11 - Proximal Tubule Reabsorption and Secretion
1/10
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
11 Terms
proximal tubule
first segment of nephron where bulk of reabsorption occurs
65% of water and solutes reabsorbed, 117L of water reabsorbed
contains microvilli that enhances surface area of proximal tubule for reabsorption
contains lots of mitochondria to power reabsorption
leaky tight junctions allow paracellular diffusion
in contact with peritubular capillaries → efficient solute transfer
reabsorption of substances
some solutes reabsorbed more avidly than others because of the presence of transporters specific to certain solutes in nephron
glucose and amino acids completely reabsorbed
80% of bicarbonate is reabsorbed
inulin → amount of inulin within PT stays the same but filtrate concentration increases since water is reabsorbed
if there is more solute left in proximal tubule than inulin → secreted
if there is less solute left in proximal tubule than inulin → reabsorbed
transcellular vs paracellular reabsorption
transcellular → requires transporters or channels on apical or basolateral membranes
primary active, secondary active, passive diffusion
paracellular → driven by concentration gradients and leaky tight junctions
proximal tubule reabsorption and secretion
reabsorption → Na+, water, HCO3-, amino acids, glucose
secretion → drugs
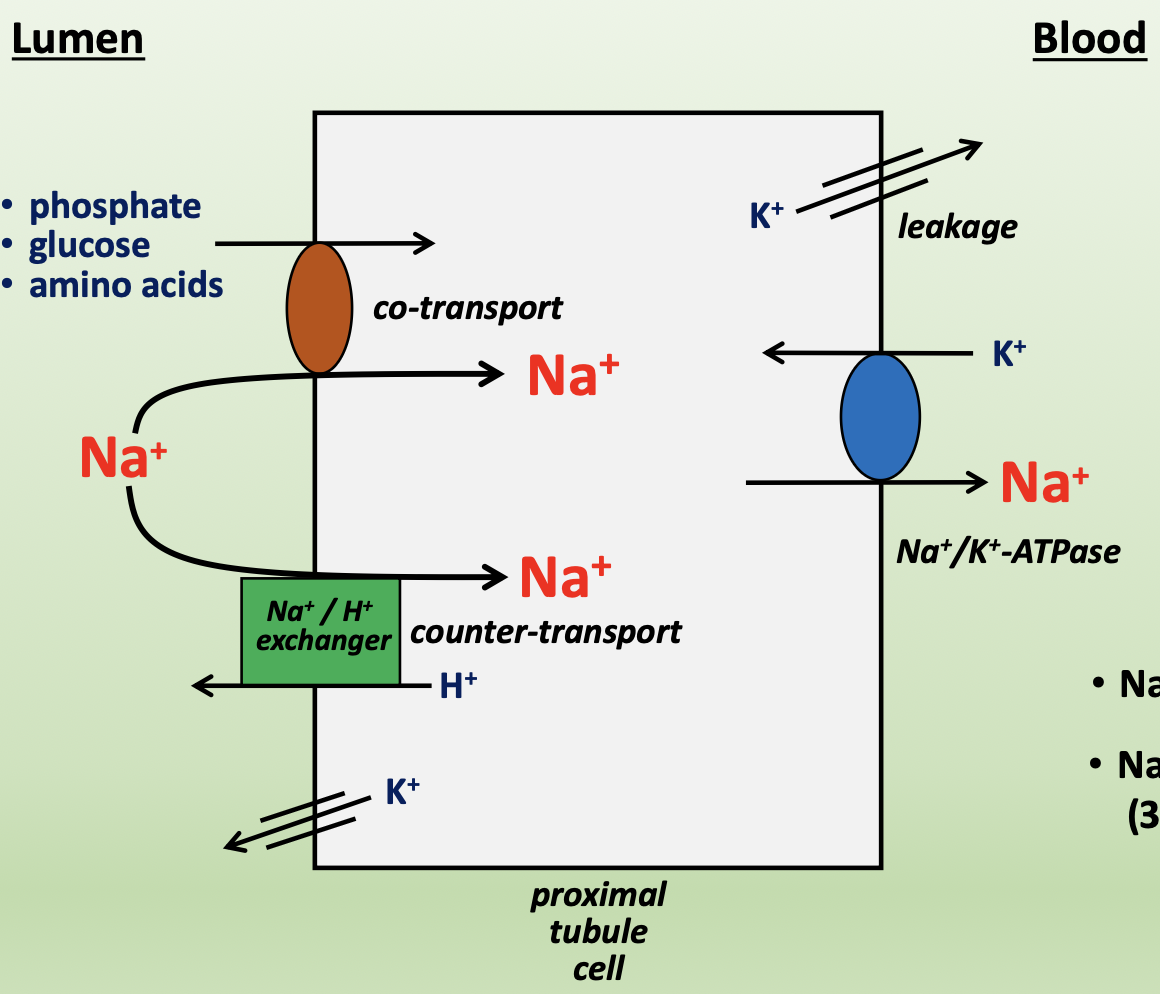
Na+ transport in proximal tubule
Na+ is reabsorbed from proximal tubule
Na+ enters cell from lumen down its concentration gradient (apical)
co-transport with phosphate, glucose, or amino acids
Na+/H+ exchanger → counter-transporter
Na+ exits cell into blood against its concentration gradient (basolateral)
Na+/K+-ATPase → pumps 3 Na+ out and 2 K+ in, establishes Na+ gradient
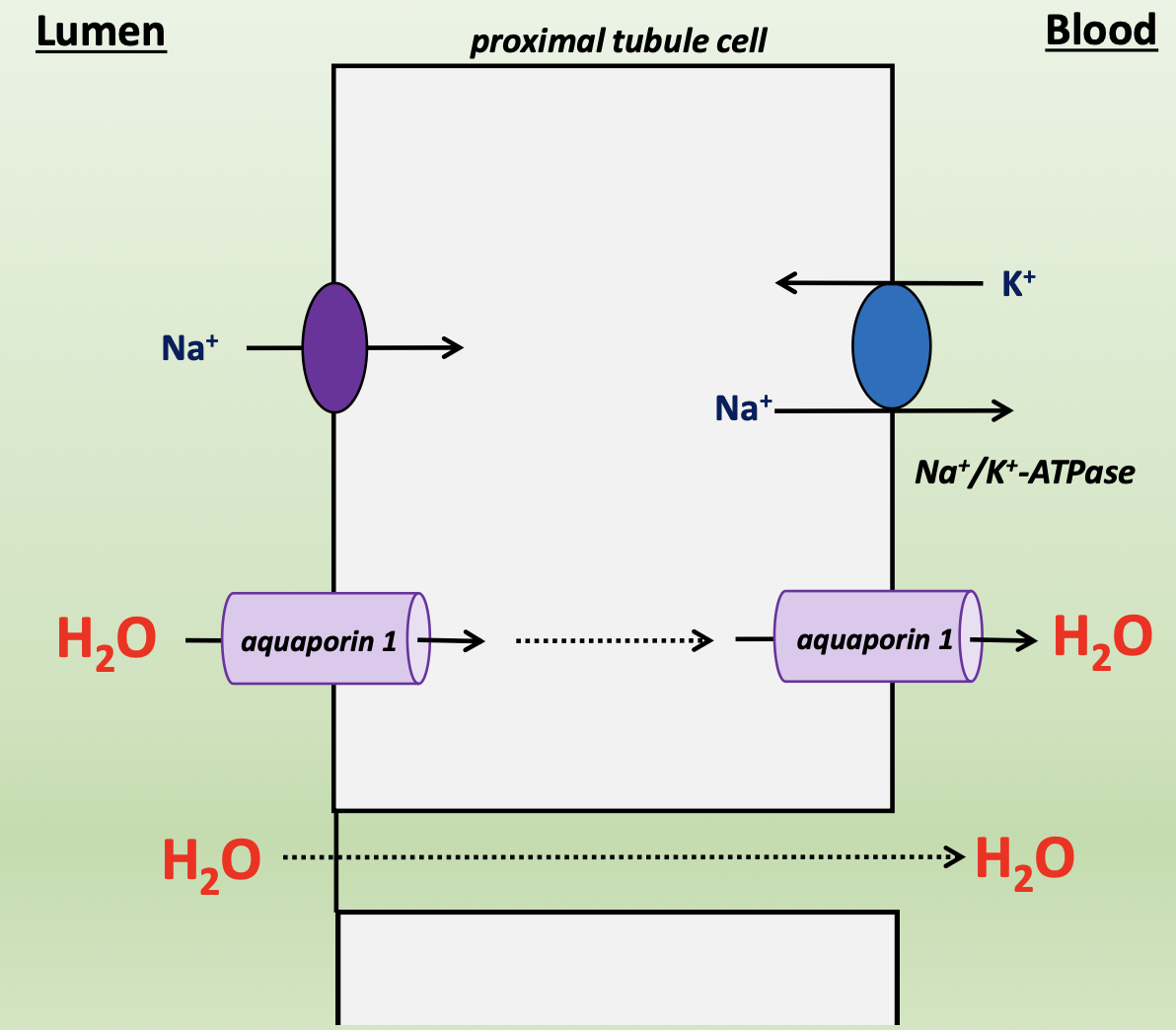
water transport in proximal tubule
as Na+ is reabsorbed, water follows
75% of water reabsorbed trancellularly through aquaporin 1 (apical/basolateral)
25% of water reabsorbed paracellularly through tight junctions
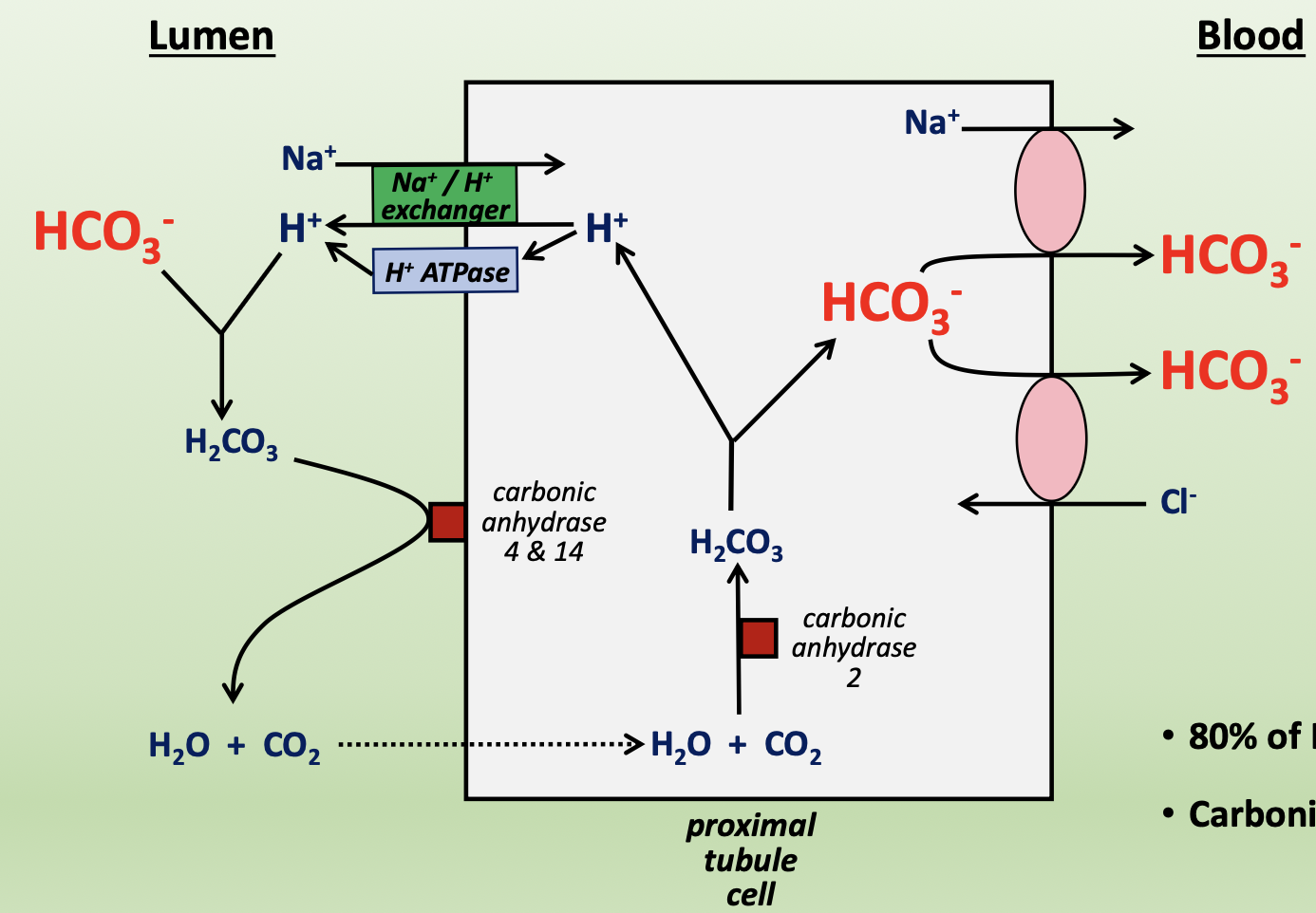
HCO3- transport in proximal tubule
80% of HCO3- is reabsorbed from proximal tubule, with carbonic anhydrase playing a key role in reabsorption
in the lumen (apical)
H+ is pulled out of cell via Na+/H+ exchanger and H+-ATPase
H+ combines with HCO3- to form H2CO3
H2CO3 converts to water and CO2 via carbonic anhydrase 4 and 14
water and CO2 passively diffuse into cell
in proximal tubule cell
water and CO2 combine via carbonic anhydrase 2 to form H2CO3
H2CO3 breaks down into H+ and HCO3-
in the blood (basolateral)
HCO3- is transported into cell via Na+ co-transporter or Cl- counter-transporter
amino acid transport in proximal tubule
filtered small proteins get broken down by proteases in proximal tubule brush border or endocytosed and hydrolyzed by peptidases
amino acids are reabsorbed by a variety of transporters, specific for each amino acid (apical/basolateral)
drug transport in proximal tubule
penicillin, drugs, and diuretics are secreted by a variety of transporters (apical/basolateral)
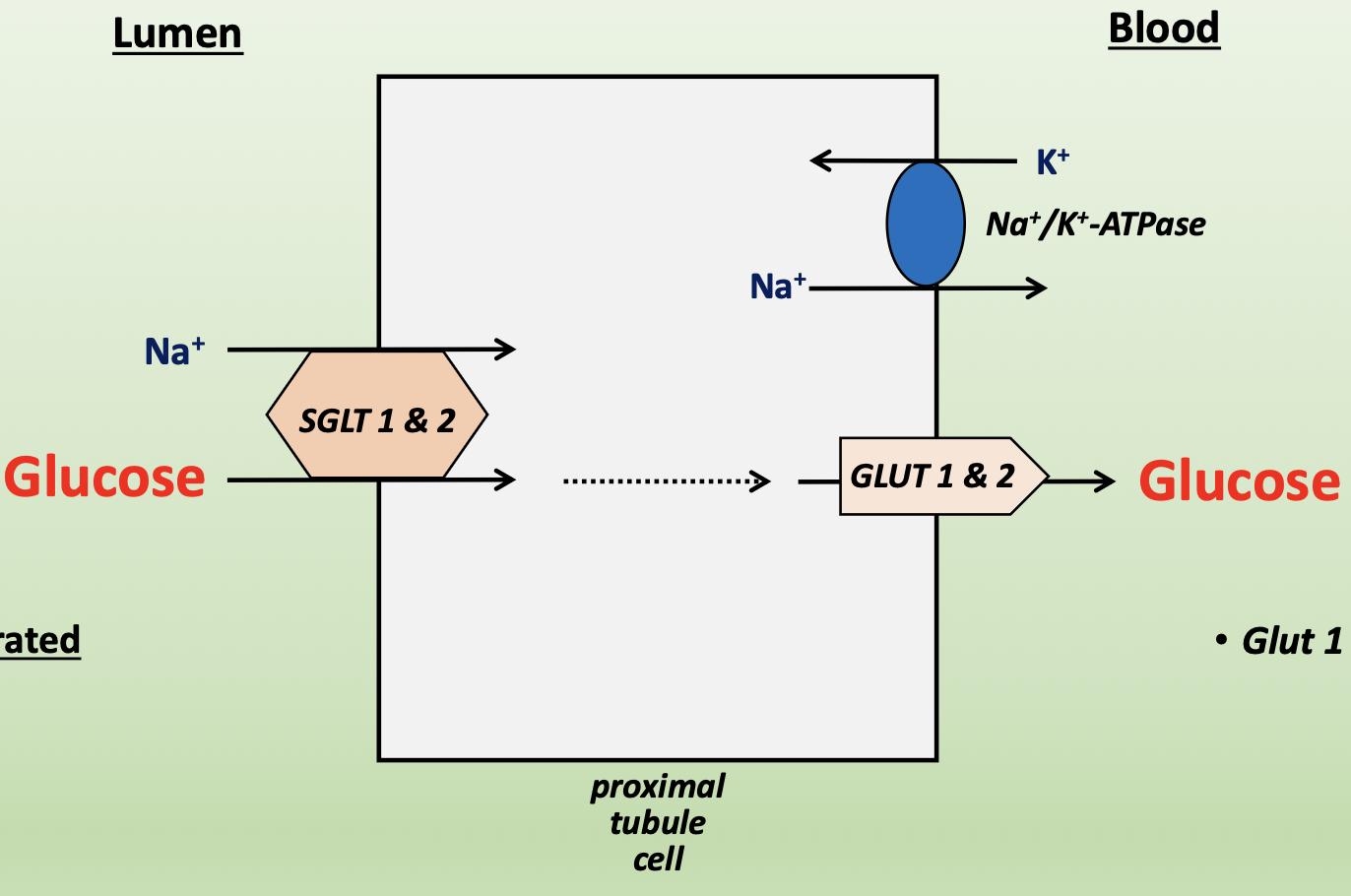
glucose transport in proximal tubule
glucose is reabsorbed from proximal tubule
SGLT1/2 → glucose co-transporter with Na+ from lumen into cell (apical)
secondary active transport due to high glucose concentrations in cell
can become saturated and rate-limiting
GLUT1/2 → facilitated diffusion of glucose from cell to blood (basolateral)
Na+ pumped into blood via Na+/K+-ATPase
glucose reabsorption and secretion
as plasma glucose concentration increases, amount of glucose in tubular lumen (filtrate) increases → filtered load = [plasma] x GFRinulin
reabsorbed → maximum glucose transport from lumen into cell
SGLT1/2 become saturated
Tmglucose = 375 mg/min
excreted → glucose spills into urine and is excreted since transporters or filtered
threshold = 300 mg/dL
splay: curve in reabsorption and secretion lines between threshold and Tm
reflects anatomical and kinetic differences in nephron, variation among nephron transport capacity
increased glucose in filtrate causes osmotic diuresis and increases urine output