health services management econ
1/112
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
113 Terms
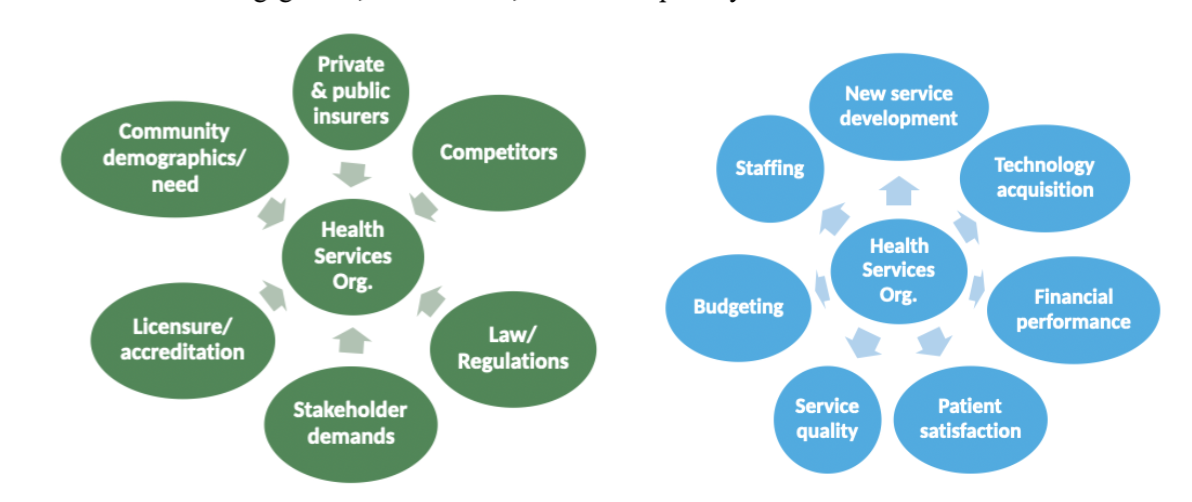
healthcare organization
An entity designed for a specific purpose:
To create products provide services, using people and resources to improve health; and
To maintain relationships with customers, suppliers, competitors, and regulators
direct care
Provide healthcare services to individual people firsthand
Traditionally paid by insurance
non direct care
Provide products and services that support healthcare services
May be paid by insurance or out-of pocket
healthcare management
Accomplishing organizational goals by controlling and regulating activities and behaviors within established relationships to coincide with previously established plans
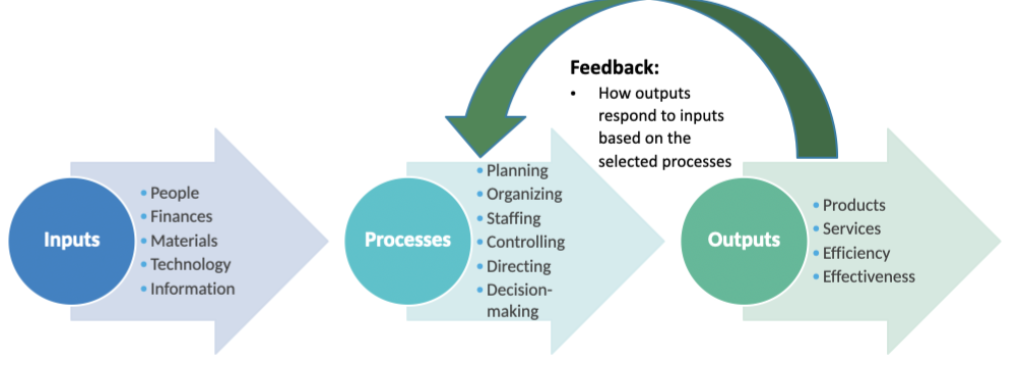
planning
set priorities and performance targets
organizing
designate reporting relationships and responsibilities
staffing
recruit, develop, and retain workforce
controlling
monitor performance and take corrective action
directing
lead, motivate, and communicate with staff
decision making
weigh pros and cons of alternative actions
systems theory
Measures workplace effectiveness based on interaction between organization and its environment
Open vs closed system
To what extent is the organization interacting with its environment?
We have to pay attention to the people and how they are relating to one another in the organization, while also focusing on outside processes
patient centered management
Systems approach, interdisciplinary
Addressing root causes of disease, social determinants of health, patient engagement, collaboration, cultural competency
leadership - board of directors
Establish mission
Set vision
Motivate stakeholders
Be effective spokesperson
Determine future strategy
Transform organization
Network
management - staff
Staff personnel
Assure patient centered practices
Control resources
Supervise services provided
Oversee adherence to regulations
counsel/develop employees
Manage operations
organizational culture
Shared beliefs, attitudes, and behavior that prescribe the way things are dine
The character, personality, and experience of organizational life
Guiding principles defined and shaped by the organization’s values, mission, vision, and managers
mission statement
Fundamental purpose
What the organization does, for whom, and why
Broad and enduring
vision statement
Desired future state
What organization plans to accomplish over a period of time (ex 3 to five years)
values
Principles in which organization believes
Shape purpose, goals, and daily behavior
Serve as a foundation for activities
healthcare organization governance
Responsibility for organization’s strategic oversight
governing body
Group of people who collectively assume responsibility for organization’s governance
Board of trustees - nonprofits
Board of directors - for profits
sources of authority
State law
Organization’s bylaws
Articles of incorporation
board member duty of care
Act with good faith and competence - ordinarily prudent person in similar circumstances
Make informed reasonable decisions
board member duty of loyalty
Act in organization’s best interest
Avoid conflicts of interest/do not use information for personal gain
board member duty of obedience
Act consistent with organiations goals and missions
Follow the law and organization rules
governing board responsibilities
Strategic planning, including mission vision and value
Oversight of quality performance and measurement
Financial oversight
Ceo selection, performance, evaluation, and succession planning
Risk and identification and oversight
Communication and accountability
Governance
ex officio board members
Employees are not usually governing board members
The CEO may be an ex officio board member
Does not vote
Serves on the board as a result of their employment in that job
for profit organizations
Public investor owned or private equity
Goal compensate investors
How is profit used?Distribute profit to shareholders
Do they pay income tax?
yes
Must they offer charity care?
May offer to be a good citizen but no tax advantage for doing so
nonprofit organizations
Public charity or Private foundation
Benefit the public - promotion of health for a community’s benefit
How is profit used?
Reinvest profit back into organization
Do they pay income tax?
Exempt from income tax
Must they offer charity care?
Must provide some charity care in exchange for tax exempt status
revenue
what the organization earns from providing services
money available to fund operations
expenses
what it costs the organization to provide servies
profit (or loss)
total revenues minus total expenses
profit margin
profit divided by total revenue
990 summary
Number of employees
Number of volunteers
990 mission and programs
Brief description of mission
Accomplishments for 3 largest program service areas
990 governance, management, and disclosure
Number of voting members on governing body
Conflict of interest policies
990 compensation
Names of current board members (typically not paid(
Names of “key employees”
990 statement of revenue
Program service revenue
Government grants
Fundraising
What the organization earns from providing services
990 statement of functional expenses
Salaries and wages
Employee benefits
Fees (legal, accounting, fundraising expenses, etc)
Advertising
Office expenses
What it costs the organization to provide services
990 reconciliation of net assets
Total revenue less expenses
Organization’s profit or loss
primary health services
Family medicine
Internal medicine
Pediatrics
OBGYN
Diagnostic lab/radiology
Emergency medicine
Pharmaceutical
preventative health services
Pre and perinatal
Health screenings
Well child visits
Pediatric eye, ear, dental screenings
Immunizations
Family planning
Preventative dental
enabling services
Referrals to specialists
Case management
Help with accessing public benefits
Outreach and education
Transportation
Interpretation and translation
optional servies
Mental health and SUDs
Recuperative care
Environmental health
Agricultural workers
what is missing from the FPL?
What is missing?
Taxes
Regional price differences
Payments from antipoverty programs (EITC, housing subsidies, SNAP)
Assumes 2 parent households, 1 parent working and 1 staying home full time
Food accounts for smaller share of household expenses today, having been overtaken by costs of housing, childcare, transportation, and health care
MIT’s living wage calculator
determines the amount that a full time worker must earn to cover their family’s basic needs
Varies by family size and county
Accounts lowest option to meet minimum but adequate needs for food, child care, health care, housing, transportation, civic engagement, internet/mobile, and other necessities, as well as income and payroll taxes
Does not account for eating out, leisure time, vacations, savings, or retirement/long term investments
price
consumers have less purchasing power due to price increase
time
travel time and waiting time - opportunity costs, lost wages
income
purchasing power, incentive to stay healthy and maintain ability to work
care quality
- patient perception of higher quality increases demand
health status
increased demand when health status decreases
education
increased health literacy, earning capacity, likelihood of insurance
age
age related health declines—inccreased demand, increased service intensity
tastes and preferences
- other factors that influence an individual’s willingness to purchase
complementary goods
demand for complements also decreases, things that are used together ex. syringes and vaccines
substitute goods
demand for substitutes increases (assuming buyer has information about substitutes and their prices)
ex. physical therapy vs surgery
socioeconomic factors
40% Education, employment, income, family and social support, community safety
physical environment
10% Air and water quality, housing and transit
health behaviors
30% Tobacco use, diet and exercise, alcohol and drug use, sexual activity,
clinical care
20% Access to care and quality
health inputs
Health care, diet, exercise, environment, income, and time
Leads to health capital stock over time
Leads to health outputs each year
Healthy days, physically and mentally, activity limitations
commercial determinants of health
behaviors of private entities in the healthcare industry that influence health based on what is or is not provided to whom, when, where, how, and at what cost
Manufacturers (pharmaceutical and medical device firms)
Providers (hospitals, clinicians, trade associations)
Payers (insurance)
Other firms (consulting firm)
health industry as an essential service
which can also cause considerable harm, contributing to high spending with poor outcomes
Political practices (lobbying)
Preference shaping (consumption of individual medical services > promotion of public health and equity)
Legal and extralegal environment (corporate ownership and market consolidation)
Product generation and promotion (marketing, provider induced demand)
income
preventative care, healthy food, insurance, education/health literacy, living environment, working conditions
health
number of hours worked/amount earned, more health expenses/less disposable income, leave of absence/inability to do work
absolute income hypothesis
increased income leads to increased consumption of health goods and services leads to lower mortality/morbidity
Assumes relationship between income level and health is constant (linear) and income is the only factor determining purchasing decisions
law of diminishing marginal utility
As you continue to consume a given product, you will eventually get less additional utility (satisfaction) from each unit you consume
Income has a diminishing effect on health: substantial improvement in health initially as income increases
Health improvements get smaller as income increases
Whitehall study
Tracked health outcomes of 18000 british male civil servants for 10 years, beginning in 1967
Those with lowest ranking jobs were 3x as likely to die younger than those with highest ranking hobs
Lower ranking hobs were associated with obesity, smoking, low physical activity levels, higher prevalence of underlying disease, and high blood pressure
Whitehall II study tracked over 10000 people from 1985-2013 and found consistent results showing a stable relationship between occupational rank and health
headstart program
receive federal funds to provide preschool services to children ages 3-5
“Promote the school readiness of young children from loaw income families by enhancing their cognitive, social, and emotional development)
Children are eligible if
Family income below FPL
Recieves temporary assistance or supplemental security income benefits
Family is homeless
Child is in foster care
Federal law provides that children who are eligible for special education services should be prioritized for head start services
healthcare spending and financing
US healthcare spending was nearly 4.9 trillion in 2023
Spending
Hospital care - 31%
Physician and clinical spending - 20%
Prescription drugs - 10%
Nursing homes - 4%
Dental services - 4%
Home health care - 3%
Other spending - 28% - professional servives, medical equipment, other nondureable medical products, government administreation, gov public health activities etc
Financing
Out of pocket - 10%
Private health insurance 30%
Medicare 21%
Medicaid 18%
Other funding 21%
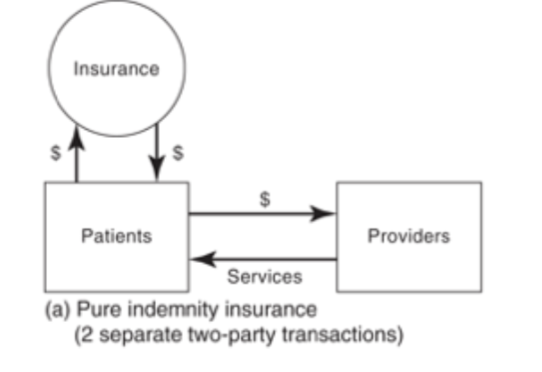
the healthcare services market
is not a perfectly competitive market because there is not equal information, nor is there equal market powers, also there is a third party (insurance)
how does a healthcare market differ from perfect competition
Perfect competition
Buyer pays seller for good/service
Buyer and seller are price takers
Price is the only term that matters
Buyer decides what to purchase
Price is the same for all buyers
Healthcare market
Multiple pirates involved in payment
Seller or payer may influence price
Trust, quality, licensure/regulation
incomplete/asymmetric information
Price discrimination (different prices for different buyers)
insurers role in the healthcare market
Pool and price risk
Manage service utilization
Reimburse providers for care
why by health insurance
Protection from large bills if one becomes seriously or chronically ill
Costs beyond capacity of individual savings or contributions from family/friends
Some predictability for out of pocket cost of routine medical care
Probability and expected value of healthcare costs averaged over a large group of people is predictable
health insurance
method of pooling financial risk so that one person’s loss is shared across so many people
benefits of risk pooling
Patients:
limited financial risk/peace of mind
Ability to obtain medical care could not otherwise afford
Insurers
Profits when premiums collected exceed provider reimbursement and administrative costs
Profits from interest earned on premium funds before paid out
Providers
Increased demand for healthcare services
Regular payments
actuarially fair price
Estimated annual cost of healthcare for the covered population +
loading factor
administrative costs and profits
how premiums are set
actuarially fair price + loading factor
medial loss ratio
the percent of premium income that insurers pay out for medical claims (vs administrative costs and profit)
why are insurance premiums rising
Higher service costs
Higher use of specialty prescriptions
Provider consolidation
Higher utilization
Workforce shortages
which types of insurance are subsidized by the federal government?
medicare: part A funded by payroll taxes paid by employers and employees
Parts b and d funded by income taxes and enrollee premiums
Medicaid: funded by federal and state taxes. Nominal out-of-pocket costs enrollees
Individual market - provides tax credits and subsidies - premiums paid by individuals. Federal subsidies based on income
Some help for employer-sponsored but clients are likely not aware. Employer payment is not taxable to employees
price sensitivity/elasticity
Demand for healthcare goods and services is generally price inelastic (price changes do not affect the quantity demanded)
However, there is some variation in by service type:
Price sensitive (demand increases as price decreases)
Mental health coverage
Prescription drugs
Not price sensitive (price changes do not change demand)
Hospital admissions
Six in 10 covered workers have an annual deductible of $1,000 or more
moral hazard in the healthcare market
Insurance generally increases consumption of healthcare services by making people less aware of, and less sensitive to, price
Excess service use results in higher premiums and higher healthcare prices
Insurers use cost sharing and/or utilization management to control “excess” service use
rand health insurance experiment
Increased premiums
Decreased enrollment and coverage renewals
Largest effects on those with the lowest income
Many become uninsured and faced increased barrier to care and financial burdens
Increased cost sharing
Even small levels decreased use of needle services
Increased use of more expensive services (ER)
Negative effects on health outcomes
Increased financial burdens for families
Money?
State savings are limited
Offset by disenrollment, increased cost in other areas, and administrative expenses
ACA no cost sharing requriements
Vaccines
Newborn screenings
FDA approved contraceptives
Statins to prevent cardiovascular disease
Colorectal cancer screening
PREP drugs to prevent HIV
Type 2 diabetes screening
conventional insurance
Providers are independent of health plan
No utilization management
no preferred provider network, fee for service, patient pays for a portion of provider charge
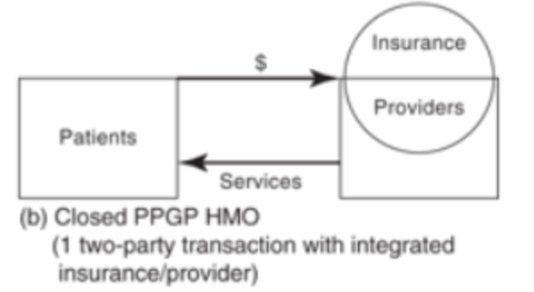
Closed pre paid panel group practice HMOs
Providers are integrated within health plan
Strict utilization management
Restrictive, quality of care decreases because of how strict they were—with plans that refused other care needed
open HMO, PPO, POS
Network providers contracted with health plan
Some utilization management

HMO
health maintenance organization - must see network providers —patient pays set monthly charge rgardless of service use (capacitation)
PPO
preferred provider organization, low cost sharing for in network services, no gatekeeper for specialist or hospital services
POS
point of service plan - lower cost sharing for in network services, need referral for specialist or hospital services
HDHP/SO
high deductible ehealth plan with savings option - deductible of at least $1000 single/$2000 family coverage, offered with health reimbursement or health savings account
HDHP/SOs allow for lower premiums
Incentivizes patients to “shop around”
how managed care can reduce costs
Total premiums = (price x quantity) + overhead
Reduce price -
Decrease provider payment
Increase patient cost sharing
Reduce quantity
Referrals
Prior authorization
Limit on number of days/visits
Reject claim as not medically necessary
Substitute cheaper inputs
RX formularies
Replace doctors with md-level practitioners
Require physical therapy v surgery
Reorganize
Integrate providers with health plan (closed panel HMO)
what is the price of healthcare services
it depends on coverage, deductibles paid, cost sharing, and co insurance
Prices paid by private insurance are higher than those paid by public programs
charges
the “list price” for a healthcare service (amount charged by provider without any discounts)
Does not reflect what (most) patients pay
Typically set abnormally high (in relation to cost of providing the service)
prices
total amount that provider expects to receive from insurer/patient as payment for a healthcare service
Accounts for discounts negotiated by insurers (provider agrees to lower price in exchange for higher patient volume)
advantages and disadvantages of fee for service
Fee schedule is prospective
Payment is retrospective
Provider receives set amount for each service provided to patient
Payment is based on volume, not quality
Incentive to provide more services and more intense services
Waste and unnecessary care
simplified capitation
Payment is prospective
Provider receives fixed monthly amount to provide a defined set of services to each patient
Provider is paid regardless of whether patients use services
Incentive to provide fewer services and/or keep patients healthy
Patients may go without care they actually need
value based care
Legal and regulatory changes
Standards and capabilities for data collection, sharing, and analysis
New models to improve care coordination across settings
New models that incentivize high quality, cost-efficient care
Provider performance measures based on clinical best practices
pay for performance
Provider receives set amount for each service provided to patient, plus incentives for reporting data or achieving certain quality measures
Financial incentives may be bonuses or penalties
Incentives are not based on achieving cost targets