Pharm Lecture 1
1/147
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
148 Terms
What is pharmacology?
biomedical science studying the interaction of chemical substances with living cells
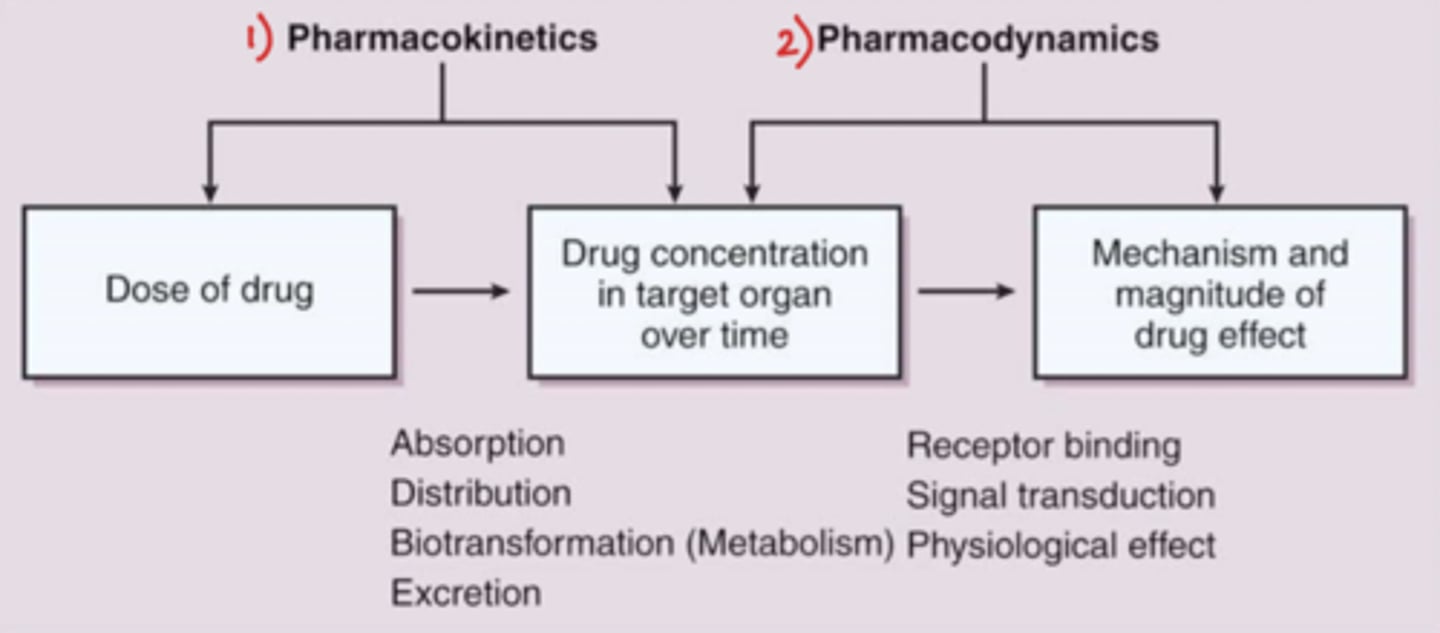
What are the two subdivisions of pharmacology?
1) Pharmacodynamics
2) Pharmacokinetics
What is Pdynamics?
- What the drug does to the body
- includes receptor binding/drug target, signal transduction, and the physiologic effect of the drug
What is Pkinetics?
- What the body does to the drug
- ADME (absorption, distribution, metabolism, excretion)
What is the relationship between Pkinetics and Pdynamics?
- Pkinetics: dose of drug --> drug concentration in target organ over time
- Pdynamics: drug concentration in target organ over time --> mechanism and magnitude of drug effect
- Pkinetics leads to Pdynamics!
What are 4 examples of natural sources of drugs?
1) plants (alkaloids containing nitrogen groups)
2) Microbes/microorganisms (antibiotics)
3) animals (hormones)
4) minerals (few therapeutic agents, Lithium)
What are 3 examples of drugs that come from plants?
1) morphine (opium)
2) quinine (cinchona bark)
3) atropine (belladonna)
What are 2 examples of drugs that come from microbes/microorganisms?
1) Penicillium
2) Streptomyces species
What are synthetic drugs?
- Chemotherapeutic agents prepared from chemicals in the lab, man made
- Helps create better meds
How do synthetic drugs help create better meds?
- via molecular modeling (ex: R-isomer to L-isomer)
- structural changes = better formulation = less side effects!
What is the drug preparation process? Use the example of opium being isolated from the poppy.
1) begin with the natural source: opium poppy flower.
2) crude drug preparation: the dried juice of the poppy seed capsule (active ingredient of opium) is extracted
3) pure drug compound: the pure drug is extracted, producing morphine in this case
4) pharmaceutical preparations: convert the pure drug into tablet form, oral solutions, or IV solutions
What are 7 common pharmaceutical forms of drugs?
1. Tablets/Capsules
2. Suspensions/solutions
3. Skin patches
4. Aerosols
5. Topical agents
6. Suppositories
7. IM, SC, IV (injectables)
What is the difference between active and inert ingredients in tablets?
- active ingredients: carry the active component of the drug
- inert ingredients (inactive/excipients): determine the shape and stability of the pill + help with disintegration, dissolution, and absorption of drug
What are 2 purposes of the enteric coating on a pill/tablet?
- protects the drug from acidic gastric HCl in the stomach (allowing it more time to sit in the stomach)
- protects the stomach lining from the drug itself
What are 2 examples of drugs with enteric coating + the purpose of their coating?
1) aspirin EC --> coated to protect the stomach lining from the med (can create ulcers if not coated)
2) pantoprazole (Protonix) --> can be very easily disintegrated in the GI tract, coated to avoid this
What are SR, ER, CD tablets?
- sustained release, extended release, controlled diffusion
- release the drug over many hours
- usually seen in 1x daily meds
Can capsules also have SR, ER, CD properties?
yes, sometimes pellets in a capsule have CD properties (ex: Cardizem)
Why are SR/ER tablets useful?
Patient only have to take 1x daily --> promotes better compliance and adherence to medications vs. immediate release
To review, what are enteric-coated products + 2 pros of them?
- content absorbed in the small intestine
- 2 pros: prolonged stability in the GI tract + less GI irritation
What are 5 examples of enteric-coated products?
1) Diclofenac and Misoprostol
2) Aspirin
3) Bisacodyl
4) Ferrous sulfate
5) Pantoprazole
To review, what are SR, ER, CD products + 2 pros of them?
- content gradualy released overtime
- 2 pros: prolonged duration of action + less frequent administration
What are 4 examples of slow or extended release products?
1) Cardizem CD, LA, SR (Diltiazem)
2) Toprol-XL (Metoprolol)
3) K-Dur, Klor-con (Potassium chloride)
4) Oxycontin (Oxycodone)
^just know the generic in parentheses, but the brand name will have the letters in them (ex: Cardizem literally says CD in it)
For patients on Enteral Gastric Feeding (EGF), should you use enteric-coated products or SR,ER,CD products?
you should use immediate release (and crush if possible) or liquid formulations, if available!
What kind of tablets can be crushed?
- any tablet with no enteric coating or SR/ER/CD
- any tablet with no special formulation
Why can't you crush a tablet with a special formation?
crushing a tablet with special formulation renders it ineffective as the special formulation is now destroyed
What are 3 types of products you CAN'T crush?
1) sublingual products
2) enteric-coated products
3) SR products
You have prescribed a patient Adderral XR for once daily use. Patient is having a hard time swallowing the pill and calls your office asking if she can crush the pill and take it with food. What would your response be and why?
NO! Crushing an XR pill will destroy the special formulation designed to make the medication extended-release
She will not get the proper effects of the medication --> can possibly get too much at once, NOT GOOD!
What are 3 types of solutions/suspensions?
1. Oral (syrups, elixirs)
2. Sterile (parenteral administration)
3. Sterile powders for reconstitution with sterile liquids
When are syrups/elixirs commonly used?
In pediatrics/geriatrics
Groups that cannot swallow tablets well
When should you be cautious about using syrup form of medication?
If patient has diabetes
Syrups contain sugar!
What should you be cautious of when administering an elixir form of medication?
If there is potential for alcohol drug interaction
Elixirs are sweetened alcoholic solutions, if the patient is taking another medication that has an alcohol-drug reaction, it can have severe side effects
Ex: Disulfuram --> rxn can cause severe vasodilation (erythema, BP drop)
What are some characteristics of skin patches? (3)
- slow release of drug
- rate controlling membrane that regulates diffusion of the drug into the skin
- contains sufficient lipid solubility to enable skin penetration
Would you use skin patches for emergencies?
no (they're too slow!)
What is bridging with medication?
Starting a patient with IV/oral form of med as well as the patch, 3 days later can discontinue IV/oral form and continue with patch
WHY? The skin patch can take a few days to work. IV/oral form will give patient immediate benefits and can continue regimen with skin patch once it begins to work
What are 4 examples of skin patch medications?
1) nicotine patches
2) lidocaine
3) birth control
4) dramamine
What are aerosol medications? What are they useful for and what can they minimize?
- administered by inhalation through nose/mouth
- useful for respiratory disorders
- minimize systemic side effects
What are 3 examples of topical agents?
1) ointments
2) creams
3) lotions
What are suppositories? How are they given?
Solid dosage forms intended for insertion into body orifices where they melt, soften and dissociate
Typically given rectally, vaginally, or urethrally
What are 5 routes of administration?
1) enteral
2) parenteral
3) transdermal
4) inhalational
5) topical
What is an enteral medication? What are 4 types of enteral absorption?
- a drug that can be absorbed from the GI tract
- types include: sublingual (under the tongue), buccal (inside the cheek), oral and rectal (ex: suppositories!)
What is a parenteral medication?
a medication that does not pass through GI tract, typically given via injection
What are some examples of parenteral routes of administration?
- IV: intravenous
- IM: intramuscular
- SC: subcutaneous
^ main 3
- intrathecal, epidural
- intraarticular, intradermal
What is the most readily absorbed medication via injection?
IV > IM > SC
Only __________ drugs can go the transdermal route of administration.
lipophilic
What are the advantages and disadvantages of PO medication (oral route)?
Advantages:
- Convenient
- Relatively safe
- Economical
Disadvantages:
- Cannot be used for drugs that are inactivated by GI tract, irritate the GI tract, or drugs with large first pass effect
While the IV, IM, and SC parenteral routes have quicker absorption, what are some disadvantages of each?
- SC: can't be used for drugs that irritate cutaneous tissues, or drugs given in large volumes
- IM: may cause bleeding if patient is receiving an anticoagulant (DON'T USE IN ICU)
- IV: more risks for toxicity + more expensive
You have a patient with pneumonia in the hospital. Both IV and oral are 100% bioavailable, but oral is cheaper. Should you switch the patient from IV to oral?
YES (as long as the patient isn't bleeding or clinically unstable)
What is the first-pass effect?
- drugs absorbed via GI tract are first circulated to the liver via the hepatic portal vein
- liver acts as a filter: only part of the drug will leave the liver to reach its target organ
If a medication has a high first-pass effect, will it be administered orally?
no (bc concentration is greatly reduced before reaching systemic circulation)
If a medication has a high first-pass effect, what are 6 alternative routes to administer the med?
1) Sublingual
2) Buccal
3) Topical
4) Rectal
5) Parenteral
6) Transdermal
How do sublingual medications work?
Content is dissolved and absorbed in the oral mucosa for immediate release, has quick onset of action
What are 2 examples of sublingual products? Are they effective for patients with feeding tubes?
1) nitroglycerin (for heart attacks, used sublingually because of quick onset of action)
2) Isosorbide dinitrate
- not effective in patients with feeding tube
If a patient has an enterogastric feeding tube, what kind of medication would you give them?
A crushable form of medication
NOT any extended release, would want an immediate release or liquid formulation if available
What does each term involve?
a) toxicology
b) pharmacotherapeutics
c) pharmacognosy
d) medicinal chemistry
e) pharmaceutics
f) pharmacogenetics
a) poisons
b) treatment, clinical trials
c) isolation from natural sources
d) design/chemical synthesis
e) formulations
f) genetic factors
What is the chemical name of aspirin?
Acetysalicylic acid or ASA
What is the chemical and generic name of Tylenol?
- chemical: APAP
- generic: acetaminophen
What are the steps to drug development in the US?
1. Discovery and characterization of a new drug
2. Pre-clinical studies
3. IND application
4. Clinical studies: 3 phases
5. Submission of NDA
6. Approval of NDA (FDA approved)
7. Postmarketing surveillance
What 2 things happen in discovery and characterization of new drug?
1) isolate or synthesize a new drug
2) determine chemical + pharmaceutical properties of new drug
What 2 things happen in pre-clinical studies?
1) determine Pkinetic and Pdynamic properties of the drug
2) test animals for toxicity
What 3 things are included in an IND application?
1) outline properites of the drug
2) report results of studies to date
3) propose clinical studies
What are the 3 phases of clinical studies?
1) Phase 1: gather data on drug safety and Pkinetics in healthy volunteers
2) Phase 2: gather data on a small group of patients
3) Phase 3: obstain statistical evidence of drug safety and efficacy (actual studies w/placebo vs. real that are reported by literature)
What 3 things are included in a submission of NDA?
1) outline properties of the drug
2) report results of all experimental and clinical studies
3) propose labeling of drug and clinical indications for use
What happens after approval of NDA?
marketing of drug
What is postmarketing surveillance?
- aka Phase IV
- the FDA seeks voluntary reporting of adverse drug reactions from healthcare professionals through MedWatch program after a drug is approved and put onto the market
Why is post marketing surveillance important?
can detect uncommon drug rxns not found during clinical trials
What happens if multiple adverse reactions are reported to the FDA on a drug?
They will put a black box warning in package insert to alert patients
If severe enough --> will be recalled and taken off the market
How much variability does the FDA approve for generic version of drugs?
20%
ex: if Drug A is the principal drug and gives 100% effect, if Drug B gives 80-100% effect it will still be approved as a generic version of Drug A
How long until a generic version of a drug can be developed?
17 years
What are 4 different ways a drug can be absorbed into the systemic circulation?
1) Passive diffusion (most drugs)
2) Lipid diffusion: drug dissolves in lipid components of cell
3) Aqueous diffusion (via aqueous pores)
4) Active transport/facilitated diffusion (few drugs)
Regarding drug absorption,
a) what is an example of lipid diffusion
b) what type of drugs use aqueous diffusion
c) what does active transport/facilitated diffusion require
a) blood brain barrier
b) ONLY low molecular weight (LMW) drugs
c) carrier molecule + form of energy
Regarding the enteral drug administration,
a) what is the drug absorbed by
b) what are 3 types of routes of administration
a) GI tract
b) oral, sublingual and buccal (Nitroglycerin), rectal
True or False? Oral administrations have slow absorption and a first pass effect.
false (they have VARIABLE absorption and a first pass effect)
True or False? Sublingual and buccal administrations have rapid absorption and little first pass effect.
false (they do have rapid absorption, but NO first pass effect)
Do rectal administrations have a first pass effect?
they have a localized or systemic effect, with little first pass effect
What is the advantage of parenteral drug administration?
bypasses the process of absorption (first-pass effect) with immediate elevated blood levels
Why are depot IM medications not suitable for IV injection?
depot IM contain oil in them, making them insoluble in blood --> if given IV, can cause embolus (ex: haloperidol)
If you are giving a medication through injection, what should you be aware of?
Muscle mass and blood flow --> if either are poor, there is not enough blood getting to periphery, can alter absorption
If you're giving insulin to a patient in the ICU, should you give it IV or SC?
IV (patients won't be able to absorb SC)
In weak acids, the protonated form is:
(H+)
NON IONIZED
In weak bases, the protonated form is:
(HB+)
IONIZED
Can ionized molecules be absorbed and penetrate the membrane?
No, polarized molecules have difficulty passing through the cell membrane via diffusion
Why are non-ionized molecules able to penetrate the membrane?
- less polar
- more soluble
What is the pKa of a drug?
The pH at which the molecule is 50% protonated and 50% non-protonated
If pH < pKa, then:
Protonated form predominates
If pH > pKa, then:
Non-protonated form predominates
What is the Henderson-Hasselbalch equation?
used to determine the ratio of protonated to non-protonated forms
log (protonated/unprotonated) = pKa - pH
Salicylic acid is a weak acid with a pKa of 3. At a pH of 2, what is the ratio of protonated to non-protonated forms?
log [HA]/[A-] = pKa -pH
log [HA]/[A-] = 3-2 = 1
inverse log (1) = [HA]/[A-]
Therefore, [HA]/[A-] = 10/1 = 10
Amphetamine is a weak base with a pKa of 10. At a pH of 8, what is the ratio of protonated to non-protonated forms?
log [HB+]/[B] = pKa -pH
log [HB+]/[B] = 10 - 8 = 2
inverse log (2) = [HB+]/[B]
Therefore, [HB+]/[B] = 100/1 = 100
What is the ion trapping concept?
The idea of trapping ions of medications and not allowing them to enter the circulation --> effective in ODs
Degree of ionization and rate of renal excretion will depend on what 2 factors?
1) pKa of the compound
2) pH of renal tubular fluid
Rate of excretion of a weak acid will be accelerated by:
Alkalanizing the urine
Rate of excretion of a weak base will be accelerated by:
Acidifying the urine
If a patient is having an aspirin overdose, what can you do to increase the rate of excretion of the aspirin?
alkalanize the urine by giving Na+ bicarb infusion IV q 3-4 h to increase urine pH to 7-8
Why does giving bicarbonate to treat aspirin OD work?
- ratio (protonated/non-protonated) ion is altered
- aspirin (HA) will donate a proton to form an anion (A-)
- results in more ionized aspirin (which won't go through cell membrane)
- therefore, aspirin is excreted
What are 4 factors affecting drug distribution?
1. Organ blood flow
2. Plasma protein binding
3. Molecular size
4. Lipid solubility
What is plasma protein binding?
Medication will try to bind to proteins within the body (specifically, albumin) --> will slow drug from getting to its target
The amount of medication that binds to albumin affects what is left to enter cells
What is drug biotransformation/metabolism?
the conversion of drugs to metabolites, making them more polar and water-soluble (allowing the body to excrete them more easily)
Where does drug biotransformation/metabolism occur?
Primarily in liver, kidney, gut, tissues, etc.
What are 2 other examples of drug transformation?
1) prodrug: inactive compounds become active
2) first pass effect
What do phase 1 and 2 metabolic reactions do?
Change the configuration of medications so we can excrete them from the body
Basically, metabolizing the drug into smaller form