ANAT214 post midterm notes
1/131
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
132 Terms
What are the boundaries of the heart relative to the thoracic wall?
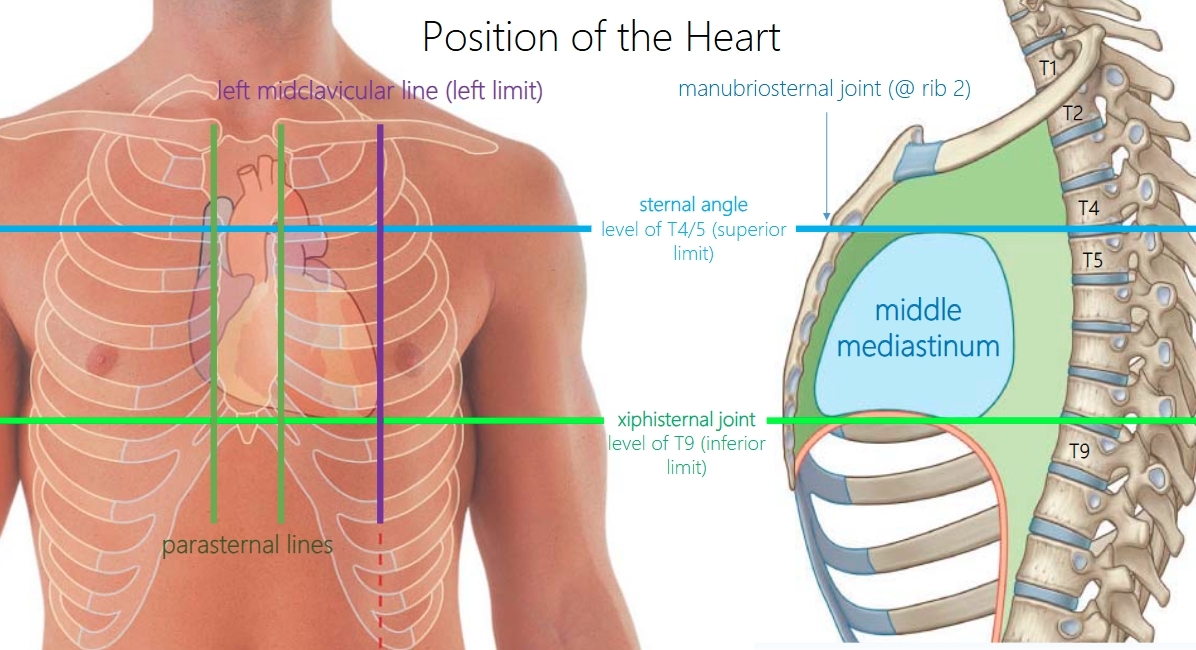
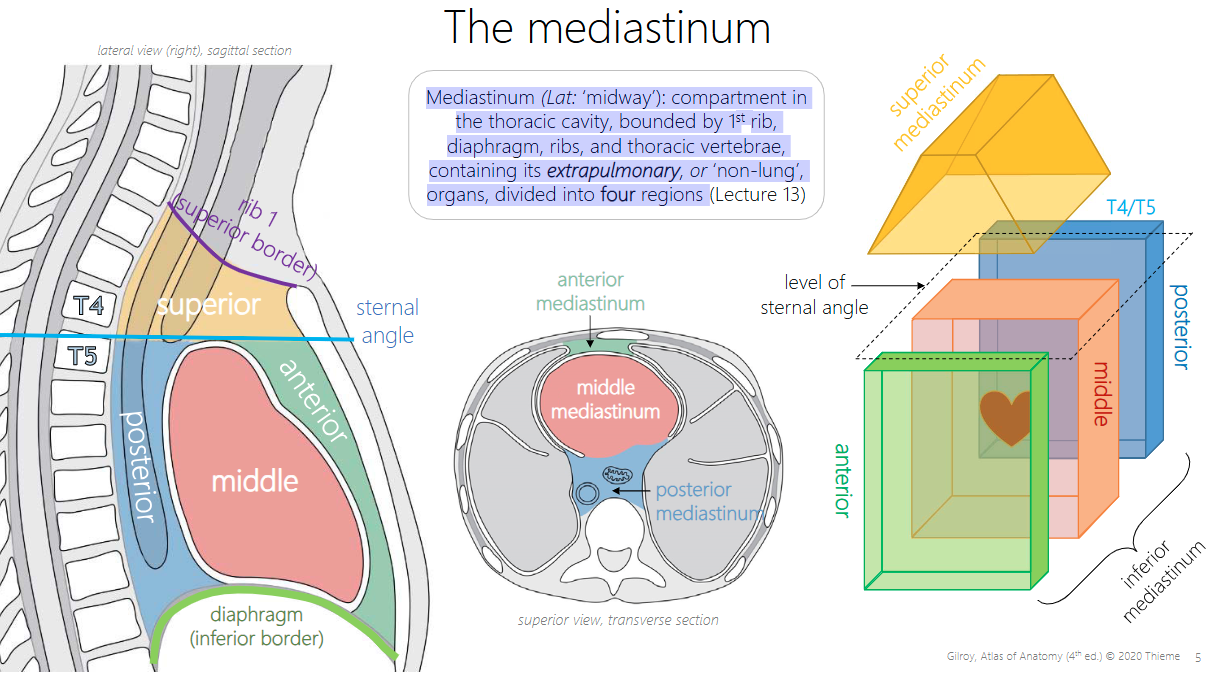
mediastinum
Mediastinum (Lat: ‘midway’): compartment in the thoracic cavity, bounded by 1st rib, diaphragm, ribs, and thoracic vertebrae, containing its extrapulmonary, or ‘non-lung’, organs, divided into four regions (Anterior, middle, posterior, superior)
What are the 4 divisions of the mediastinum? What are their boundaries?
Superior border: Rib 1
Inferior border: Diaphragm
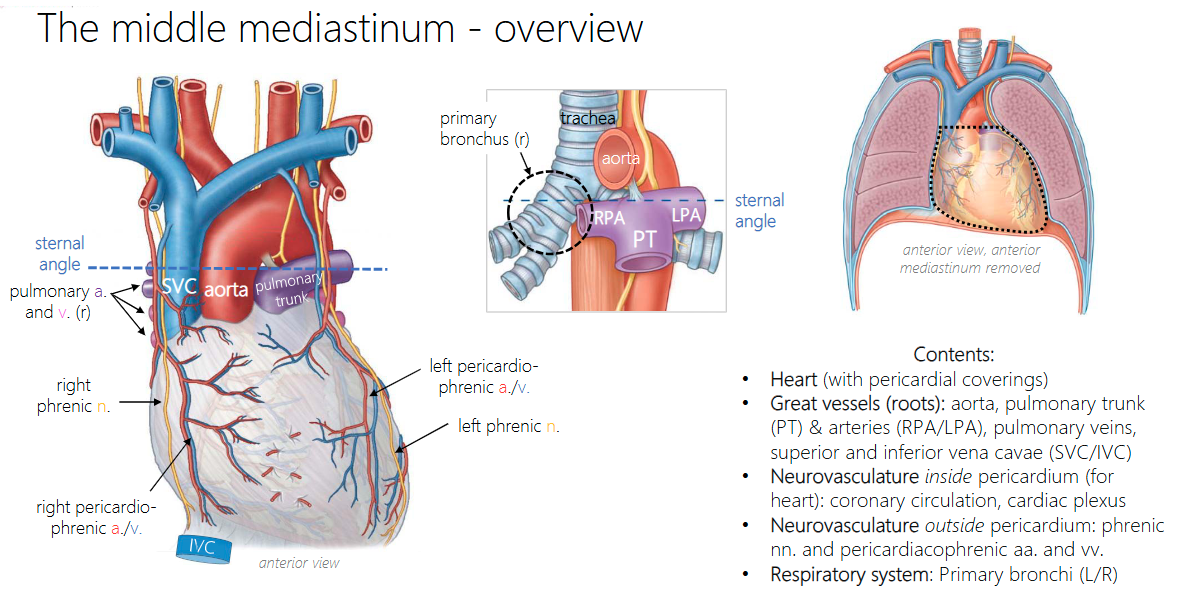
What does the middle mediastinum contain?
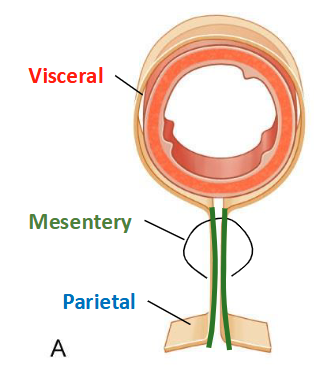
What are the 3 membranes of the heart?
Like the lungs, the heart is enveloped in a continuous double layer of serous membrane – the serous pericardium – enclosing a potential space – the pericardial cavity. Unlike the lungs, the heart has an additional outer membrane – the fibrous pericardium (FC).

Fibrous pericardium
outermost, dense connective tissue, anchored to roots of great vessels, diaphragm, and thoracic wall, may be covered in pericardial fat
restricts the expansion of the heart to help direct blood out the ventricles.
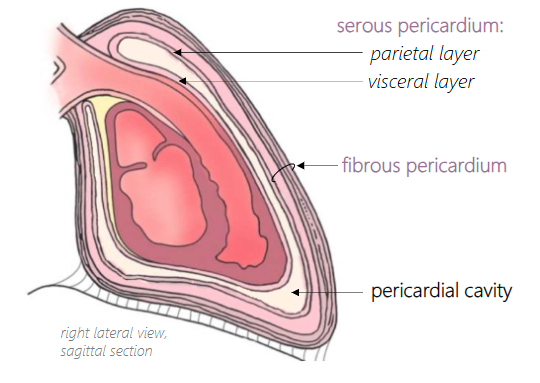
Serous pericardium parietal layer
adhered to deep surface of fibrous pericardium (hard to separate)
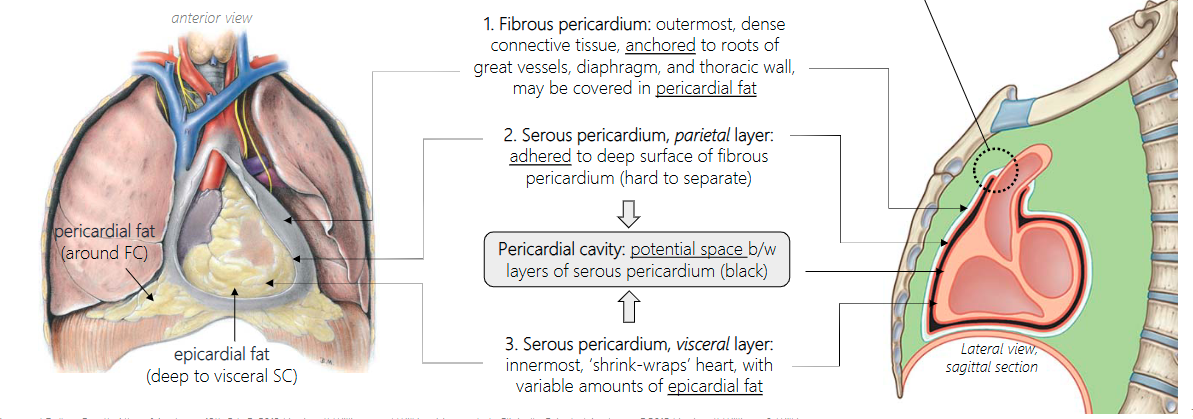
Pericardial cavity
potential space b/w layers of serous pericardium (black)
Serous pericardium, visceral layer
innermost, ‘shrink-wraps’ heart, with variable amounts of epicardial fat
Where does the visceral pericardium become the parietal pericardium?
At the great vessels

Why is there serous fluid in the pericardium?
The pericardial cavity normally contains only a few mL of serous fluid to ease gliding of the beating heart against surrounding tissues.
Pericardial effusion
Buildup of excess fluid in the pericardial cavity (i.e., between serous layers). If slow, fibrous pericardium can stretch over time in response
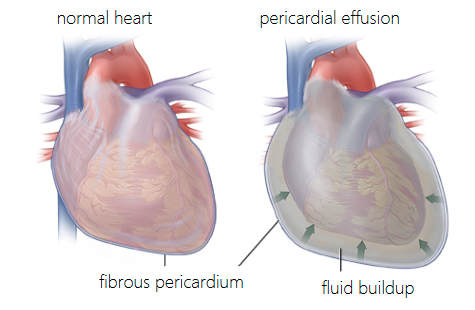
Cardiac tamponade
large and/or rapid pericardial effusion causes heart to accelerate to maintain blood volume pumped, despite decreasing pericardial space, heart may stop beating. Intervention: pericardiocentesis
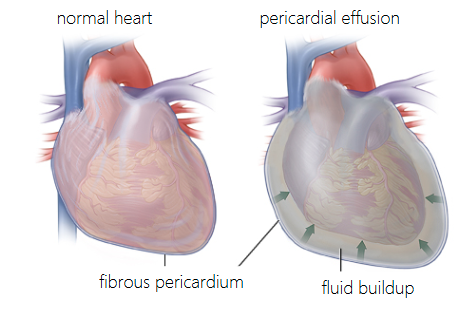
What’s the anatomical position of the heart?
In anatomical position, the heart is rotated left around the longitudinal axis, and its inferior end (apex) is tilted left and anteriorly. Different chambers are visible on anterior and posterior surfaces
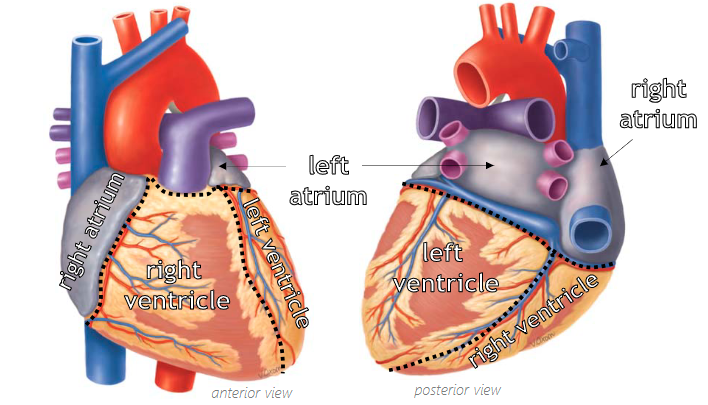
What are the 2 sulci of the heart?
Atrioventricular & Interventricular
Atrioventricular sulcus location?
ring around heart, between atria and ventricles
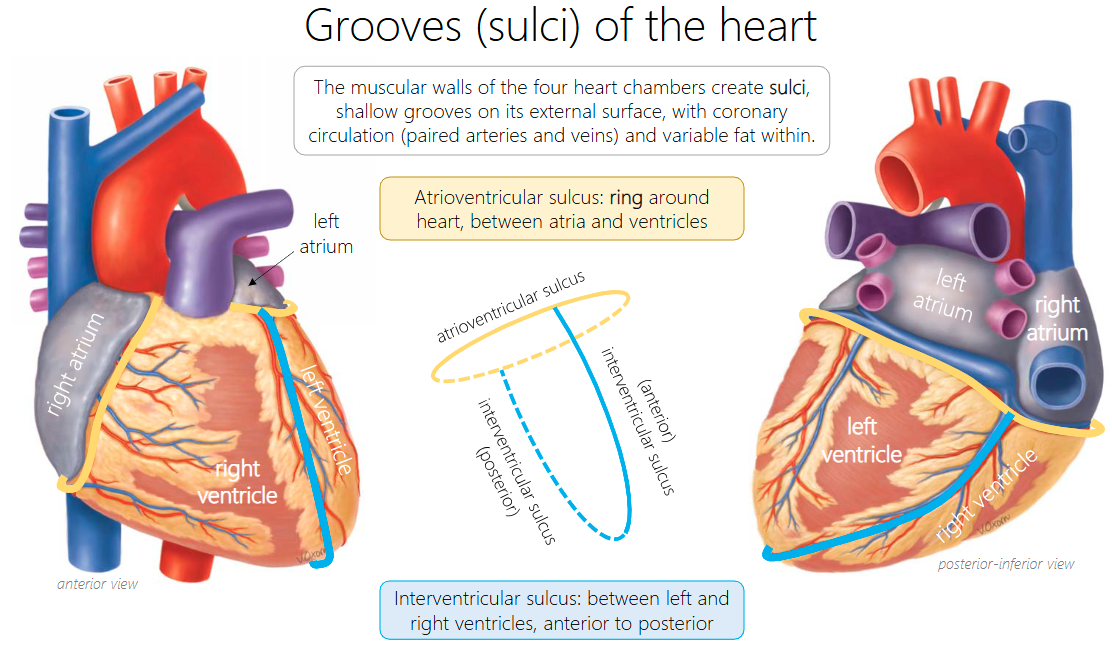
Interventricular sulcus location?
between left and right ventricles, anterior to posterior

Is there communication between left and right pumps in the heart?
No
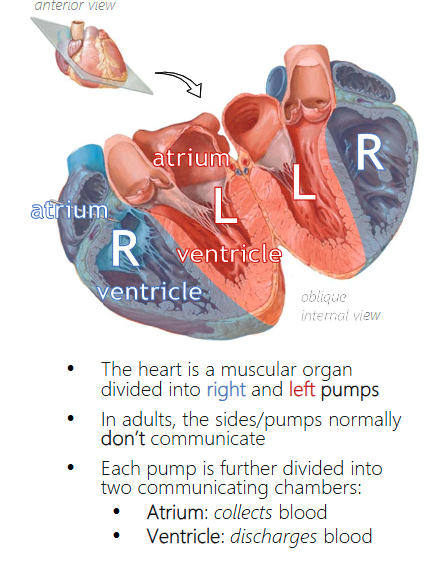
What circulation does the right pump contribute to?
Pulmonary
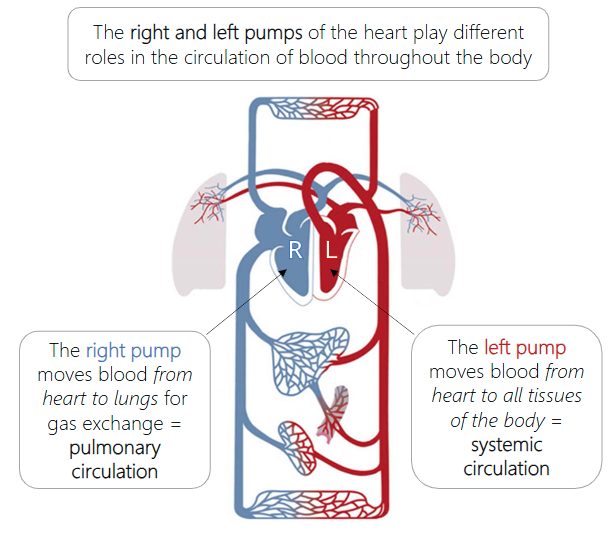
What circulation does the left pump contribute to?
Systemic
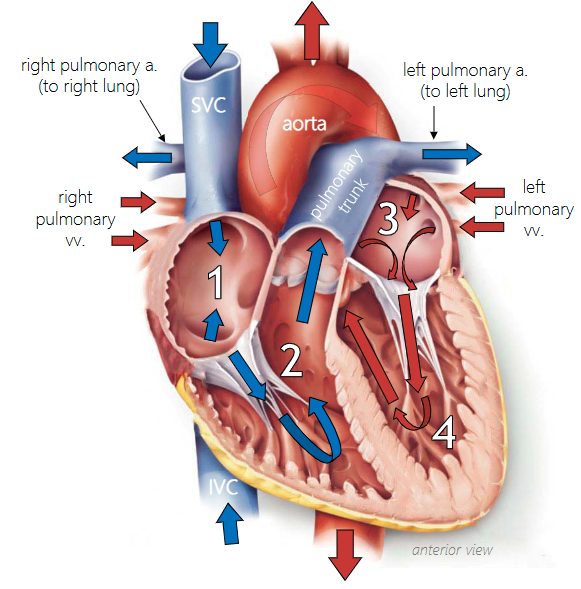
Cardiac blood flow
1. Deoxygenated blood from systemic circulation
collects into RIGHT ATRIUM (from vena cavae &
coronary circulation), and passes into right ventricle
2. Deoxygenated blood is then pumped from
RIGHT VENTRICLE into pulmonary trunk & arteries
(2x) and into pulmonary circulation (to lungs)
3. Oxygenated blood from pulmonary circulation
collects in LEFT ATRIUM from pulmonary veins
(4x) and passes into left ventricle
4. Oxygenated blood is then pumped from LEFT
VENTRICLE, into systemic circulation through aorta
and all its branches
Where does the right atrium collect blood from?
Collects deoxygenated blood → from systemic circulation via superior vena cava (SVC), inferior vena cava (IVC), and coronary sinus, the latter two have valves to prevent backflow
Posterior vs anterior wall of the heart
Posterior atrial wall (where vessels enter) is smooth, but anterior & lateral wall contains parallel folds of pectinate muscles, extending into right auricle.
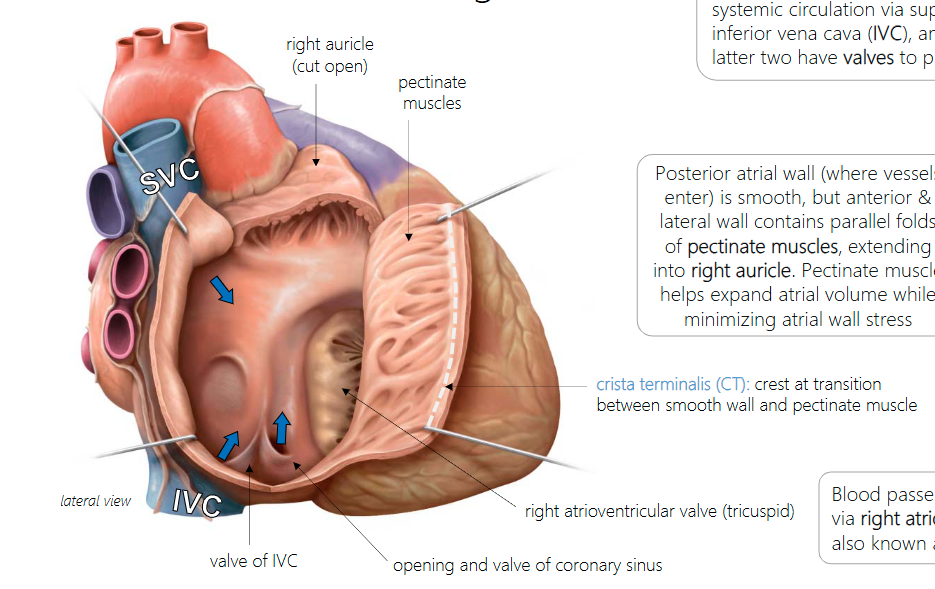
pectinate muscles function?
Pectinate muscle helps expand atrial volume while minimizing atrial wall stress
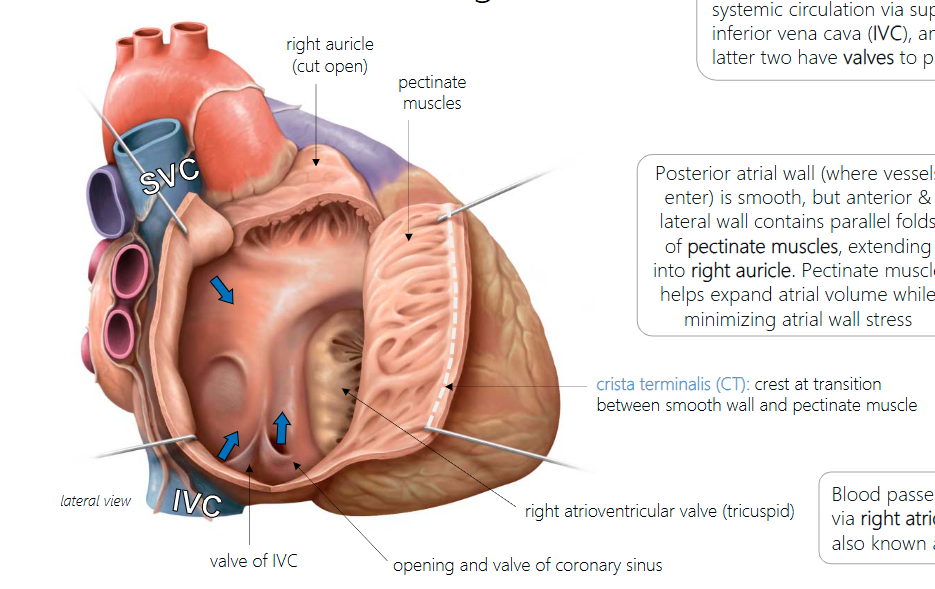
crista terminalis (CT)
crest at transition between smooth wall and pectinate muscle
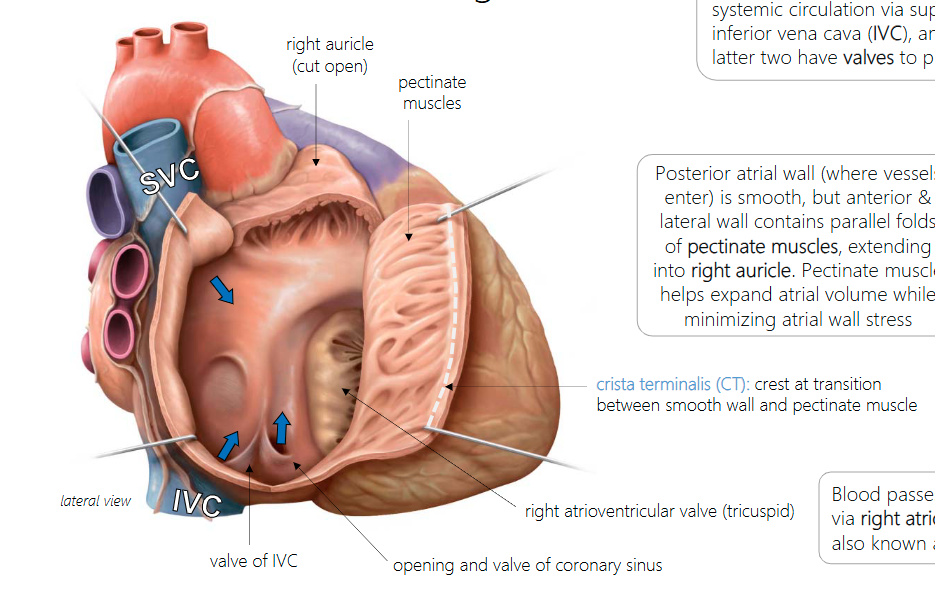
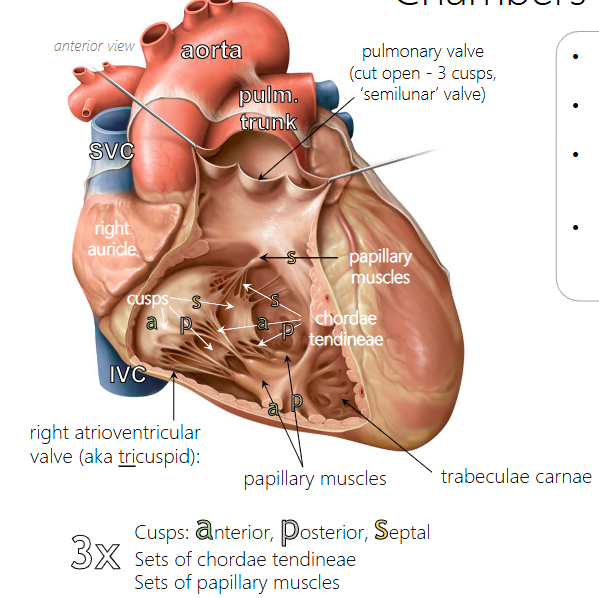
What is the right atrioventricular valve held by?
Three cusps, linked by chordae tendineae to three sets of papillary muscles (anterior, posterior, septal)

chordae tendineae & papillary muscles function?
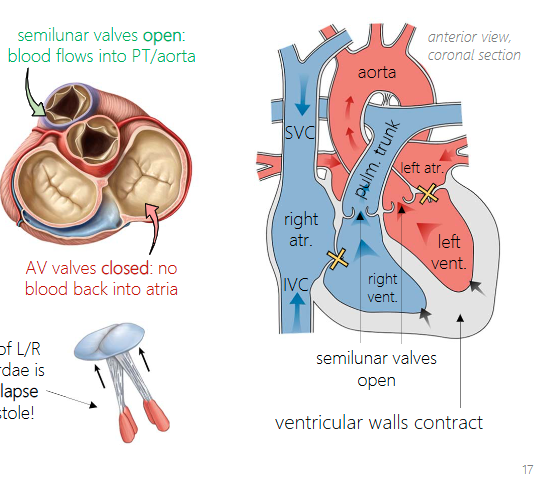
The papillary muscles and chordae ‘hold on’ to the cusps to keep them from prolapsing into the right atrium during ventricular contraction (systole)
trabeculae carnae function?
The ventricle walls, assisted by the trabeculae carnae (‘meaty struts’), pump deoxygenated blood through pulmonary valve (aka right semilunar valve) into the pulmonary trunk
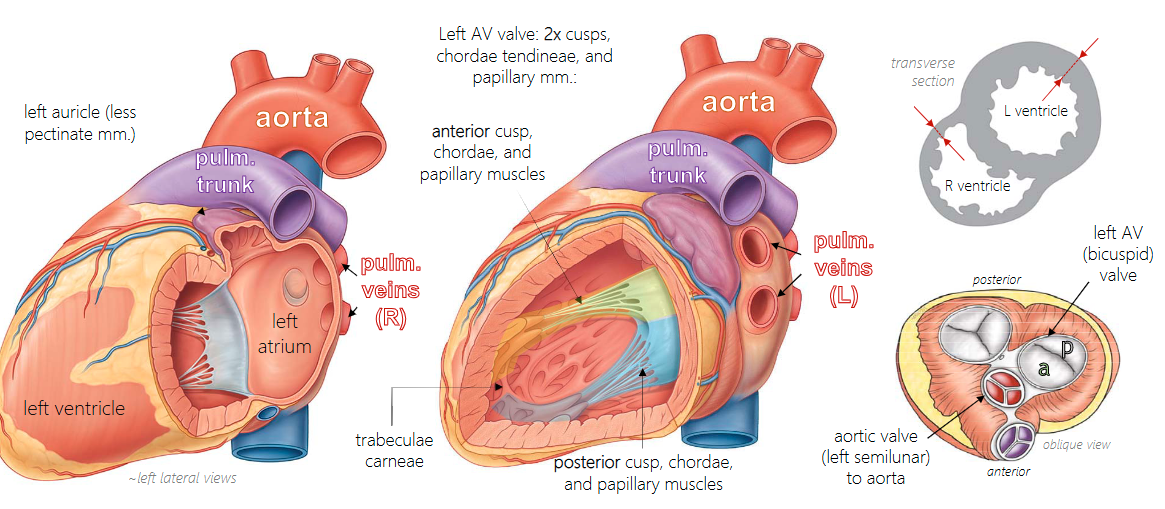
Left vs right atrium/ventricle
(1) four pulmonary veins enter left atrium
(2) left auricle has less pectinate muscle
(3) left atrioventricular valve (aka bicuspid, mitral) has only two sets of cusps/chordae/papillary muscles
(4) ventricular wall thicker
ductus arteriosus (DA)
a duct that allows mixed blood pumped into pulmonary trunk to pass into aorta rather than pulmonary arteries. After birth, it degenerates to form the ligamentum arteriosum

foramen ovale (FO)
is an opening in the wall between the atria that allows mixed blood from the IVC to bypass right ventricle and go into left atrium instead. After birth, it seals to form the fossa ovalis

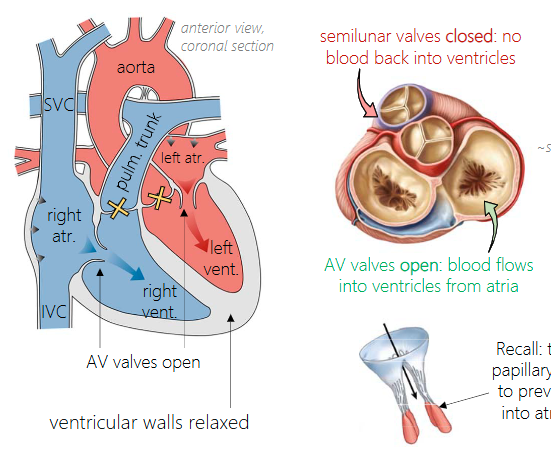
Ventricular diastole
both ventricles relax and refill with blood via open atrioventricular (AV) valves, but semilunar valves are closed to prevent backflow into the ventricles
longer phase
Ventricular systole
both ventricles contract and blood is pumped out via open semilunar valves, but now AV valves are closed to prevent backflow into atria
longer phase
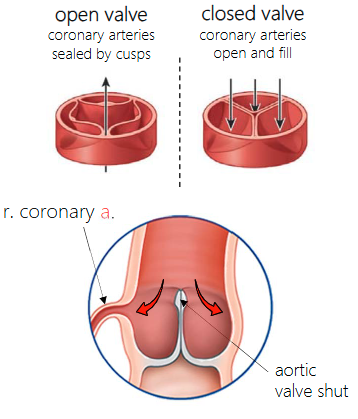
Coronary arteries location?
Their openings are located in sinuses created by the aortic valve cusps
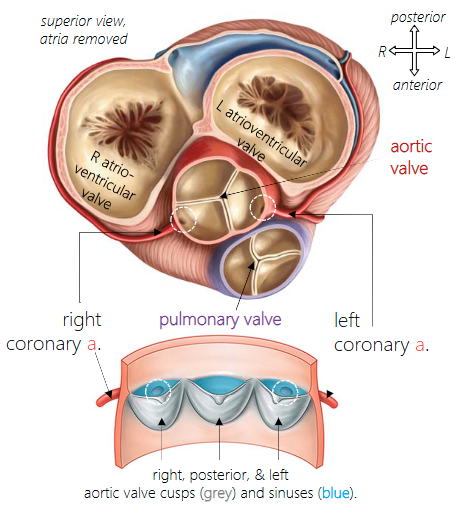
When do the coronary arteries fill with blood?
The aortic valve sinuses and coronary arteries fill with blood when the aortic valve shuts, i.e., during ventricular diastole.
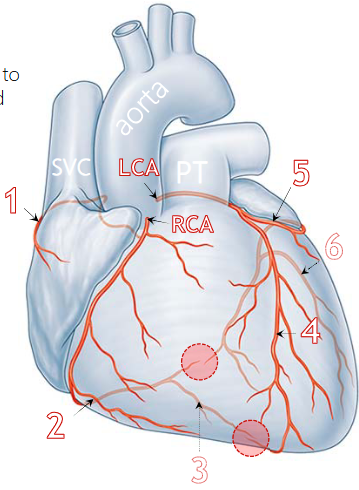
Right coronary artery (RCA) location?
Emerges at anterior/right base of aorta, runs to the right in the atrioventricular sulcus, around to posterior surface.
What are the 3 main branches of the right coronary artery?
What are the 3 main branches of the left coronary artery?
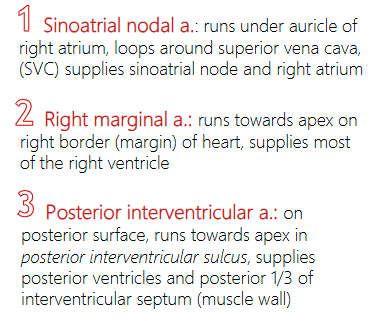
Sinoatrial nodal a. location and function?
(1) runs under auricle of right atrium, loops around superior vena cava, (SVC) supplies sinoatrial node and right atrium
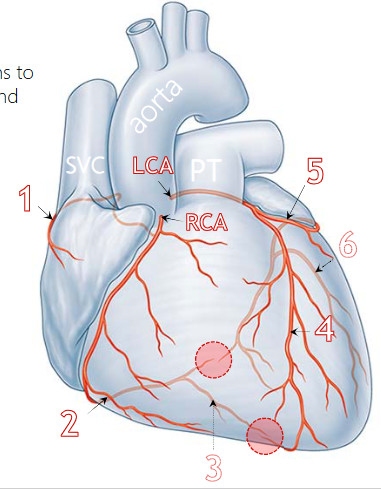
Right marginal a. location and function?
(2) runs towards apex on right border (margin) of heart, supplies most of the right ventricle
Posterior interventricular a. location and function?
(3) on posterior surface, runs towards apex in posterior interventricular sulcus, supplies posterior ventricles and posterior 1/3 of interventricular septum (muscle wall)
Anterior interventricular a. location and function?
(4) runs towards apex in anterior interventricular sulcus, supplies anterior ventricles and 2/3 of interventricular septum
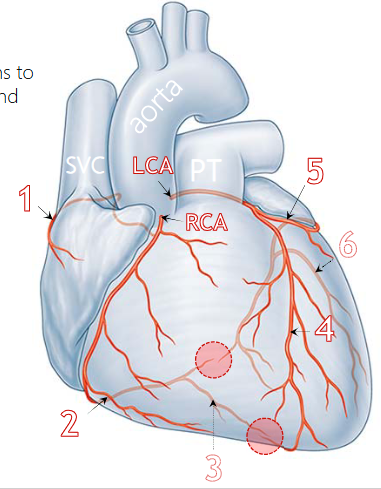
Circumflex a. location and function?
(5) runs under auricle of left atrium, in atrioventricular sulcus, onto posterior surface, supplies left atrium and via #6:
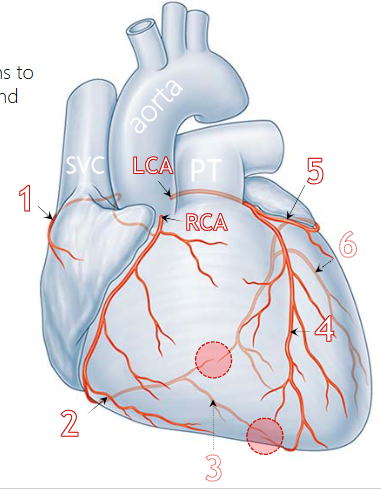
Left marginal a. location and function?
(6) branch of circumflex a., runs towards apex on left border (margin) of heart, supplies most of the left ventricle
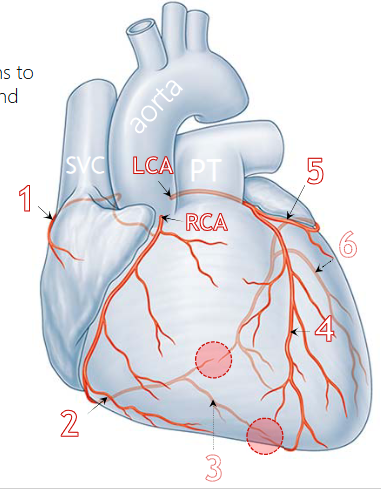
What are the 2 anastomoses in the coronary circulation?
between end of right coronary and circumflex aa., and between anterior and posterior interventricular aa.
red circle

What veins does the heart drain into?
Cardiac veins
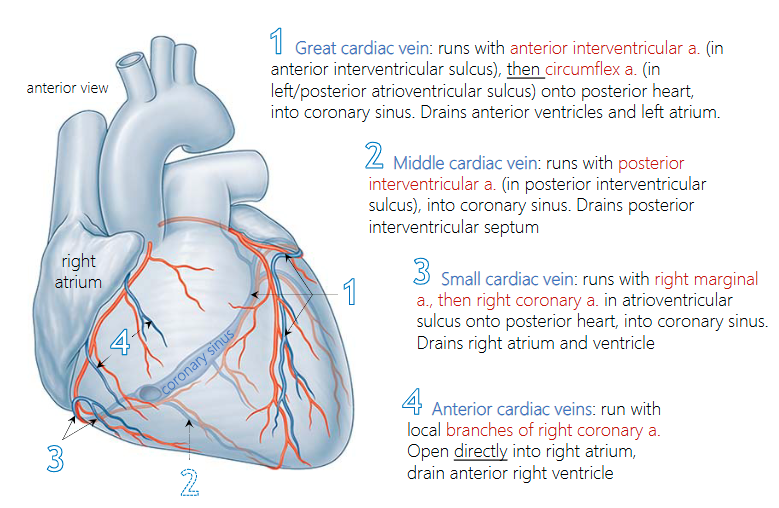
What 2 coronary veins does the Great cardiac vein run with? What and where does it drain?
(1)
runs with the anterior interventricular a. & circumflex a.
Drains the anterior ventricles and left atrium.
Drains into the coronary sinus
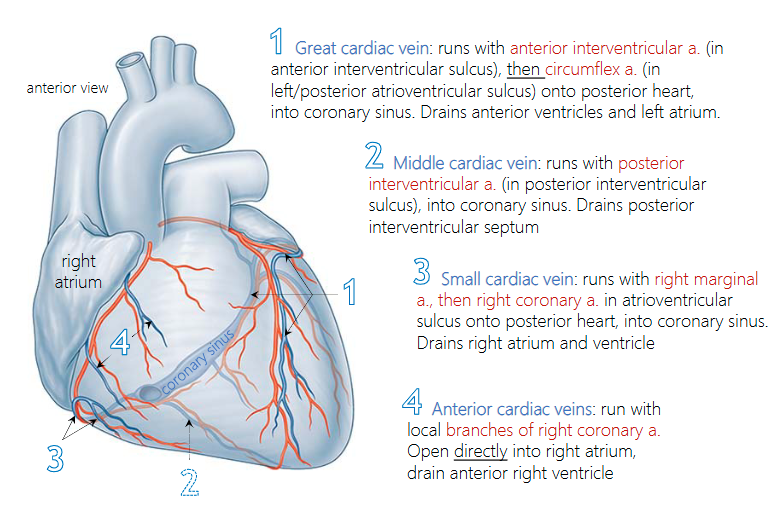
What 2 coronary veins does the middle cardiac vein run with? What and where does it drain?
(2)
runs with the posterior interventricular a
Drains the posterior interventricular septum
Drains into the coronary sinus
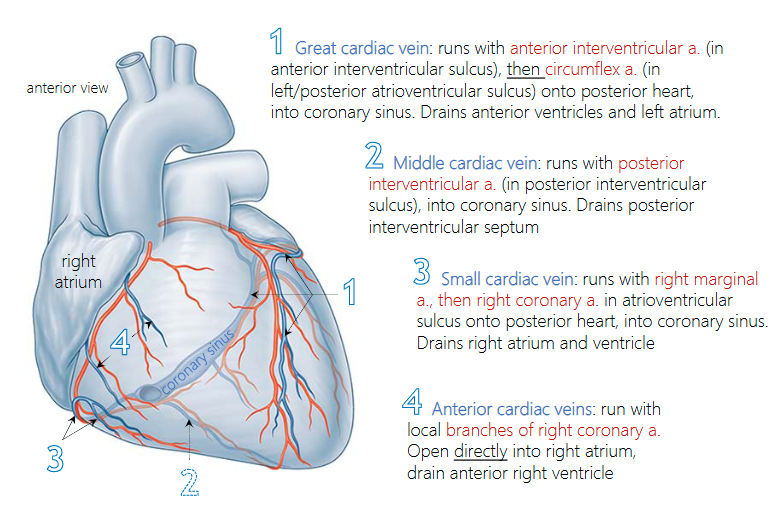
What 2 coronary veins does the small cardiac vein run with? What and where does it drain?
runs with the right marginal a. & right coronary a.
Drains the right atrium and ventricle
Drains into the coronary sinus
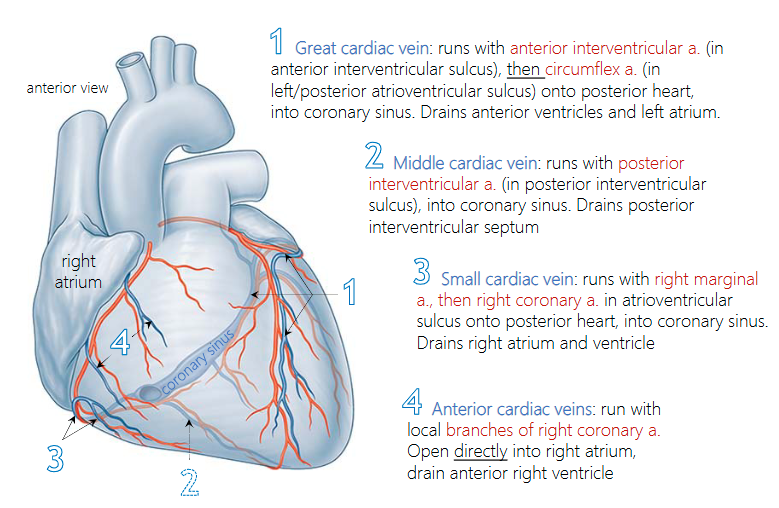
What 2 coronary veins does the anterior cardiac vein run with? What and where does it drain?
runs with the branches of right coronary a.
drains into the right atrium
drains the anterior right ventricle
Coronary sinus
swelling in atrioventricular sulcus that collects venous blood from great, middle and small cardiac veins, opens into right atrium near inferior vena cava (IVC)

What is the efferent (motor) component of the heart?
somatic nervous system, with voluntary control, and an autonomic nervous system (ANS), providing involuntary control over internal organs, smooth & cardiac muscle, and glands
Where does sympathetic control of the heart come from?
comes from ‘sympathetic cardiac nerves’ arising from the cervical ganglia and the sympathetic chain (T1-T4)
Increase HR
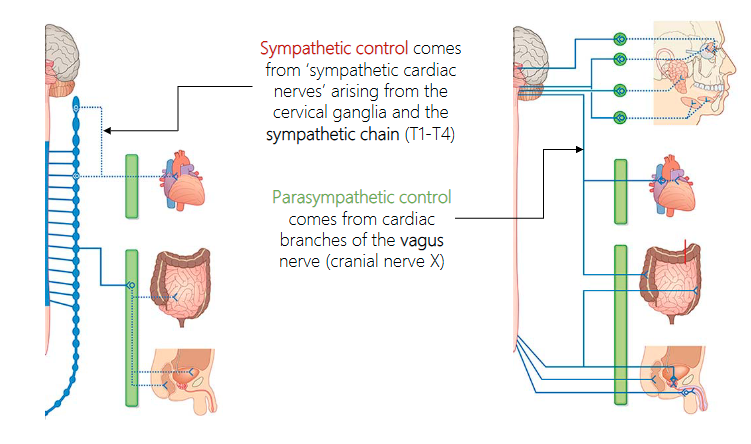
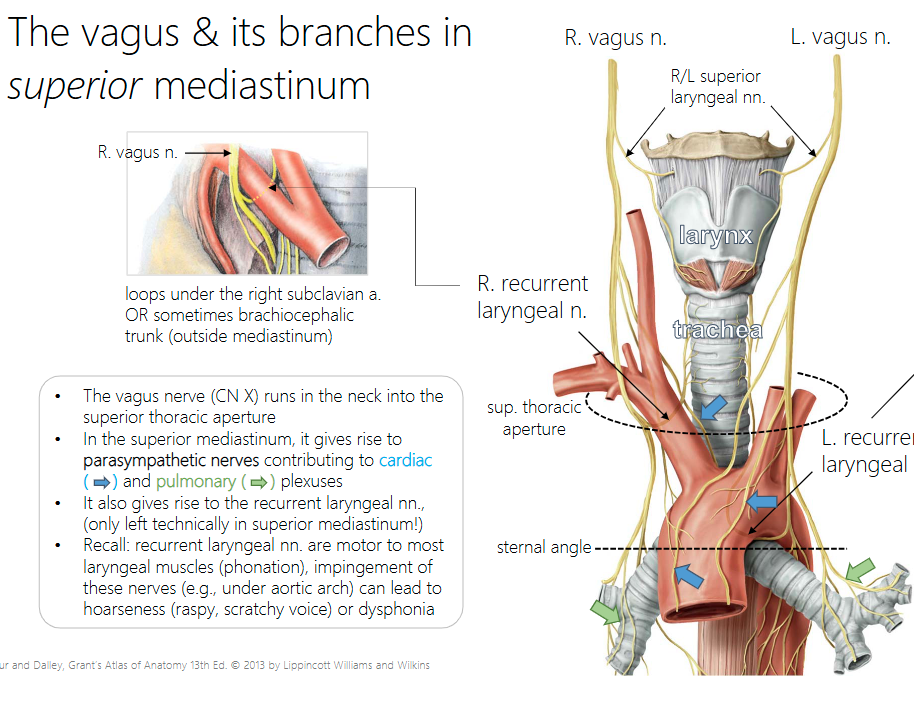
Where does parasympathetic control of the heart come from?
comes from cardiac branches of the vagus nerve (cranial nerve X)
Decrease HR
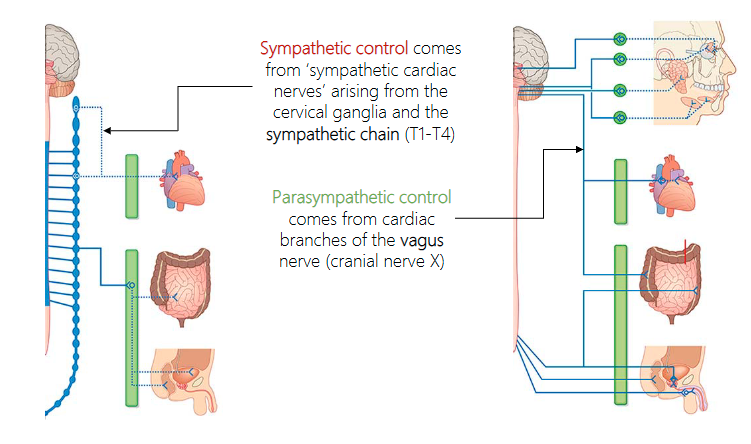
cardiac plexus
SNS & PSNS fibers mesh to form a cardiac plexus, providing branches to conduction system of heart, coronary vasculature, and myocardium (heart muscle walls)
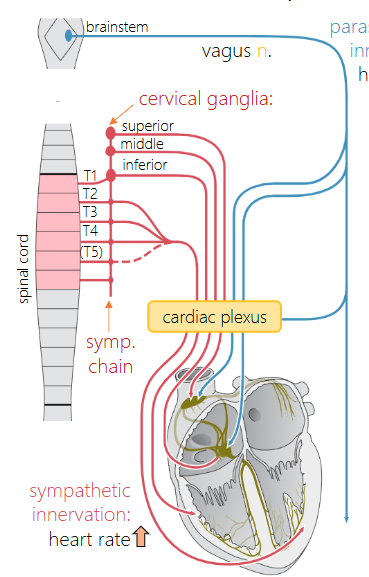
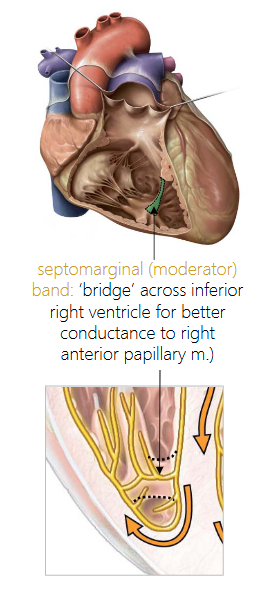
septomarginal (moderator) band
‘bridge’ across inferior right ventricle for better conductance to right anterior papillary m.)
What’s the natural peacemaker of the heart
the SA node is the heart’s natural pacemaker, here’s the artificial version
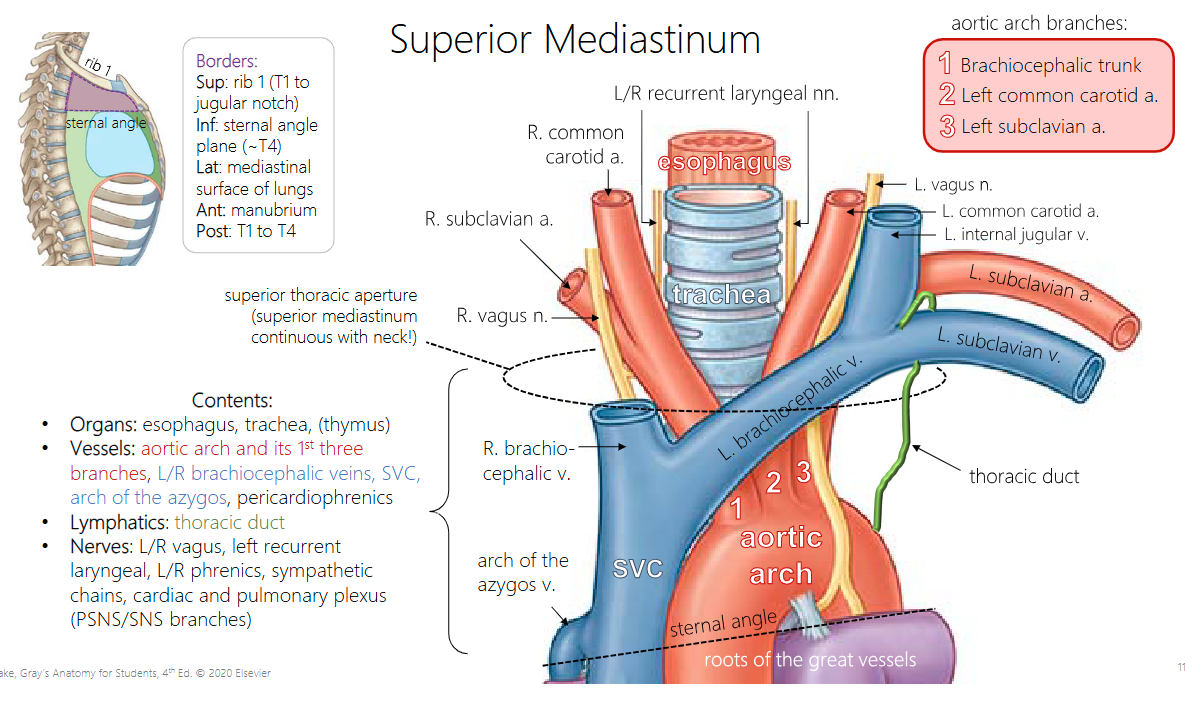
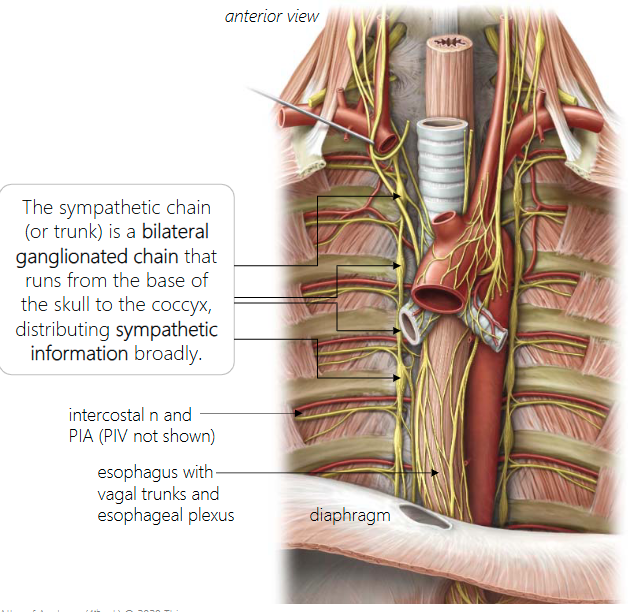
What does the superior mediastinum contain?
• Organs: esophagus, trachea, (thymus)
• Vessels: aortic arch and its 1st three branches, L/R brachiocephalic veins, SVC, arch of the azygos, pericardiophrenics
• Lymphatics: thoracic duct
• Nerves: L/R vagus, left recurrent laryngeal, L/R phrenics, sympathetic chains, cardiac and pulmonary plexus (PSNS/SNS branches
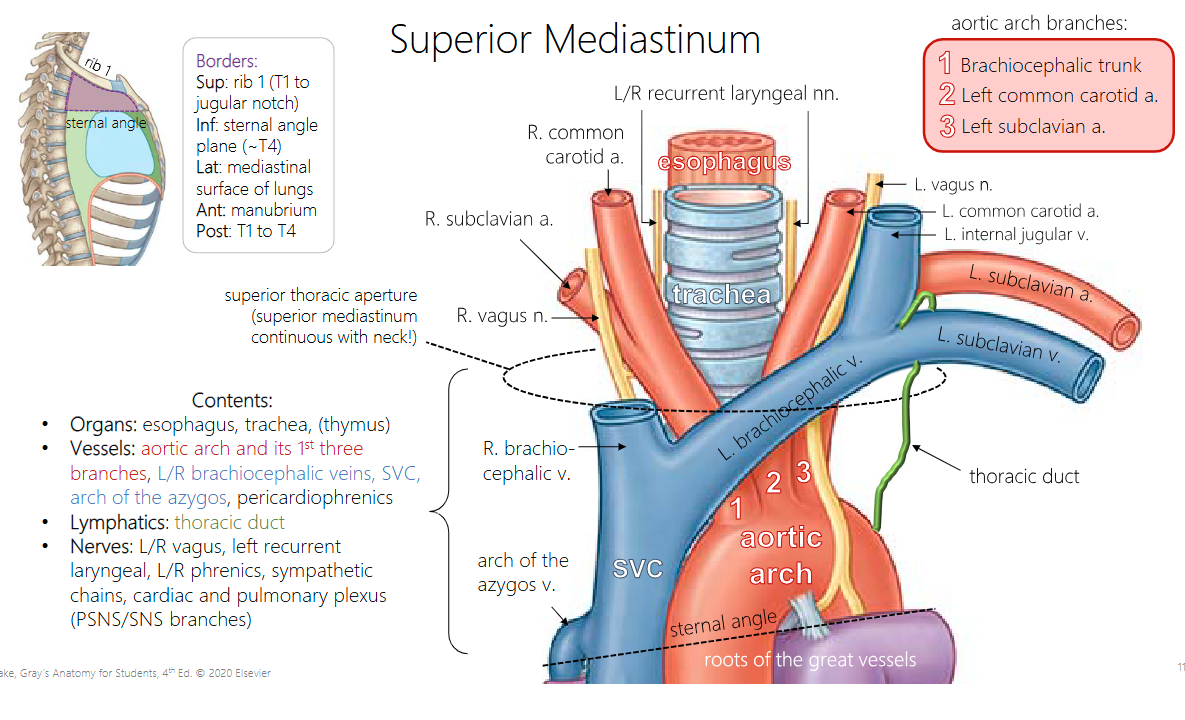
What are the 3 aortic branches?
How does the left recurrent laryngeal nerve travel differently from the right?
The left loops under aortic arch, posterior to ligamentum arteriosum, in superior mediastinum
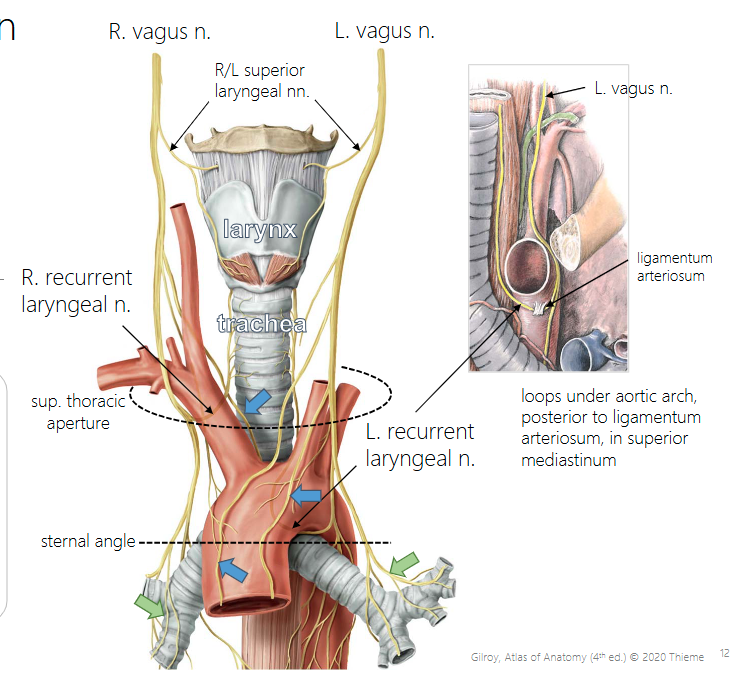
How does the right recurrent laryngeal nerve travel differently from the left?
The right loops under the right subclavian a. OR sometimes brachiocephalic trunk (outside mediastinum)
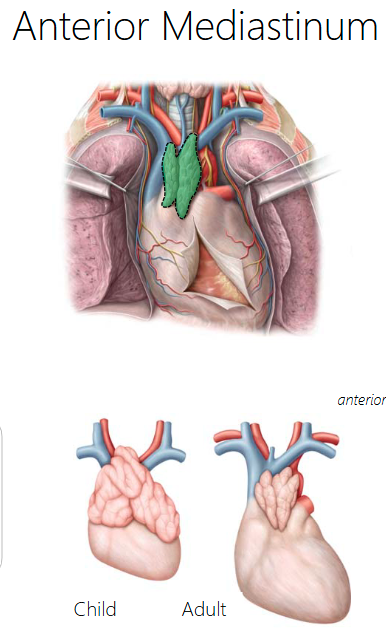
Where is the thymus gland located?
Anterior mediastinum
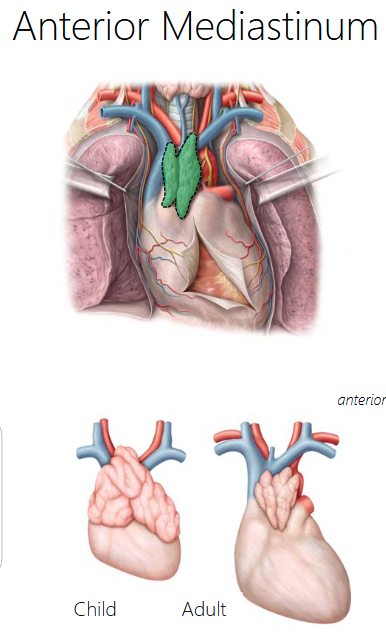
Thymus gland function?
a lymphoid organ responsible for the differentiation of T-cells (T lymphocytes). There are also lymph nodes, fat and connective tissue
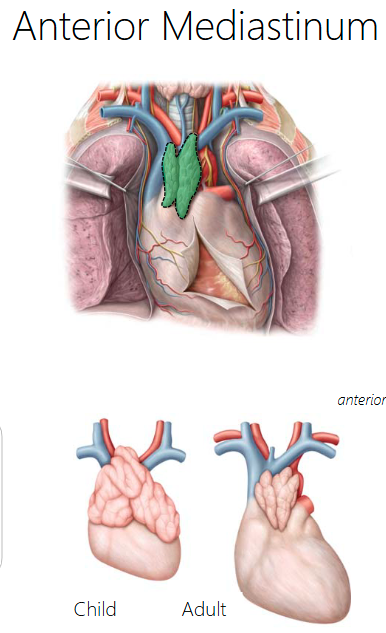
Is the thymus gland larger in children or adults? What happens as you get older?
the thymus is relatively larger in children/youth, and will degenerate and become fibro-fatty tissue in adults
What does the posterior mediastinum communicate with?
Superior mediastinum
What structures do the posterior and superior mediastinum both share?
sympathetic chain, esophagus, vagus nn., aorta (arch + thoracic), azygos (arch + vein), thoracic duct.
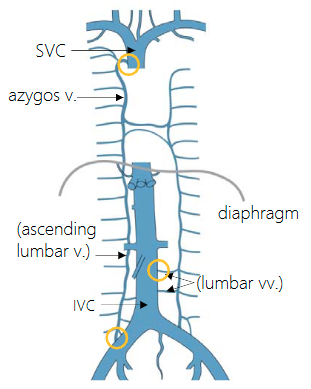
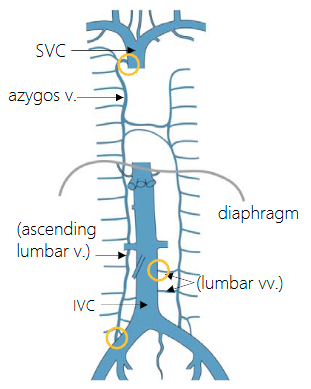
Azygos and hemiazygos vein function?
Azygos and hemiazygos veins drain the posterior thoracic and posterior intercostal veins into the vena cava. But the azygos also offers a collateral passage for venous blood to bypass blockages in the venae cavae (cavo-caval anastomosis)
Anastomoses in the yellow circles run into the superior vena cava to drain
Thoracic duct function?
The thoracic duct is the main ‘collecting’ duct draining ~3/4 of the body’s lymph.

Where does the remaining ¼ of the body’s lymph get drained?
The rest is drained by the right lymphatic duct, both into the brachiocephalic veins at the ‘venous angles’

How is the left hemiazygos vein different from the right?
The left doesn’t drain into the vena cava directly; it crosses over to the right, then it drains through it.
Esophagus function? What does it pass through?
The esophagus is a muscular tube that connects the pharynx to the stomach, running through superior and posterior mediastinum.
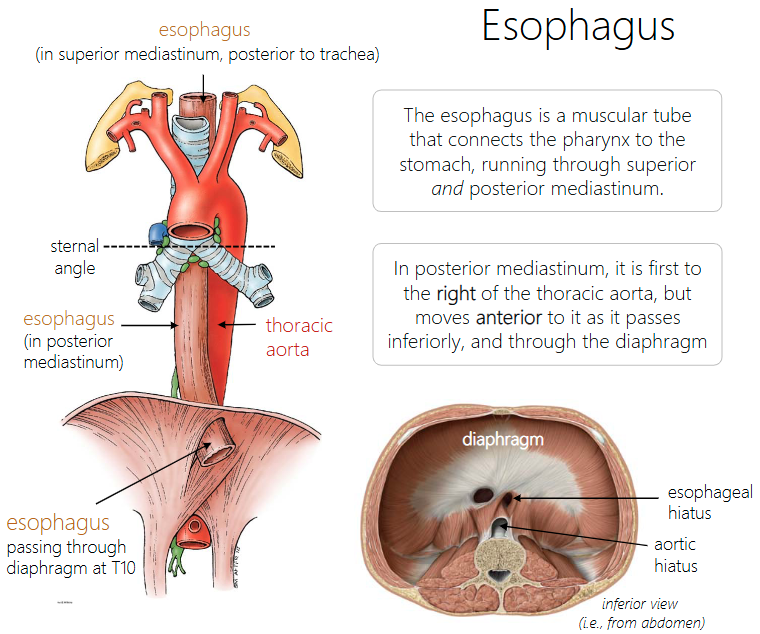
Where is the esophagus located relative to the aorta in the posterior mediastinum? Where does it move as we move inferiorly?
In the posterior mediastinum, it is first to the right of the thoracic aorta, but moves anterior to it as it passes inferiorly, and through the diaphragm.

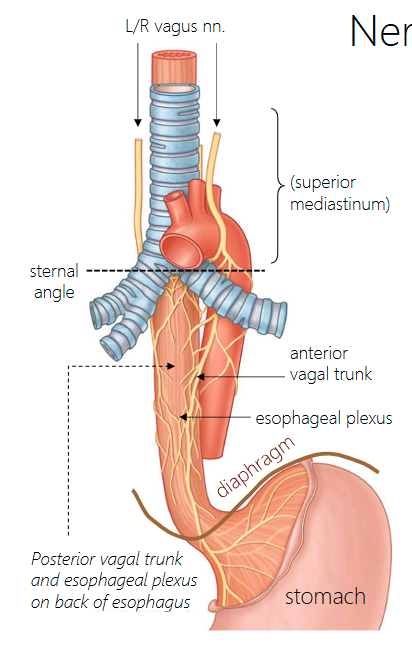
Where do the left and right Vagus shift to after they enter the posterior mediastinum? What do they become?
As they enter the posterior mediastinum, the vagus nerves pass posterior to the hilum of the lungs, lateral to the esophagus. Shortly after, they shift so that left vagus becomes anterior vagal trunk, while right vagus becomes posterior vagal trunk. (mnemonic “LARP”: Left vagus to Anterior vagal trunk, Right vagus to Posterior vagal trunk)
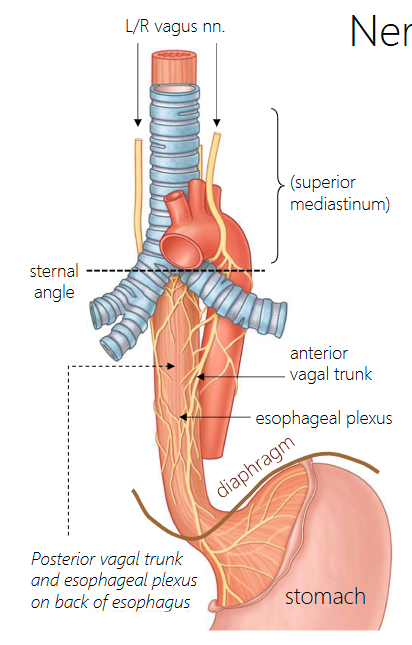
How is the esophageal plexus formed?
The vagal trunks send branches to each other, and join with branches from the sympathetic chain to form the esophageal plexus, providing ANS innervation to the esophageal smooth muscle.
esophageal plexus function?
Peristalsis
What do the vagal trunks innervate?
parasympathetic innervation in the abdomen and GI tract.
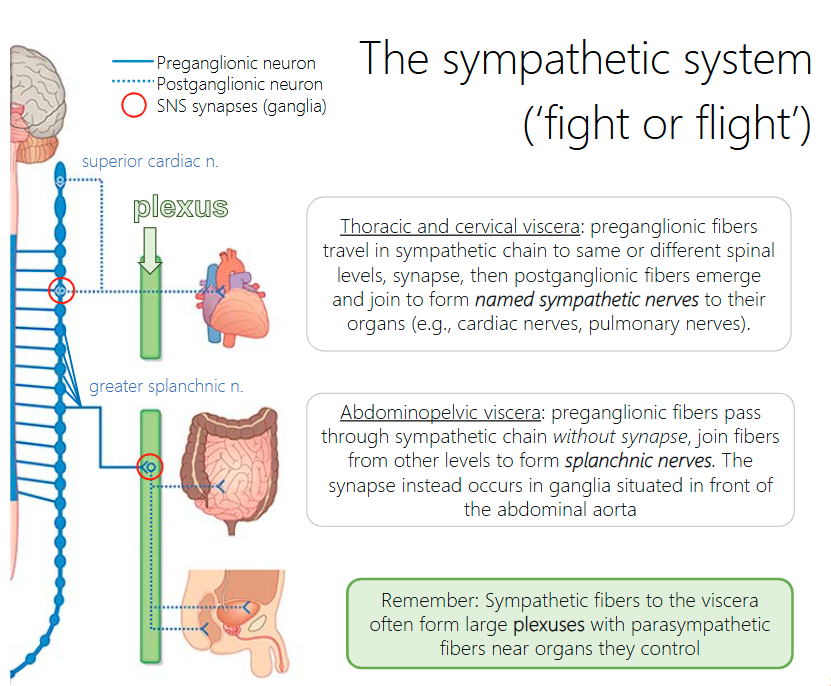
What is the sympathetic chain?
The sympathetic chain (or trunk) is a bilateral ganglionated chain that runs from the base of the skull to the coccyx, distributing sympathetic information broadly.
Explain the pathway that sympathetic thoracic and cervical preganglionic fibers travel to reach their target
preganglionic fibers travel in sympathetic chain to same or different spinal levels, synapse, then postganglionic fibers emerge and join to form named sympathetic nerves to their organs (e.g., cardiac nerves, pulmonary nerves).
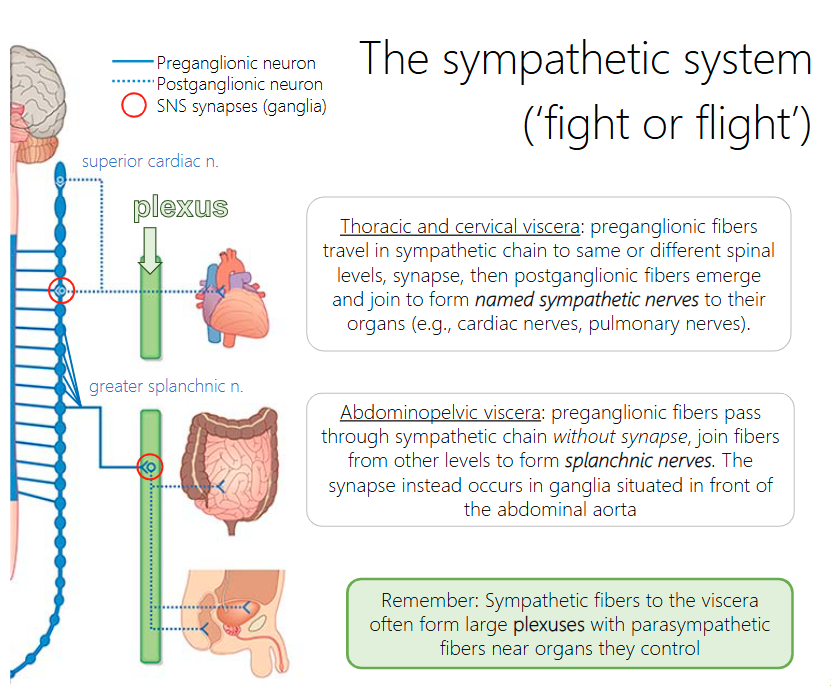
Explain the pathway that sympathetic abdominal preganglionic fibres travel to reach their target
preganglionic fibers pass through sympathetic chain without synapse, join fibers from other levels to form splanchnic nerves. The synapse instead occurs in ganglia situated in front of the abdominal aorta
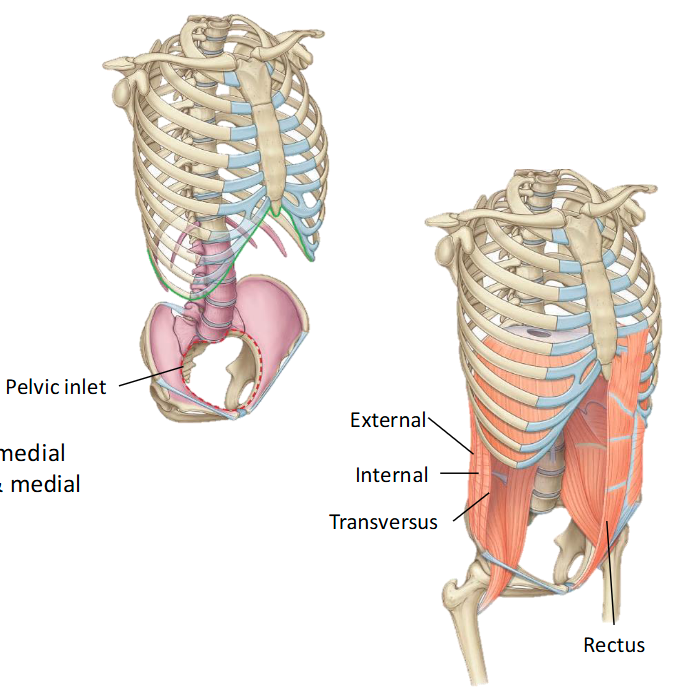
Where is the Abdomen located?
Is a region of the trunk between thorax & pelvis. Composed of abdominal wall & the abdominal cavity.
What are the borders of the abdomen?
Superior: Inferior thoracic aperture – Closed by thoracic diaphragm Inferior: Pelvic inlet
Is the abdominal wall made more of bone or muscle?
Muscle
What bones contribute to the abdominal wall?
• Vertebrae: 5 lumbar vertebrae
• Pelvis: Superior aspect of pelvic bone
• Thorax: Costal margin, rib XI-XII, xiphoid process
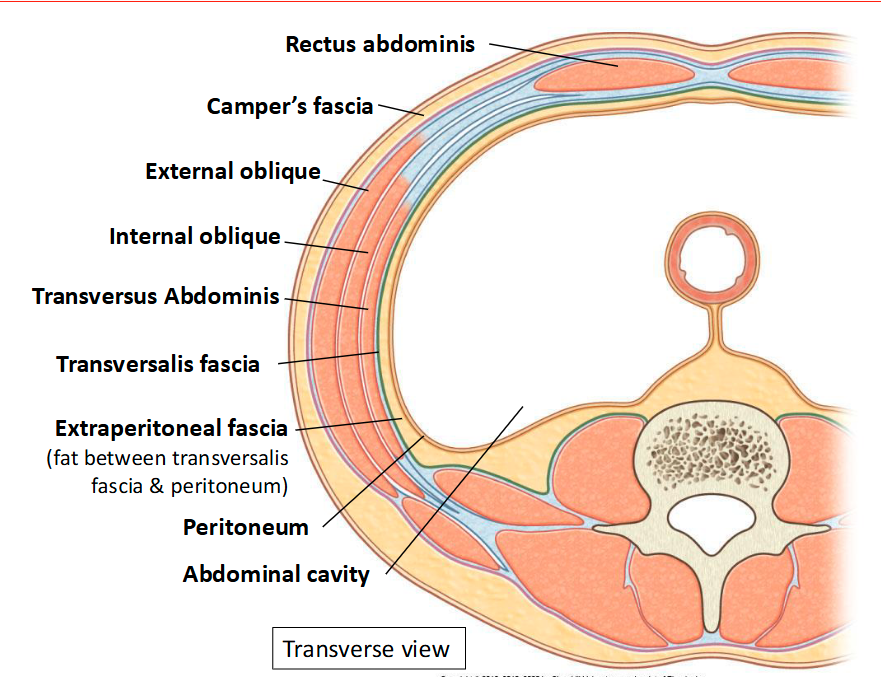
What are the fascia that covers the abdominal wall?
Superficial fascia: under skin (fatty layer – Camper’s) Transversalis fascia: deep to abdominal muscles
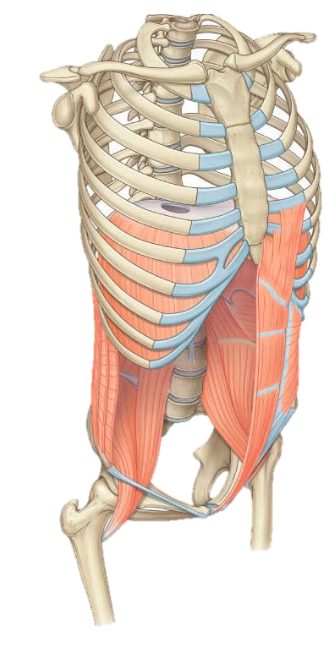
What are muscles of the abdominal wall?
Muscles:
• Post.: quadratus lumborum, psoas, iliacus
• Lat.: Abdominal muscles:
-External oblique: superficial, sup. & lat. to inf. & medial
-Internal oblique: middle layer, inf. & lat. to sup. & medial
-Transversus abdominis: innermost, transverse
• Ant.: Rectus abdominis incased in rectus sheath
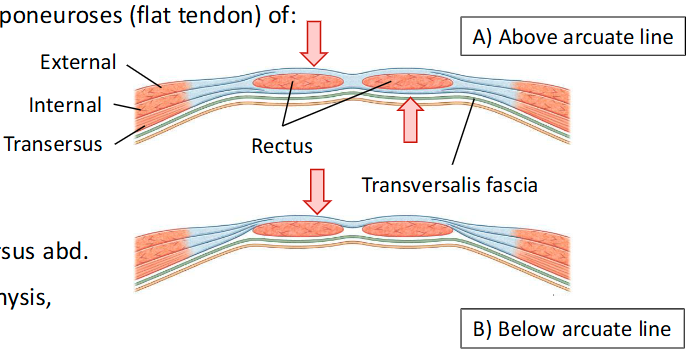
What is the rectus sheath? What is it made by?
Rectus Sheath: Tendinous sheath formed by layering of aponeuroses (flat tendon) of:
• External oblique
• Internal oblique (splits and covers the rectus muscle)
• Transversus abdominis
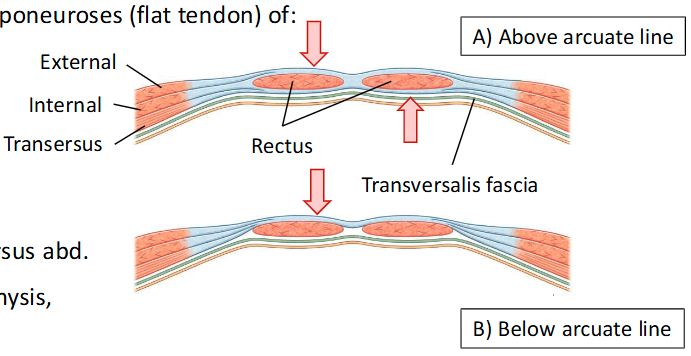
What abdominal muscles can we observe on the anterior and posterior above the arcuate line?
Anterior aspect: external + anterior ½ of internal obliques
Posterior aspect: posterior ½ of internal oblique + transversus abd.
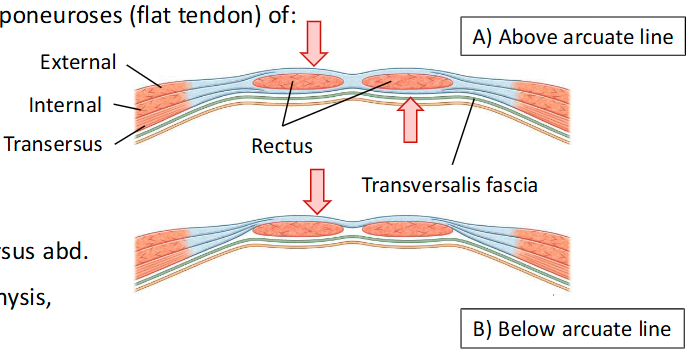
What happens to all the muscles below the arcuate line?
ALL aponeuroses move anterior to rectus abdominis
What creates the other line?
Transition of the abdominal muscles anteriorly makes an arch of fibres = arcuate line
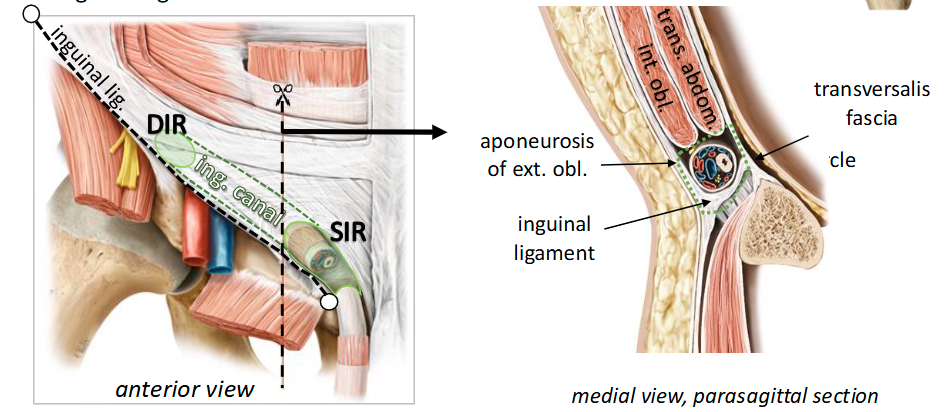
What is the Inguinal Ligament?
This ligament is essentially a thickened, folded portion of the external oblique aponeurosis. It stretches from the anterior superior iliac spine (ASIS) to the pubic tubercle
Inguinal canal function?
Passageway for structures to travel between the abdominal wall and genitalia
Lingual canal boundaries?
••Anterior wall: aponeurosis of ext. oblique -> superficial inguinal ring (SIR)
• Roof: int. oblique and trans. abdominis
• Posterior wall: Transversalis fascia -> deep inguinal ring (DIR)
• Floor: Inguinal ligament
Innervation of the abdominal wall
Skin, abdominal muscles & parietal peritoneum:
• Thoracoabdominal nerves (T7-T11),
• Subcostal nerve (T12) & L1
• Ilioihypogastric T12 & L1
What provides arterial supply to the abdominal wall?
From internal thoracic arteries:
• Musculophrenic: along costal margin
• Superior epigastric: travels post to rectus abdominis
From external iliac arteries:
• Inferior epigastric: travels post to rectus abdominis
Will anastomoses with sup. epigastric artery

If you had a tumour in the visceral pleura/peritoneum, would you feel pain? How about parietal?
Visceral no, parietal yes
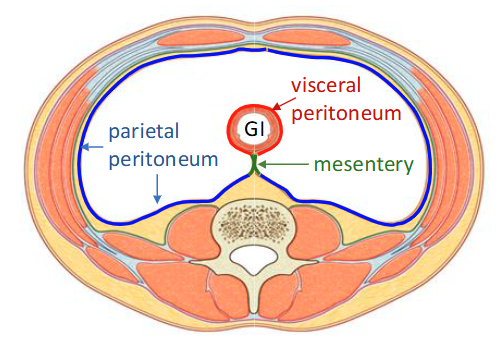
What are the layers of the abdominal cavity? (not a question, understand the picture)
Parietal and visceral peritoneum covers?
Parietal: lines abdominal wall
Visceral: Covers organs
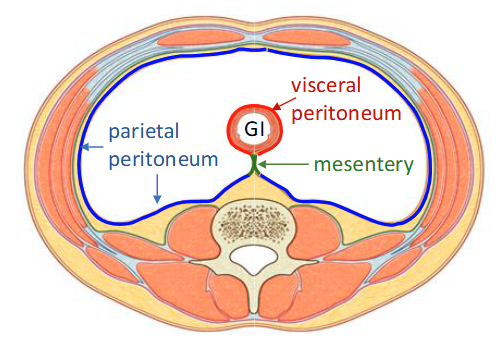
Mesentery
Connects to tubes for stability and allows movement
Mesentery examples?
• Mesentery: small intestine
• Transverse mesocolon: transverse colon
• Sigmoid mesocolon: sigmoid colon
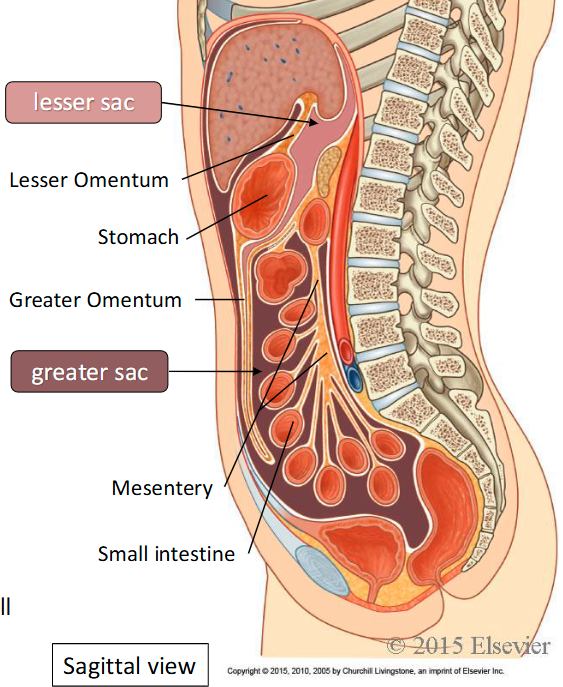
Intraperitoneal Organs
Organs suspended in the peritoneal cavity created by the mesentery