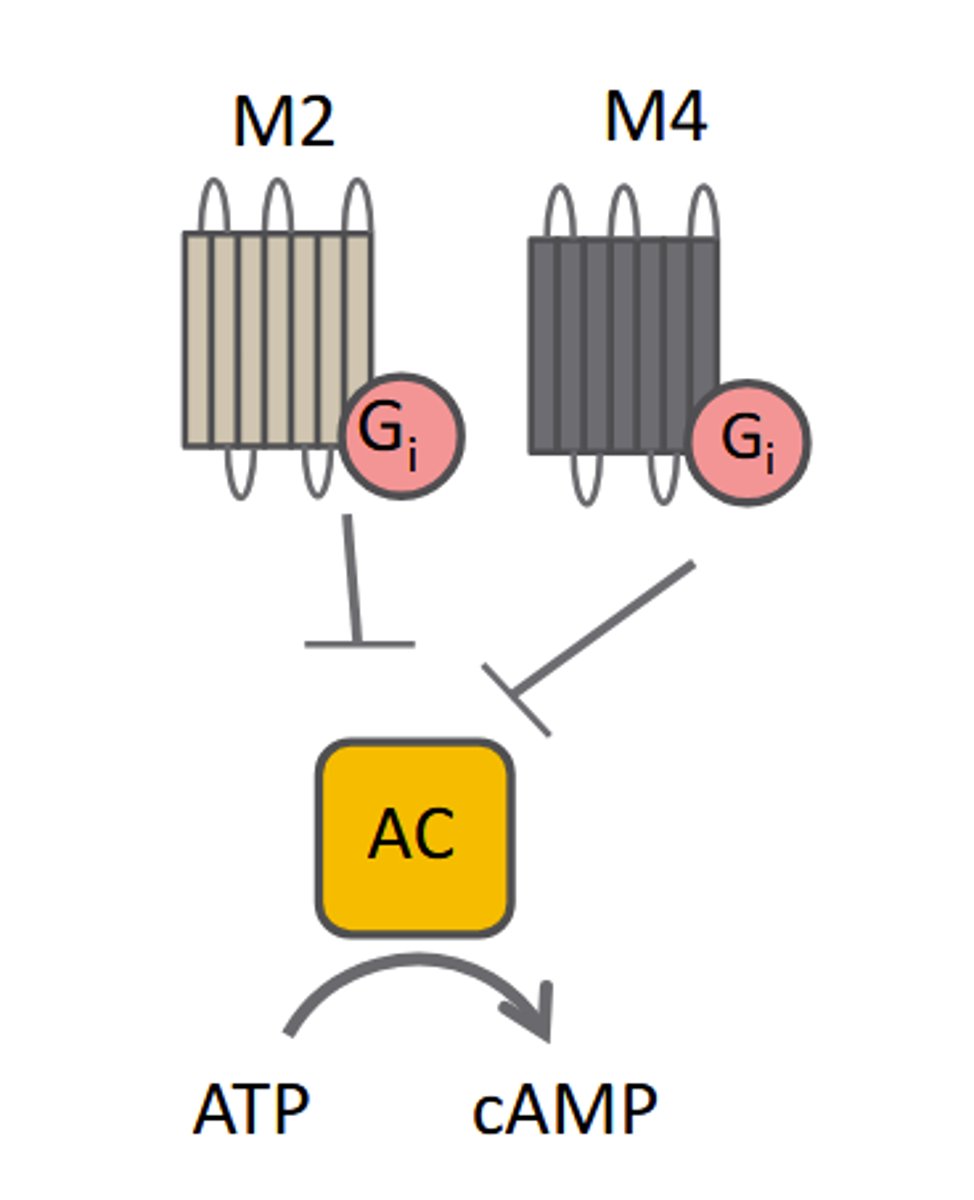
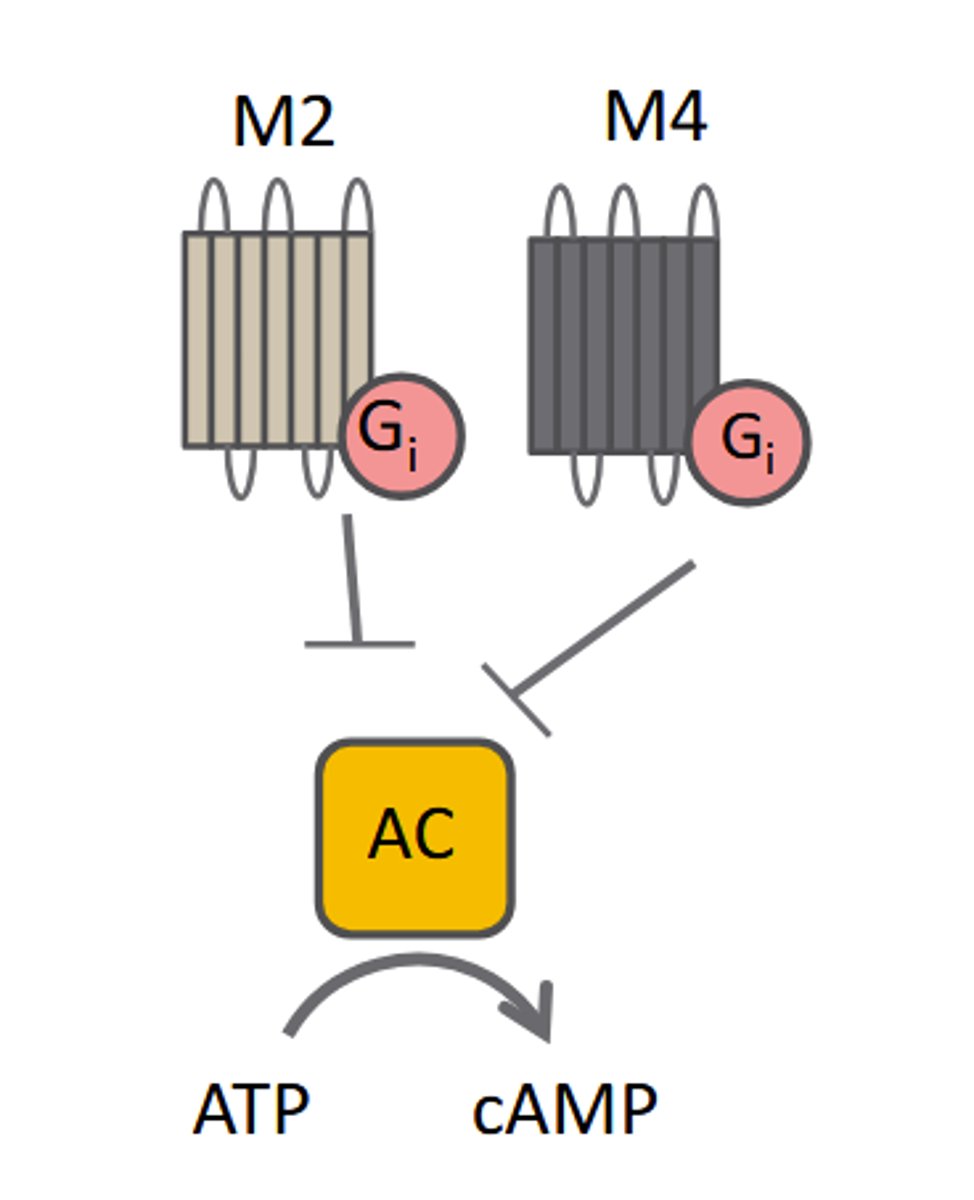
M2 mAChRs
M 2: Inhibitory: Gi-linked: ↓AC, ↓cAMP
M3 mAChRs
M 3: Excitatory: Gq-linked: ↑PLC, ↑IP3, DAG
M4 mAChRs
M 4: Inhibitory: Gi-linked: ↓AC, ↓cAMP
M5 mACHRs
M 5: Excitatory: Gq-linked: ↑PLC, ↑IP3, DAG
Scopolamine
Non-selective mAChR antagonist
Atropine
Non-selective mAChR antagonist
Curare
non-selective nAChR antagonist
Dihydro-β-erythrodine
(α4) 2(β4) 3 antagonist
α-bungarotoxin
Antagonist at (α7) 5 nAChR
Type (α7) 5 (nAChR)
Passes Na +, K+ and Ca2+
Mediates pro-cognitive effect
Type (α4) 2(β4) 3 (nAChR)
Passes Na + and K+ (not Ca2+ )
Mediates rewarding effects of nicotine
hort interneurons in caudate/putamen
basal ganglia
o Interneurons in striatum use Ach; M4+M5 AChR
o Regulate motor output: respond to environment
with established motor responses.
o Inhibited by DA neurons of substantia nigra
o Parkinson's Disease: Loss of DA inhibition
causes excess ACh, producing resting tremors
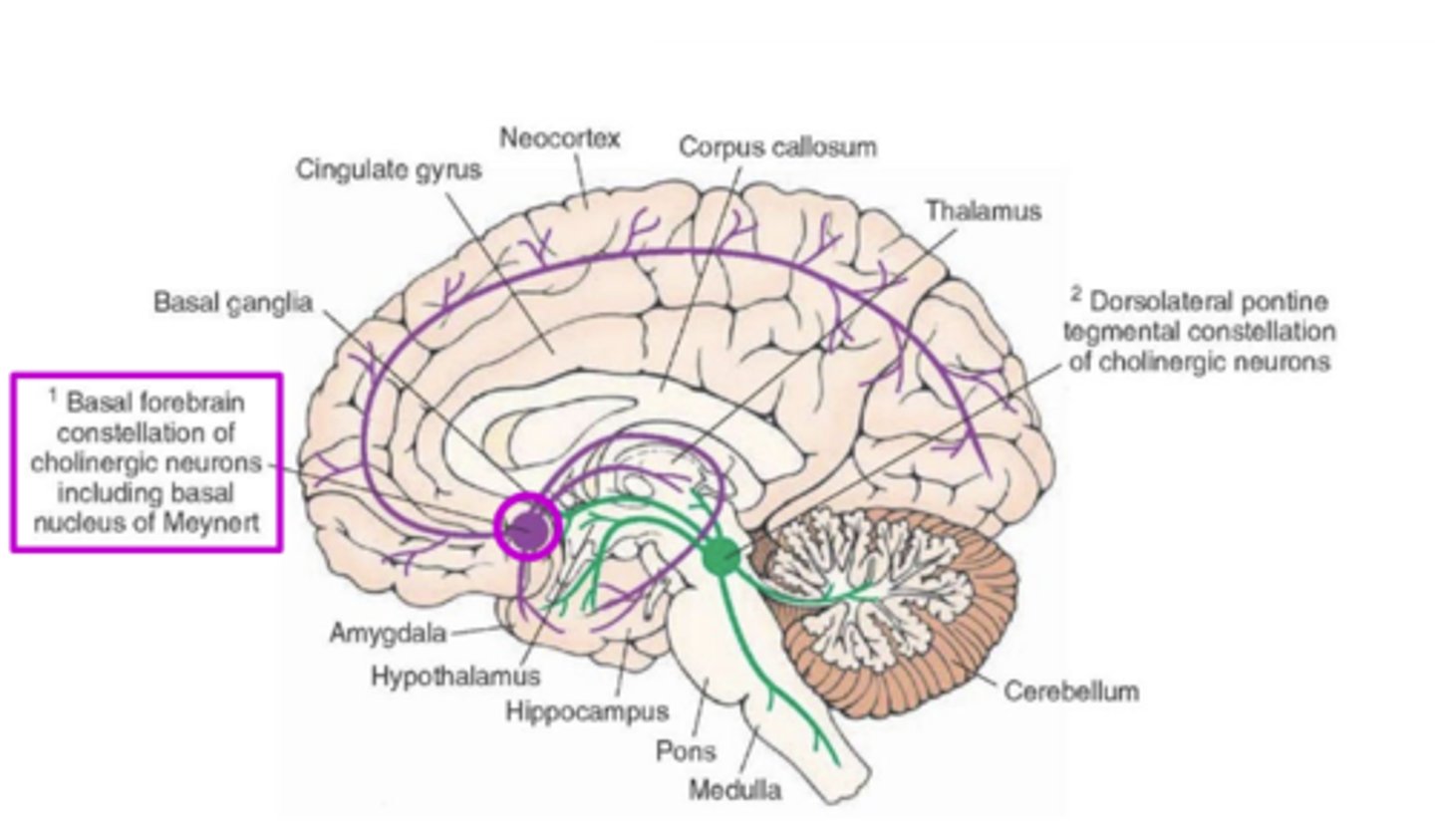
ACh-containing neurons form two major pathways in brain:
1)Pontomesencephalotegmental complex:
2)Basal forebrain:
Which ACh containing neural pathway:
-Cholinergic cell bodies in brain stem
pedunculopontine nucleus + laterodorsal
tegmental nucleus;
-Activity mediated by M1AChR.
-Increases autonomic outflow; increases secretions
-Regulates pain: M2, M4AChR activity ↓ pain through
nociceptor inhibition. AChE inhibitors ↑ACh, ↑ analgesia
Pontomesencephalotegmental complex:
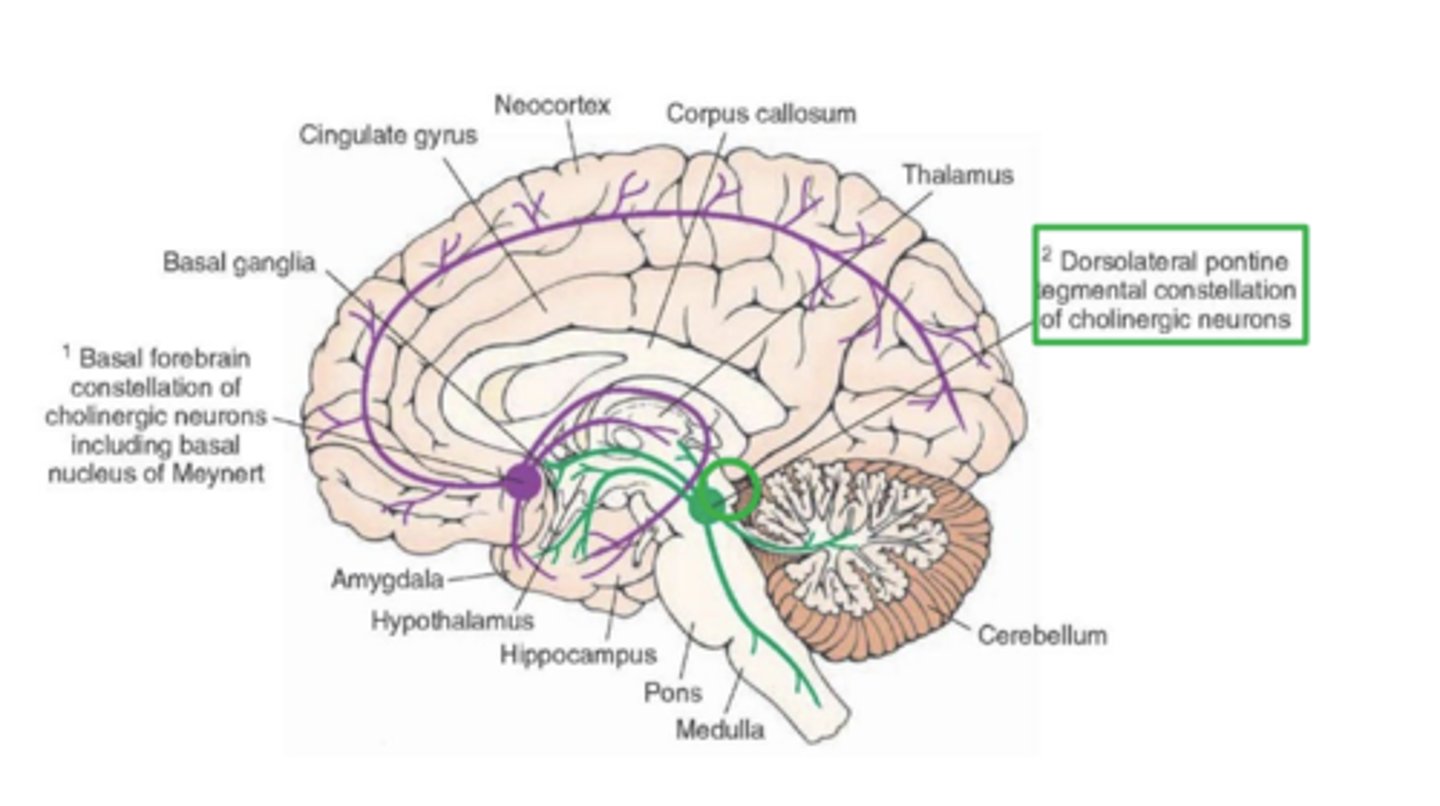
Which ACh containing neural pathway:
-cholinergic cell bodies originate
from basal optic nucleus of Meynert and septal
nucleus.
-Major brain acetylcholine system;
regulates/modulates most system
-Neuromodulation: AChR autoreceptors decrease NT release
-(α4) 2(β4) 3 nAChR on A10-DA path:
mediate nicotine, drug reward
Basal Forebrain
ACh action: Cognition
Activity of M1, M2 receptors in cerebral cortex and hippocampus increase cognitive
performance and improve memory. Basal forebrain output correlated with improved learning and memory
- (α7) 5 nAChR activity associated with improved cognitive performance.
- Scopolamine: antagonizes mAChR in brain, produces delirium and amnesia.
- Alzheimer's disease: Loss of cholinergic neurons a hallmark of AD. Damage and dysfunction of
cholinergic system in brain correlates with the progression of memory deficits.
ACh action: attention
Increase acetylcholine in cortex improves response time and processing of sensory stimuli
ACh action: arousal
Cholinergic systems regulate waking/sleep; ACh promotes REM sleep.
ACh may enhance sensory perception to facilitate waking. Effect may be neuromodulatory in basal forebrain
Nicotine
Agonist for all nicotinic-family acetylcholine receptors. Stimulant, addictive, pro-cognitive?
Scopolamine
Non-selective mAChR antagonist. WHO med. Used to treat motion sickness, nausea, vomiting
Muscarine
Agonist for all muscarinic-family acetylcholine receptors.
Organophosphates/Sarin
AChE inhibitors. Pesticides; deadly poisons.
Atropine
Non-selective mAChR antagonist. WHO med. ↑HR; counteracts AChE inhibitors. Hallucinogen.
Curare
non-selective nAChR antagonist. Weakens skeletal muscles, paralyzing diaphragm; asphyxiation
A major mediator of anaphylaxis and inflammation; mediates gastric acid secretion. (Autocoid)
Histamine
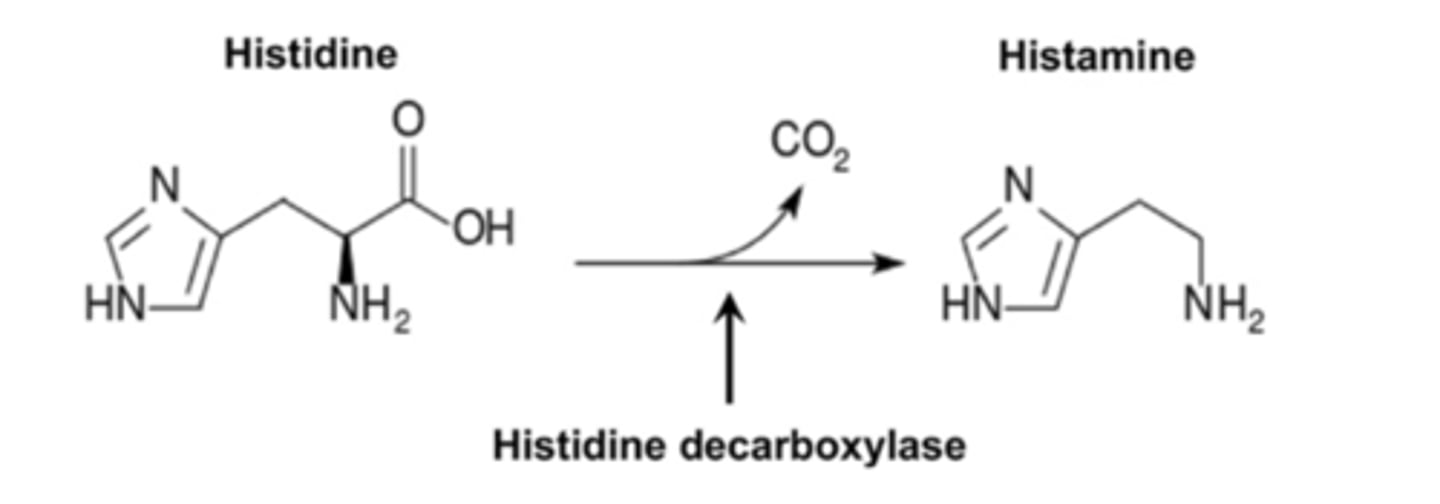
Histamine Synthesis
histamine is formed by decarboxylation of the essential amino acid histidine,
catalyzed by the enzyme L-histidine decarboxylase
A major mediator of anaphylaxis and inflammation; mediates gastric acid secretion also acts as a neurotransmitter in the CNS.
Histamine
Once formed, histamine is either _____ or ______
rapidly stored or rapidly inactivated
Histamine is rich at sites of potential injury, bound in granules of ______ and ____
mast cells and basophils
________ cells of stomach: release histamine to ↑ stomach acid from parietal cells
Enterochromaffin-like Cells
Where is histamine found in the brain
tuberomammillary nucleus of hypothalamus
Histamine is stored in synaptic vesicles by:
Vesicular Monoamine Transporter (VMAT)
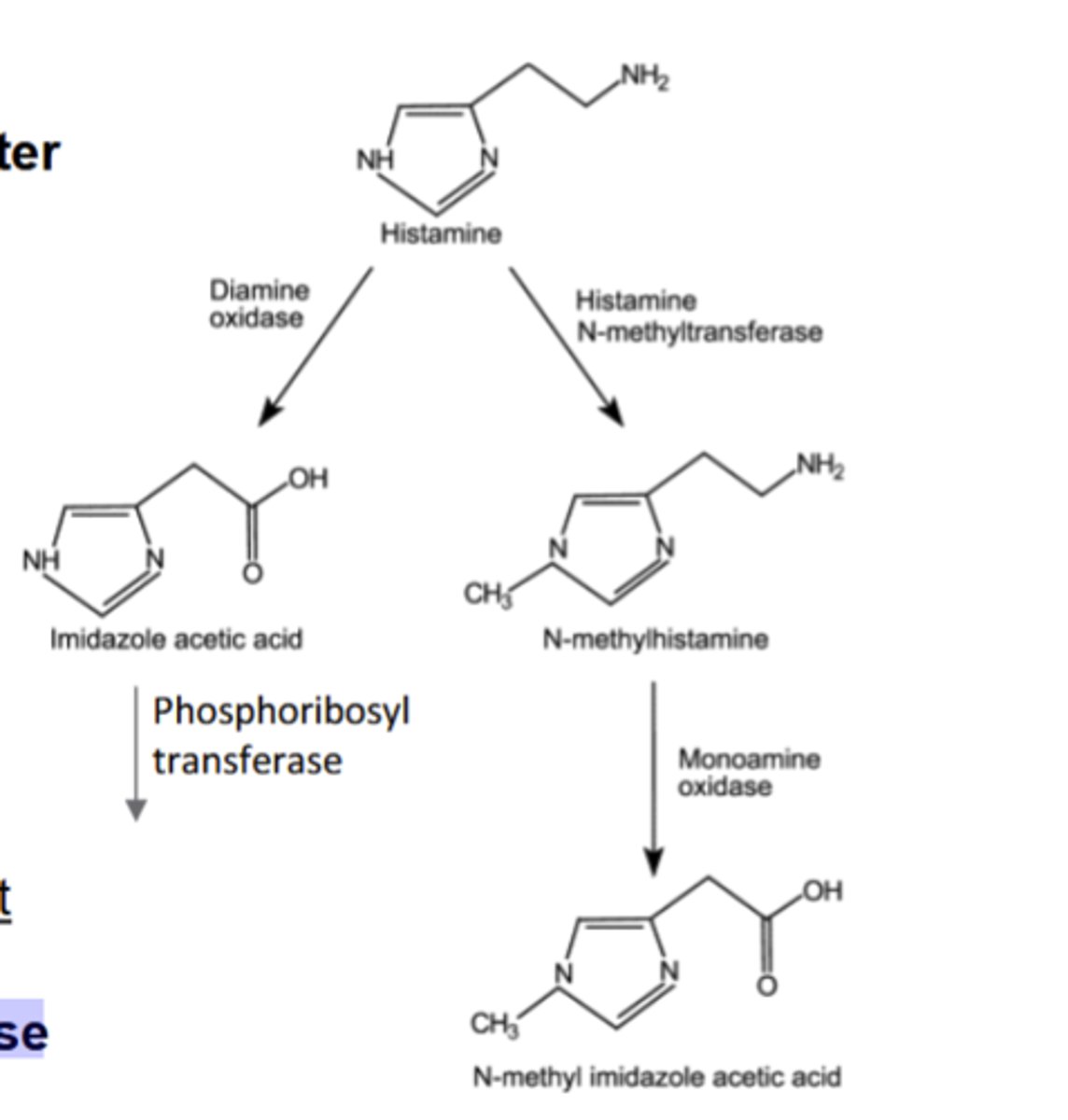
What are the 2 major pathways of Histamine metabolism?
1)Histamine-N-methyltransferase, then monoamine oxidase (primary method, terminates histamine signaling in synaptic cleft)
2)Diamine Oxidase, then phosphoribosyl transferase (less common)
Histamine is a NT for which receptors?
4 Histamine Receptors (H1-H4)
H1 Receptor: Location, Agonists, Antagonists, G-Protein, excitatory or inhibitory?
Location: smooth muscle, tuberomammillary nucleus, PNS: sensory neurons
Agonists: 2-CH3-Histamine
Antagonists:Cetirizine
G-Protein: Gq
Excitatory
H2 Receptor: Location, Agonists, Antagonists, G-Protein, excitatory or inhibitory?
Location: PNS:smooth muscle, parietal cells (stomach)
Agonists: Amthamine
Antagonists: Ramitidine, Famotidine
G-Protein: Gs
Excitatory
H3 Receptor: Location, Agonists, Antagonists, G-Protein, excitatory or inhibitory?
Location: presynaptic CNS, cortex and subcortex
Agonists: (R)-alpha-CH3-histamine
Antagonists: Pitolisant
G-Protein: Gi/Go
Inhibitory
H4 Receptor: Location, Agonists, Antagonists, G-Protein, excitatory or inhibitory?
Location: Basophil, Thymus
Agonists: 4-CH3-histamine
Antagonists: Thioperamide
G-Protein: Gi/Go
Inhibitory
Actions of Histamine cells in periphery
-inflammation response
-Sexual function and libido
-Promotes gastric acid secretion
Histamine action in inflammation response
Mast cell + basophil granules release histamine ↑swelling, vasodilation, otherautacoids. Causes hypersensitivity to pain. ↑bronchoconstriction; mediates allergy responses.
Histamine and H4 receptor agonists strong promotors of pruritus(itching sensation) and burning feeling
Histamine action in sexual function and libido
H2R antagonists produce erectiledysfunction; direct histamine injection reverses
Histamine action on gastric acid secretion
Enterochromaffin-like (ECL) cellsin the stomach release histamine, stimulating H2 receptors onparietal cells, causing release of stomach acid from those cells.
Histamine release dec/inc with pH
decreases
H2R antagonists block → inc/dec acid
decrease
Where in the CNS do H4 receptors cause pruritis?
This effect is mediated by peripheral H4receptors.
Which Histamine receptors are found in the CNS?
Neurons containing H1 and H3 receptors identified in CNS
In the Histamine CNS Tuberomammillary pathway, which histamine receptors are involved?
H1 receptors + histamine as NT
Origin/Projections of the Histamine CNS Tuberomammillary pathway
Originates in tuberomammillary nuclei of hypothalamus, projects to dorsal raphe, locuscoeruleus, cortex, amygdala, nucleus accumbens, pituitary, hypothalamus

How do Projections of the Histamine CNS Tuberomammillary pathway to basal forebrain and pons affect the release of ACh
they increase ACh release
Actions of the Histamine CNS Tuberomammillary pathway
-Increased cortical activity
-Regulates noiciception
-Regulate neuroendocrine, body temperature and cardiovascular activity.
-H1 agonists inhibit appetite
-Neuromodulation
How does the Histamine CNS Tuberomammillary pathway act on cortical activity?
Increase cortical activity: promotes arousal, wakefulness
H1 agonists in cortex improve cognition; antihistamines ↑ sedation
How does the Histamine CNS Tuberomammillary pathway act on noiciception?
Regulates nociception: Activates inhibitory GABA system, thereby suppressing descendingpain control pathway in dorsal raphe and LC
Low concentrations of H1 receptors in PNS sensory nerve endings: promote hypersensitivity to pain
How does the Histamine CNS Tuberomammillary pathway act on neuromodulation?
Presynaptic H3 receptors in brain act as autoreceptors: reducing their own release. Theyalso decrease release of acetylcholine, NE, DA and serotonin to modulate nociception + signal satiety.