Pain
1/72
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
73 Terms
Pain Definition
An unpleasant sensory and emotional experience associated
with actual or potential tissue damage.
Acute Vs Chronic Pain
Acute - A useful biological response provoked by injury or disease, which is short term. Responses are usually adaptive.
Chronic - A pain persisting for 6 months or more and tends to not respond well to pharmacological treatment. Responses are often maladaptive.
Gate-Control Theory of Pain
A theory that explains how our perception of pain is not just a direct result of tissue damage, but is also modulated by a "gate" mechanism in the spinal cord and influenced by psychological factors.
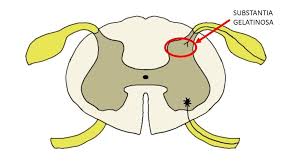
Where is the gate located?
The Substantia Gelatinosa
Nocireceptors
Nerves that transmit pain sensations from the site of injury to the spinal gate.
A-Delta Fibres
Nociceptor type that transmits information about very strong noxious stimuli (potential or actual tissue damage).
Key characteristics of A-delta fibres.
Myelinated
Senses pain
Afferent nerve
Associated with sharp, temporary pain
C-polymodal fibres.
Nociceptor type that carries information about dull, throbbing, longer-lasting pain.
Key characteristics of C-polymodal fibres.
Slow conducting
Non-myelinated (contributes to slow speed)
A-beta fibres.
The type of nerve fibres often referred to as "anti-pain" fibres.
Function of A-beta fibres.
Their activation (e.g., through rubbing, massage, heat) inhibits the perception of pain.
Key characteristics of A-beta fibres.
Myelinated
Mechanically sesitive
Afferent nerve
Why is pain usually experienced in two distinct phases?
Becuase the different nociceptor fibres (A-delta and C-polymodal) transmit information at different speeds.
The first phase of pain: sensation and fibre type.
A sharp pain, which is mediated by the faster A-delta fibres.
The second phase of pain: sensation and fibre type.
A more chronic, throbbing pain, mediated by the slower C-polymodal fibres.
How can pain signals be counteracted via the periphery CNS?
By activating the A-beta fibres (e.g., rubbing the area).
Example: Mum rubbing their childs hurt arm
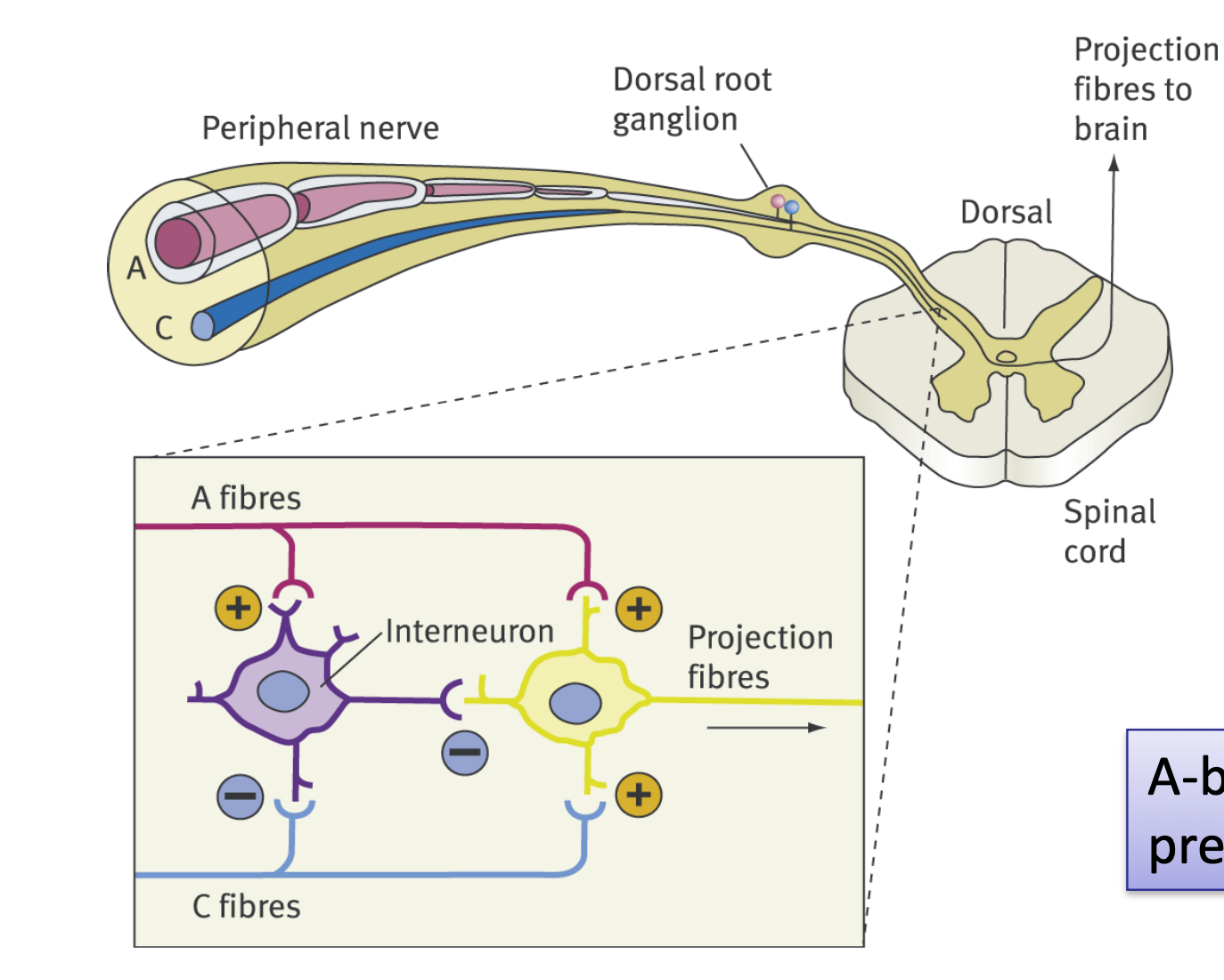
According to the diagram, what is the pathway of a sensory signal from the body?
Peripheral nerve -> Dorsal root ganglion -> Dorsal horn of Spinal cord -> Projection fibres to brain.
Where are the cell bodies of the peripheral nerves located?
In the dorsal root ganglion
What 2 fibres are shown synapsing in the spinal chord?
A-beta fibres and C-polymodal fibres fibres
What two neurons do the 'A-beta fibres' excite (+)?
The interneuron and the projection fibres
What two neurons do the 'C fibres' interact with?
They inhibit (-) the Interneuron and excite (+) the Projection fibres.
What is the role of the Interneuron in this diagram?
It inhibits (-) the Projection fibres, helping to 'close the gate' to pain signals.
Which fibres carry the signal from the spinal cord up to the brain?
Projection fibres
Based on the diagram, what is the effect of 'A-beta fibre' activation?
It excites the inhibitory Interneuron, which helps to reduce the signal from the Projection fibres (closes the gate).
What is the name of the area in the spinal cord where this interaction occurs?
The substantia gelatinosa (in the dorsal horn).
Hoe does anxiety and depression affect pain?
They decrease pain tolerance and increase the reporting of pain
How does attention influence pain?
Focusing on pain increases the experience of pain
How do expectations affect pain?
Your Expectation | Effect on the Spinal Gate | Result |
Expect Pain (Increase) | The brain sends signals down the spinal cord that open the gate (disinhibition). | The incoming pain signal (nociception) is amplified, and you feel more intense pain. |
Expect Relief (Reduction) | The brain sends signals down the spinal cord that close the gate (inhibition). | The incoming pain signal is dampened, and you feel less pain. |
Name the four types of thought listed that influence the pain experience.
Attributions of cause
Beliefs about tolerance
Beliefs about control
Expectations of relief (placebo effect)
A patient's self-assessment of how much pain they can handle is what type of influencing thought?
Beliefs about the ability to tolerate pain.

Who postulated the gat control mechanism?
Melzack and Wall
What peripheral fibres send information to the substantia gelantiosa?
A and C fibres
What fibres send signals down from the brain to influence the gating mechanism?
Reticulospinal fibres
What activates the reticulospinal fibres?
Cognitive and emotional responses to pain from the brain
What is the function of the descending (Reticulospinal) pathway on the gate?
It inhibits the gating mechanism
— Closes the gate/ Stops pain signal
What is ultimately transmitted to the 'pain centres in the brain'?
The summation of both pain and neural inputs (the output of the gate).
What two types of input arrive at the spinal gate simultaneously?
Information about physical damage (from peripheral pain receptors).
Related cognitions and emotions (from the CNS/Brain).
The peripheral pain receptors transmit information to a series of 'gates' where before going to the brain?
The spinal colum
How do cognitions and emotions from the brain reach the spinal column gate?
Through the activation of CNS reticulospinal nerve fibres that take information down the spinal column.
What is the state of the gate when pain perception is high?
The gate is OPEN
What is the state of the gate when pain perception is low?
The gate is CLOSED
What is the function of the ‘Gating mechanism’?
It recieves and sums up inputs from pain fibres, other peripheral fibres, and the brain to determine the final signal to the transmission cells
What is the function of the ‘Transmission cells’?
They recieve the calculated signal from the gating mechanism and sends the final pain message to the brain.
Factors that OPEN the gate (increase pain)
• Physical: Injury, inactivity, long-term drug/alcohol use.
• Behavioural: Poor activity pacing (doing too much), poor sleep.
• Emotional: Anxiety, depression, stress, helplessness.
• Cognitive: Focussing on pain, worrying, catastrophising.
Factors That Tend to CLOSE the Pain Gate (Decrease Pain)
• Physical: Appropriate medication, heat/cold, massage.
• Behavioural: Exercise, relaxation training, sleep hygiene.
• Emotional: Laughter, optimism, engaging in enjoyable activities.
• Cognitive: Distraction, active coping.
What are the two main categories of pain assessment scales shown?
Unidimensional scales
Multidimensional Scales
Unidimensional Scale
These scales focus only on the intensity or severity of pain. They are quick and easy to use but lack detail about the quality or emotional impact of the pain.
Example - Visual analog scale
Multidimensional scales
These scales capture the complexity of the pain experience by assessing different aspects (sensory, emotional, evaluative) beyond mere intensity.
Examples - McGill Pain questionaire
Subjectivity of Pain (Sternbach's Definition)
The accepted definition holds that pain is entirely defined by the patient's report, establishing self-report as the gold standard for assessment.
Mnemonic for pain
Letter | Question Category | What to Ask the Patient |
S | Site | Where exactly is the pain? Can you point to it? |
O | Onset | When did the pain start? Was it sudden or gradual? |
C | Character | What is the pain like? (e.g., Sharp, stabbing, dull, throbbing, burning.) |
R | Radiation | Does the pain spread or move anywhere else? |
A | Associated symptoms | Are there any other symptoms that accompany the pain? (e.g., Nausea, fever, sweating, numbness.) |
T | Timing/Pattern | Is the pain constant, intermittent, or does it follow a specific pattern? |
E | Exacerbating/Relieving factors | What makes the pain worse (exacerbates it)? What makes the pain better (relieves it)? |
S | Severity | How bad is the pain on a scale of 0 to 10, where 10 is the worst pain imaginable? |
What was the historical primary aim of pain management?
To eliminate pain
List the 5 aims of modern pain management
Reduce pain perception
Improve coping ability
Increase functional ability
Decrease drug reliance and distress
Respect for attempts at self-management
In modern pain management, what is prioritized over completely eliminating the pain?
Improving coping ability and increasing functional ability.
Which modern aim acknowledges the patient's agency in their treatment?
Respect for attempts at self-management.
First line of treatment?
In acute settings (e.g., post-surgery or trauma), medication (pharmacology) is the initial and primary method used to reduce high-intensity pain signals.
What level of treatment does psychological intervention form in acute pain management?
Second-level Intervention
Second-level Intervention
Psychological strategies are used adjunctively to medication to enhance comfort and control, but they are not typically the immediate first step.
What are the two main ways psychological intervention increases patient control in acute pain?
Increasing patient control (e.g., patient-controlled analgesia or PCA).
Teaching coping skills.
What does increasing patient control do?
Increasing Patient Control: Giving the patient the ability to self-manage treatment helps reduce anxiety and feelings of helplessness, which, according to the Gate Control Theory, helps close the pain gate.
What does patient controlled analgesia do?
Giving the patient the ability to self-manage treatment helps reduce anxiety and feelings of helplessness, which, according to the Gate Control Theory, helps close the pain gate.
What are the two primary coping skills taught for acute pain?
The two most common and effective skills taught for acute pain are Distraction (shifting mental focus away from the pain) and Relaxation (reducing physical tension and anxiety).
Name a non-pharmacological technique mentioned that can be used for psychological intervention in acute pain.
Hypnosis
Define 'Primary (intrapersonal) gain' in the context of chronic pain.
Primary (intrapersonal) gain
Secondary (interpersonal) gain
Tertiary gain
Explain primary (intrapersonal) gain in context of chronic pain
Expressions of pain result in the cessation of an aversive consequence (e.g., avoiding household chores or going to work).
Define 'Secondary (interpersonal) gain' in the context of chronic pain.
Pain behaviour yields a positive outcome from others, such as expressions of sympathy or care.
Define 'Tertiary gain' in the context of chronic pain.
Feelings of pleasure or satisfaction experienced by the person helping one in pain.
List the 'Five D's' that describe the results/consequences of chronic pain.
Dramatisation of complaints
Disuse through inactivity
Drug misuse (over-medicating)
Dependency on others
Disability due to inactivity
Behavioral strategies for chronic pain are based on which learning principle?
Operant learning (contingency management). Focuses on reinforcing adaptive behaviours (like exercise) and ignoring pain behaviours.
Cognitive strategies in chronic pain management?
Central to changing the pain experience. Focuses on altering maladaptive beliefs about the unmanageability of pain, challenging distorted thinking (like catastrophising) and providing information to reduce anxiety.
What does PMP stand for?
Pain Management Programmes
What type of team delivers a PMP?
A Multidisciplinary Team (MDT) including doctors, nurses, physiotherapists, psychologists, etc.
What theoretical principles underpin Pain Management Programmes?
Cognitive-behavioural principles (CBT).
Why are PMPs often delivered in a group format?
To normalise the pain experience and maximise learning.